Abstract
Purpose
Discuss current indications, techniques, complications and results of periacetabular osteotomy (PAO) to treat the adolescent and young adult with symptomatic acetabular dysplasia or the rare minimally symptomatic patient with dysplasia with a guarded prognosis without PAO surgery.
Methods
Review of clinical experience with PAO at our and other high-volume centres.
Results
At a mean follow-up of 18 years after PAO, more than 75% of hips are preserved. At 30-year follow-up, longest term reported series notes survival of one-third of hips.
Conclusion
Both middle- and long-term results suggest efficacy of PAO in improving function and prognosis in most symptomatic adolescent and young adult patients with spherically congruous pre-arthritic dysplastic hips.
Keywords: Acetabular dysplasia, hip dysplasia, acetabular osteotomy, pelvic osteotomy
Introduction
Developmental dysplasia of the hip (DDH) is a major cause of dysfunction in many countries around the world. While screening for DDH in infants is commonly practised, many adolescents and young adults continue to present with symptomatic hip dysplasia. These delayed presentations are most likely the result of missed childhood diagnoses of DDH or diagnosed cases of DDH that were incompletely treated earlier in childhood. Hip dysplasia in this age group is a frequent cause of osteoarthritis and total hip arthroplasty at a relatively young age. The typical deformity involves anatomical acetabular insufficiency, with decreased acetabular contact area and subsequent overload of the acetabular rim. Acetabular redirection surgery to improve the mechanics in the hip with a dysplastic acetabulum was first suggested and utilized by Salter in the 1960s when he noted anterolateral uncovering of the femoral head in children with DDH.1 His innominate osteotomy provided increased anterolateral coverage of the hip and was highly effective in improving the mechanical function of many hips with DDH. With time, our appreciation of the complexities to the dysplastic hip has improved. The Salter osteotomy has been superseded by more complex and powerful redirectional procedures, among which the Bernese periacetabular osteotomy (PAO) is the most frequently employed in North America and Europe.2
The rationale for acetabular redirection in the dysplastic hip is to normalize mechanics of the hip by reducing the excessive stresses on the acetabular rim and adjacent labrum. The PAO, as an acetabular redirection procedure, does not directly augment the insufficient regions of the acetabulum area of the cartilaginous acetabulum and rim. The PAO improves hip mechanics by optimizing the position of the lunate cartilage available to transmit forces during weight-bearing activities, which effectively decreases contact stresses and forces to the acetabular rim and labrum. PAO has distinct advantages over other osteotomies for the mature hip, including the triple osteotomy and rotational acetabular osteotomy. It can be performed through a single anterior incision with approaches designed to spare the abductors and rectus femoris.3,4 The PAO creates a relatively large acetabular fragment with sufficient vascularity to allow arthrotomy for intra-articular work5 while preserving a portion of the posterior column to maintain pelvic stability and minimize compromise of the birth canal. Last, internal fixation with multiple screws complements the osteotomy’s inherently stable geometry to permit early partial weight-bearing without need for external immobilization.
This review will pay particular attention to the optimal indications for PAO. Surgical techniques, complications and results of PAO in the middle- and long-term will also be discussed. Our goal is to continually improve the treatment, and subsequent outcomes, of the large population of patients who continue to present in adolescence and adulthood with residual acetabular dysplasia.
Indications for PAO
The classic indication for PAO is the skeletally mature, symptomatic patient with a spherically congruous but dysplastic hip. In practice, PAO, or similar acetabular redirectional osteotomy, should be considered for skeletally mature patients with spherically congruous acetabular dysplasia severe enough to have a poor prognosis unless corrected. Spherical hips with lateral centre-edge (CE) angle below 20° and roof angle tilt of more than 15° are associated with a high risk of symptoms and osteoarthritis without correction,6 while hips with milder coverage insufficiency (lateral CE angle (LCEA) < 28°) have also been identified as at risk for early degeneration.7 Combined deformities, such as femoral asphericity due to a cam lesion, can further accelerate the degenerative process. Early detection of these patients is essential in providing timely treatments.
Patient evaluation
The patient interview is crucial in accurately diagnosing and setting reasonable expectations for treatment. Symptoms associated with the dysplasia are typically secondary to abductor fatigue (lateral/posterolateral pain) and/or overload of the capsule and/or labrum (anterior groin pain). In general, symptom severity will be indicative of the level of mechanical dysfunction present in the hip. Symptoms tend to be most pronounced during upright weight-bearing activity. Combined symptoms during stance and sitting positions should raise awareness of impingement pathology, specifically cam-type deformities of the proximal femur.
