Abstract
Delayed-onset muscle soreness (DOMS), an ultrastructural muscle injury, is one of the most common reasons for impaired muscle performance. The purpose of this study was to investigate the influence of sport compression garments on the development of exercise-induced intramuscular edema in the context of DOMS. DOMS was induced in 15 healthy participants. The participants performed a standardized eccentric exercise of the calf muscles. Magnetic resonance imaging (MRI) was performed at baseline and 60h after exercise (T2-weighted signal intensity and T2 relaxation time was evaluated in each compartment and the intramuscular edema in the medial head of the gastrocnemius muscle was segmented). After the exercise, a conventional compression garment (18-21 mmHg) was placed on one randomized calf for 60h. The level of muscle soreness was evaluated using a visual analogue pain scale. T2-weighted signal intensity, T2 relaxation time and intramuscular edema showed a significant interaction for time with increased signal intensities/intramuscular edema in the medial head of the gastrocnemius muscle at follow-up compared to baseline. No significant main effect for compression or interaction between time and limb occurred. Further, no significant differences in the soleus muscle and the lateral head of the gastrocnemius muscle were noted between limbs or over time. After exercise, there was significantly increased muscle soreness in both lower legs in resting condition and when going downstairs and a decreased range of motion in the ankle joint. No significant difference was observed between the compressed and the non-compressed calf. Our results indicate that wearing conventional compression garments after DOMS has been induced has no significant effect on the development of muscle edema, muscle soreness, range of motion and calf circumference.
Key points.
MRI can be used for a reliable evaluation of DOMS.
Compression garments (class I) have no significant effect on muscle edema in DOMS
Compression garments (class I) have no significant effect on muscle soreness, calf circumference and range of motion in DOMS
Key words: Muscle injury, MRI, T2 mapping, T2-weighted imaging, eccentric training
Introduction
Muscle injuries are one of the most common sports injuries, presenting an incidence of 10-55% of all injuries (Best and Hunter, 2000; Huard et al., 2002; Jarvinen et al., 2005). Delayed-onset muscle soreness (DOMS), an entity of ultrastructural muscle injury, is classified as an overexertion-functional muscle disorder type Ib according to the Munich Consensus Statement (Mueller-Wohlfahrt et al., 2013). DOMS is caused by high eccentric muscle contractions or unaccustomed exercises (Armstrong, 1984). Biopsy analysis of muscle has revealed that eccentric training causes Z-band streaming and broadening and destroys sarcomeres in the myofibrils (Friden et al., 1983), which leads to myofiber necrosis and inflammation (Paulsen et al., 2012).
DOMS is one of the most common reasons for impaired muscle performance in sports and is associated with muscle soreness, reduced muscle strength, and range of motion, and is frequently observed both in professional and recreational athletes (Kim and Kim, 2014; Mizuno et al., 2016; Pearcey et al., 2015). The signs and symptoms begin 6-12 h after exercise, increase progressively until they reach peak pain at 48-72 h, and decrease until they disappear 5-7 days later (Valle et al., 2013).
Lower limb compression garments are increasingly popular among athletes who wish to improve performance and to reduce exercise-induced discomfort and injury risk (Beliard et al., 2015). Furthermore, compression stockings have wide, evidence-based application for treating clinical pathologies such as deep vein thrombosis and chronic venous insufficiency (Ibegbuna et al., 2003; Scurr et al., 2001).
The impact of compression therapy during exercise or during recovery and its clinical outcome regarding DOMS is a subject of controversy (Beliard et al., 2015; Goto et al., 2017; Hill et al., 2014). Most results suggesting that compression garments are effective in enhancing recovery of muscle damage, whereas no clear relation between regeneration and applied pressure or wear time are known and underlying mechanisms are poorly understood (Beliard et al., 2015; Hill et al., 2014; Marques-Jimenez et al., 2016).
T2-weighted magnetic resonance images are frequently utilized for detecting muscle damage resulting from repeated eccentric muscle contraction (Nosaka and Clarkson, 1996; Valle et al., 2013; Yanagisawa et al., 2015). Increased T2-weighted signal intensity indicates intramuscular fluid accumulation, which shows good correlation to the degree of ultrastructural damage in the context of DOMS and suggests the use of MRI for the quantitative assessment of exercise-induced muscle damage (Nurenberg et al., 1992; Yanagisawa et al., 2015).
To our knowledge, no one has proven the somewhat speculative concept that applying compression attenuates changes in osmotic pressure and reduces venous blood pooling, the space available for swelling, hemorrhage, or hematoma formation after exercise-induced muscle damage (Duffield et al., 2014; Kraemer WJ, 2004). Hence, the purpose of this study was to investigate the influence of commercially available sport compression garments on the development of exercise-induced intramuscular edema in the context of DOMS. We hypothesized that wearing compression garments during recovery reduces intramuscular edema caused by disruption of the muscle fiber structure during eccentric training by reducing the available space for swelling.
Methods
Ethical approval
The local ethics committee approved the performance of the present study with no requirements (Friedrich-Alexander-University (FAU) Erlangen-Nuremberg, Erlangen, Germany). All participants were informed of the benefits and risks of the investigation prior to signing an institutionally approved informed consent document to participate in the study.
Study population
Fifteen healthy volunteers (7 female; 8 male; age, 25 ± 6 years; height, 1.79 ± 0.11 m; body weight, 69 ± 12 kg) from the medical and sports faculties were recruited as participants. No participant had signs, symptoms, or history of chronic diseases and no current acute or overuse lower limb injuries or muscle injuries in their history. No participant had lower limb malalignment, and all participants presented full ranges of motion for the hip, knee, and ankle joints. The participants were advised to avoid any sports activities for 1 week prior to the investigation date. Exclusion criteria were any symptoms of lower limb muscle soreness 3 months prior to the study and regular training habits, including eccentric or plyometric exercises. All participants trained regularly in recreational sports, including swimming, triathlon, soccer, running, boxing, and lacrosse. The average training frequency of the participants corresponded to grade 3 of the Valderrabano Sport Scale (2.6 ± 0.4) with more than 5 training hours per week (Valderrabano et al., 2006).
Standardized eccentric exercise of the calf muscles
To induce DOMS, the participants performed a standardized, established eccentric calf muscle exercise (Hotfiel et al., 2017; Kellermann et al., 2017). During the whole exercise the participants were instructed and motivated by a licensed fitness coach.
