Abstract
Purpose
The aims of this study on late-detected developmental dislocation of the hip (DDH) were to assess the outcome in patients aged 55 to 60 years and to define prognostic factors.
Methods
The study included 60 patients (74 hips). Primary treatment was skin traction to obtain closed reduction, followed by hip spica plaster cast. There were 52 girls and eight boys with a mean age at reduction of 19.6 months (8 to 37). Criteria for good long-term outcome were no osteoarthritis (OA) or total hip arthroplasty (THA) and modified Harris Hip Score ≥ 80 points.
Results
The mean patient age at follow-up was 57.7 years (55 to 60). Good long-term clinical and radiographic outcome occurred in 39 of 73 hips (53%). In all, 24 hips (32%) had undergone THA at a mean patient age of 48.1 years (31 to 58). Survival analysis with conversion to THA as endpoint showed a reduction in survival from 100% at patient age 30 years to 62% at 58 years. Risk factors for poor outcome were age at reduction ≥ 1.5 years and residual dysplasia (Severin grades III/IV) at skeletal maturity.
Conclusion
With a mean follow-up of patient age 58 years, the outcome of late-detected DDH, treated with traction and closed reduction, was satisfactory in more than half the hips. This indicates that the hip will probably last more than 50 years if risk factors like age at reduction ≥ 1.5 years, residual dysplasia and avascular necrosis are avoided.
Keywords: late-detected developmental dislocation of the hip, closed reduction, long-term outcome, risk factors
Introduction
There is no consensus regarding the optimal treatment of late-detected developmental dislocation of the hip (DDH). Closed reduction with preliminary traction was common in the past,1,2 whereas open reduction has become more frequently used during recent decades.3–5 Successful outcome means that the hip should last a lifetime, with avoidance of osteoarthritis (OA) and total hip arthroplasty (THA). The outcome deteriorates with increasing length of follow-up. OA after late-detected DDH was markedly more frequent in patients > 40 years than in younger patients.6 Therefore, studies with a follow-up ≥ 50 years are desirable to compare different treatment strategies.
Some decades ago, late-detected DDH was usually managed with a period of skin traction to obtain closed reduction. The 50-year follow-up of this treatment was recently published.7 With continued follow-up, the present study reports the outcome at a mean patient age of almost 58 years. The aims of the study were to answer the following questions:
What is the long-term outcome at patient age 55 to 60 years of closed reduction of late-detected DDH in children aged six to 36 months at the time of diagnosis?
Which factors are associated with satisfactory and unsatisfactory outcome?
Patients and methods
Patients for this retrospective study were treated with closed reduction for late-detected DDH during the period 1958 to 1962. The inclusion criteria were: no associated anomaly, no neuromuscular disorder, no previous treatment in other hospitals and age at diagnosis six to 36 months. Patients with acetabular dysplasia only or slight subluxation were not included. With these criteria, 60 patients (74 hips) were included. They were 52 girls (87%) and eight boys. Their mean age at the time of diagnosis was 17.4 months (six to 34). DDH was unilateral in 46 patients and bilateral in 14. The left side was affected more often than the right side (43 versus 31). In all, 61 hips (82%) had total dislocation and 13 had subluxation with femoral head coverage < 50%. The study was approved by the Regional Committee of Medical Research Ethics and the hospital’s Privacy and Data Protection Officer, and informed consent was received from the patients.
The patients were initially treated with skin traction to obtain gradual reduction. Bilateral longitudinal traction with slight flexion and abduction of the hips was applied. The degree of abduction and traction force was gradually increased. After about one week, moderate internal rotation was added through the use of additional adhesive straps around the thighs and a cross pull. An anteroposterior radiograph was obtained every other week. Reduction was considered satisfactory when the centre of the femoral head had been pulled down to a position opposite the triradiate cartilage. With the patient under general anaesthesia, a bilateral hip spica cast was applied, immobilizing hips, knees and feet and maintaining the position obtained by traction; no formal ‘reduction manoeuvre’ was performed. The position of the hips was slight flexion, 40° to 60° of abduction and moderate internal rotation. The average time in traction was 33 days (16 to 65). The mean age at spica cast application was 19.6 months (8 to 37). In all 28 hips were reduced at a patient age of less than 18 months, whereas 46 were 18 months or older. Hip spica was used for a mean period of 9.2 months (6 to 15). The spica was changed every three months.
