Abstract
Purpose
Developmental dysplasia of the hip (DDH) after walking age is difficult to treat. Dega pelvic osteotomy is combined with open reduction and femoral osteotomy to obtain concentric stable reduction with good coverage of the femoral head. The purpose of this study is to evaluate the use of the Dega osteotomy in the treatment of DDH in two different age groups.
Methods
A total of 45 patients (52 hips) with a mean age of 3.9 years (1.2 to 12.8) were treated with open reduction, Dega osteotomy and femoral osteotomy. There were 38 dislocated and 14 subluxated hips. Bilateral DDH was observed in seven female patients. Radiographic parameters included acetabular index, centre-edge angle of Wiberg and migration percentage. The final radiographic outcome was evaluated according to the Severin classification.
Results
The mean follow-up period was four years (3 to 9). According to the Severin criteria 78.8% were types I or II whereas 21.2% showed types III or IV. There was no statistically significant difference in final outcome between children less than three years of age and older children at the time of surgery.
One hip in children with unilateral involvement had developed coxa magna, that interfered with hip concentricity. Three hips (5.8%) showed avascular necrosis of the femoral head.
Conclusion
Dega osteotomy is a safe and adequate procedure for the management of developmental dysplasia of the hip in walking patients with low complication rates. Restoring the acetabulum to normal or nearly normal can result in good medium-term results.
Level of Evidence
III
Keywords: Dega osteotomy, developmental dysplasia of the hip, open reduction
Introduction
Treatment of developmental dysplasia of the hip (DDH) after walking age is difficult because of adaptive shortening of the extra-articular soft tissues, acetabular dysplasia, capsular constriction and increased femoral anteversion.1
Open reduction can be performed with or without femoral and/or pelvic osteotomy. The one-stage procedure (open reduction, capsulorrhaphy and innominate osteotomy) is preferred by many surgeons. In late presenting children, pelvic osteotomy is needed to achieve a stable concentric reduction.2–5
Dega osteotomy is one of the most commonly used osteotomies in the management of DDH. The first transiliac osteotomy was performed and registered by Wiktor Dega in 1958 in Poznan Hospital in Poland (Figs 1 and 2). Dega’s initial osteotomy was first mentioned briefly in a 1964 German publication,6 but it was not until 1969, in a Polish publication, that he first referred to this initial osteotomy as a supra-acetabular semicircular osteotomy.7
Fig. 1.
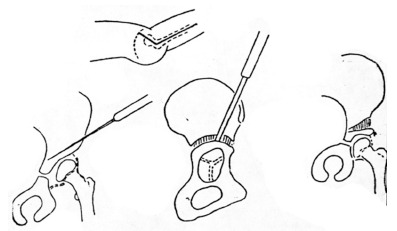
Original drawing of pelvic osteotomy by Wiktor Dega (permission to reprint obtained from Chir Narzadow Ruchu Ortop Pol).7
Fig. 2.

The radiograph of the first Dega osteotomy performed in 1958 in Poznan (Poland) (courtesy of Department of Orthopedics, Wiktor Dega’s Orthopaedic and Rehabilitation Clinical Hospital, Poznan University of Medical Sciences, Poland).
The iliac osteotomy described by Wiktor Dega in Poland in 19697 is an acetabuloplasty that changes the acetabular configuration and its inclination. This allows an adequate acetabular coverage for anterior, lateral and mainly posterior deficiencies.6 In the 1964 German publication, Dega did not provide a detailed description of the osteotomy, but he did emphasize that the medial iliac cortex was not to be cut, to prevent the acetabular fragment from displacing medially in a ‘manner consistent with a Chiari osteotomy’. The osteotomy was described as a semicircular cut through the lateral wall of the ilium directed toward but not through the medial cortex of the ilium. It established a basis for the subsequent development of what Dega termed a transiliac osteotomy.7,8
The aim of this study was to evaluate radiographic results of Dega osteotomy after three to nine years of follow-up and to examine whether there was any association between radiographic outcome and age at surgery.
