Abstract
Correlates of protection (CoPs) against the highly contagious respiratory disease whooping cough, caused by Bordetella pertussis, remain elusive. Characterizing the antibody response to this pathogen is essential towards identifying potential CoPs. Here, we evaluate levels, avidity and functionality of B. pertussis-specific-antibodies from paired plasma samples derived from symptomatic and recovered pertussis patients, as well as controls. Natural infection is expected to induce protective immunity. IgG levels and avidity to nine B. pertussis antigens were determined using a novel multiplex panel. Furthermore, opsonophagocytosis of a B. pertussis clinical isolate by neutrophils was measured. Findings indicate that following infection, B. pertussis-specific antibody levels of (ex-) pertussis patients waned, while the avidity of antibodies directed against the majority of studied antigens increased. Opsonophagocytosis indices decreased upon recovery, but remained higher than controls. Random forest analysis of all the data revealed that 28% of the opsonophagocytosis index variances could be explained by filamentous hemagglutinin- followed by pertussis toxin-specific antibodies. We propose to further explore which other B. pertussis-specific antibodies can better predict opsonophagocytosis. Moreover, other B. pertussis-specific antibody functions as well as the possible integration of these functions in combination with other immune cell properties should be evaluated towards the identification of CoPs against pertussis.
Introduction
Whooping cough, a highly contagious respiratory disease caused by the Gram-negative bacterium Bordetella pertussis, has resurged despite high vaccine coverage1,2. In the 1990s, the whole cell pertussis vaccine was replaced by the current acellular pertussis vaccine (ACV) in many industrialized countries. The ACV effectively prevents disease. However, protective immunity is lost 4–7 years post-vaccination and this vaccine does not protect against transmission3–5 urging the development of an improved vaccine. Evaluating pertussis vaccine-induced protection poses a problem as correlates of protection (CoPs)6 against pertussis have not been defined. A CoP can be defined as an (immune) marker that statistically correlates with vaccine efficacy but is not necessarily mechanistically responsible for protection6. While high levels of anti-pertussis toxin (Ptx) have been shown to be indicative for protection against disease, no reliable threshold has been established7–9. It is widely accepted that a well-defined CoP will not be unveiled merely by monitoring the antibody levels induced by the ACV10,11. In addition to the quantity, the quality and functionality of antibodies should also be evaluated12. This has not been extensively studied in pertussis, as typically IgG levels and isotypes are measured13.
For pertussis, a CoP would ideally correlate with the inability of the bacterium to colonise the airways and would hence correlate with protection from transmission of this pathogen. One of the functions of antibodies is to facilitate the uptake of bacteria via Fc-γ-receptor-mediated opsonophagocytosis by, for example, neutrophils which play an important role in clearing B. pertussis during infection and thus in preventing colonisation14. The relevance of avidity, indicating the strength by which the antibody binds the antigen, in relation to opsonophagocytosis has not been documented for B. pertussis. However, antibody avidity has been shown to be important for opsonophagocytosis of other bacteria including Streptococcus pneumoniae15.
Natural infection with B. pertussis induces a strong immune response across all age groups13. Compared to vaccine-induced protection, it provides the longest protection from disease with estimates of up to 20 years3. In an attempt to identify CoPs, we evaluated the levels and quality of antibodies directed against nine different virulence factors as well as the functionality of B. pertussis-specific antibodies in paired plasma samples of symptomatic as well as recovered pertussis patients, who are expected to have protective immunity conferred by natural infection. These antigens included the well-studied ACV components, Ptx, pertactin (Prn), filamentous hemagglutinin (FHA) and fimbriae (Fim) 2 and 3 and the virulence factors lipooligosaccharide (LOS), Bordetella resistance to killing A (BrkA), virulence associated gene 8 (Vag8) as well as whole outer membrane vesicles (OMVs). The antibody functionality was assessed by means of an antibody-mediated opsonophagocytosis assay (OPA) using a recently circulating B. pertussis strain. Moreover, integrated analysis of the generated data on levels and avidity was performed in an attempt to identify B. pertussis-specific antibodies predictive for opsonophagocytosis of this pathogen as potential CoPs against pertussis.
Results
Waning of antigen-specific antibodies years after B. pertussis infection
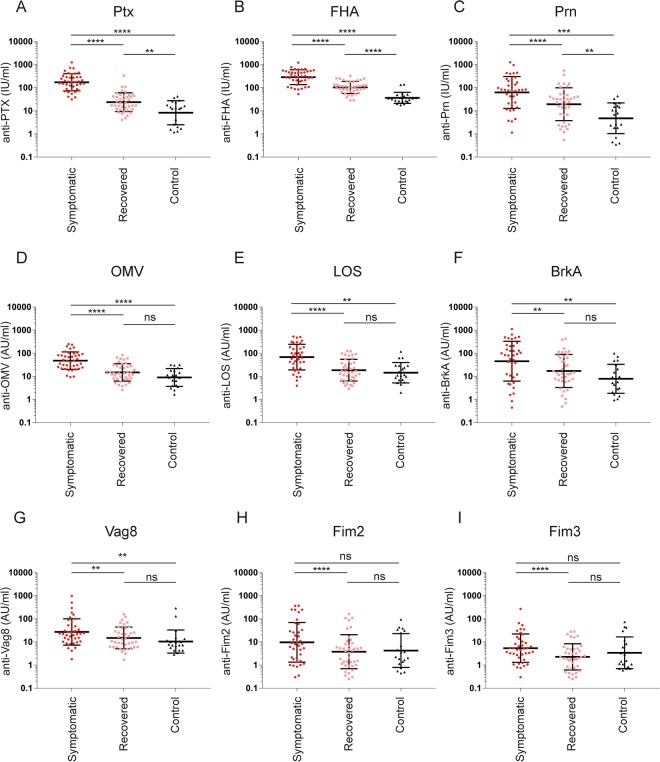
To characterize the natural antibody response to B. pertussis we determined levels of IgG, not only against the well-studied vaccine antigens Ptx, FHA, Prn, Fim2 and Fim313,16, but also against Vag8, BrkA, LOS and OMVs using paired plasma samples of symptomatic and recovered pertussis patients and controls (Fig. 1).
Figure 1.