Each participant warmed-up using two sets of heel raises of 15 repetitions, with one 20-sec break between the sets. Immediately after the warm-up, the eccentric exercise was performed on a specifically manufactured stair (Figure 1). It started with the participants raising their heels, maximally contracting the calf muscle (Figure 1A) for 1 sec and then putting the heels down slowly within 3 sec until the soles touched a -35° slant plate (Figure 1B). To return to the starting position (heels raised) and to relieve the calf muscle during concentric contraction, the participants pulled themselves up on a pull-up bar installed above their heads to focus on eccentric contraction (Figure 1C). To increase the load, each subject wore a weighted vest bearing approximately 25% of their body weight during the whole exercise. All participants performed 5 sets of 30 repetitions and rested 10 sec between each set, whereby the last set was performed until muscle fatigue, so that no further repetition of eccentric exercise was possible.
Figure 1.

Procedure of the standardized eccentric exercise of the calf muscles: (A) start position (heel raised), (B) eccentric contraction (-35°), (C) composites of the whole setting.
Compression therapy
Immediately after standardized eccentric exercise, a conventional sports compression garment, compression class I (Compression Sock Run & Walk, 18-21 mmHg, 97% polyamide, 7% elastane, Bauerfeind AG, Zeulenroda-Triebes, Germany) was placed according to the manufacturer’s instructions on one randomized calf (Figure 2). The compression sock was worn continuously for 60 h after eccentric exercise and was removed for the first time for follow-up examination.
Figure 2.

Compression therapy of one randomized calf with a conventional compression sock (class 1, 18 – 21 mmHg) for 60 h after standardized eccentric exercise of the calf muscles.
Creatine kinase (CK) levels
Blood CK levels were measured at baseline and 60 h after the eccentric exercise. Approximately 5 mL blood was collected by vein puncture from an antecubital vein into serum tubes. CK measurement was conducted using the UV test according to the IFCC method (37°C) (Cobas 6000, Roche Diagnostics, Mannheim, Germany).
Muscle soreness assessment
The level of muscle soreness was evaluated using a pain scale (Mundipharma GmbH, Limburg, Germany) that displays a visual analogue scale (VAS) of 100 mm on the front (0, no pain; 100, worst pain) and a numerical rating scale (NRS) on the back. Muscle soreness was assessed at baseline and 60 h after the exercise. The participants were asked to mark their soreness at rest and during activity (going downstairs).
Range of motion (ROM)
The range of motion of both ankle joints was assessed manually with a goniometer. Representative was the maximal passive dorsiflexion at baseline and at post-intervention, while the participant was sitting off the edge of table with free hanging lower legs. The center of the goniometer was positioned on the lateral malleolus with one side horizontal next to the calf and the other side parallel to the lateral foot and being adjusted in accordance to the ability of motion. All measurements of the ROM were performed by the same orthopedic surgeon (T.H.) (Hotfiel et al., 2017; Kellermann et al., 2017).
Calf circumference
The maximum calf circumference was measured using a tape measure while the participant was sitting off the edge of table with free hanging lower legs. The location of measurement was labeled with a permanent marker at baseline to ensure the same location was measured at follow-up. All measurements of the calf circumference were performed by the same orthopedic surgeon (T.H.) (Hotfiel et al., 2017; Kellermann et al., 2017).
Magnetic resonance imaging
MRI was performed at baseline and 60 h after standardized eccentric exercise. No MRI contraindications were stated for any participant.
Imaging of both lower legs was carried out simultaneously at the Department of Radiology of the University Hospital Erlangen (Germany) with a 3T MRI scanner (Magnetom Skyra Fit 3T, Siemens Healthineers, Erlangen, Germany) using a dedicated 32-channel spine coil and an 18-channel body coil (Siemens Healthineers).
An axial T2 mapping sequence (total acquisition time, 9:05 min; echo time, ranging from 10.64 to 190.8 ms; repetition time, 3000 ms; resolution, 0.7 × 0.7 × 8.0 mm), an axial T2-weighted turbo inversion recovery magnitude (TIRM) sequence (total acquisition time, 3:31 min; inversion time, 260 ms; echo time, 69 ms; repetition time, 5120 ms; flip angle, 145°; resolution, 0.8 × 0.8 × 4.0 mm), and a coronal T2-weighted TIRM sequence (total acquisition time, 3:42 min; inversion time, 260 ms; echo time, 68 ms; repetition time, 5120 ms; flip angle, 180°; resolution, 0.9 × 0.9 × 4.0 mm) were applied to the lower leg. Additionally, we performed a T1-weighted turbo spin-echo (TSE) sequence (total acquisition time, 3:01 min; echo time, 14 ms; repetition time, 582 ms; resolution, 0.7 × 0.7 × 5.0 mm) to depict the anatomy and morphology of the lower leg.
Image analysis
The MRI data were blinded and analyzed by an experienced radiologist. Image analysis was performed using a professional image processing program (syngo.via VB10, Siemens Healthineers). The compartments of the lower leg were determined by defining specific regions of interest (ROIs) in the axial T1-weighted sequence images according to the anatomic margin of each muscle [medial gastrocnemius muscle (MGM), lateral gastrocnemius muscle (LGM), soleus muscle (SM)] and copying them over the T2-weighted TIRM and T2-mapping sequence images. Analysis of the axial MR images was performed at the maximum circumference of the proximal lower leg, which was marked with permanent markers and specific MRI markers during the whole trial to get identical slice positions.
The test-retest reliability was evaluated by the same reader four months after the initial assessment by analyzing data sets of five randomly chosen volunteers. The results of the first investigation and the MRI data were blinded.
The signal intensities of the T2-weighted TIRM ROIs of the MGM, LGM, and SM were normalized to the mean values of an agarose-containing tube (40 mmol/L NaCl and 5% agarose) that had been placed between the lower legs. Further, the pre-exercise, normalized signal intensity of the MGM, LGM, and SM was defined as 1.0.
For calculating the volume of post-exercise intramuscular edema in the MGM, the expected post-exercise T2-weighted TIRM signal intensities of the MGM were calculated using the rule of three [expected signal intensity post-exercise MGM = (signal intensity pre-exercise MGM × signal intensity of agarose post-exercise)/signal intensity of agarose pre-exercise].