Because of residual acetabular dysplasia with subluxation (14 hips) or without subluxation (11 hips), late surgical intervention was performed in 22 patients (25 hips) at a mean patient age of 11.4 years (5 to 19). Proximal femoral osteotomy with varus and derotation was performed in 11 hips, acetabular shelf operation with a modification of the Spitzy technique in 12 hips and pelvic osteotomy with Salter’s technique in two hips. Postoperative complications included postoperative wound infection after two shelf operations. In one of these, deep infection developed with resulting OA and a poor outcome. In the other hip, the infection healed after antibiotics and the outcome was good.
Radiographic evaluation
Conventional anteroposterior radiographs of the pelvis were taken with the patient in the supine position. Care was taken to position the patient with the legs parallel and to avoid rotation of the pelvis and hips. The film-focus distance was 115 cm. The radiographic assessment was performed by the author, who has extensive experience in evaluation of radiographs of hips in children and adults. The migration percentage (MP) was measured according to Reimers.8 If MP is < 33% the hip is located. When MP is 33% to 89% the hip is subluxated and MP ≥ 90% means total dislocation.The centre-edge (CE) angle was measured as described by Wiberg.9 Avascular necrosis of the femoral head (AVN) was assessed according to Kalamchi and MacEwen.10 The radiographic outcome at skeletal maturity was evaluated using a modification of the classification of Severin.11 Severin grade I means a normal hip with CE angle ≥ 20º. Severin grade II means minor changes in the proximal femur or acetabulum and has the same limit for CE angle as grade I. Severin grade III is acetabular dysplasia with CE angle < 20º. Severin grade IV is subluxation, which for the present study was defined as CE angle < 10º and MP ≥ 33%. The Severin classification was simplified into two grades: satisfactory outcome when the Severin grade was I or II and unsatisfactory outcome when the Severin grade was III or IV.
Long-term follow-up
In patients that had not undergone THA, clinical long-term follow-up was performed by Harris Hip Score (HHS).12 The patients were interviewed by telephone, using the modified HHS score (mHHS).13 Omitting deformity and range of movement (9 points), pain (44 points) and function (47 points) are assessed with mHHS, which has a total maximum score of 91 points. However, a multiplier of 1.1 was used for mHHS and provided a total possible score of 100.13 There is no clinically meaningful difference in outcome between HHS and mHHS.14 A good clinical outcome was defined as no THA and mHHS score of 80 to 100 points.
The radiographic outcome was classified as good in hips that had not undergone THA and had no OA. Information about THA was provided by The Norwegian Arthroplasty Register, which started registration of THAs in Norway in 1988. The data were received in November 2017 and included whether or not the patients had undergone THA and the date at the time of THA. Radiographic follow-up was not specifically performed for this study. If the most recent radiographs (usually obtained in 2012, at a mean patient age of 51 years) had shown OA, the radiographic outcome was classified as poor although no THA had been inserted. In patients with mHHS < 80 points, new radiographs during the last few years had usually been taken. The AO classification of Jacobsen and Sonne-Holm15 was used, in which minimum joint space width of < 2.0 mm in the upper, weight-bearing part of the joint is the criterion for OA.
Statistical analysis
SPSS (version 23) was used for the statistics (IBM, Armonk, New York). Categorical data were analyzed with the Pearson chi-squared test. Continuous variables were analyzed using the t-test for independent samples. All tests were two-sided. Differences were considered significant when the p-value was < 0.05. Kaplan-Meier survival analysis with conversion to THA as an endpoint was used to assess the long-term prognosis. For evaluation of prognostic factors for overall outcome, relevant variables were run in univariable models, only estimating the effect of the single variable one at a time. Variables with a p-value < 0.05 were analyzed with multiple logistic regression.
Results
In all, 21 patients (24 hips, representing 32%) had undergone THA (Fig. 1) at a mean patient age of 48.1 years (31 to 58). Poor radiographic long-term results with development of OA occurred in 32 hips (43%). Thus, eight hips with OA had not undergone THA. The mean mHHS score in these hips was 60 points (32 to 97). The patients preferred to await THA surgery for the following reasons: no or tolerable discomfort (five hips), fear of surgery (two hips) and other serious medical conditions (one hip). In order to compare the present study with previous studies of patients older than 1.5 years at the time of hip reduction, radiographic outcome was analyzed separately for patients who were ≥ 1.5 years at reduction (mean age 24 months). Poor radiographic outcome occurred in 26 hips (58%), of which THA had been inserted in 19 hips (41%).
Fig. 1.