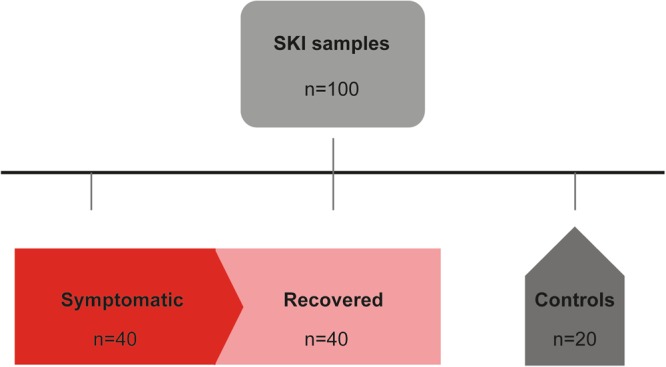
Schematic representation of SKI plasma samples used in this study. 100 plasma samples were selected from the SKI study which included 40 paired samples from symptomatic or recovered (ex) pertussis patients and 20 samples from controls.
The levels of antibodies against Ptx, FHA, Prn, OMVs, LOS, BrkA and Vag8 were significantly higher in plasma of symptomatic patients compared to the controls (Fig. 2A–G). The levels of antibodies against Fim2 and Fim3 did not significantly differ from controls (Fig. 2H and I). For the recovered patients, the levels of the specific antibodies for all tested antigens were significantly lower compared to that of the symptomatic patients. The Ptx-, FHA- and Prn-specific antibody levels for the recovered patients remained significantly higher than the controls (Fig. 2A–C) whereas those of OMV-, LOS-, BrkA-, Vag8-, Fim2- and Fim3-specific antibodies did not (Fig. 2D–I).
Figure 2.
Levels of IgG antibodies directed against nine different pertussis antigens. Antibodies directed against (A) Ptx, (B) FHA, (C) Prn, (D) OMV, (E) LOS, (F) BrkA, (G) Vag8, (H) Fim3 and (I) Fim2 were determined using a 9-valent multiplex immunoassay platform using plasma samples collected from symptomatic (circles) and recovered (squares) pertussis patients as well as from controls (triangles). Statistical testing: one-way analysis of variance (ANOVA) followed by post-hoc tests (Welch Two Sample t-test or paired t-test). The false discovery rate was controlled at the level of 10% by applying the Benjamini-Hochberg method. *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001 ****p ≤ 0.0001 ns = non-significant. Data shown in A–I represent the geometric mean ± geometric SD.
Avidity maturation of B. pertussis-specific antibodies depends on antigen specificity
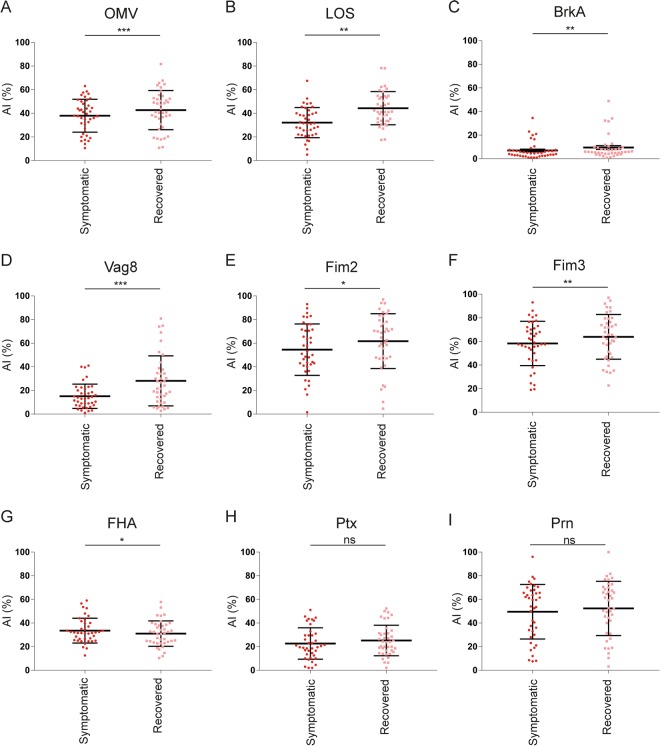
In addition to IgG levels in plasma, we determined the avidity of antigen-specific IgG antibodies in plasma of symptomatic and recovered pertussis patients. The avidity index (AI) of the OMV-, LOS-, BrkA-, Vag8-, Fim2- and Fim3-specific antibodies were significantly higher for the recovered compared to the symptomatic patients (Fig. 3A–F). The significant difference for BrkA-IgG should be interpreted with caution as the AI is low. The AI of FHA-specific antibodies was significantly but modestly decreased for the recovered compared to the symptomatic patients (Fig. 3G). No significant difference in AI of Ptx- and Prn-specific antibodies was observed (Fig. 3H and I).
Figure 3.
Avidity of IgG antibodies directed against nine different pertussis antigens. Avidity Index (AI) of antibodies directed against (A) OMVs, (B) LOS, (C) BrkA, (D) Vag8, (E) Fim2, (F) Fim3, (G) FHA, (H) Ptx and (I) Prn were determined in collected from symptomatic (circles) and recovered (squares) pertussis patients. Statistical testing: paired t-test. The false discovery rate was controlled at the level of 10% by applying the Benjamini-Hochberg method. *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001 ****p ≤ 0.0001 ns = non-significant. Data shown in A–I represent the mean ± SD.
Opsonophagocytosis wanes within years after infection but remains higher compared to controls
Since antibody-mediated opsonophagocytosis is important for the clearance of B. pertussis during infection14, we analysed the functionality of the B. pertussis- specific antibodies using the OPA. Opsonophagocytosis by primary neutrophils was assessed using the clinical B. pertussis isolate B191717, which was modified to express green fluorescent protein (GFP). We observed significantly lower opsonophagocytosis indices in plasma samples from recovered compared to symptomatic patients. Notably, the opsonophagocytosis indices from the recovered patients remained significantly higher than those of the controls (Fig. 4).
Figure 4.