The physical exam provides essential information for optimal treatment. Both static and dynamic assessment of hip function is important, as are body and limb alignment, measurement of limb length and arcs of hip movement both in extension (femoral version) and flexion (femoroacetabular impingement). Provocative manoeuvres to test for both hip instability (extension/external rotation) and hip impingement (flexion/internal rotation) should be performed. Note the manoeuvres that cause pain. Careful assessment of strength, stance and gait are important in interpreting the global health of the hip.
Imaging
Imaging information is critical in characterizing hip deformity and has been used for more than 100 years as an aid to understanding hip mechanics. The radiograph remains the benchmark for assessing structural hip abnormalities, including hip dysplasia.8 The minimum radiographic data set that is generally employed in assessing mature acetabular dysplasia includes a standing well-centred anteroposterior (AP) radiograph of the entire pelvis, faux profil views and a modified Dunn lateral radiograph, taken in 45° of flexion, 30° of abduction and neutral rotation, to show in profile that anterolateral neck area which is the most common location of reduced offset. The AP radiograph is evaluated with measures of lateral and anterior coverage (LCEA; Tönnis roof angle; attitude of anterior and posterior walls; Shenton line intact or broken). The faux profil view predominantly assesses anterior coverage, quantitated by the anterior CE angle. All radiographs should be scrutinized for changes indicative of osteoarthritis, including cartilage space width and appearance of the subchondral bone. Table 1 shows the relevant measurements commonly made on these radiographs. In patients ultimately electing to undergo PAO, anticipated post-operative congruity is best confirmed preoperatively by functional flexion abduction internal rotation radiographs, simulating effect of the proposed redirection.
Table 1.
Relevant radiographic measurements in the evaluation of acetabular dysplasia
| Anteroposterior pelvis | Faux profil |
|---|---|
| Lateral centre-edge angle | Anterior centre-edge angle |
| Tönnis roof angle | |
| Anterior wall index | Dunn lateral |
| Posterior wall index | Alpha angle |
| Centrum-collum-diaphysea angle | Head/neck offset |
| Alpha angle |
Figure 1 illustrates the preoperative radiographic imaging of a 28-year-old patient evaluated for PAO to treat her symptomatic congruous acetabular dysplasia.
Fig. 1.

Standing anteroposterior (AP) pelvis radiograph is evaluated for dysplasia and joint health. Parameters of coverage include percent of head covered (coverage index; lateral centre-edge angle); tilt of the weight-bearing zone (Tönnis roof angle); and Shenton’s line. Joint health measures include minimum cartilage space width and subchondral bone quality. The anterior and posterior acetabular walls can be seen on a well-done image. They should meet, without crossing over, at the posterosuperior rim. Radiographs show: (a) a 28-year-old female with bilateral spherically congruous acetabular dysplasia. Her preoperative AP radiograph confirms bilateral dysplasia, with right hip lateral centre-edge angle 16° and Tönnis roof angle 14° degrees. Shenton’s line is intact; (b) functional view confirms wide abduction with no hinging.
Important technological advances in assessing hip deformity include low-dose CT and MRI. CT in particular has improved our 3D understanding of acetabular deformity in dysplasia. Nepple et al9 and Wilkin et al10 showed that acetabular dysplasia presents with three patterns of under-coverage: anterior, posterior and global. Recognition of the pattern of acetabular deficiency is critical in making a meaningful acetabular reorientation. MRI affords us the best ability to evaluate the soft-tissue structures of the hip affected by acetabular dysplasia. The acetabular labrum should be assessed for tearing at the chondrolabral junction as well as global hypertrophy, both of which can remain symptomatic following PAO if not addressed. MR cartilage specific sequences, such as delayed Gadolinium-enhanced MRI (dGEMRIC), are invaluable in evaluating cartilage health in hips with signs of early osteoarthritis. Preoperative dGEMRIC scores have been shown to have a predictive value in the survival of PAO.11 Moving beyond static imaging, dynamic ultrasonography has been used for decades in diagnosing instability in infant hips, but its use as a diagnostic tool in mature hip pathology is an area of recent focus and progress.