Patients and methods
Between January 2009 and April 2015, 45 patients, 37 female and eight male (52 hips) were treated with open reduction, femoral osteotomy with shortening, and Dega osteotomy. This retrospective study was approved by our ethical committee for research. The mean age of the patients at the time of the operation was 3.9 years (1.2 to 12.8). There were 38 dislocated and 14 subluxated hips according to the Tönnis grading.9 Bilateral DDH was observed in seven female patients.
A total of 21 patients (24 hips) had been unsuccessfully treated with closed reduction under fluoroscopy guidance, followed by spica cast application for 12 weeks. This procedure was always performed before 12 months of age. The remaining 24 patients (28 hips) were referred from different hospitals as neglected DDH cases; four of them were bilateral DDH cases and seven presented with subluxed hips.
The data were analyzed using the JMP 10.0.2 statistical software (SAS, Cary, North Carolina). Analysis of variances post-hoc Tukey Honest Significant Difference test, and t-test for independent means were used. A p-value < 0.05 was considered significant.
Surgical management
The osteotomy was performed as described by Dega7,8 in his original paper (Fig. 1).
All operations were done under general anesthesia on a radiolucent table. The patient was in supine position with slight elevation of the affected side by placing a roll under the ilium. The entire lower limb and the affected half of the pelvis was prepared and draped. The anterolateral approach to the open reduction of the hip was used. The exposure of the iliac bone was performed by iliac apophysis reflection.
The abductor muscles were sharply reflected off of the lateral wall of the ilium just distal to the iliac apophysis. The apophysis itself was not split, but it was detached laterally at the junction of cartilage and outer bony table, from the anterosuperior iliac spine to the posterior crest. Then the whole iliac apophysis was displaced medially.
For open reduction, the rectus femoris was dissected from the underlying joint capsule, and its conjoint tendon was divided and retracted distally. The joint capsule was dissected with a periosteal elevator medially from the ilium and from any false acetabulum down to the true acetabulum, and laterally from the abductor muscles. The capsule was exposed superiorly around to the posterior aspect to facilitate capsulorrhaphy, and inferiorly to its insertion into the bottom of the acetabulum. The psoas tendon was identified just medial to the anteroinferior iliac spine.
The capsule was incised parallel with and about 1 cm distal to the rim of the acetabulum, then incised at a right angle to the first incision, thus creating a T-shaped incision. Kocher-Ochsner clamps (Aesculap Chifa Sp.z.o.o., Nowy Tomy l, Poland) were used to retract the capsule and expose the femoral head and the ligamentum teres. The ligamentum teres was detached from the femoral head and grasped with a Kocher clamp. The ligamentum teres was traced down to the true acetabulum and to the transverse acetabular ligament, and excised. The transverse acetabular ligament was divided to enlarge the inferior aspect of the acetabulum, and any pulvinar in the true acetabulum was excised using a rongeur or sharp dissector. The hip, then, was reduced.
Next, Dega osteotomy was performed to decrease acetabular dysplasia and to enhance containment of the femoral head. The orientation of the osteotomy was first marked on the lateral cortex of the ilium. The direction of the osteotomy is curvilinear when viewed from the lateral cortex, starting just above the anteroinferior iliac spine, curving gently cephalad and posteriorly to reach a point superior to the midpoint of the acetabulum and then continuing posteriorly to end approximately 1 cm to 1.5 cm in front of the sciatic notch.