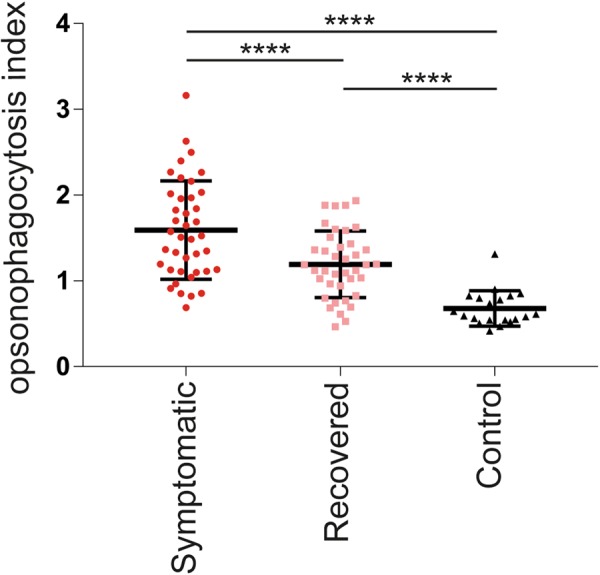
Opsonophagocytosis indices wane years after pertussis infection. Antibody-mediated opsonophagocytosis indices were determined using paired plasma samples collected from symptomatic (circles) and recovered (squares) pertussis patients. Plasma samples from controls (triangles) were also included. Statistical testing: one-way analysis of variance (ANOVA) followed by post-hoc tests (Welch Two Sample t-test or paired t-test). The false discovery rate was controlled at the level of 10% by applying the Benjamini-Hochberg method. ****p ≤ 0.0001. Data shown represent the mean ± SD.
Lower IgG levels, opsonophagocytosis indices and higher avidities of B. pertussis-antibodies are generally observed for recovered compared to symptomatic patients
In order to analyse all the obtained data, a PCA was performed based on the IgG levels and avidity as well as the opsonophagocytosis indices. As shown in Fig. 5, the three groups of the cohort form clusters, with the symptomatic patients positioned furthest away from the controls and the recovered patients being positioned in between. The lines depict the inter-correlations of the various parameters measured in all samples. Firstly, the lines indicate that the axes of differentiation of the majority of the antibody levels had similar alignments and were mainly directed towards the higher scores of the two principal components, mostly populated by the symptomatic group. Secondly, the axes of differentiation of the avidities pointed mainly in the direction of the recovered group. This analysis reflects the findings represented in Figs 2 and 3 which show lower antibody levels and higher AI in the recovered versus symptomatic patients for most of the studied antigens. Likewise, the PCA reflects the findings presented in Fig. 4 where the axes of differentiation of the opsonophagocytosis indices pointed in the direction of the symptomatic group.
Figure 5.
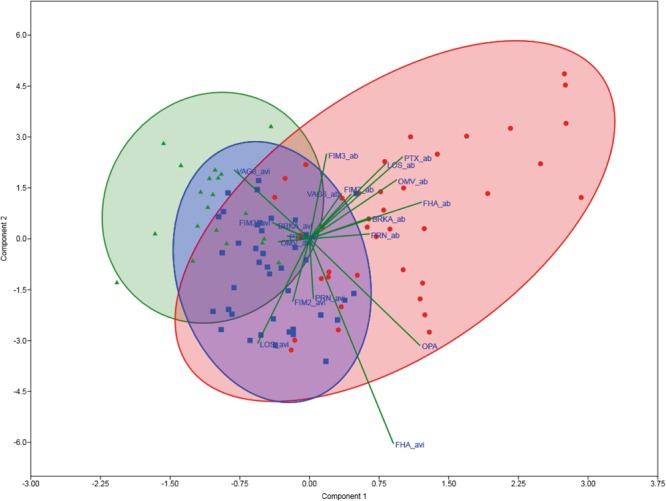
PCA of all obtained data. PCA was performed based on the antibody levels, AI and opsonophagocytosis indices for all plasma samples used in this study. The axes of differentiation of the antibody levels and AI are shown by the lines. Plasma samples collected from symptomatic patients are depicted as red dots, from recovered patients as blue squares and from controls as green triangles. The red, blue and green ellipses indicate clustering of the symptomatic, recovered and control samples, respectively. Lines indicate the axes of differentiation of the different parameters measured in this study.
Random forest analysis reveals predictive value of FHA and Ptx antibodies for opsonophagocytosis indices
A random forest (RF) analysis was performed to determine which of our measured variables, namely effective-IgG levels as well as age and sex, was most predictive for the observed opsonophagocytosis and may serve as potential CoPs. The analysis showed that 28% of the variance of the opsonophagocytosis indices is explained by our model. Results indicate that FHA- followed by Ptx-specific antibodies are most predictive for the accounted variances in the opsonophagocytosis indices (Fig. 6). Multiple linear regression analysis with the same variables considered in the RF analysis revealed significant p-values for FHA and Ptx effective-IgGs supporting their potential predictive role (Table 1).
Figure 6.
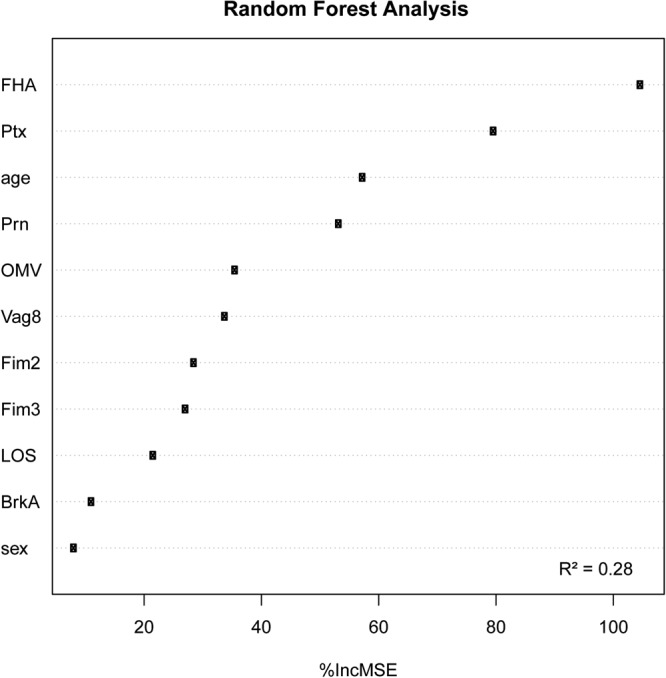
Random Forest analysis integrating all available data. Random Forest analysis was performed using a model that includes the log transformed values of the effective-IgG levels directed against the nine different antigens, as well as the age and sex of the participants. R2 represents the fraction of the total opsonophagocytosis indices variance which can be explained by variations in the effective-IgG levels, where a value of 1 would mean that the variance in the measured opsonophagocytosis indices is solely explained by the considered predictive variables. The percentage of increase in the mean square error (%IncMSE) after randomly permuting the values of the considered predictive variables gives an indication of how influential each considered variable is on predicting OPA values to the extent of the OPA variance which can be explained by the model (R2).