The threshold of intramuscular edema was defined as the sum of expected post-exercise T2-weighted TIRM signal intensity and the five-fold standard deviation. This threshold was used to determine the volume of edematous muscle via manual segmentation in the post-exercise coronal T2-weighted TIRM images, which covered the whole lower leg of every volunteer. Hyperintense vessels were segmented in the baseline images and subtracted from the segmented volume in the post-exercise images (Figure 4). Commercially available software was used for the segmentation (Chimaera GmbH, Erlangen, Germany).
Figure 4.
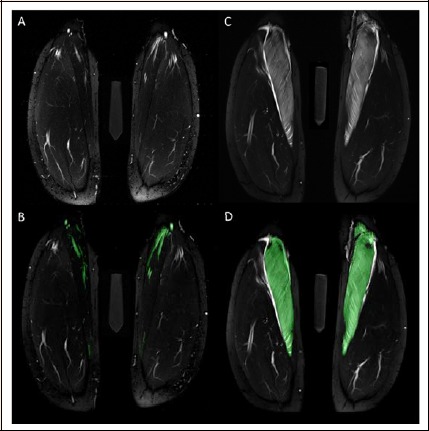
Volume of edematous muscle was assessed in the T2-weighted TIRM images acquired 60 h after standardized eccentric exercise of the calf muscles (C, D). Exemplary images before (C) and after color-coded manual segmentation (D) of the edematous medial gastrocnemius muscle are shown. Hyperintense vessels were segmented in the baseline images (B) and subtracted from the segmented volume in the post-exercise images (D).
For grading of the exercise-induced muscle damage, a modification of the Peetrons classification was used: grade 0 indicated a negative MRI without any visible pathology, grade I represented edema but no architectural disorganization, grade II indicated architectural disruption indicating partial tear, and grade III indicated total muscle rupture (Peetrons, 2002). An induced DOMS was considered for all subjects with grade I lesions.
Statistical analysis
A 2-way, 2 repeated measures ANOVA with time (baseline vs. follow-up) and treatment (compression vs. non-compression) as the repeated independent variables was performed for each of the dependent variables of interest: T2-weighted TIRM signal intensity, T2 relaxation time [ms], volume of intramuscular edema [mL], calf circumference and range of motion of the ankle joint (dorsiflexion). The Benjamini-Hochberg method was used to calculate the False Discovery Rate (FDR) and correct for multiple comparisons. Statistical tests resulting in p < 0.05 were considered significant with an FDR cutoff of α = 0.2 (Glickman et al., 2014). Intraobserver reliability was evaluated by using intraclass correlation coefficient (ICC). Muscle soreness scores were analyzed with the Wilcoxon signed-rank test. CK activity values were checked for normality with the Shapiro-Wilk test. In case of normality, the paired t-test was used to compare data from baseline to follow-up; otherwise, the Wilcoxon signed-rank test was used. All statistical tests were performed using SPSS version 21 (Chicago, IL, USA) and P-values of <0.05 indicated statistical significance.
Results
Muscle edema
The MRI examination of all 15 participants was of satisfactory quality. There were no notable motion artifacts.
At baseline, the MRI investigations revealed no anatomical disorders or signs of acute or overuse injuries in all participants. We were unable to detect any signs of intramuscular edema in any compartment of the triceps surae muscle under physiological conditions.
Sixty hours after the exercise, all subjects presented grade I lesions in the MGM according to the modified Peetrons classification. No subject had signs of LGM or SM intramuscular edema (Figure 3).
Figure 3.
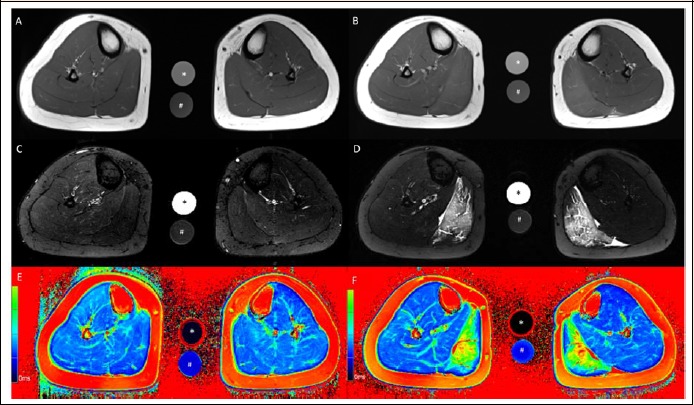
Axial T1-weighted (A, B), axial T2-weighted TIRM (C, D) and axial T2 mapping (E, F) images of the lower leg at baseline (A, C, E) and 60 h after standardized eccentric exercise of the calf muscles (B, D, F). Muscle edema is apparent in the medial gastrocnemius muscle in the post-exercise images (B, D, F). This participant wore the compression sock on the left calf for 60 h after eccentric exercise. The calibration tubes contain 40 mmol/L NaCl (*) and 40 mmol/L NaCl 5% agarose (#).
For normalized T2-weighted TIRM signal intensity, there was no statistical interaction (p = 0.83) or treatment main effect (p = 0.67); however, there was a main effect for time, with a signal intensity at follow-up (2.0 ± 1.1) being significantly higher (p = 0.002) than at baseline (1.0 ± 0.2). For T2 relaxation time there was no statistical interaction (p = 0.96) or treatment main effect (p = 0.95); however, there was a main effect for time (p = 0.005), with T2 relaxation time at follow-up (54.6 ± 19.3 ms) being significantly higher than baseline (37.7 ± 3.2 ms) (Figure 3). No effect of time or treatment was present for the T2-weighted signal intensity or T2 relaxation time of the LGM and SM (Table 1).
Table 1.