Treatment selection and planning
After patient evaluation, the results of history, physical examination and imaging must be synthesized to develop an optimal treatment strategy. The decision to proceed with PAO surgery must weigh the potential benefits of the operation with the risks inherent to the surgery and recovery process. Historically, the best results of PAO occur in patient subgroups that are relatively young, have spherically congruent articular surfaces and healthy cartilage at the time of surgery. Preoperative risk factors for a poor long-term result include older age, poor joint congruency and radiographic evidence of osteoarthritis. Thorough evaluation allows an accurate discussion of reasonable expectations for outcome following PAO, which is essential to help patients to make truly informed decisions. This is especially important in that failure to meet preoperative expectations (realistic or unrealistic) can lead to dissatisfaction and perceived failure of treatment, though the technical result may be highly satisfactory. Table 2 is a compiled list of considerations that should be made when developing a patient-specific preoperative plan.
Table 2.
Preoperative considerations prior to periacetabular osteotomy (PAO) surgery
| Preoperative checklist | Recommendations |
|---|---|
| Acetabular labral tears | Significant labral pathology (full thickness tears, large degenerative labrums) can remain symptomatic following PAO in spite of the mechanical offloading. The labrum should be evaluated and repaired as indicated by arthrotomy or arthroscopy. |
| Anterior inferior iliac spine (AIIS) | The AIIS should be evaluated on preoperative anteroposterior pelvis and faux profil radiographs. As the acetabular fragment is moved, a prominent AIIS will be placed into a position of impingement. Movement should be carefully checked after reorientation in these cases. |
| Femoral cam deformity | Cam deformities are seen in 30% to 40% of acetabular dysplasia cases. Impingement is a known cause of early PAO failures, so significant cam deformities should be addressed at the time of surgery via arthrotomy or arthroscopy. |
| Joint congruity | Preoperative Von-Rosen (flexion/abduction/internal rotation) views should be obtained in severe deformities. If concentric reduction not attained on this functional view, concomitant femoral-sided osteotomy can be considered. |
Surgical technique for PAO
Detailed discussions of surgical technique for PAO are available in the literature.12 The basic design for the PAO procedure, as developed by Ganz et al2 in the 1980s, is still followed today, with osteotomies of the anterior ischium; superior pubic ramus; anterior to posterior supra-acetabular ilium; and posterior column. The attitude and position of the osteotomy lines will vary slightly according to the anatomy of the individual pelvis and for the character of the realignment desired.
Patient setup
Routine preoperative and perioperative preparation includes patient education in partial weight-bearing crutch gait. Blood typing is typically recommended in the event that intraoperative or postoperative transfusion is required. In an effort to minimize intraoperative blood loss, transexamic acid is used unless contraindicated. Anesthesia is typically accomplished through a combination of general anesthesia with a lumbar plexus block. We have abandoned epidural anesthesia as it impaired early postoperative mobilization. Neuromuscular blockade is avoided, to allow intraoperative monitoring of motor nerve function. This is important, because the femoral, obturator and sciatic nerves lie in proximity to the osteotomy cuts. Any muscle contraction noted during the procedure suggests nerve irritation and immediate assessment to avoid impending nerve injury.
Fluoroscopy can be useful at various points during the PAO. The imaging machine should be positioned to obtain adequate AP pelvis and oblique faux profil-like views as needed. Intraoperative imaging can be useful in confirming optimal chisel and osteotome placement at certain points during the PAO. The experienced surgeon, in the routine case, however, should be able to identify important topical anatomic landmarks, and to plan and localize all osteotomies without the image intensifier. Confirmation by imaging is of course recommended as required in the individual case.
Surgical approach and osteotomies
The patient is positioned supine on a radiolucent Jackson type table, with the ipsilateral leg draped free. The trunk is prepped and draped to the midline and proximally to the costal margin. The limited direct anterior approach is routinely employed, sparing the abductor muscles and subperiosteally exposing the anterior ilium, iliopectineal line, posterior column, quadrilateral surface and the superior ramus to and beyond the iliopectineal eminence. The rectus tendon origin is routinely preserved unless an extensive arthrotomy is required, in which case the rectus tendon origin can be divided to provide more capsular exposure.4
The anterior ischial osteotomy (Fig .2a) is approached through the iliopectineal bursa, located between the medial capsule and the psoas tendon. This interval is opened and developed until the infracotyloid groove of the ischium, just distal to the inferior lip of the acetabulum and can be palpated with a long scissors. After the edges of the groove are identified, the bursal window, which lies between the medial capsule and the psoas tendon, can be gently dilated with blunt retractors. This allows safe placement of the angled chisel to perform the first osteotomy, at the level of the infracotyloid groove of the anterior ischium. This osteotomy, which cannot be directly visualized, begins just distal to the inferior lip of the acetabulum, leaving a bone bridge approximately 1 cm wide below the acetabulum. The chisel tip is placed just proximal to the obturator externus tendon, which normally occupies the groove. Both medial and lateral cortices of the anterior ischium must be divided as the chisel advances from anterior to posterior. Image intensifier control is useful both in initial placement of the chisel (AP and oblique projections) and in confirming that the osteotomy progresses satisfactorily (faux profil).