Table 1.
Multi-linear regression analysis with the same parameters considered in the random forest analysis using the effective-IgG levels (IgG levels and avidity).
| (log10 (IgG x Avidity) | Estimate | Std. Error | p-value |
|---|---|---|---|
| Prn | 0.002 | 0.064 | 0.977 |
| FHA | 0.350 | 0.110 | 0.002 |
| Fim2 | −0.183 | 0.079 | 0.023 |
| Fim3 | 0.172 | 0.085 | 0.045 |
| Ptx | 0.225 | 0.092 | 0.017 |
| LOS | −0.055 | 0.168 | 0.743 |
| Vag8 | 0.073 | 0.125 | 0.562 |
| OMV | 0.062 | 0.196 | 0.753 |
| BrkA | 0.117 | 0.088 | 0.187 |
| Age | 0.003 | 0.002 | 0.247 |
| Sex | 0.009 | 0.011 | 0.433 |
Discussion
In the attempt to identify serological CoPs against pertussis, our study pioneers by integrating the dynamics of different antibody properties. These include their specificity to nine different B. pertussis antigens, their avidity and functional capacity to opsonise live B. pertussis. These assays were performed using paired plasma samples from symptomatic and recovered pertussis patients, who are expected to have protective immunity conferred by natural infection. As previously shown, the levels of antibodies to Ptx, FHA, Prn, Fim2, Fim3 and OMVs waned years after infection13. Antibodies against the other studied antigens, BrkA, Vag8 and LOS, also decreased when patients had recovered from clinical disease. BrkA, Vag8 and LOS were included in this study because they are outer membrane antigens and could be anchors for antibody-mediated phagocytosis.
Besides the waning of B. pertussis-specific antibody levels, we also show avidity maturation for the majority of specific antibodies years after B. pertussis infection with the exception of Prn, FHA and Ptx. High avidity antibodies are classically secreted by specific B cells that are positively selected during repeated exposures in germinal centre reactions18. In contrast to our findings, avidity maturation of Ptx antibodies was previously shown in paired samples of pertussis patients19. This difference may be due to the time between collections of the paired samples, which in our case was on average three years instead of four weeks after diagnosis as performed in the before mentioned study. Avidity of antibodies has also been measured following ACV booster vaccination. The authors showed that Ptx and Prn antibody avidity increased one year post-vaccination20. This emphasizes that in the search for CoPs against pertussis it is important to consider the antibody kinetics, not only of the levels but also of the avidity, which may differ following infection or vaccination21.
During an infection with B. pertussis, neutrophils infiltrate the lung where they are important for the clearance of this respiratory pathogen14. Here, we show that three years after infection opsonophagocytosis indices decrease but remain significantly higher compared to the controls. This is the first reported B. pertussis-specific opsonophagocytosis assay using the recently isolated B. pertussis clinical strain B1917 instead of the laboratory strain Tohama I, which has been used in the past. B1917 has the advantage of being a representative strain for the strains that were circulating at the time of our clinical study17. The OPA here described can discriminate between controls, symptomatic and recovered (ex) pertussis patients. Based on these findings, we propose antibody-mediated opsonophagocytosis of B. pertussis as a possible CoP against pertussis. Assays which measure the capacity of antibodies to opsonize pathogens for phagocytosis are currently used in the field of pneumococcal vaccination11. Opsonophagocytosis has also been shown to correlate with protection against malaria22.
Analysis of our data with the RF model using effective-IgGs levels of B. pertussis-specific antibodies uncovered FHA- followed by Ptx-antibodies as being the two variables that best predict the opsonophagocytosis indices. These findings corroborate earlier studies in which the authors also found a correlation between FHA- and to a lesser extend Ptx-specific antibodies and opsonophagocytosis23. In contrast to our findings, others have shown either that high anti-FHA levels inhibit opsonophagocytosis24 or that anti-Prn is important for opsonophagocytosis25. These differences may be explained by the various read-outs (bacterial uptake by flow cytometry, respiratory burst or microscopy) used to determine opsonophagocytosis, as well as the timing of serum or plasma sample collection. Effective-IgG levels to FHA, a vaccine antigen and major adhesion of B. pertussis26, best predicted the variances of the opsonophagocytosis indices. FHA-antibodies are expected to bind to the bacterial membrane and mediate bacterial uptake by engaging Fc-γ receptors on neutrophils27. It remains unknown whether FHA-specific antibodies generated upon infection and vaccination are similar in functionality. Antibodies against the additionally included outer membrane-localised antigens LOS28, Vag8 and BrkA29,30, important immune modulators mediating resistance against antimicrobial peptides (LOS) and complement (LOS, Vag8 and BrkA), were not predictive for the opsonophagocytosis indices according to the RF analysis. It is possible that these antibodies are of an IgG subclass that does not mediate opsonophagocytosis or that the antigen is masked on the bacterial membrane. However, this does not exclude other functional roles for human antibodies against these additional surface antigens. Monoclonal antibodies directed against LOS were found to be important in preventing B. pertussis infection in a mouse model31 and BrkA-specific antibodies have been implicated in bactericidal killing of B. pertussis32. Further studies should address these matters. The second best predictor for opsonophagocytosis was the presence of antibodies directed to Ptx. Because this toxin is generally secreted by B. pertussis and induces high levels of antibodies following infection16,33,34, we speculate that the association found in the RF model is not mechanistically related. Interestingly, FHA- and Ptx-specific antibodies did not show an increased avidity in the recovered pertussis patients suggesting that perhaps high antibody avidity for these antigens is not necessarily important for opsonophagocytosis of B. pertussis. Whether the FHA, and possibly Ptx, antibodies are mechanistically related to neutrophil opsonophagocytosis will have to be verified by either depleting or and/or isolating these antibodies from plasma, as well as by performing the OPA with B. pertussis that do not express FHA or Ptx. To determine whether these antibodies indeed also protect from colonisation with B. pertussis, an in vitro model using differentiated human airway epithelial cells35,36 may be used for validation. Moreover, eventually the novel controlled human infection pertussis model37 could be valuable to determine protection from colonization by specific antibodies.