Post-exercise muscle edema in the compressed and the non-compressed calf.
| Compressed calf | Non-compressed calf | p-value of ANOVA | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre-exercise | Post-exercise | Pre-exercise | Post-exercise | Time | Treatment | Time*Treatment | ||
| Signal intensity (T2-weighted TIRM sequence) | MGM | 1.0 ± 0.3 | 1.9 ± 1.1 | 1.0 ± 0.2 | 2.1 ± 1.1 | 0.002 | 0.674 | 0.829 |
| LGM | 1.0 ± 0.3 | 1.00 ± 0.1 | 1.0 ± 0.3 | 1.1 ± 0.5 | 0.060 | 0.580 | 0.179 | |
| SM | 1.0 ± 0.3 | 0.9 ± 0.3 | 1.0 ± 0.3 | 0.9 ± 0.2 | 0.231 | 0.753 | 0.914 | |
| T2 relaxation time [ms] | MGM | 37.4 ± 9.6 | 54.5 ± 12.3 | 38.1 ± 9.2 | 54.6 ± 14.1 | 0.005 | 0.951 | 0.956 |
| LGM | 38.4 ± 8.1 | 39.7 ± 8.7 | 37.4 ± 7.6 | 41.1 ± 8.3 | 0.165 | 0.884 | 0.244 | |
| SM | 39.9 ± 6.1 | 44.0 ± 8.4 | 39.7 ± 6.0 | 40.5 ± 6.2 | 0.260 | 0.340 | 0.370 | |
Relative values of T2-weighted TIRM signal intensity and absolute T2 relaxation time [ms] (mean ± SD) in the medial gastrocnemius muscle (MGM), the lateral gastrocnemius muscle (LGM) and the soleus muscle (SM) of the compressed and the non-compressed calf at baseline and 60 h after standardized eccentric exercise. P-values of the performed 2-way, 2 repeated measures ANOVA (analysis of variance) with time (baseline vs. post-intervention), treatment (compression vs. non-compression) and the interaction of time and treatment are given
For intramuscular edema in the MGM there was no statistical interaction (p = 0.87) or treatment main effect (p= 0.73); however, there was a main effect for time (p = 0.005), with a intramuscular edema at follow-up (104.6 ± 98,4 mL) being significantly larger than baseline (7.2 ± 5.6 mL). An example is shown in Figure 4.
The ICC for the test-retest reliability were 0.85 for the normalized T2-weighted TIRM signal intensity and 0.88 for the T2 relaxation time in the MGM at the maximum circumference of the proximal lower. The ICC for the segmentation of intramuscular edema in coronal T2-weighted TIRM images was calculated with 0.92. Intraobserver variability for the two different measurement time points was low, as the ICC indicate a good (ICC > 0.75) and partly even excellent (ICC > 0.9) reliability (Koo and Li, 2016).
Muscle soreness
The examination performed 60 h after the exercise revealed significantly increased muscle soreness in both lower legs in resting condition (compression: 0 ± 0 vs. 1.5 ± 1.2, p = 0.001; non-compression: 0 ± 0 vs. 1.5 ± 1.4, p = 0.004) and when going downstairs (compression: 0 ± 0 vs. 5.6 ± 1.6, p < 0.001; non-compression: 0 ± 0 vs. 5.3 ± 1.9, p < 0.001). Furthermore, no difference in muscle soreness was observed between the compressed and non-compressed calf in resting condition post-exercise (1.5 ± 1.2 vs. 1.5 ± 1.4, p = 0.467) and during activity (5.6 ± 1.6 vs. 5.3 ± 1.9, p = 0.233) (Table 2).
Table 2.
Post-exercise muscle soreness in the compressed and the non-compressed calf using a visual analogue scale (VAS).
| Compressed calf | Non-compressed calf | p-value | |||||
|---|---|---|---|---|---|---|---|
| Pre-exercise | Post-exercise | Pre-exercise | Post-exercise | Compressed calf; pre vs. post-exercise | Non-compressed calf; pre vs. post-exercise | Post-exercise; compressed vs. non-compressed calf | |
| Resting conditions | 0 ± 0 | 1.5 ± 1.2 | 0 ± 0 | 1.5 ± 1.4 | 0.001 | 0.004 | 0.467 |
| Going downstairs | 0 ± 0 | 5.6 ± 1.6 | 0 ± 0 | 5.3 ± 1.9 | < 0.001 | < 0.001 | 0.233 |
Muscle soreness was assessed at baseline and 60 h after standardized eccentric exercise (compressed vs. non-compressed calf) in resting condition and when going downstairs (mean ± SD).
Range of motion
For passive ankle dorsiflexion, there was no statistical interaction (p = 0.46) or treatment main effect (p = 0.36); however, there was a main effect for time, with ankle dorsiflexion at follow-up (7.9 ± 6.2°) being significantly less (p = 0.02) than at baseline (13.0 ± 3.4°).
Calf circumference
For calf circumference, there was no statistical interaction (p = 0.32) or treatment main effect (p = 0.18); however, there was a main effect for time (p = 0.03), with circumference at follow-up (35.6 ± 1.8 cm) being significantly larger than baseline (35.1 ± 1.7 cm).
Creatine kinase levels
The CK levels were 132.3 ± 48.2 U/L at baseline and 3742.4 ± 4021.1 U/L 60 h after the exercise (p = 0.01).
Discussion
To our knowledge, this is the first study assessing compression garment prevention of DOMS by evaluating muscle soreness, ROM of the ankle joint, calf circumference and muscle edema using 3T MRI. Our results indicate that wearing conventional sports compression garments, compression class I (18-21 mmHg), during the regeneration phase has no significant effect on the development of muscle edema after DOMS had been induced. Furthermore, we observed no significant effect on muscle soreness, calf circumference or on the ROM of the ankle joint.
Muscle fibers are subject to greater mechanical stress during eccentric muscle contraction (Yanagisawa et al., 2015). The described eccentric exercise protocol has been successfully established in previous studies (Hotfiel et al., 2017; Kellermann et al., 2017) and can be considered effective in inducing DOMS, as we were able to observe significant changes in muscle soreness, ROM of the ankle joint, CK level, intramuscular T2-weighted signal intensity, and T2 relaxation time.
DOMS is considered an ultrastructural muscle lesion entity and has been classified as an overexertion-functional muscle disorder type Ib (Mueller-Wohlfahrt et al., 2013), which can be detected on MRI as intramuscular edema (Yanagisawa et al., 2015). Intramuscular fluid accumulation prolongs the T2 relaxation time of an exercised muscle and increases the signal intensity on T2-weighted images (Fulford et al., 2015; Yanagisawa et al., 2003). Previous studies have reported that changes in T2-weighted signal intensity peak after around three days post–eccentric training (Fulford et al., 2015; Yanagisawa et al., 2015). In addition, Nurenberg et al. showed in a histopathological study a good correlation between ultrastructural injury and MRI signal intensity after inducing DOMS (Nurenberg et al., 1992).