Leaving the sciatic notch intact allowed anterior and lateral coverage, whereas leaving a portion of the inner table and entering through the notch allows more posterior coverage. The direction of required coverage is determined intraoperatively by direct observation of the hip joint. A more cephalad starting point and a steeper osteotomy angle allow for more lateral coverage. The closer the osteotomy is to the acetabulum, the thinner and more pliable the acetabular fragment will be, theoretically allowing for more reshaping and less redirection to occur. The most cephalad extent of the osteotomy is in the middle of the acetabulum, at a point on the ilium determined by the steepness of the acetabulum. Very steep acetabular inclinations required correspondingly a higher midpoint. A guidewire was inserted under fluoroscopic control at the most cephalad point of the curvilinear marking line, directed caudally and medially to ensure that the osteotomy will exit at the appropriate level just above the horizontal limb of the triradiate cartilage. A straight 0.25-inch or 0.5-inch (0.64 cm or 1.3 cm) osteotome was used to perform the bone incision, which extends obliquely medially and inferiorly, paralleling the guide-wire to exit through the inner cortex just above the iliopubic and ilioischial limbs of the triradiate cartilage. With experience, the osteotomy might be performed safely without fluoroscopic guidance, as in Dega’s original description. A half-inch osteotome or small laminar spreader was then used to gently lever open the osteotomy site either anteriorly or laterally in a controlled manner. While the osteotomy site was being opened, the osteotomy on the outer cortex of the ilium extended toward the sciatic notch as a greenstick fracture. However, since the posterior portion of the inner cortex is still intact, the outer cortical greenstick fracture does not weaken the recoil and stability at the osteotomy site. The osteotomy site was kept open by inserting two correctly sized bone grafts.
The correct graft size was determined by simply noting the opening of the osteotomy gap created by the laminar spreader or the levering osteotome.
In congenital dysplasia, acetabular deficiency is most pronounced anteriorly, mandating placement of the larger graft more anteriorly. A smaller graft is then wedged more posteriorly, just in front of the intact sciatic notch. Care was taken to ensure that both grafts are of an appropriate width and that the amount of correction of the dysplastic acetabulum provides enough coverage of the femoral head. The grafts came from a bicortical autologous bone graft from the iliac crest or, if femoral shortening had been performed, the segment of the femur that was removed was utilized as a graft. The graft should be wedge shaped.
Once the grafts were inserted, they became stable because of the inherent recoil at the osteotomy site produced by the intact sciatic notch. Variations in the graft size and placement, extent of the outer and inner cortical incisions, and thickness of the acetabular fragment make it possible to both reorient and reshape the acetabulum.
Next, the two halves of the iliac epiphysis were sutured together over the iliac crest, or reduction of the displaced epiphysis over the iliac bone, according to the approach performed. The rectus femoris and the sartorius were sutured to their origins. Next, the subcutaneous tissue and skin were closed with a continuous subcuticular suture.
Femoral shortening in older patients with DDH can facilitate easy reduction and reduce the tension on the proximal femoral epiphysis. In this series, femoral shortening was performed in all hips using the segment as a graft for the Dega osteotomy site. Stabilization of the femoral osteotomy was performed using small dynamic compression plates.
Postoperatively the patients were immobilized in one and one-half hip spica cast with the hip in slight flexion for at least six weeks, approximately 10° of internal rotation and 20° to 30° abduction.
Anteroposterior and lateral radiographs were taken immediately after surgery, after six weeks or at removal of the spica cast, and then at six-month intervals until the last follow-up (Figs 3 and 4).
Fig. 3.

(a) Preoperative radiograph of a boy 1.5 years of age with dislocation of his right hip (hip number 5 in Table 1); (b) radiograph of the same patient at a follow-up of three years.
Fig. 4.

(a) Preoperative radiograph of boy 4.0 years of age with dislocation of his left hip (hip number 30 in Table 1); (b) radiograph of the same patient at a follow-up of three years.
Patients were divided into two age groups: group A – 1.2 to 2.9 years (24 patients/25 hips) and group B – 3.0 to 12.8 years (21 patients/27 hips).