Although FHA- and Ptx- specific antibodies were the best predictors for opsonophagocytosis in our model, their presence only explained 28% of the opsonophagocytosis indices variances. Adenylate cyclase toxin (ACT) produced by B. pertussis reduces phagocytosis and subsequent bacterial killing by neutrophils14,38. Previously, antibodies directed against this toxin have been shown to promote phagocytosis of B. pertussis via toxin-neutralization39. ACT is not only secreted but also remains associated to the bacterial membrane by interacting with FHA40,41. ACT-specific antibodies could hence also opsonize B. pertussis. Although ACT was not included in the antigen panel of this study, it is likely that part of the unexplained variances can be attributed to ACT-specific antibodies. Also, other specificities cannot be excluded, as the naturally acquired or vaccine-induced B. pertussis serum reactomes are very diverse and broad42. Future studies should explore whether ACT-specific or other B. pertussis-specific antibodies further predict opsonophagocytosis.
This work represents a first step towards identifying CoPs by the combined analysis of different parameters of B. pertussis-specific antibodies from (ex) pertussis patients. These findings should be interpreted with caution as the longitudinal pertussis cohort used is small and includes individuals of different ages with different vaccination status and most likely previous infection backgrounds. Due to the low sample size we were unable to analyse our data by grouping the individuals according to age. Furthermore, our cohort does not include young infants whom are the main victims of severe pertussis. The induction of B. pertussis-specific antibodies and their functional properties may differ between infants and the older individuals in our cohort, possibly due to the presence of maternal antibodies43, which should be taken into account when developing novel childhood pertussis vaccines.
We furthermore suggest exploring antibody characteristics such as subclass and fucosylation status44 which can influence opsonizing capacity or other antibody effector functions. Additionally, protective mechanisms including neutrophil respiratory burst45 and subsequent killing, as well as complement-mediated killing of B. pertussis46–48 could be studied. Recently, levels of specific memory B cells, that can give rise to a fast increase in antibody levels upon an infection with B. pertussis, were implied in protection20,49,50. Moreover, it is clear that not only antibodies or B cells are involved in protection against pertussis, as T helper 1(Th1) and Th17 cells49,51 have also been implicated as very important players in the protective immune response against B. pertussis. Taken together, the pertussis field should broaden the way identification of CoPs is approached and be open to multifactorial CoPs against pertussis, which could be a combination of antibody levels, antibody functionality as well as B. pertussis specific T and B cell responses. With respect to antibodies, integration of different specific antibody parameters may bring the field closer to the identification of the required CoPs against pertussis.
Materials and Methods
Ethics
Participants donating blood for plasma isolation were Dutch symptomatic (ex-) pertussis patients selected from a cross-sectional observational study previously described (Specifieke Kinkhoest Immuniteit; SKI)13. The study was approved by the accredited Medical Research Ethics Committee (MREC) STEG followed by management of the METC UMC Utrecht (Dutch Central Committee on Research Involving Human Subjects (CCMO) nr: NL16334.040.07). Collection of all samples used was conducted according to the principles of the Declaration of Helsinki and all participants, parents/guardians of minor participants and blood donors for primary cell isolation provided written informed consent. Samples were treated anonymously.
Study population
Forty individuals (age 7–73 years, median 49.4 years, at inclusion; male/female ratio: 0.35/0.65) who presented clinical pertussis symptoms and were physician-diagnosed with pertussis, either by PCR or serology, were selected from the SKI cohort, a Dutch natural infection cohort established between 2008 and 201213. Selection was based on whether two longitudinal samples were available namely, early after diagnosis (1.7 to 9.0 weeks, median 3.15 weeks, i.e. symptomatic) when the patients still presented pertussis symptoms and years later (2.7 to 4.7 years, median 3.2 years, i.e. recovered) when the patients had recovered from clinical disease. An additional 20 household contacts from the SKI cohort (age 7.9–48.2 years, median 21.4 years; male/female ratio 0.5/0.5, i.e. controls) who were seronegative (negative anti-Ptx titres) for pertussis and vaccinated according to the Dutch national immunisation program were also selected (Fig. 1).
Plasma collection and neutrophil isolation
Blood samples in the SKI study were collected using vacutainer CPT cell preparation tubes (BD Biosciences, San Jose, CA, USA). Plasma was isolated using standard procedures and stored at −80 °C. Plasma was heat inactivated (HI) for 20 minutes at 56 °C. Human neutrophils were isolated from donor blood as described previously52. Briefly, heparinized venous blood obtained from healthy donors in vacutainer collection tubes (BD Biosciences) was twice diluted in PBS (Gibco) and layered onto a gradient of Ficoll-Paque Premium (GE Healthcare Life Sciences) and Histopaque-1119 (Sigma-Aldrich). After centrifugation for 20 minutes at 400 g, neutrophils were collected from the Histopaque layer and washed with RPMI-1640 (Gibco), supplemented with 0.05% human serum albumin (HSA, Sanquin). Neutrophils were used in the opsonophagocytosis assay shortly after isolation.
Bacteria
B. pertussis B191717 was transformed with plasmid pCW505 resulting in cytoplasmic expression of GFP (B1917-GFP)25. Bacteria were grown on Bordet-Gengou agar plates containing 15% sheep blood (BD Biosciences) supplemented with 30 µg/ml gentamycin (Merck, Darmstadt, Germany) at 35 °C, 5% CO2 for four days. Subsequently, bacteria were recultured in Thalen-IJssel medium53 overnight (start OD 0.05, 35 °C, 130 rpm) until mid-log phase (OD 0.7) was reached before use.
Pertussis antigens
Ptx and FHA were obtained from Kaketsuken (Obuko, Japan). Fim2 was a kind gift from Dr. A Gorringe, Fim3 and Prn were purified in-house. LOS was extracted from strain B1917 by means of hot phenol-water as previously described54. OMVs of B1917, containing various outer membrane antigens, were generated as previously described55 with some modifications and recombinant passenger domains of Vag8 and BrkA were expressed in Escherichia. coli as described elsewhere47.