These detectable alterations in tissue water content could be explained by inflammatory responses following microtrauma in the muscle fibers, which result in the loss of sarcomere structural integrity (Ulbricht et al., 2015). Inflammatory cells such as neutrophils and macrophages are attracted to the damage site to remove the disrupted muscle tissue fragments and initiate muscle repair (Kanda et al., 2013; Paulsen et al., 2005; Peake et al., 2005; Yanagisawa et al., 2015). In general, neutrophils infiltrate damaged muscle within several hours after eccentric exercise and are replaced by blood monocyte-derived macrophages within approximately 24 h post-exercise (Peake et al., 2005). The infiltration of inflammatory cells from the blood vessels is accompanied by fluid effusion (Peake et al., 2005). Various cytokines that act as inflammatory mediators that increase vascular permeability are produced in the damaged muscle within several hours after repeated eccentric contraction (Paulsen et al., 2005; Peake et al., 2005).
Furthermore, ultrastructural muscle damage has been found to be associated with increased cytosolic calcium concentrations, which is believed to activate proteolytic enzymes, increase cell membrane permeability, and lead to the release of interstitial fluid (MacIntyre et al., 1995). The ultrastructural muscle lacerations and the inflammatory triggered responses are in line with our results, as we were able to describe induced intramuscular edema in the MRI and significant changes in CK levels after eccentric training in all subjects. CK efflux would also result from the loss of sarcolemmal integrity (increased permeability and/or breakdown of the membrane surrounding the muscle cell) due to the mechanical stress (Friden et al., 1983; Yanagisawa et al., 2015). Like many other studies, we are able to demonstrate a significant effect of eccentric exercise on the level of muscle soreness (Gatterer et al., 2015; Yanagisawa et al., 2015), which typically peaks after 48 – 72 h (Yanagisawa et al., 2015). Muscle soreness likely reflects ultrastructural muscle fiber damage, and mechanoreceptor stimulation may contribute to the perception of soreness (Weerakkody et al., 2001).
Despite the widespread occurrence of DOMS, there is little consensus on which treatments may be the most effective at alleviating symptoms and accelerating recovery from this performance-limiting condition (Nelson, 2013). Adequate therapy of DOMS, which is also defined as a grade I lesion in MRI, is highly relevant, as most of the muscle injuries that occur in sports are grade I injuries (Ekstrand et al., 2016). Even low-grade injuries, which exhibit signs of intramuscular edema without structural tears, should be treated seriously, as they may result in muscular weakness or lead to tears and recurrent injuries (Ekstrand et al., 2013).
In this context, the effects of wearing compression garments during regeneration are subject of ongoing discussions (Beliard et al., 2015; Goto et al., 2017; Hill et al., 2014; Marques-Jimenez et al., 2016).
No significant effect of compression therapy on muscle soreness, ROM and calf circumference was observed in our study, which is in line with Kerherve et al. (Kerherve et al., 2017). They reported in a recently published study no effect of compression garments (23±2 mmHg) in trail running at the lower leg in 14 participants concerning muscle soreness over a period of 1h until 7 days after induction of DOMS, which extends the findings of several other studies (Bovenschen et al., 2013; Driller and Halson, 2013; Mizuno et al., 2016). Besides muscle soreness, no effect of wearing compression garments on calf circumference was reported in an endurance trial of 18 males divided in two groups of downhill and level running (Mizuno et al., 2016). In contrast, Kim et al. observed lower muscle soreness in 8 healthy students wearing a compression garment (5-10 mmHg) for 24 h after an eccentric exercise using the elbow flexor (Kim and Lee, 2017). This is in line with the findings of Kraemer et al., who described a prevented loss of elbow motion, decreased soreness and reduced swelling of the upper arm in 10 women wearing a compression sleeve (10 mmHg) for 5 days (Kraemer et al., 2001). In 2014, Goto et al. reported rapid recovery of one-repetition maximum for maximal voluntary contraction for knee extension and for chest press by wearing a whole-body compression garment for 24 h after resistance exercises and a reduced arm and thigh circumference (Goto and Morishima, 2014) Otherwise, the same author reported in a recently published study that wearing a whole-body compression garment during the post-exercise period after two bouts of strenuous exercise sessions did not promote recovery of muscle function for lower limb muscles nor did it attenuate exercise-induced muscle damage in 11 physically active males (Goto et al., 2017). Kraemer et al. also observed that wearing full-body compression garments for 24 h following intensive resistance exercise led to faster recovery of power output during bench press exercises (Kraemer et al., 2010), which is in line with Shimokochi et al. (Shimokochi et al., 2017), who investigated the effects of wearing whole body compression garments during night sleep on muscle fatigue recovery after high-intensity eccentric and concentric knee extensor exercises. The maximum voluntary isometric contraction force for knee extensor muscles 24 hours after the fatiguing protocol was approximately 10% greater in the compression group than in the non-compression condition (Shimokochi et al., 2017). Furthermore, wearing a compression garment (15 mmHg) in the post-exercise period for 12 h significantly improved recovery of jump performance following 100 drop jumps which was accompanied with reduced muscle soreness (Jakeman et al., 2010). By contrast, sprint performances were not significantly altered by the wearing of compression garments and no change of body mass occurred, whereas lower 24 h post exercise ratings of muscle soreness were reported (Doan et al., 2003; Duffield and Portus, 2007). It has been suggested that localized swelling may be one of the causes of soreness following damaging exercise (Jakeman et al., 2010), which can be seen as a possible explanation for our results. Though, further verification of this suggestion is required. However, the wide variation in methodological design, often accompanied with a small sample size, combined with different compression grades and duration of application, exercise modalities and interindividually differences of investigated population, may contribute to the apparently inconsistent clinical outcomes (Hill et al., 2014).