Radiographic parameters included Tönnis classification of dislocation,9 acetabular index (AI),10 centre-edge angle of Wiberg (CE)11 and migration percentage (MP) according to Reimers.12 The final radiographic outcome was evaluated according to the Severin classification.13 However, when MP was 33%, the hip is subluxated12 and was classified in Severin group IV.
After assessment of radiographic healing of the osteotomy site, progressive weight-bearing was begun. Walking with full weight-bearing was allowed four months after surgery.
The presence of avascular necrosis (AVN) of the femoral head was determined using the criteria of Salter14 on the preoperative radiographs and radiographs during the follow-up period.
Coxa magna was defined as the asymmetrical, circumferential enlargement and deformation of the femoral head and neck. Definitions in the literature vary but enlargement with asymmetry > 10% in size is a reasonable cut-off for diagnosis.15
Results
The mean follow-up period was 4.0 years (3 to 9). Pre- and postoperative information about each patient and hip has been included in a general table (Table 1). Preoperative factors according to age groups at Dega operation are shown in Table 2. There were significantly more hips with complete dislocation in children three or more years old and also a larger proportion of bilateral DDH in this group.
Table 1.
Information on pre- and postoperative variables in all 45 patients (52 hips)
| N | CR | Gender | Age (yrs at index operation) | Displ | AI pre | AIfu | CEfu | MPfu | Severin group (at last follow-up) | AVNfu | Reoperation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1L | 2 | F | 1.2 | TD | 33 | 15 | 28 | 8 | I | No AVN | - |
| 2R | 1 | F | 1.2 | Sub | 32 | 13 | 33 | 17 | II | No AVN | - |
| 3R | 2 | F | 1.5 | TD | 37 | 18 | 47 | 3 | I | No AVN | - |
| 4R | 2 | F | 1.5 | Sub | 35 | 21 | 17 | 58 | IV | No AVN | - |
| 5R | 1 | M | 1.5 | TD | 35 | 20 | 33 | 0 | I | No AVN | - |
| 6L | 1 | F | 1.6 | Sub | 36 | 18 | 30 | 6 | I | No AVN | - |
| 7R | 2 | F | 1.6 | Sub | 49 | 28 | -19 | 78 | IV | No AVN | - |
| 8L | 2 | F | 1.6 | Sub | 32 | 24 | 30 | 12 | II | No AVN | - |
| 9R | 1 | M | 1.6 | TD | 34 | 24 | 10 | 38 | IV | No AVN | - |
| 10L | 1 | F | 1.7 | Sub | 42 | 11 | 27 | 18 | II | No AVN | - |
| 11R | 2 | F | 1.8 | TD | 35 | 17 | 30 | 0 | I | No AVN | - |
| 12R | 2 | F | 1.8 | Sub | 35 | 17 | 32 | 0 | I | No AVN | - |
| 13R | 1 | F | 1.9 | TD | 46 | 19 | 34 | 0 | I | No AVN | - |
| 14R | 1 | F | 1.9 | TD | 52 | 15 | 28 | 12 | II | No AVN | - |
| 15L | 1 | M | 1.9 | TD | 38 | 15 | 34 | 0 | I | No AVN | - |
| 16L | 2 | M | 2.0 | Sub | 44 | 18 | 21 | 0 | I | No AVN | - |