Multiplex immunoassay
Levels of total IgG directed against B. pertussis antigens Ptx, FHA, Prn, Fim2, Fim3, Vag8, BrkA, LOS and OMV were measured in HI-plasma samples by an in-house multiplex immunoassay (MIA) described earlier13. The International WHO pertussis standard (NIBSC 06/140) served as reference for IgG levels against Ptx, FHA and Prn (International units, IU/ml). Human Normal Immunoglobulin solution for infusion (KIOVIG, Baxalta, Belgium) was used as an in-house reference to measure levels of IgG against the remaining six antigens, expressed as arbitrary units per ml (AU/ml) based on observed relative magnitudes of fluorescence intensity where KIOVIG was set at 500 AU/ml. For detection, goat-anti-human IgG-PE (Jackson ImmunoResearch, USA) was used. Analysis was performed with a Bio-Plex 200 using Bio-Plex Manager software version 5.5 (Bio-Rad Laboratories, West Grove, PA, USA). The various antigen coupled bead regions were not found to interfere with one another.
Avidity assay
The avidity of pertussis-specific IgG antibodies was measured in the MIA using HI-plasma as described previously56 with modifications. Briefly, plasma samples were allowed to bind for 45 minutes with the respective pertussis antigen coupled to fluorescently labelled microspheres. After washing, samples were incubated for 15 minutes in PBS either in the absence or presence of 9 M urea, to elute lower-avidity antibodies. Subsequently, samples were washed, goat-anti-human IgG-PE (Jackson ImmunoResearch, USA) was used as detection antibody and analysis was performed with a Bio-Plex 200 using Bio-Plex Manager software version 5.5 (Bio-Rad) The avidity index (AI) was expressed as a percentage of the remaining IgG levels in the presence of urea relative to the IgG levels measured in PBS only.
Opsonophagocytosis assay
Opsonophagocytosis of B. pertussis B1917 by human neutrophils was evaluated using a method described in literature with minor modifications27,57. Briefly, B1917-GFP (multiplicity of infection is 70) were opsonized with 5% HI-plasma in RPMI supplemented with 0.3% human serum albumin (HSA, Sanquin) for 20 minutes at 37 °C. Subsequently, freshly isolated neutrophils (7.5 × 104 cells) were added in a total volume of 50 µl and incubated for 25 minutes at 4 °C. After a wash step with cold RPMI-HSA, neutrophils were resuspended in RPMI-HSA and incubated for 30 minutes at 37 °C. The incubation times used were selected based on OPA pilot experiments. Cells were fixed with 1.5% paraformaldehyde and visualized using the FACSCanto II (BD Bioscience). The assay was performed in duplicate on three different days. To correct for plate and day differences, a standalone-control plasma sample was taken along on each plate for each day and a plate factor was calculated. The arbitrary opsonophagocytosis indices were calculated by dividing the mean fluorescent intensity (MFI) obtained in the presence of plasma by the MFI obtained upon incubating cells with bacteria without plasma, corrected for the plate factor.
Data analysis
Differences in antibody levels and opsonophagocytosis indices between the groups were tested with one-way analysis of variance (ANOVA) followed by post-hoc tests (Welch Two Sample t-test or paired t-test). For differences in the AI a paired t-test was performed. P values ≤ 0.05 were considered statistically significant. The false discovery rate was controlled at the level of 10% by applying the Benjamini-Hochberg method to the results of all tests (Supplementary Table 2).
Principal component analysis (PCA) was used to explore dis(similarities) among the antibody levels, AI and opsonophagocytosis indices of the three groups.
To determine which of the measured antibodies were most predictive for the observed opsonophagocytosis, a random forest (RF) analysis was performed58. The model considered in this analysis uses for each antigen the effective-IgG level, which we define as the logarithm of the product of IgG levels and AI (IgG*AI). A multiple linear regression analysis using the same effective-IgG levels was also performed. Descriptive statistics of the data can be found in Supplementary Table 1.
Electronic supplementary material
Acknowledgements
We are grateful to participants and employees from the SKI-study, especially study nurse Lidian Izeboud for the inclusion of the paired samples. We would like to thank Mr. A Hachhouch (RIVM) for his technical support, Ms. J. Westdijk (RIVM) for the purification of Fim3, Dr. A. Gorringe (Public Health England, UK) for kindly providing Fim2 and Dr. E. Pupo Escalona (Intravacc, the Netherlands) for providing the LOS preparation. This work was supported by the Strategic Program from the National institute for Public Health and the Environment, the Netherlands (RIVM-S/112001 grant to EP) and V/150407 grant to EP and CACMVE. IJ was partially supported by the research program VENI which is financed by the Netherlands Organization for Scientific Research (NWO) (016.156.051).
Author Contributions
E.S.H., B.K., H.J.H. and D.H. performed the experiments. A.A.B.M. and L.M.G. performed the statistical testing I.V.T., C.A.C.M.V.E. and E.P. were involved in the study design. E.H., A.A.B.M. and L.M.G. drafted the figures. E.H., I.J., C.A.C.M.V.E. and E.P. wrote the manuscript. All authors reviewed the manuscript.
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Cecile A. C. M. van Els and Elena Pinelli contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-30558-8.