Limitations
Our study has some limitations. First, the number of participants included is rather small considering that there can be inter-individual differences related to DOMS expression with the potential for a non-responder. Hence, we performed a high-resolution MRI at follow-up which confirmed the presence of DOMS as intramuscular edema in every participant. Second, our data are representative of the applied study setting and should be considered cautiously in a different setting. We assessed DOMS at a follow-up of 60 h after eccentric training, as 48-72 h is considered the time window for the manifestation of DOMS. However, we are aware of inter-individual differences in DOMS. A third limitation is the use of each subject as its own control. One calf may influence the outcome of the other calf due to a systemic inflammatory healing response. We chose an intra-individual control group, as inter-individual differences in DOMS expression and CK expression have occurred in our preliminary tests and have been described in several studies (Kraemer et al., 2001; Yanagisawa et al., 2015). Results may be biased by non-responders, which could be under-recognized if they were treated with compression garments; and results may possibly provide false-positive benefits for the use of compression garments. Therefore, results should be confirmed by a further investigation recruiting two separate groups of participants, one wearing compression garments on both legs and the other without any compression garments.
Since regaining levels of performance and force delivery is an integral part of recovery from exercise induced muscle damage, future studies are also needed to explore the relation between compression garments and intramuscular edema on enhancing performance.
Conclusion
Our results indicate that wearing conventional sports compression garments after DOMS has been induced has no significant effect on muscle edema and muscle soreness. Our study provides insights into regeneration in the context of DOMS. This may result in implications for diagnostic and therapeutic strategies and for the understanding of pathophysiology in DOMS.
Acknowledgements
The expert technical assistance of Johanna Seelmann is gratefully acknowledged. Our sincere thanks to the study participants. We also thank the Imaging Science Institute (Erlangen, Germany) for providing us with measurement time at the 3T MRI scanner. The local ethics committee approved the performance of the present study with no requirements. The study was supported by the independent GOTS Research Grant 2016 provided by the Society for Orthopaedic Traumatologic Sports Medicine. All performed examinations of the study comply with the current laws of the Federal Republic of Germany. The authors declare that no competing interests exist.
Biographies
Rafael HEISS
Employment
Department of Radiology, University Hospital Erlangen, Friedrich-Alexander-Universität (FAU) Erlangen-Nürnberg, Erlangen, Germany
Degree
MD, Dr. med.
Research interests
Musculoskeletal imaging, diagnostics and treatment of structural and ultrastructural muscle injures, ultra-high-field MRI, cardiovascular radiology
E-mail: rafael.heiss@uk-erlangen.de
Thilo HOTFIEL
Employment
Division of Orthopedic Rheumatology, Department of Orthopedic Surgery, Friedrich-Alexander-University Erlangen-Nuremberg, Erlangen, Germany
Degree
MD, Dr. med.
Research interests
Diagnostics and treatment of structural and ultrastructural muscle injures, overuse injuries in elite runners and triathletes, evaluation of new diagnostic approaches in musculoskeletal imaging, lower limb biomechanics
E-mail: thilo.hotfiel@fau.de
Marion KELLERMANN
Employment
Division of Orthopedic Rheumatology, Department of Orthopedic Surgery, Friedrich-Alexander-University Erlangen-Nuremberg, Erlangen, Germany
Degree
medical student
Research interests
DOMS, Intramuscular Perfusion, CEUS, Muscle Injury, Compression therapy
E-mail: kellermann-m@gmx.de
Matthias S. MAY
Employment
Department of Radiology, University Hospital Erlangen, Friedrich-Alexander-Universität (FAU) Erlangen-Nürnberg, Erlangen, Germany
Degree
MD, PD Dr. med.
Research interests
Computed Tomography: Radiation Dose, Cardiac, Head and Neck, Chest, Abdominal, Pediatric Magnetic Resonance: Cardiac, Angiography
E-mail: matthias.may@uk-erlangen.de
Wolfgang WUEST
Employment
Department of Radiology, Univ. Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg, Erlangen, Germany
Degree
MD, PD Dr. med.
Research interests
Head and neck, cardiovascular radiology
E-mail: wolfgang.wuest@uk-erlangen.de
Rolf JANKA
Employment
Department of Radiology, University Hospital Erlangen, Friedrich-Alexander-Universität (FAU) Erlangen-Nürnberg, Erlangen, Germany
Degree
MD, Prof. Dr. med.
Research interests
Cardiac, Angiography, Musculoskeletal
E-mail: rolf.janka@uk-erlangen.de
Armin M. NAGEL
Employment
Department of Radiology, University Hospital Erlangen, Friedrich-Alexander-Universität (FAU) Erlangen-Nürnberg, Erlangen, Germany
Degree
PhD, Prof. Dr. rer. nat.
Research interests
Metabolic and functional magnetic resonance imaging (MRI), non-proton MRI, ultra-high-field MRI, MRI physics
E-mail: armin.nagel@uk-erlangen.de
Michael UDER
Employment
Department of Radiology, University Hospital Erlangen, Friedrich-Alexander-Universität (FAU) Erlangen-Nürnberg, Erlangen, Germany
Degree
MD, Prof. Dr. med.
Research interests
Urogenital radiology, Interventional radiology, Cardiac
E-mail: michael.uder@uk-erlangen.de
Matthias HAMMON
Employment
Department of Radiology, University Hospital Erlangen, Friedrich-Alexander-Universität (FAU) Erlangen-Nürnberg, Erlangen, Germany
Degree
MD, PD Dr. med.