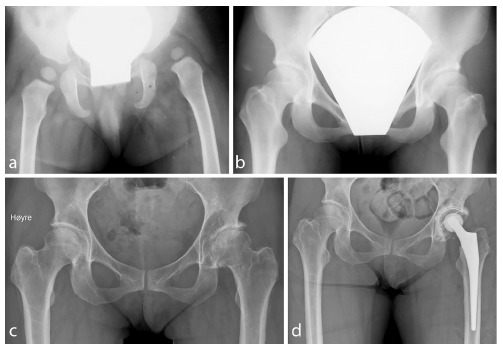
(a) The initial radiograph of a 14-month-old girl with dislocation of her left hip; (b) radiograph at the age of 19 years, showing normal hips with centre-edge angle of the left hip 21°; (c) radiograph at age 50 years, showing osteoarthritis of the left hip, total hip arthroplasty (THA) was inserted three months later; (d) radiograph three days after THA of the left hip.
The long-term clinical outcome was available in all the patients except one who did not respond to the telephone calls. The mean age of patients who had not undergone THA was 57.7 years (55 to 60). The mean mHHS of the 49 hips that had not undergone THA was 90 points (32 to 100). The clinical outcome was good in 41 of 73 hips (56%), with a mean HHS of 97 points (81 to 100). Clinical outcome was poor in the remaining 32 hips (44%), of which 24 hips had undergone THA and eight hips had mHHS < 80 points. The mean mHHS in these eight hips was 52 points (32 to 74). A separate analysis of patients ≥ 1.5 years at the time of reduction showed that 25 out of 45 hips (56%) had a poor clinical result.
Combined clinical and radiographic outcome was good (no OA, no THA, mHHS ≥ 80 points) in 39 hips (53%) (Fig. 2) and poor in 34 hips (47%). Separate analysis of patients ≥ 1.5 years at reduction showed that 27 of 45 hips (60%) had poor outcome. Potential predictive factors for satisfactory and unsatisfactory long-term outcome are presented in Table 1. Univariable analysis showed that significant risk factors for poor outcome (p < 0.05) were age at reduction ≥ 1.5 years and residual dysplasia (Severin grade III/IV) at skeletal maturity. These variables were also statistically significant in multivariable logistic regression.
Fig. 2.

(a) The initial radiograph at age 17 months of a girl with dislocation of her left hip; (b) radiograph at the age of 16 years shows normal hips; (c) radiograph at the age of 52 years shows no osteoarthritis. At the last clinical follow-up at 57 years she had no complaints and modified Harris Hip Score was 100 points.
Table 1.
Overall long-term outcome (combined clinical and radiographic outcome) in 73 hips at a mean patient age of 58 years. Results are given as number of hips
| Parameters | Long-term outcome | |||
|---|---|---|---|---|
| Satisfactory | Unsatisfactory | Univariable p-value | Multivariable p-value | |
| Age < 1.5 yrs | 21 | 7 | 0.004 | 0.049 |
| Age ≥ 1.5 yrs | 18 | 27 | ||
| Dislocation | 29 | 31 | 0.061 | |
| Subluxation | 10 | 3 | ||
| Unilateral DDH | 25 | 20 | 0.644 | |
| Bilateral DDH | 14 | 14 | ||
| Side: Right | 13 | 17 | 0.149 | |
| Side: Left | 26 | 17 | ||
| Avascular necrosis | 1 | 5 | 0.060 | |
| No avascular necrosis | 38 | 29 | ||
| Severin grade I/II at SM | 26 | 14 | 0.002 | 0.019 |
| Severin grade III/IV at SM | 7 | 14 | ||
Statistical analysis: univariable: Pearson’s chi-squared test; multivariable: logistic regression
DDH, developmental dislocation of the hip; SM, skeletal maturity
Survival analyses with conversion to THA as an endpoint for all hips and according to age groups is presented in Table 2 and Fig. 3. Survival was 100% at patient age 30 years and fell slightly up to 40 years, when survival was 95%. Thereafter, survival decreased gradually, ending with a rate of 62% at patient age 58 years. A separate analysis in patients aged 1.5 years or more at reduction showed similar survival rates as the total material until age 40 years; thereafter 8% lower survival rates were found in older patients.
Table 2.