References
- 1.Tan, T. et al. Pertussis Across the Globe: Recent Epidemiologic Trends From 2000–2013. Pediatr Infect Dis J, 10.1097/INF.0000000000000795 (2015). [DOI] [PubMed]
- 2.Celentano LP, et al. Resurgence of pertussis in Europe. Pediatr Infect Dis J. 2005;24:761–765. doi: 10.1097/01.inf.0000177282.53500.77. [DOI] [PubMed] [Google Scholar]
- 3.Wendelboe AM, Van Rie A, Salmaso S, Englund JA. Duration of immunity against pertussis after natural infection or vaccination. Pediatr Infect Dis J. 2005;24:S58–61. doi: 10.1097/01.inf.0000160914.59160.41. [DOI] [PubMed] [Google Scholar]
- 4.Klein NP, Bartlett J, Rowhani-Rahbar A, Fireman B, Baxter R. Waning protection after fifth dose of acellular pertussis vaccine in children. N Engl J Med. 2012;367:1012–1019. doi: 10.1056/NEJMoa1200850. [DOI] [PubMed] [Google Scholar]
- 5.Sheridan SL, Ware RS, Grimwood K, Lambert SB. Number and order of whole cell pertussis vaccines in infancy and disease protection. JAMA. 2012;308:454–456. doi: 10.1001/jama.2012.6364. [DOI] [PubMed] [Google Scholar]
- 6.Plotkin SA, Gilbert PB. Nomenclature for immune correlates of protection after vaccination. Clin Infect Dis. 2012;54:1615–1617. doi: 10.1093/cid/cis238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taranger J, et al. Correlation between pertussis toxin IgG antibodies in postvaccination sera and subsequent protection against pertussis. J Infect Dis. 2000;181:1010–1013. doi: 10.1086/315318. [DOI] [PubMed] [Google Scholar]
- 8.Cherry JD, Gornbein J, Heininger U, Stehr K. A search for serologic correlates of immunity to Bordetella pertussis cough illnesses. Vaccine. 1998;16:1901–1906. doi: 10.1016/S0264-410X(98)00226-6. [DOI] [PubMed] [Google Scholar]
- 9.Storsaeter J, Hallander HO, Gustafsson L, Olin P. Levels of anti-pertussis antibodies related to protection after household exposure to Bordetella pertussis. Vaccine. 1998;16:1907–1916. doi: 10.1016/S0264-410X(98)00227-8. [DOI] [PubMed] [Google Scholar]
- 10.Mills KH. Immunity to Bordetella pertussis. Microbes Infect. 2001;3:655–677. doi: 10.1016/S1286-4579(01)01421-6. [DOI] [PubMed] [Google Scholar]
- 11.Plotkin SA. Correlates of protection induced by vaccination. Clin Vaccine Immunol. 2010;17:1055–1065. doi: 10.1128/CVI.00131-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forthal DN. Functions of Antibodies. Microbiol Spectr. 2014;2:AID-0019–2014. doi: 10.1128/microbiolspec.AID-0019-2014. [DOI] [PubMed] [Google Scholar]
- 13.van Twillert I, et al. Impact of age and vaccination history on long-term serological responses after symptomatic B. pertussis infection, a high dimensional data analysis. Sci Rep. 2017;7:40328. doi: 10.1038/srep40328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eby JC, Hoffman CL, Gonyar LA, Hewlett EL. Review of the neutrophil response to Bordetella pertussis infection. Pathog Dis. 2015;73:ftv081. doi: 10.1093/femspd/ftv081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Romero-Steiner S, et al. Reduction in functional antibody activity against Streptococcus pneumoniae in vaccinated elderly individuals highly correlates with decreased IgG antibody avidity. Clin Infect Dis. 1999;29:281–288. doi: 10.1086/520200. [DOI] [PubMed] [Google Scholar]
- 16.Heininger U, Cherry JD, Stehr K. Serologic response and antibody-titer decay in adults with pertussis. Clin Infect Dis. 2004;38:591–594. doi: 10.1086/381439. [DOI] [PubMed] [Google Scholar]
- 17.Bart, M. J. et al. Complete Genome Sequences of Bordetella pertussis Isolates B1917 and B1920, Representing Two Predominant Global Lineages. Genome Announc2, 10.1128/genomeA.01301-14 (2014). [DOI] [PMC free article] [PubMed]
- 18.Dorner T, Radbruch A. Antibodies and B cell memory in viral immunity. Immunity. 2007;27:384–392. doi: 10.1016/j.immuni.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Barkoff AM, et al. Differences in avidity of IgG antibodies to pertussis toxin after acellular pertussis booster vaccination and natural infection. Vaccine. 2012;30:6897–6902. doi: 10.1016/j.vaccine.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Hendrikx LH, et al. Enhanced memory B-cell immune responses after a second acellular pertussis booster vaccination in children 9 years of age. Vaccine. 2011;30:51–58. doi: 10.1016/j.vaccine.2011.10.048. [DOI] [PubMed] [Google Scholar]
- 21.Dalby T, Petersen JW, Harboe ZB, Krogfelt KA. Antibody responses to pertussis toxin display different kinetics after clinical Bordetella pertussis infection than after vaccination with an acellular pertussis vaccine. J Med Microbiol. 2010;59:1029–1036. doi: 10.1099/jmm.0.020826-0. [DOI] [PubMed] [Google Scholar]
- 22.Osier FH, et al. Opsonic phagocytosis of Plasmodium falciparum merozoites: mechanism in human immunity and a correlate of protection against malaria. BMC Med. 2014;12:108. doi: 10.1186/1741-7015-12-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aase A, et al. Opsonophagocytic activity and other serological indications of Bordetella pertussis infection in military recruits in Norway. Clin Vaccine Immunol. 2007;14:855–862. doi: 10.1128/CVI.00081-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mobberley-Schuman PS, Connelly B, Weiss AA. Phagocytosis of Bordetella pertussis incubated with convalescent serum. J Infect Dis. 2003;187:1646–1653. doi: 10.1086/374741. [DOI] [PubMed] [Google Scholar]
- 25.Hellwig SM, Rodriguez ME, Berbers GA, van de Winkel JG, Mooi FR. Crucial role of antibodies to pertactin in Bordetella pertussis immunity. J Infect Dis. 2003;188:738–742. doi: 10.1086/377283. [DOI] [PubMed] [Google Scholar]
- 26.Coutte L, et al. Role of adhesin release for mucosal colonization by a bacterial pathogen. J Exp Med. 2003;197:735–742. doi: 10.1084/jem.20021153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rodriguez ME, et al. Fc receptor-mediated immunity against Bordetella pertussis. J Immunol. 2001;167:6545–6551. doi: 10.4049/jimmunol.167.11.6545. [DOI] [PubMed] [Google Scholar]
- 28.Harvill ET, et al. Multiple Roles for Bordetella Lipopolysaccharide Molecules during Respiratory Tract Infection. Infection and Immunity. 2000;68:6720–6728. doi: 10.1128/IAI.68.12.6720-6728.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marr N, Shah NR, Lee R, Kim EJ, Fernandez RC. Bordetella pertussis Autotransporter Vag8 Binds Human C1 Esterase Inhibitor and Confers Serum Resistance. PLoS One. 2011;6:e20585. doi: 10.1371/journal.pone.0020585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barnes MG, Weiss AA. BrkA Protein of Bordetella pertussis Inhibits the Classical Pathway of Complement after C1 Deposition. Infection and Immunity. 2001;69:3067–3072. doi: 10.1128/IAI.69.5.3067-3072.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shahin RD, Hamel J, Leef MF, Brodeur BR. Analysis of protective and nonprotective monoclonal antibodies specific for Bordetella pertussis lipooligosaccharide. Infect Immun. 1994;62:722–725. doi: 10.1128/iai.62.2.722-725.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oliver DC, Fernandez RC. Antibodies to BrkA augment killing of Bordetella pertussis. Vaccine. 2001;20:235–241. doi: 10.1016/S0264-410X(01)00269-9. [DOI] [PubMed] [Google Scholar]