| 17L | 1 | F | 2.0 | TD | 48 | 24 | 23 | 18 | II | No AVN | - |
| 18L | 1 | F | 2.0 | TD | 47 | 20 | 14 | 38 | IV | No AVN | - |
| 19R | 1 | 2.5 | TD | 37 | 17 | 36 | 0 | I | No AVN | ||
| 20L | 2 | F | 2.1 | TD | 33 | 21 | 33 | 0 | I | No AVN | - |
| 21R | 1 | F | 2.2 | TD | 52 | 20 | 28 | 6 | I | No AVN | - |
| 22R | 2 | F | 2.3 | Sub | 30 | 16 | 32 | 16 | I | No AVN | - |
| 23L | 1 | F | 2.5 | TD | 33 | 27 | 34 | 0 | I | No AVN | - |
| 24R | 2 | F | 2.7 | Sub | 44 | 26 | 24 | 15 | II | No AVN | - |
| 25L | 2 | M | 2.8 | Sub | 32 | 24 | 26 | 15 | II | No AVN | - |
| 26R | 2 | F | 3.3 | TD | 52 | 16 | 24 | 13 | II | No AVN | - |
| 27L | 3.5 | TD | 43 | 13 | 22 | 29 | III | No AVN | |||
| 28L | 1 | F | 4.0 | TD | 53 | 30 | 30 | 12 | II | No AVN | - |
| 29R | 4.3 | TD | 43 | 29 | 35 | 6 | I | No AVN | |||
| 30L | 1 | M | 4.0 | TD | 34 | 15 | 31 | 6 | I | No AVN | - |
| 31L | 1 | F | 4.0 | TD | 30 | 11 | 29 | 9 | I | No AVN | - |
| 32R | 4.1 | TD | 29 | 12 | 35 | 0 | I | No AVN | |||
| 33L | 1 | F | 4.3 | Sub | 31 | 25 | 35 | 10 | I | No AVN | - |
| 34L | 2 | F | 4.4 | TD | 49 | 31 | -7 | 61 | IV | No AVN | - |
| 35R | 4.5 | TD | 47 | 22 | 21 | 0 | I | No AVN | |||
| 36L | 1 | F | 4.4 | TD | 31 | 11 | 27 | 9 | I | AVN | - |
| 37L | 1 | F | 4.4 | TD | 34 | 19 | 53 | 10 | II | No AVN | - |
| 38R | 4.6 | Sub | 30 | 22 | 41 | 0 | I | No AVN | |||
| 39R | 1 | F | 4.6 | TD | 47 | 21 | 32 | 9 | I | No AVN | - |
| 40L | 2 | F | 5.4 | TD | 34 | 24 | 18 | 35 | IV | AVN | - |
| 41R | 2 | F | 5.6 | TD | 33 | 14 | 30 | 24 | II | No AVN | - |
| 42L | 2 | F | 4.9 | TD | 39 | 13 | 31 | 0 | I | No AVN | - |
| 43R | 5.9 | TD | 36 | 21 | 14 | 37 | IV | No AVN | |||
| 44R | 2 | F | 6.2 | TD | 44 | 22 | 25 | 17 | II | No AVN | - |
| 45R | 2 | M | 6.5 | Sub | 52 | 43 | 3 | 54 | IV | No AVN | - |
| 46L | 1 | F | 7.3 | TD | 36 | 20 | 11 | 46 | IV | AVN | - |
| 47R | 1 | M | 7.6 | TD | 35 | 20 | 43 | 6 | I | No AVN | - |
| 48L | 1 | F | 7.5 | TD | 34 | 29 | 18 | 19 | II | No AVN | PO |
| 49R | 1 | F | 7.7 | TD | 40 | 28 | 22 | 8 | II | No AVN | - |
| 50R | 1 | F | 9.6 | TD | 46 | 26 | 28 | 19 | II | No AVN | - |
| 51L | 2 | F | 9.8 | TD | 47 | 19 | 40 | 0 | I | No AVN | - |
| 52L | 2 | F | 12.8 | TD | 40 | 20 | 2 | 53 | IV | No AVN | - |
TaN, hip number; R, right, L, left; CR, closed reduction; 1, no previous closed reduction; 2, previous failed closed reduction; Displ, grade of displacement; Sub, subluxation; TD, total displacement; Aipre, acetabular index preoperatively’ Aifu, AI at last follow-up; Cefu, centre-edge angle at last follow-up; MPfu, migration percentage at last follow-up; AVNfu, avascular necrosis at last follow-up; PO, periacetabular osteotomy
Table 2.