Kaplan-Meier survival analysis of hips with late-detected developmental dislocation of the hip with conversion to total hip arthroplasty as endpoint, in all 74 hips and according to patient age at hip reduction < 1.5 years and ≥ 1.5 years
| Patient age (yrs) | Survival | |||||
|---|---|---|---|---|---|---|
| Total material | Age < 1.5 yrs | Age ≥ 1.5 yrs | ||||
| % | 95% CI | % | 95% CI | % | 95% CI | |
| 30 | 100 | 100 | 100 | |||
| 35 | 96 | 91 to 100 | 100 | 94 | 87 to 100 | |
| 40 | 95 | 90 to 100 | 100 | 91 | 83 to 99 | |
| 45 | 88 | 80 to 96 | 100 | 80 | 68 to 92 | |
| 50 | 84 | 75 to 93 | 96 | 89 – 100 | 76 | 63 to 89 |
| 55 | 73 | 63 to 83 | 89 | 83 – 95 | 65 | 51 to 79 |
| 58 | 62 | 47 to 77 | 78 | 59 – 97 | 54 | 36 to 72 |
Age: patient age at reduction
CI, confidence interval
Fig. 3.

Kaplan-Meier survival analysis of all 74 hips and 46 hips in patients ≥ 1.5 years at the time of reduction, with total hip arthroplasty as the endpoint (bars are 95% confidence intervals).
There was a strong association between long-term clinical and radiographic outcomes. No patient with a HHS of 100 points had OA. There was agreement between clinical and radiographic results in 69 out of 73 hips (95%) and disagreement in four hips. The latter were two patients with OA but high mHHS (81 and 97 points) and two patients with poor mHHS (48 and 74 points) but no OA.
Discussion
This study represents the longest follow-up to date of late-detected DDH. After a mean follow-up to patient age 58 years, the combined clinical and radiographic outcome was satisfactory (mHHS ≥ 80 points and no OA) in 53% of the hips. The main risk factors for poor outcome were age at reduction ≥ 1.5 years and residual hip dysplasia/subluxation.
Long-term outcome deteriorates with duration of follow-up.1 The previous study with the longest duration of follow-up appears to be that of Thomas et al.6 They studied patients who were > 1.5 years of age at the time of hip reduction and had been treated with open reduction and Salter pelvic osteotomy. The OA rate at the latest follow-up (mean patient age 46 years) was 48% of the hips. A separate analysis of our patients who were ≥ 1.5 years at the time of reduction indicated similar results, with an OA rate of 58% with 12 years longer follow-up.
Survival analysis with conversion to THA as the endpoint, requires very long follow-up to be reliable. Only the study of Thomas et al6 has sufficiently long follow-up. They reported survival rates of 99%, 86% and 54%, respectively, at follow-up of 30, 40 and 45 years. Our corresponding rates in patients ≥ 1.5 years at reduction were 100%, 91% and 80%. The survival rates at 30 and 40 years were similar, but Thomas et al6 had a marked reduction in survival after age 40 years, which was not confirmed in the present study. There seems to be no plausible explanation for this discrepancy in patterns of long-term survival.
After a mean follow-up of 30 years, Malvitz and Weinstein1 found a fairly strong association between functional and radiographic results, which is in accordance with our experience. The most important categories of the HHS are pain (44 points) and function (47 points). Since there is no clinically meaningful difference in outcome between HHS and mHHS,14 mHHS without the categories ‘range of motion’ and ‘absence of deformity’ is sufficient. Thus, reliable long-term results can be obtained in patients who do not want to attend a radiographic follow-up. The clinical long-term outcome in hips that had not undergone THA, with a mean HHS of 90 points, was in keeping with previous studies with shorter follow-up, where the mean hip score of ‘surviving’ hips was 88 to 94 points.6,16,17
Among the most important risk factors for poor long-term outcome was age at reduction, which confirms the experience of previous studies.1,18,19 Thomas et al6 did not find age a significant risk factor and assumed this could be due to a statistical type II effect. Another reason could be that they studied rather older patients (≥ 1.5 years at hip reduction). Malvitz and Weinstein1 included patients aged from a few months to eight years and found that the younger the patient the better the long-term outcome, but emphasized that the ‘critical age’ was controversial. In our study of patients between 0.5 and three years, the critical age seemed to be 1.5 years, since younger patients had OA in only 21% of their affected hips whereas the rate was 58% in older patients.
Residual dysplasia/subluxation (Severin grades III/IV) at skeletal maturity was a risk factor for the development of OA, which confirms the experience of previous long-term studies.1,9,18 This indicates that hips with especially low femoral head coverage (CE angle < 10° and MP ≥ 33%) during childhood and adolescence, should be surgically corrected with the hope of avoiding or postponing OA in adult life. AVN tended to be a significant risk factor for poor long-term outcome in univariable analysis, in agreement with previous studies.1,16,18,19 However, the number of hips with AVN was rather small, which reduced the reliability of the statistical assessment of this variable.