- 33.Locht C, Coutte L, Mielcarek N. The ins and outs of pertussis toxin. FEBS J. 2011;278:4668–4682. doi: 10.1111/j.1742-4658.2011.08237.x. [DOI] [PubMed] [Google Scholar]
- 34.van Twillert I, et al. The Use of Innovative Two-Component Cluster Analysis and Serodiagnostic Cut-Off Methods to Estimate Prevalence of Pertussis Reinfections. PLoS One. 2016;11:e0148507. doi: 10.1371/journal.pone.0148507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guevara C, et al. Highly differentiated human airway epithelial cells: a model to study host cell-parasite interactions in pertussis. Infect Dis (Lond) 2016;48:177–188. doi: 10.3109/23744235.2015.1100323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krunkosky TM, Jordan JL, Chambers E, Krause DC. Mycoplasma pneumoniae host-pathogen studies in an air-liquid culture of differentiated human airway epithelial cells. Microb Pathog. 2007;42:98–103. doi: 10.1016/j.micpath.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 37.de Graaf H, et al. Investigating Bordetella pertussis colonisation and immunity: protocol for an inpatient controlled human infection model. BMJ Open. 2017;7:e018594. doi: 10.1136/bmjopen-2017-018594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kamanova J, et al. Adenylate cyclase toxin subverts phagocyte function by RhoA inhibition and unproductive ruffling. J Immunol. 2008;181:5587–5597. doi: 10.4049/jimmunol.181.8.5587. [DOI] [PubMed] [Google Scholar]
- 39.Weingart CL, Mobberley-Schuman PS, Hewlett EL, Gray MC, Weiss AA. Neutralizing antibodies to adenylate cyclase toxin promote phagocytosis of Bordetella pertussis by human neutrophils. Infect Immun. 2000;68:7152–7155. doi: 10.1128/IAI.68.12.7152-7155.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carbonetti NH. Pertussis toxin and adenylate cyclase toxin: key virulence factors of Bordetella pertussis and cell biology tools. Future Microbiol. 2010;5:455–469. doi: 10.2217/fmb.09.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hewlett EL, Urban MA, Manclark CR, Wolff J. Extracytoplasmic adenylate cyclase of Bordetella pertussis. Proc Natl Acad Sci USA. 1976;73:1926–1930. doi: 10.1073/pnas.73.6.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Valentini D, Ferrara G, Advani R, Hallander HO, Maeurer MJ. Serum reactome induced by Bordetella pertussis infection and Pertussis vaccines: qualitative differences in serum antibody recognition patterns revealed by peptide microarray analysis. BMC Immunol. 2015;16:40. doi: 10.1186/s12865-015-0090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Niewiesk S. Maternal antibodies: clinical significance, mechanism of interference with immune responses, and possible vaccination strategies. Front Immunol. 2014;5:446. doi: 10.3389/fimmu.2014.00446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vidarsson G, Dekkers G, Rispens T. IgG subclasses and allotypes: from structure to effector functions. Front Immunol. 2014;5:520. doi: 10.3389/fimmu.2014.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Steed LL, Akporiaye ET, Friedman RL. Bordetella pertussis induces respiratory burst activity in human polymorphonuclear leukocytes. Infect Immun. 1992;60:2101–2105. doi: 10.1128/iai.60.5.2101-2105.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brookes C, et al. Bordetella pertussis isolates vary in their interactions with human complement components. Emerg Microbes Infect. 2018;7:81. doi: 10.1038/s41426-018-0084-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hovingh ES, et al. Acquisition of C1 inhibitor by Bordetella pertussis virulence associated gene 8 results in C2 and C4 consumption away from the bacterial surface. PLoS Pathog. 2017;13:e1006531. doi: 10.1371/journal.ppat.1006531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Barnes MG, Weiss AA. Activation of the complement cascade by Bordetella pertussis. FEMS Microbiol Lett. 2003;220:271–275. doi: 10.1016/S0378-1097(03)00132-0. [DOI] [PubMed] [Google Scholar]
- 49.van Twillert I, et al. Age related differences in dynamics of specific memory B cell populations after clinical pertussis infection. PLoS One. 2014;9:e85227. doi: 10.1371/journal.pone.0085227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marcellini V, et al. Protection against Pertussis in Humans Correlates to Elevated Serum Antibodies and Memory B Cells. Front Immunol. 2017;8:1158. doi: 10.3389/fimmu.2017.01158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Higgs R, Higgins SC, Ross PJ, Mills KHG. Immunity to the respiratory pathogen Bordetella pertussis. Mucosal Immunology. 2012;5:485–500. doi: 10.1038/mi.2012.54. [DOI] [PubMed] [Google Scholar]
- 52.Bestebroer J, et al. Staphylococcal superantigen-like 5 binds PSGL-1 and inhibits P-selectin-mediated neutrophil rolling. Blood. 2007;109:2936–2943. doi: 10.1182/blood-2006-06-015461. [DOI] [PubMed] [Google Scholar]
- 53.Thalen M, et al. Rational medium design for Bordetella pertussis: basic metabolism. J Biotechnol. 1999;75:147–159. doi: 10.1016/S0168-1656(99)00155-8. [DOI] [PubMed] [Google Scholar]
- 54.Westphal OaJ. K.. Bacterial Lipopolysaccharides Extraction with Phenol-Water and Further Applications of the Procedure. Methods in Carbohydrate Chemistry. 1965;5:83–91. [Google Scholar]
- 55.Saunders NB, et al. Immunogenicity of intranasally administered meningococcal native outer membrane vesicles in mice. Infect Immun. 1999;67:113–119. doi: 10.1128/iai.67.1.113-119.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stenger RM, et al. Fast, antigen-saving multiplex immunoassay to determine levels and avidity of mouse serum antibodies to pertussis, diphtheria, and tetanus antigens. Clin Vaccine Immunol. 2011;18:595–603. doi: 10.1128/CVI.00061-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rodriguez ME, Van der Pol WL, Van de Winkel JG. Flow cytometry-based phagocytosis assay for sensitive detection of opsonic activity of pneumococcal capsular polysaccharide antibodies in human sera. J Immunol Methods. 2001;252:33–44. doi: 10.1016/S0022-1759(01)00329-5. [DOI] [PubMed] [Google Scholar]
- 58.Breiman L. Random Forests. Machine Learning. 2001;45:5–32. doi: 10.1023/A:1010933404324. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.