Fig. 2.
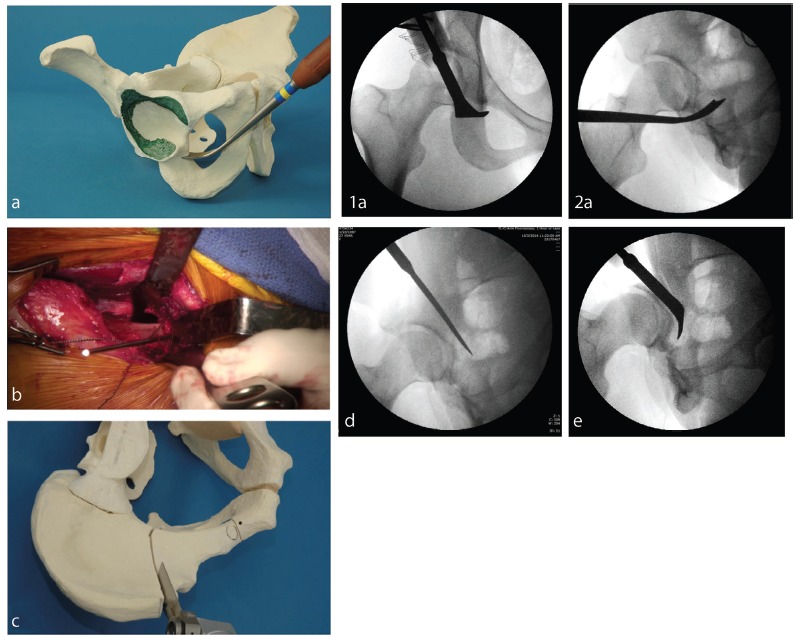
Intraoperative images confirm desired placement of osteotomies and desired realignment of the acetabulum to compensate for both anterior and lateral insufficiency: (a) anterior ischial osteotomy (infracotyloid groove), showing (1) correct placement within the groove, just distal to inferior lip of acetabulum and (2) image intensifier in anteroposterior and oblique projections confirms correct placement of chisel just distal to acetabulum; (b) superior pubic ramus osteotomy lies just medial to iliopectineal eminence; (c) iliac osteotomy begins just distal to the anterior superior spine, directed toward the apex of the greater sciatic notch. It ends at a point about 1 cm lateral to the iliopectineal line and approximately 3 cm anterior to the sacroiliac joint; (d) the posterior column osteotomy is made with a straight chisel. It begins at the posterior end of the iliac osteotomy. It is directed at the ischial spine, bisecting the posterior column, safely between the posterior acetabular wall and the anterior wall of the greater sciatic notch. The image intensifier in an oblique projection can confirm the proper position of this osoteotomy; (e) posterior ischial osteotomy. This osteotomy is made with a curved or angled chisel.
The superior pubic ramus osteotomy (Fig .2b), which routinely is done after the anterior ischial osteotomy, involves risk to the nearby obturator nerve. The hip is flexed and abducted to protect the psoas and femoral neurovascular structures as the periosteum is atraumatically dissected from the superior ramus. Retractors are placed around the ramus, into the obturator foramen and within the periosteal sleeve, to protect the obturator neurovascular bundle. The osteotomy is completed just medial to the iliopectineal eminence with either an osteotome, oscillating saw or Gigli saw. Confirmation of completeness of this osteotomy is mandatory, since this osteotomy must be free to allow acetabular reorientation.
