Abstract.
We investigated the in vitro activity of a novel fifth-generation cephalosporin–tazobactam combination, ceftolozane–tazobactam against Burkholderia pseudomallei, the etiological agent of melioidosis. Using both disc diffusion and minimum inhibitory concentration (MIC) strip techniques against 56 clinical isolates and an national collection of type cultures (NCTC) strain, the MIC to ceftolozane–tazobactam was found to be between 0.75 and 4 mcg/mL. The MIC50 was found to be 1.5 mcg/mL and MIC90 was 2.0 mcg/mL. This study provides initial evidence of ceftolozane–tazobactam as a novel agent in the management of melioidosis.
Burkholderia pseudomallei, the etiological agent of meloidosis, is a Gram-negative bacterium that is endemic to tropical regions including Southeast Asia and Northern Australia. It can cause a spectrum of disease ranging from acute pneumonia and septicemia through to an indolent presentation such as osteomyelitis. In addition, there can be reactivation of latent disease which can occur many decades after potential exposure.1,2
Treatment of B. pseudomallei is difficult because of resistance to narrow-spectrum penicillins, first- and second-generation cephalosporins, and aminoglycosides, notably gentamicin and tobramycin.3 Antimicrobial agents that have been successfully used in the acute treatment of B. pseudomallei include carbapenems (meropenem and imipenem) and ceftazidime.4
A novel cephalosporin/beta-lactamase inhibitor combination, ceftolozane–tazobactam, has been released to the market. This was developed primarily for the treatment of multiresistant Pseudomonas aeruginosa and extended-spectrum beta-lactamase–producing Enterobacteriaceae. It is an intravenous dosed drug that has been shown in non-inferiority trials to have similar efficacy as meropenem in complicated intra-abdominal infections and levofloxacin in urinary tract infections.5,6
In this study, we seek to elucidate the in vitro activity of ceftolozane–tazobactam against B. pseudomallei by determining the minimum inhibitory concentration (MIC) for a library of clinical isolates and comparing this with disc diffusion testing.
A total of 56 clinical isolates were taken from a historical collection of B. pseudomallei isolates stored by the microbiology department of the Townsville Hospital, Queensland, Australia. Isolates were from patients who acquired the disease in North Queensland, the Northern Territory, and Papua New Guinea and NCTC strain 13178.
The isolates were recovered from −70°C storage and grown on blood agar for 24 hours in an ambient environment at 35°C. The isolates were then subcultured for purity; identification of the isolates was performed using the VITEK 2 ID GNB card system (Biomerieux, Inc., Hazelwood, MO) before susceptibility testing. Minimum inhibitory concentrations were determined using the MIC test strip technique (Liofilchem, Roseto degli Abruzzi, Italy). Each strip contained a concentration gradient of ceftolozane with a fixed concentration of tazobactam (4 mcg/mL) which when used as per the manufacturer’s instructions could determine an MIC between 0.016 and 256 mcg/mL.
Isolated colonies were suspended in 0.85% saline achieving a 0.5 McFarland standard turbidity as measured using a DensiChek instrument (bioMérieux, Inc., Hazelwood, MO). This was then swabbed to form a lawn on Mueller Hinton agar (bioMérieux) and the strips applied to the agar. The plates were then incubated in an inverted position at 35°C for 20 hours in an ambient environment. Interpretation of the strip MIC was performed as per the manufacturer’s instructions. Disc diffusion testing was performed using 30 mcg ceftolozane/10 mcg tazobactam discs (Mastdisc; Mastgroup, Merseyside, United Kingdom) on Mueller Hinton agar incubated at 35°C for 20 hours in an ambient environment. The disc diffusion testing and zone size interpretation were performed in accordance with the European committee on antimicrobial susceptibility testing (EUCAST) methodology. Escherichia coli (ATCC 25922), Staphylococcus aureus (ATCC 29213), and P. aeruginosa (ATCC 27853) were used as quality control isolates.