Research interests
Musculoskeletal imaging, sodium MRI, computer applications in radiology, prostate imaging, pediatric radiology
E-mail: matthias.hammon@uk-erlangen.de
References
- Armstrong R.B. (1984) Mechanisms of exercise-induced delayed onset muscular soreness: a brief review. Medicine and Science in Sports and Exercise 16, 529-538. [PubMed] [Google Scholar]
- Beliard S., Chauveau M., Moscatiello T., Cros F., Ecarnot F., Becker F. (2015) Compression garments and exercise: no influence of pressure applied. Journal of Sports Science and Medicine 14, 75-83. [PMC free article] [PubMed] [Google Scholar]
- Best T.M., Hunter K.D. (2000) Muscle injury and repair. Physical Medicine and Rehabilitation Clinics of North America 11, 251-266. [PubMed] [Google Scholar]
- Bovenschen H.J., Booij M.T., van der Vleuten C.J. (2013) Graduated compression stockings for runners: friend, foe, or fake? Journal of Athletic Training 48, 226-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doan B.K., Kwon Y.H., Newton R.U., Shim J., Popper E.M., Rogers R.A., Bolt L.R., Robertson M., Kraemer W.J. (2003) Evaluation of a lower-body compression garment. Journal of Sports Sciences 21, 601-610. [DOI] [PubMed] [Google Scholar]
- Driller M.W., Halson S.L. (2013) The effects of wearing lower body compression garments during a cycling performance test. International Journal of Sports Physiology and Performance 8, 300-306. [DOI] [PubMed] [Google Scholar]
- Duffield R., Murphy A., Kellett A., Reid M. (2014) Recovery from repeated on-court tennis sessions: combining cold-water immersion, compression, and sleep recovery interventions. Int J International Journal of Sports Physiology and Performance 9, 273-282. [DOI] [PubMed] [Google Scholar]
- Duffield R., Portus M. (2007) Comparison of three types of full-body compression garments on throwing and repeat-sprint performance in cricket players. British Journal of Sports Medicine 41, 409-414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekstrand J., Askling C., Magnusson H., Mithoefer K. (2013) Return to play after thigh muscle injury in elite football players: implementation and validation of the Munich muscle injury classification. Br J Sports Med 47, 769-774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekstrand J., Lee J.C., Healy J.C. (2016) MRI findings and return to play in football: a prospective analysis of 255 hamstring injuries in the UEFA Elite Club Injury Study. British Journal of Sports Medicine 50, 738-743. [DOI] [PubMed] [Google Scholar]
- Friden J., Sjostrom M., Ekblom B. (1983) Myofibrillar damage following intense eccentric exercise in man. International Journal of Sports Medicine 4, 170-176. [DOI] [PubMed] [Google Scholar]
- Fulford J., Eston R.G., Rowlands A.V., Davies R.C. (2015) Assessment of magnetic resonance techniques to measure muscle damage 24 h after eccentric exercise. Scandinavian Journal of Medicine & Science in Sports 25, e28-39. [DOI] [PubMed] [Google Scholar]
- Gatterer H., Peters P., Philippe M., Burtscher M. (2015) The effect of pulsating electrostatic field application on the development of delayed onset of muscle soreness (DOMS) symptoms after eccentric exercise. Journal of Physical Therapy Science 27, 3105-3107t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glickman M.E., Rao S.R., Schultz M.R. (2014) False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. Journal of Clinical Epidemiology 67, 850-857. [DOI] [PubMed] [Google Scholar]
- Goto K., Mizuno S., Mori A. (2017) Efficacy of wearing compression garments during post-exercise period after two repeated bouts of strenuous exercise: a randomized crossover design in healthy, active males. Sports Medicine Open 3, 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto K., Morishima T. (2014) Compression garment promotes muscular strength recovery after resistance exercise. Medicine and Science in Sports and Exercise 46, 2265-2270. [DOI] [PubMed] [Google Scholar]
- Hill J., Howatson G., van Someren K., Leeder J., Pedlar C. (2014) Compression garments and recovery from exercise-induced muscle damage: a meta-analysis. British Journal of Sports Medicine 48, 1340-1346. [DOI] [PubMed] [Google Scholar]
- Hotfiel T., Kellermann M., Swoboda B., Wildner D., Golditz T., Grim C., Raithel M., Uder M., Heiss R. (2017) Application of Acoustic Radiation Force Impulse (ARFI) Elastography in Imaging of Delayed Onset Muscle Soreness (DOMS): A Comparative Analysis With 3T MRI. Journal of Sport Rehabilitation 1-21, May 17. [DOI] [PubMed] [Google Scholar]
- Huard J., Li Y., Fu F.H. (2002) Muscle injuries and repair: current trends in research. The Journal of Bone and Joint Surgery. American Volume 84-A, 822-832. [PubMed] [Google Scholar]
- Ibegbuna V., Delis K.T., Nicolaides A.N., Aina O. (2003) Effect of elastic compression stockings on venous hemodynamics during walking. Journal of Vascular Surgery 37, 420-425. [DOI] [PubMed] [Google Scholar]
- Jakeman J.R., Byrne C., Eston R.G. (2010) Lower limb compression garment improves recovery from exercise-induced muscle damage in young, active females. European Journal of Applied Physiology and Occupational Physiology 109, 1137-1144. [DOI] [PubMed] [Google Scholar]
- Jarvinen T.A., Jarvinen T.L., Kaariainen M., Kalimo H., Jarvinen M. (2005) Muscle injuries: biology and treatment. The American Journal of Sports Medicine 33, 745-764. [DOI] [PubMed] [Google Scholar]
- Kanda K., Sugama K., Hayashida H., Sakuma J., Kawakami Y., Miura S., Yoshioka H., Mori Y., Suzuki K. (2013) Eccentric exercise-induced delayed-onset muscle soreness and changes in markers of muscle damage and inflammation. Exercise Immunology Review 19, 72-85. [PubMed] [Google Scholar]
- Kellermann M., Heiss R., Swoboda B., Gelse K., Freiwald J., Grim C., Nagel A., Uder M., Wildner D., Hotfiel T. (2017) Intramuscular Perfusion Response in Delayed Onset Muscle Soreness (DOMS): A Quantitative Analysis with Contrast-Enhanced Ultrasound (CEUS). International Journal of Sports Medicine 38, 833-841. [DOI] [PubMed] [Google Scholar]