The supra-acetabular iliac osteotomy (Fig .2c) requires atraumatic creation of a lateral sub-gluteal window at a level at or just distal to the ASIS osteotomy, with care to avoid disruption of the abductor origin. A small lateral retractor placed through this window gently retracts the abductors while a reverse Hohmann retractor placed on the quadrilateral plate is used to expose the medial iliac wing. An oscillating saw is used to osteotomize the ileum. This osteotomy should traverse the ilium from the distal aspect of the anterior superior iliac spine (ASIS) osteotomy to a point 1 cm shy of the iliopectineal line. This osteotomy should be nearly perfectly vertical in orientation and will appear to parallel an imaginary floor when viewed on faux profil imaging.
The posterior column osteotomy (Fig .2d) is made entirely from within the pelvis. It begins at the posterior end of the iliac osteotomy and is directed toward the ischial spine. The posterior column osteotomy bisects the posterior column as it passes over the iliopectineal line, passing between the posterior acetabulum and the greater sciatic notch. Straight osteotomes are used to create the superficial aspect of the osteotomy typically to the level of the acetabular isthmus, or about 3 cm to 4 cm into the true pelvis.
The posterior ischial osteotomy (Fig .2e) is angled more anteriorly and slightly laterally, to connect with the previously-made anterior ischial osteotomy. A bone spreader then placed in the anterior iliac osteotomy and brought up to some tension can help in mobilizing the acetabular fragment. At this point, the acetabular fragment often breaks free. If not, the angled Ganz chisel is used to osteotomize the small remaining posterior-inferior ischial bridge. The sciatic nerve is in close proximity to the distal, lateral aspect of this osteotomy. Careful positioning of the ipsilateral limb in extension and slight abduction can during this stage of the procedure reduce risk of neurapraxia.
Acetabular correction
The acetabular reorientation typically involves improving lateral coverage, anterior coverage and posterior coverage, in varying proportions (Fig. 3). The preoperative plan should include an assessment of how much angular correction is optimal. This will be based upon preoperative imaging and patient-reported symptom and exam findings. Any desired translation of the hip joint centre should also be considered.
Fig. 3.

Reorientation of acetabular fragment is achieved with a Weber bone clamp and Schanz screw placed in the anterior ilium above the joint to allow precise reorientation of acetabular fragment. Provisional fixation is achieved with smooth Kirschner-wires drilled from the iliac crest into the acetabular fragment. An anteroposterior full pelvis radiograph is taken to assess acetabular correction. This image confirms desired correction, with horizontal sourcil and normal version with no crossover sign or posterior wall sign. Definitive fixation is then achieved, with long cortical screws replacing the Kirchner-wires.
Prior to acetabular reorientation, the freedom of movement of the osteotomized acetabular fragment must be confirmed. Often, manipulating the fragment by tensioning a pair of laminar spreaders is helpful in freeing up soft-tissue constraints or persistent small bone bridges. Placement of a Schanz screw from anterior to posterior in the superior portion of the acetabular fragment is routinely used to grip the acetabular fragment to control reorientation. We find the supplemental use of a Weber bone clamp, with its tongs applied to the most medial portion of the acetabular fragment adjacent to the superior pubic ramus osteotomy is also helpful during reorientation.
After the desired reorientation is achieved, provisional fixation is obtained with multiple smooth Kirschner-wires drilled through iliac crest and into the acetabular fragment. The trajectory for placement is typically superior and posterior to the joint. The Schanz screw then is removed to allow assessment of passive hip movement.
With temporary fixation achieved, the adequacy of the correction is evaluated provisionally by fluoroscopic imaging. A well centered AP pelvis radiograph, however, is essential in assessing well the adequacy of the correction. The limited field-of-view offered by most image intensifiers can be misleading, especially with the AP image. Lowering the image intensifier as close to the body as possible will facilitate the widest field of view. General guidelines for an optimal correction on the AP pelvis image include a weight-bearing zone close to horizontal; no lateral translation of the hip centre; no crossover sign; well-balanced anterior and posterior coverage as reflected by the anterior and posterior walls indices; and concentric reduction of the centre of the femoral head under the weight-bearing zone of the acetabulum. An oblique faux profil-like view may be obtained with the image intensifier to assess anterior coverage as well as potential impingement. The anterior inferior iliac spine (AIIS) should also be considered as a potential cause of extra-articular impingement in its new, more distal position.
After a radiographically satisfying correction is achieved, passive range of movement should be checked, since anterior impingement is a known source of early failure and poor outcomes. At least 95° to 100° of flexion and 15° to 20° of internal rotation in flexion should be preserved to ensure postoperative function without impingement.