Preoperative factors according to age groups at the time of Dega osteotomy
| Variables | Group A < 3 yrs | Group B 3 to 12 yrs | p-value* |
|---|---|---|---|
| Subluxation (n) | 11 | 3 | 0.008 |
| Dislocation (n) | 14 | 24 | |
| Unilateral Dega (n) | 23 | 15 | 0.003 |
| Bilateral Dega (n) | 2 | 12 | |
| No previous reduction (n) | 13 | 15 | 0.797 |
| Previous closed reduction (n) | 12 | 12 | |
| AI preoperatively (°) | 38.8 | 39.6 | 0.709 |
n, number of hips; AI, acetabular index;
using T-test for independent means (statistically significant if < 0,05
According to the Severin criteria of radiographic results, 78.8% (41 hips) were types I or II whereas 21.2% (11 hips) showed types III or IV. No hips were rated groups V or VI. Table 3 shows the results at the last follow-up according to the age groups. Although the outcome was somewhat better in children less than three years of age at surgery (84% Severin groups I/II versus 74%), the difference was not statistically significant (Table 3).
Table 3.
Radiographic results at the last follow-up according to age groups
| Variables | Group A < 3 yrs | Group B 3 to 12 yrs | p-value* |
|---|---|---|---|
| Severin groups I/II (n) | 21 | 20 | 0.381 |
| Severin groups III/IV (n) | 4 | 7 | |
| AI (°) | 19.5 | 21.3 | 0.293 |
| Centre-edge angle (°) | 26.6 | 25.7 | 0.396 |
| Migration percentage (%) | 14.3 | 18.2 | 0.230 |
n, number of hips; AI, acetabular index;
using T-test for independent means (statistically significant if < 0.05)
The early postoperative CE angle ranged from 2° to 50° and the mean values were 32.1° for group A and 27.8° for group B. The CE showed further change up to the final follow-up with a mean of 26.62° for group A and 25.67° for group B (Table 3). AI was corrected from 38.8° preoperatively to an average of 19.5° at the final follow-up for group A and from 39.6° to 21.3° for group B. The mean MP at the last follow-up was 14.3% in group A and 18.2 % in group B. There were no statistically significant differences between the age groups in the radiographic variables (AI, CE angle and MP) at the last follow-up (Table 3).
Three hips (5.8%) developed AVN of the femoral head (Table 1). One patient was diagnosed preoperatively at age four years. In two patients in group B, AVN was detected one year after Dega osteotomy. In one patient with unilateral hip involvement coxa magna was diagnosed. It was associated with loss of hip congruency but was not associated with AVN. Periacetabular osteotomy (PAO) was performed in one hip seven years after the index surgery.
Discussion
Several types of pelvic osteotomies to stabilize the reduced hip in older children have been described. Currently, incomplete transiliac acetabuloplasty with the use of the technique of Dega and the complete pelvic osteotomy of Salter are most often performed. When the dysplasia is severe, Dega osteotomy is the procedure of choice as it provides more correction to the acetabular index, while, when the dysplasia is mild to moderate, Salter osteotomy can provide satisfactory correction. Caution should be taken during Salter osteotomy when combined with femoral derotational osteotomy, however, to avoid posterior subluxation of the femoral head.16
According to our knowledge, our study is the first comparison of two different age groups. There is still controversy concerning the upper age limit that is suitable for reduction in neglected cases of DDH. It is claimed that as long as the triradiate cartilage is still open and growing, there is a possibility of achieving a stable concentric reduction.1 In this study, the final radiological evaluation was 78.8% of favourable results (excellent and good) and 21.2% of unfavourable results. There was no statistically significant correlation between the outcome and the age of the patients at the time of surgery. Younger age at the time of the index surgery does not guarantee better final radiological outcome. It may suggest that the operation should be performed early, but may be also performed in older age. This supports the findings of other authors.1,16
AI was used as one of the references of the acetabular remodelling after Dega osteotomy. The mean AI of all the hips was markedly corrected from 39° preoperatively to 20° at the last follow-up. This correction is in accordance with previous studies that have reported a range of AI values of 11° to 25° at the last follow-up (Table 4).1,16–19 This shows the high efficacy of Dega pelvic osteotomy in restoration of AI close to normal values. The upper normal limit of AI, defined as mean plus 2 sd, is 23° at age five to seven years,20 and Severin considered that the acetabulum was normal if AI was < 21° above age ten years.13
Table 4.