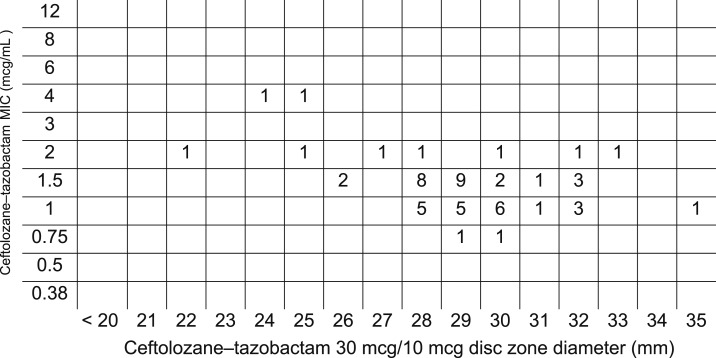
The three quality control strains demonstrated acceptable MIC results within the ranges outlined by the manufacturer of ceftolozane–tazobactam and the MIC test strips.7 An MIC and disk diffusion diameter was determined for each isolate and no contamination occurred. The range of MIC to ceftolozane–tazobactam was between 0.75 and 4 mcg/mL. The MIC50 and MIC90 values for ceftolozane–tazobactam were 1.5 and 2.0 mcg/mL, respectively (Figure 1).
Figure 1.
Disc diffusion zone sizes plotted against the minimum inhibitory concentration (MIC) strip of ceftolozane combined with a fixed concentration of tazobactam.
The results of this preliminary study demonstrate that the novel cephalosporin/beta-lactamase combination ceftolozane–tazobactam has in vitro activity against B. pseudomallei isolates. All of the isolates tested were found to have an MIC of ≤ 4 mcg/mL. Recently EUCAST has published the ceftolozane–tazobactam MIC breakpoints for P. aeruginosa as > 4 mcg/mL on the basis of pharmacokinetic/pharmacodynamic (PK/PD) modeling.8 This breakpoint was supported by the Food and Drug Administration (FDA) in the registration of ceftolozane–tazobactam at a dose of 1.5 g every 8 hours.7 As ceftolozane has structural similarities to ceftazidime, it is possible that a similar breakpoint might apply for B. pseudomallei which has a Clinical and Laboratory Standards Institute (CCSI) breakpoint to ceftazidime of 8 mcg/mL. However, without having a PK/PD target for B. pseudomallei, these MICs cannot be interpreted with any certainty.
There are several limitations to this study. Ceftolozane could not be tested in the absence of tazobactam; therefore, the contribution of activity against B. pseudomallei could not be attributed solely to the active agent. Second, there have been no time-kill studies or animal experimental studies performed to determine the activity of ceftolozane–tazobactam against B. pseudomallei. Last, the relationship between in vitro studies and in vivo clinical success is not clear because of the complex nature of infections.
In conclusion, this study provides evidence of in vitro susceptibility of B. pseudomallei against a novel cephalosporin/beta-lactamase inhibitor. However, further studies are required to confirm that these initial findings translate into clinical outcomes.
Disclaimer: The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
REFERENCES
- 1.Cheng AC, Currie BJ, 2005. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev 18: 383–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.White NJ, 2003. Melioidosis. Lancet 361: 1715–1722. [DOI] [PubMed] [Google Scholar]
- 3.Schweizer HP, 2012. Mechanisms of antibiotic resistance in Burkholderia pseudomallei: implications for treatment of melioidosis. Future Microbiol 7: 1389–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng AC, 2010. Melioidosis: advances in diagnosis and treatment. Curr Opin Infect Dis 23: 554–559. [DOI] [PubMed] [Google Scholar]
- 5.Huntington JA, Sakoulas G, Umeh O, Cloutier DJ, Steenbergen JN, Bliss C, Goldstein EJ, 2016. Efficacy of ceftolozane/tazobactam versus levofloxacin in the treatment of complicated urinary tract infections (cUTIs) caused by levofloxacin-resistant pathogens: results from the ASPECT-cUTI trial. J Antimicrob Chemother 71: 2014–2021. [DOI] [PubMed] [Google Scholar]
- 6.Solomkin J, et al. 2015. Ceftolozane/tazobactam plus metronidazole for complicated intra-abdominal infections in an era of multidrug resistance: results from a randomized, double-blind, phase 3 trial (ASPECT-cIAI). Clin Infect Dis 60: 1462–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.FDA , 2014. Prescribing Information—Ceftolozane/Tazobactam Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/206829lbl.pdf. Accessed January 16, 2018.
- 8.EUCAST , 2017. Addendum on Ceftolozane-Tazobactam Zone Diameter Breakpoints for Pseudomonas aeruginosa. Available at: http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/Addenda/Addendum_June_2017_ceftolozane-tazobactam.pdf. Accessed August 28, 2017.