To directly assess for impingement, direct inspection is useful. Contact between the anterior hip structures – specifically between the neck and the anterior rim and AIIS – can be noted visually and by direct palpation during manipulation. If there is any question, the AIIS is readily accessible for osteoplasty. The femoral neck can be accessed through an anterior arthrotomy, which is done routinely if any question of impingement is present. Anterior labral issues felt to be major enough for direct inspection or surgical treatment can also be assessed via anterior arthrotomy, but better visualization is achieved arthroscopically (best done prior to the PAO, though it can be done under the same anesthetic, using a separate distraction table). If the new acetabular position is deemed less than ideal on either imaging or impingement analysis, the Kirschner-wires are withdrawn from the acetabular fragment (but kept within the stable iliac wing) and the acetabular orientation can be adjusted to a better position.
If a satisfactory correction is achieved and confirmed on radiographic and impingement testing, definitive fixation can be performed. Routine adequate fixation adequate can be achieved by placing multiple screws (3.5 mm or 4.5 mm) through the iliac crest and into the acetabular fragment. Classically, an additional AP screw, for improved rotatory stabilization, is placed from the anterior-inferior spine area across the ilium into the posterior ilium beyond the posterior column osteotomy. We employ this extra screw in large patients and in patients with poor bone stock or poor bone quality.
Stability of the reconstruction must be critically assessed. Ideally, there is impaction of the posterosuperior corner of the acetabular fragment into the iliac osteotomy site, and there is direct contact at the superior ramus osteotomy. Protruding edges are trimmed to reduce soft-tissue irritation, with the harvested bone graft subsequently packed into the interstices of the osteotomies. Hemostasis is usually satisfied at this point in the procedure, though moderate bleeding may occur from osteotomy surfaces while the fragment is being manipulated.
Soft-tissue closure must be secure, since early postoperative function is desirable. Careful attention to the soft tissues during exposure facilitates healing of not only soft tissues but of the underlying bone.
Postoperative care
After approximately 24 hours of regional blockade by constant infusion into the lumbar plexus catheter, patients typically sit in a chair. By postoperative day 2, they are encouraged to begin a partial weight-bearing gait with crutches. Antithrombotic prophylaxis with low-dose aspirin is started the morning of post-operative day 1 and continued for four weeks. Prophylaxis against heterotopic ossification is done with naproxen, which is also used for four weeks. Discharge from hospital usually occurs by the fourth postoperative day. Resumption of full weight-bearing follows recovery of necessary muscle function and evidence of adequate osteotomy healing as confirmed by AP and faux profil radiographs (Fig. 4). This typically occurs eight to 12 weeks postoperatively, dependent on patient age and degree of correction required. Routine radiographs are taken at monthly intervals until complete osteotomy healing. Patients are followed annually with clinical examinations and radiographs, or more frequently if required. Full activity, including sport, is resumed according to individualized protocols, though in general, at least six to 12 months is required before full return of maximum achievable function has taken place.13,14
Fig. 4.
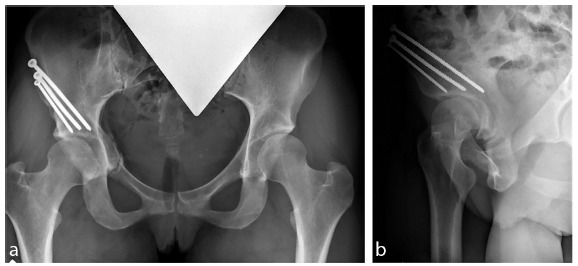
Postoperative images of same 28-year-old woman confirm maintenance of correction and near-complete radiographic healing at four months postoperatively. She was clinically healed. She had discontinued crutch use at three months and was symptom-free. Left periacetabular osteotomy planned: (a) anteroposterior view confirms healing and correction. There is no crossover sign. Lateral centre-edge (CE) angle measures 25° (normal is about 25° to 35°). Roof angle is 4° (normal is about 0° to 10°). Shenton’s line is intact; (b) faux profil view reveals anterior CE angle is 28° (normal is about 20° to 35°).