Comparison of results of Dega osteotomy from previous studies and the present study
| Study | Hips (n) | Age (yrs) | Follow-up (yrs) | Severin I/II (%) | AI pre | AI post | CE angle |
|---|---|---|---|---|---|---|---|
| Al-Ghamdi et al 201219 | 21 | 4.6 (1.7 to 8.3) | 7.3 | 71 | 37 | 19 | 25 |
| Grudziak and Ward 200116 | 24 | 5.8 | 4.6 | - | 33 | 12 | 31 |
| Ruszkowski and Pucher 200517 | 33 | 1.3 (0.5 to 2) | 9.4 | 72 | 36 | 11 | 33 |
| El-Sayed et al 20151 | 58 | 4.1 (2.1 to 7.5) | 16.7 | 73 | 39 | 25 | 34 |
| Karlen et al 200918 | 26 | 3.1 | 4.3 | - | 37 | 13 | - |
| Czubak et al 2018 (present study) | 52 | 3.9 (1.2 to 12.8) | 4.0 | 79 | 39 | 20 | 26 |
AI, acetabular index; CE, centre-edge;
The CE angle in this study improved to a mean value of 26° at the last follow-up. These results are similar to those reported by other authors, where the mean CE angle at follow-up varied from 25° to 34° (Table 4).
Three hips (5.8%) developed AVN. AVN is one of the major complications in DDH management, and there are differences in the rate of AVN reported in various studies.4,5,14 Some studies included only primary untreated hips, others included only patients with a previous history of attempts at closed reduction, and some series included all patients with DDH, even those with a history of failed open reduction. As suggested by many authors, this might correlate directly with the type of pelvic osteotomy because of premature closure of the triradiated cartilage, which might also lead to residual acetabular dysplasia.1,17–19,21,22.
Our study showed that the combined procedure of open reduction, femoral shortening, and Dega osteotomy was an adequate single-stage surgery in patients with late-detected DDH. The results correlate with the findings of many authors,1,16–19,21,22 as the first operation of the patient is the golden chance for better results and a favourable outcome with fewer complications.
Conclusions
Dega pelvic osteotomy added to open reduction and femoral shortening is a safe and adequate procedure for the management of DDH patients after walking age, with low complication rates.
Restoration of the acetabulum to normal or nearly normal resulted in good short- and medium-term results.
There was no statistically significant difference between the final radiological outcome of younger and older patients.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA Licence Text
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) license (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. IRB approval was waived as it was not necessary in this type of study.
Informed Consent: Informed consent was not necessary for this work.
ICMJE Conflict of interest statement
None declared.