- Kerherve H.A., Samozino P., Descombe F., Pinay M., Millet G.Y., Pasqualini M., Rupp T. (2017) Calf Compression Sleeves Change Biomechanics but Not Performance and Physiological Responses in Trail Running. Frontiers in Physiology 8, 247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Lee J. (2017) Effect of compression garments on delayed-onset muscle soreness and blood inflammatory markers after eccentric exercise: a randomized controlled trial. Journal of Exercise Rehabilitation 13, 541-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.K., Kim M.C. (2014) The affect on delayed onset muscle soreness recovery for ultrasound with bee venom. Journal of Physical Therapy Science 26, 1419-1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo T.K., Li M.Y. (2016) A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. Journal of Chiropractic Medicine 15, 155-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer W.J., Bush J.A., Wickham R.B., Denegar C.R., Gomez A.L., Gotshalk L.A., Duncan N.D., Volek J.S., Putukian M., Sebastianelli W.J. (2001) Influence of compression therapy on symptoms following soft tissue injury from maximal eccentric exercise. The Journal of Orthopaedic and Sports Physical Therapy 31, 282-290. [DOI] [PubMed] [Google Scholar]
- Kraemer WJ, F.D., Spiering BA. (2004) Compression in the treatment of acute muscle injuries in sport. International SportMed Journal 5, 200. [Google Scholar]
- Kraemer W.J., Flanagan S.D., Comstock B.A., Fragala M.S., Earp J.E., Dunn-Lewis C., Ho J.Y., Thomas G.A., Solomon-Hill G., Penwell Z.R., Powell M.D., Wolf M.R., Volek J.S., Denegar C.R., Maresh C.M. (2010) Effects of a whole body compression garment on markers of recovery after a heavy resistance workout in men and women. Journal of Strength and Conditioning Research 24, 804-814. [DOI] [PubMed] [Google Scholar]
- MacIntyre D.L., Reid W.D., McKenzie D.C. (1995) Delayed muscle soreness. The inflammatory response to muscle injury and its clinical implications. Sports Medicine 20, 24-40. [DOI] [PubMed] [Google Scholar]
- Marques-Jimenez D., Calleja-Gonzalez J., Arratibel I., Delextrat A., Terrados N. (2016) Are compression garments effective for the recovery of exercise-induced muscle damage? A systematic review with meta-analysis. Physiology & Behavior 153, 133-148. [DOI] [PubMed] [Google Scholar]
- Mizuno S., Morii I., Tsuchiya Y., Goto K. (2016) Wearing Compression Garment after Endurance Exercise Promotes Recovery of Exercise Performance. International Journal of Sports Medicine 37, 870-877. [DOI] [PubMed] [Google Scholar]
- Mueller-Wohlfahrt H.W., Haensel L., Mithoefer K., Ekstrand J., English B., McNally S., Orchard J., van Dijk C.N., Kerkhoffs G.M., Schamasch P., Blottner D., Swaerd L., Goedhart E., Ueblacker P. (2013) Terminology and classification of muscle injuries in sport: the Munich consensus statement. British Journal of Sports Medicine 47, 342-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson N. (2013) Delayed onset muscle soreness: is massage effective? Journal of Bodywork and Movement Therapies 17, 475-482. [DOI] [PubMed] [Google Scholar]
- Nosaka K., Clarkson P.M. (1996) Variability in serum creatine kinase response after eccentric exercise of the elbow flexors. International Journal of Sports Medicine 17, 120-127. [DOI] [PubMed] [Google Scholar]
- Nurenberg P., Giddings C.J., Stray-Gundersen J., Fleckenstein J.L., Gonyea W.J., Peshock R.M. (1992) MR imaging-guided muscle biopsy for correlation of increased signal intensity with ultrastructural change and delayed-onset muscle soreness after exercise. Radiology 184, 865-869. [DOI] [PubMed] [Google Scholar]
- Paulsen G., Benestad H.B., Strom-Gundersen I., Morkrid L., Lappegard K.T., Raastad T. (2005) Delayed leukocytosis and cytokine response to high-force eccentric exercise. Medicine and Science in Sports and Exercise 37, 1877-1883. [DOI] [PubMed] [Google Scholar]
- Paulsen G., Mikkelsen U.R., Raastad T., Peake J.M. (2012) Leucocytes, cytokines and satellite cells: what role do they play i/nablemuscle damage and regeneration following eccentric exercise? Exercise Immunology Review 18, 42-97. [PubMed] [Google Scholar]
- Peake J., Nosaka K., Suzuki K. (2005) Characterization of inflammatory responses to eccentric exercise in humans. Exercise Immunology Review 11, 64-85. [PubMed] [Google Scholar]
- Pearcey G.E., Bradbury-Squires D.J., Kawamoto J.E., Drinkwater E.J., Behm D.G., Button D.C. (2015) Foam rolling for delayed-onset muscle soreness and recovery of dynamic performance measures. Journal of Athletic Training 50, 5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peetrons P. (2002) Ultrasound of muscles. European Radiology 12, 35-43, Jan. [DOI] [PubMed] [Google Scholar]
- Scurr J.H., Machin S.J., Bailey-King S., Mackie I.J., McDonald S., Smith P.D. (2001) Frequency and prevention of symptomless deep-vein thrombosis in long-haul flights: a randomised trial. The Lancet 357, 1485-1489. [DOI] [PubMed] [Google Scholar]
- Shimokochi Y., Kuwano S., Yamaguchi T., Abutani H., Shima N. (2017) Effects of Wearing a Compression Garment During Night Sleep on Recovery From High-Intensity Eccentric-Concentric Quadriceps Muscle Fatigue. Journal of Strength and Conditioning Research 31, 2816-2824. [DOI] [PubMed] [Google Scholar]
- Ulbricht A., Gehlert S., Leciejewski B., Schiffer T., Bloch W., Hohfeld J. (2015) Induction and adaptation of chaperone-assisted selective autophagy CASA in response to resistance exercise in human skeletal muscle. Autophagy 11, 538-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valderrabano V., Pagenstert G., Horisberger M., Knupp M., Hintermann B. (2006) Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. The American Journal of Sports Medicine 34, 993-939. [DOI] [PubMed] [Google Scholar]
- Valle X., Til L., Drobnic F., Turmo A., Montoro J.B., Valero O., Artells R. (2013) Compression garments to prevent delayed onset muscle soreness in soccer players. Muscles, Ligaments and Tendons Journal 3, 295-302. [PMC free article] [PubMed] [Google Scholar]
- Weerakkody N.S., Whitehead N.P., Canny B.J., Gregory J.E., Proske U. (2001) Large-fiber mechanoreceptors contribute to muscle soreness after eccentric exercise. The Journal of Pain 2, 209-219. [DOI] [PubMed] [Google Scholar]
- Yanagisawa H., Kurita R., Kamata T., Yoshioka K., Kato D., Iwasawa A., Nakazato T., Torimura M., Niwa O. (2015) Effect of the sp(2)/sp(3) Ratio in a Hybrid Nanocarbon Thin Film Electrode for Anodic Stripping Voltammetry Fabricated by Unbalanced Magnetron Sputtering Equipment. Analytical Sciences 31, 635-641. [DOI] [PubMed] [Google Scholar]
- Yanagisawa O., Niitsu M., Yoshioka H., Goto K., Itai Y. (2003) MRI determination of muscle recruitment variations in dynamic ankle plantar flexion exercise. American Journal of Physical Medicine & Rehabilitation 82, 760-765. [DOI] [PubMed] [Google Scholar]