Complications
PAO is a major complex procedure with a steep learning curve. Potential complications are many and have been well documented. The multicentre Academic Network for Conservational Hip Preservation Outcomes Research (ANCHOR) Group documented a 15% complication rate within the first ten weeks following surgery.15 In all, 77% of these early complications were self-resolving or required minimal intervention. The most common complications in this group included lateral femoral cutaneous nerve (LFCN) neurapraxia (4%) and wound-related issues (5%). Seven patients (3%) had a moderate/severe complication requiring early repeat operation or significant medical intervention. Reoperation was performed for two deep infections (1%) and one case of acetabular fragment migration (0.5%). Serious medical conditions included deep venous thrombosis in three patients (1.5%) treated pharmacologically. Another study focusing on thromboembolic events following PAO documented a risk of 9.4 per 1000 surgeries.16
Delayed complications (more than one year postoperative) were noted in 24% of patients, and most (86%) did not require intervention.15 The most common complications included heterotopic ossification (Booker grade I to IV) in 20% of patients, one of which underwent surgical resection. Nonunion of the pubic ramus, stress fracture of the ischium and nonunion of the posterior column were encountered in one patient each, and only the posterior column nonunion required surgical intervention. Moderate to severe complications were noted in five patients, all of whom required repeat surgical intervention for: heterotopic ossification (above), posterior column nonunion (above), removal of intra-articular screws (two patients) and acetabular migration (one patient).
Sierra et al17 reported that significant nerve injuries were encountered in approximately 2% of PAOs and that half of these injuries recovered function with time. While devastating neurovascular complications were not noted in the multicentre experience, they remain among the most feared complications of PAO. Kalhor et al18 has nicely outlined intraoperative techniques useful in reducing the risk of neurovascular complication. Various exposure techniques and positioning of the operative limb during surgery can enhance exposure and reduce risk to neurovascular structures.
Results
PAO has a well-documented record of success in the treatment of acetabular dysplasia in skeletally mature individuals. The Bernese experience has provided the longest follow-up to date at 30 years. The conversion rate to total hip arthroplasty or arthrodesis was 12.4% at ten years, 39.5% at 20 years.19,20 At 30-year follow-up, 30% of hips were asymptomatic without radiographic evidence of progression.21 Similarly, results from our centre showed cumulative survival of 76% at ten-year follow-up and 74% at mean 18-year follow-up.22 Our interest in the character of the result in surviving hips noted, at mean 18 years after PAO, that 53% of patients were asymptomatic, and 26% were symptomatic based on Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain score > 10. In all, 21% of hips had been replaced at a mean of nine years (sd 5) post-PAO. Troelsen et al23 described similar results from another high-volume PAO centre, with 82% of hips surviving for a decade following surgery, respectively. The multicentre ANCHOR early prospective results of 391 consecutive PAOs at two to five years postoperatively showed a 99.2% hip survival rate and 93% early satisfaction rate.24
While the overall results among these studies were consistent, the characteristics of failed PAOs were also highly similar. Older patients, patients with severe preoperative dysfunction, radiographic osteoarthritis and poor joint congruency prior to surgery were strong predictors of PAO failure in a number of studies.21,22,25 Operative causes of failure include malpositioning of the acetabulum into positions of under-coverage (instability), over-coverage (impingement) or retroversion.19,21,22,25,26 Femoral-sided asphericity was a risk factor for PAO failure, but successful osteochondroplasty was protective of PAO outcome in those patients.25 Interestingly, in patients with spherical, congruous articulations and without evidence of preoperative arthritis had a > 75% chance of progressing 20 years without symptoms or radiographic progression of osteoarthritis.20
Conclusions
Acetabular dysplasia is a common cause of hip dysfunction in the young mature patient and has often led in the past to osteoarthritis in adults. PAO, when performed on well-indicated patients in a technically sound manner, can greatly improve the function and longevity of at-risk hips. If careful clinical evaluation is combined with rational treatment selection and excellent technique, PAO can be a very effective procedure in helping the symptomatic pre-arthritic young patient with congruous acetabular dysplasia.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA Licence Text
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) license (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Ethical statement
Ethical approval: Institutional Review Board approval has been received for our PAO patient studies over last 12 years.
Informed Consent: Not required for this work.
ICMJE Conflict of interest statement
MB Millis receives editorial royalties from Elsevier. All other authors have no interest of conflict to declare.