Obvious limitations of the present study are that it was retrospective and that there was no control group. The main characteristic of the study was relatively long traction time to obtain closed reduction. Although the results were quite satisfactory, our treatment policy has, for various reasons, changed over the years to a shorter time in traction and more often open reduction.5 Several weeks of traction is inconvenient for patients and has been replaced by a traction period of only one week. We think closed reduction under general anesthesia should be attempted in children under 1.5 years. If unsuccessful, open reduction should be performed under the same anesthesia. In older children we prefer open reduction without preliminary traction, which should be combined with femoral shortening osteotomy and acetabular osteotomy in those three or more years.
Conclusions
With a follow-up to patient age 58 years, the clinical and radiographic outcome of late-detected DDH, treated with closed reduction, was satisfactory in 53% of the hips. Risk factors for poor long-term outcome were age at reduction ≥ 1.5 years and residual dysplasia and subluxation. Although our treatment concepts have changed over the last decades, the present results should be relevant for comparison with future studies, in order to evaluate whether more modern treatment concepts will give better long-term outcomes.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA Licence Text
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) license (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
ICMJE Conflict of interest statement
The author has no conflict of interest or funding to disclose.
References
- 1.Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg [Am] 1994;76-A:1777–1792. [DOI] [PubMed] [Google Scholar]
- 2.Terjesen T, Halvorsen V. Long-term results after closed reduction of late-detected hip dislocation: 60 patients followed up to skeletal maturity. Acta Orthop 2007;78:236–246. [DOI] [PubMed] [Google Scholar]
- 3.Berkeley ME, Dickson JH, Cain TE, Donovan MM. Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg [Am] 1984;66-A:412–420. [PubMed] [Google Scholar]
- 4.Gabuzda GM, Renshaw TS. Reduction of congenital dislocation of the hip. J Bone Joint Surg [Am] 1992;74-A:624–631. [PubMed] [Google Scholar]
- 5.Terjesen T, Horn J. Have changes in treatment of late-detected developmental dysplasia of the hip during the last decades led to better radiographic outcome? Clin Orthop Relat Res 2016;474:1189–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas SR, Wedge JH, Salter RB. Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. J Bone Joint Surg [Am] 2007;89-A:2341–2350. [DOI] [PubMed] [Google Scholar]
- 7.Terjesen T, Horn J, Gunderson RB. Fifty-year follow-up of late-detected hip dislocation: clinical and radiographic outcomes for seventy-one patients treated with traction to obtain gradual closed reduction. J Bone Joint Surg [Am] 2014;96-A:e28. [DOI] [PubMed] [Google Scholar]
- 8.Reimers J. The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl 1980;184:1–100. [DOI] [PubMed] [Google Scholar]
- 9.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand (Suppl 58) 1939;83:7–135. [Google Scholar]
- 10.Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg [Am] 1980;62-A:876–888. [PubMed] [Google Scholar]
- 11.Severin E. Contribution to the knowledge of congenital dislocation of the hip joint. Acta Chir Scand 1941;84:1–142. [Google Scholar]
- 12.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg [Am] 1969;51-A:737–755. [PubMed] [Google Scholar]
- 13.Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy 2000;16:578–587. [DOI] [PubMed] [Google Scholar]
- 14.Edwards PK, Queen RM, Butler RJ, Bolognesi MP, Lowry Barnes C. Are range of motion measurements needed when calculating the Harris hip score? J Arthroplasty 2016;31:815–819. [DOI] [PubMed] [Google Scholar]
- 15.Jacobsen S, Sonne-Holm S. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology (Oxford) 2005;44:211–218. [DOI] [PubMed] [Google Scholar]
- 16.Böhm P, Brzuske A. Salter innominate osteotomy for the treatment of developmental dysplasia of the hip in children: results of seventy-three consecutive osteotomies after twenty-six to thirty-five years of follow-up. J Bone Joint Surg [Am] 2002;84-A:178–186. [PubMed] [Google Scholar]
- 17.Morin C, Bisogno J, Kulkarni S, Morel G. Treatment of late-presenting developmental dislocation of the hip by progressive orthopaedic reduction and innominate osteotomy. Our results with more than 30 years of follow up. J Child Orthop 2011;5:251–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angliss R, Fujii G, Pickvance E, Wainwright AM, Benson MKD. Surgical treatment of late developmental displacement of the hip. Results after 33 years. J Bone Joint Surg [Br] 2005;87-B:384–394. [DOI] [PubMed] [Google Scholar]
- 19.Holman J, Carroll KL, Murray KA, Macleod LM, Roach JW. Long-term follow-up of open reduction surgery for developmental dislocation of the hip. J Pediatr Orthop 2012;32:121–124. [DOI] [PubMed] [Google Scholar]