References
- 1.El-Sayed MM, Hegazy M, Abdelatif NM, et al. Dega osteotomy for the management of developmental dysplasia of the hip in children aged 2–8 years: results of 58 consecutive osteotomies after 13–25 years of follow-up. J Child Orthop 2015;9:191–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carvalho Filho G, Chueire AG, Ignácio H, et al. Surgical treatment of the congenital dislocation of the hip after walking age: open reduction and Salter’s osteotomy. Acta Ortop Bras 2003;11:42–47. [Google Scholar]
- 3.Salter RB, Dubos JP. The first fifteen year’s personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop Relat Res 1974;98:72–103. [DOI] [PubMed] [Google Scholar]
- 4.Pemberton PA. Pericapsular osteotomy of the ilium for treatment of congenital subluxation and dislocation of the hip. J Bone Joint Surg [Am] 1965;47-A:65–86. [PubMed] [Google Scholar]
- 5.Ahmed E, Mohamed AH, Wael H. Surgical treatment of the late – presenting developmental dislocation of the hip after walking age. Acta Ortop Bras 2013;21:276–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dega W. Difficulties in the surgical reposition of the obsolete congenital subluxation of the hip joint in children. Beitr Orthop Traumatol 1964;11:642–647. [Google Scholar]
- 7.Dega W. Selection of surgical methods in the treatment of congenital dislocation of the hip in children. Chir Narzadow Ruchu Ortop Pol 1969;34:357–366. [PubMed] [Google Scholar]
- 8.Dega W. Transiliac osteotomy in the treatment of congenital hip dysplasia. Chir Narzadow Ruchu Ortop Pol 1974;39:601–613. [PubMed] [Google Scholar]
- 9.Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. Berlin Heidelberg: Springer-Verlag, 1987:82–83.
- 10.Hilgenreiner H. Zur Frühdiagnose und Frühbehandlung der angeborenen Hüftgelenksverrenkung. Med Klin 1925;21:1425–1429. [Google Scholar]
- 11.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special reference to the complication of osteoarthritis. Acta Chir Scand 1939;83:53–68. [Google Scholar]
- 12.Reimers J. The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl 1980;184:1–100. [DOI] [PubMed] [Google Scholar]
- 13.Severin E. Contribution to the knowledge of congenital dislocation of the hip joint. Late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scand 1941;84:1–142. [Google Scholar]
- 14.Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: a clinical and experimental investigation. Can J Surg 1969;12-1:44–61. [PubMed] [Google Scholar]
- 15.Young EY, Gebhart JJ, Bajwa N, Cooperman DR, Ahn NU. Femoral head asymmetry and coxa magna: anatomic study. J Pediatr Orthop 2014;34: 415–420. [DOI] [PubMed] [Google Scholar]
- 16.Grudziak JS, Ward WT. Dega osteotomy for the treatment of congenital dysplasia of the hip. J Bone Joint Surg [Am] 2001;83-A:845–854. [DOI] [PubMed] [Google Scholar]
- 17.Ruszkowski K, Pucher A. Simultaneous open reduction and Dega transiliac osteotomy for developmental dislocation of the hip in children under 24 months of age. J Pediatr Orthop 2005;25:695–701. [DOI] [PubMed] [Google Scholar]
- 18.Karlen JW, Skaggs DL, Ramachandran M, Kay R. The Dega osteotomy: a versatile osteotomy in the treatment of developmental and neuromuscular hip pathology. J Pediatr Orthop 2009;29:676–682. [DOI] [PubMed] [Google Scholar]
- 19.Al-Ghamdi A, Rendon JS, Al-Faya F, et al. Dega osteotomy for the correction of acetabular dysplasia of the hip: a radiographic review of 21 cases. J Pediatr Orthop 2012;32:113–120. [DOI] [PubMed] [Google Scholar]
- 20.Tönnis D, Brunken D. Differentiation of normal and pathological acetabular roof angle in the diagnosis of hip dysplasia. Evaluation of 2294 acetabular roof angles of hip joints in children. Arch Orthop Unfallchir 1968;64:197–228. [DOI] [PubMed] [Google Scholar]
- 21.Barrett WP, Staheli LT, Chew DE. The effectiveness of the Salter innominate osteotomy in the treatment of congenital dislocation of the hip. J Bone Joint Surg [Am] 1986;68-A:79–87. [PubMed] [Google Scholar]
- 22.Mazen M. Ibrahim, Mohamed R. S. El-Lakkany, Mohamed M. Wahba, et al. Combined open reduction and Dega transiliac osteotomy for developmental dysplasia of the hip in walking children. Acta Orthop Belg 2016;82:222–232. [PubMed] [Google Scholar]