References
- 1.Salter RB. Role of innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip in the older child. J Bone Joint Surg [Am] 1966;48-A:1413–1439. [PubMed] [Google Scholar]
- 2.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res 1988;232:26–36. [PubMed] [Google Scholar]
- 3.Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res 1999;364:92–98. [DOI] [PubMed] [Google Scholar]
- 4.Novais EN, Kim YJ, Carry PM, Millis MB. The Bernese periacetabular osteotomy: is transection of the rectus femoris tendon essential? Clin Orthop Relat Res 2014;472:3142–3149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beck M, Leunig M, Ellis T, Sledge JB, Ganz R. The acetabular blood supply: implications for periacetabular osteotomies. Surg Radiol Anat 2003;25:361–367. [DOI] [PubMed] [Google Scholar]
- 6.Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg [Am] 1995;77-A:985–989. [DOI] [PubMed] [Google Scholar]
- 7.Thomas GE, Palmer AJ, Batra RN, et al. Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women. A 20 year longitudinal cohort study. Osteoarthritis Cartilage 2014;22:1504–1510. [DOI] [PubMed] [Google Scholar]
- 8.Clohisy JC, Carlisle JC, Beaulé PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg [Am] 2008;90-A:47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nepple JJ, Wells J, Ross JR, et al. Three patterns of acetabular deficiency are common in young adult patients with acetabular dysplasia. Clin Orthop Relat Res 2017;475:1037–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilkin GP, Ibrahim MM, Smit KM, Beaulé PE. A contemporary definition of hip dysplasia and structural instability: toward a comprehensive classification for acetabular dysplasia. J Arthroplasty 2017;32:S20–S27. [DOI] [PubMed] [Google Scholar]
- 11.Cunningham T, Jessel R, Zurakowski D, Millis MB, Kim YJ. Delayed gadolinium-enhanced magnetic resonance imaging of cartilage to predict early failure of Bernese periacetabular osteotomy for hip dysplasia. J Bone Joint Surg [Am] 2006;88-A:1540–1548. [DOI] [PubMed] [Google Scholar]
- 12.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome: surgical technique. J Bone Joint Surg [Am] 2010;92-A:115–129. [DOI] [PubMed] [Google Scholar]
- 13.Heyworth BE, Novais EN, Murray K, et al. Return to play after periacetabular osteotomy for treatment of acetabular dysplasia in adolescent and young adult athletes. Am J Sports Med 2016;44:1573–1581. [DOI] [PubMed] [Google Scholar]
- 14.Klit J, Hartig-Andreasen C, Jacobsen S, Søballe K, Troelsen A. Periacetabular osteotomy: sporting, social and sexual activity 9–12 years post surgery. Hip Int 2014;24:27–31. [DOI] [PubMed] [Google Scholar]
- 15.Zaltz I, Baca G, Kim YJ, et al. Complications associated with the periacetabular osteotomy: a prospective multicenter study. J Bone Joint Surg [Am] 2014;96:1967–1974. [DOI] [PubMed] [Google Scholar]
- 16.Zaltz I, Beaulé P, Clohisy J, et al. Incidence of deep vein thrombosis and pulmonary embolus following periacetabular osteotomy. J Bone Joint Surg [Am] 2011;93-A:62–65. [DOI] [PubMed] [Google Scholar]
- 17.Sierra RJ, Beaule P, Zaltz I, et al. Prevention of nerve injury after periacetabular osteotomy. Clin Orthop Relat Res 2012;470:2209–2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kalhor M, Gharehdaghi J, Schoeniger R, Ganz R. Reducing the risk of nerve injury during Bernese periacetabular osteotomy: a cadaveric study. Bone Joint J 2015;97-B:636–641. [DOI] [PubMed] [Google Scholar]
- 19.Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res 2013;471:1602–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res 2008;466:1633–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lerch TD, Steppacher SD, Liechti EF, Tannast M, Siebenrock KA. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res 2017;475:1154–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wells J, Millis M, Kim YJ, et al. Survivorship of the Bernese periacetabular osteotomy: what factors are associated with long-term failure? Clin Orthop Relat Res 2017;475:396–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Troelsen A, Elmengaard B, Søballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg [Am] 2009;91-A:2169–2179. [DOI] [PubMed] [Google Scholar]
- 24.Clohisy JC, Ackerman J, Baca G, et al. Patient-reported outcomes of periacetabular osteotomy from the prospective ANCHOR cohort study. J Bone Joint Surg [Am] 2017;99:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wells J, Schoenecker P, Duncan S, et al. Intermediate-term hip survivorship and patient-reported outcomes of periacetabular osteotomy: the Washington University experience. J Bone Joint Surg [Am] 2018;100:218–225. [DOI] [PubMed] [Google Scholar]
- 26.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg [Am] 2009;91-A:2113–2123. [DOI] [PubMed] [Google Scholar]


