Abstract
The recovery of ischemic myocardium blood perfusion is the main treatment option for acute myocardial infarction (AMI). However, this treatment option has multiple side effects that directly affect the quality of life of the patients. The activation of platelet function plays an important role in the occurrence, development and treatment of AMI. The aim of the present study was to analyze the effects of remote ischemic post-conditioning on platelet activation of AMI patients with primary PCI treatment and clinical prognosis. A total of 71 patients with AMI were treated with primary percutaneous coronary intervention (PCI). They were randomly divided into control group (n=34) and observation group (n=37). The patients in the observation group were treated with remote ischemic post-conditioning. Further, flow cytometer was used to detect the platelet alpha granule membrane glycoprotein (CD62P) and the percentages of activated IIb/IIIa (PAC-1). The maximum platelet aggregation rate induced by adenosine diphosphate (ADP) and arachidonic acid (AA) was measured by light transmittance aggrometer. The incidence of major adverse cardiac events (MACE) was compared between the two groups during the follow-up period of 6 months. The percentage of CD62P (24 h after PCI) in the observation group was significantly lower than control group (P<0.05). Further, the incidence of MACE in the observation group was also lower than that of the control group (P<0.05). Remote ischemic post-conditioning could reduce the incidence of MACE in patients with AMI after primary PCI treatment. Moreover, the above observation may be related to the improvement of platelet CD62P activation.
Keywords: remote ischemic post-conditioning, acute myocardial infarction, percutaneous coronary intervention, platelet activation, maximum aggregation rate, major adverse cardiac events
Introduction
The timely opening of the culprit vessels and restoration of the blood perfusion of ischemic myocardium is the main treatment for acute myocardial infarction (AMI). It helps in maintaining heart function and improves clinical prognosis (1). However, reperfusion injury caused by percutaneous trans-luminal coronary angioplasty and percutaneous coronary intervention (PCI) results in poor blood flow as well as stent restenosis (2–4). The above factors collectively reduce the therapeutic effect and quality of life of AMI patients. Multiple studies have confirmed (5,6) that the activation of platelet function plays an important role in the occurrence, development and treatment of AMI. PCI pre-operative and post-operative antiplatelet therapy is the basis of AMI therapy.
Basic and clinical research supports in situ ischemic preconditioning (7,8) as it has ability to reduce the degree of platelet activation. On the other hand, the remote ischemic post-conditioning is different from in situ ischemic pre-conditioning. The clinical operation is simple and is quite easy (9,10). The aim of the present study was to analyze the effects of remote ischemic post-conditioning on platelet activation of AMI patients with primary PCI treatment and clinical prognosis.
Patients and methods
Patients
A total of 71 patients with the first diagnosis of acute ST-segment elevation myocardial infarction (STEMI) in The First Affiliated Hospital of Soochow University (Suzhou, China) from October, 2015 to May, 2016 were continuously selected. Inclusion criteria: ⅰ) PCI treatment performed within 90 min after first visit and ⅱ) according to the research program, the clinical data were completed, and the hospital's Ethics Approval and informed consents were obtained. Exclusion criteria: ⅰ) Patients with additional heart diseases such as dilated cardiomyopathy were excluded; ⅱ) patients with combined pump failure with the need of mechanical ventilation treatment; ⅲ) target lesions not suitable for PCI therapy, such as the left main branch, bifurcation lesions, and calcification lesions; ⅳ) high risk of bleeding, and coagulation disorders were excluded and ⅴ) severe hepatorenal dysfunction.
According to the order of admission, the patients were randomly divided into control group (n=34) and observation group (n=37). The baseline data of the two groups are comparable (Table I).
Table I.
Baseline data of the two groups.
| Variables | Control group (n=34) | Observation group (n=37) | t/χ2 | P-value |
|---|---|---|---|---|
| Male/female | 18/16 | 20/17 | 0.009 | 0.925 |
| Age (years) | 56.5±12.3 | 56.3±13.5 | 0.121 | 0.968 |
| Smoking cases | 10 (29.4%) | 13 (35.1%) | 0.265 | 0.607 |
| Hypertension cases | 19 (55.9%) | 20 (54.1%) | 0.024 | 0.877 |
| Diabetes cases | 3 (8.8%) | 5 (13.5%) | 0.390 | 0.532 |
| Family history of coronary heart disease cases | 2 (5.9%) | 3 (8.1%) | −1.000 | |
| Blood vessels | 0.723 | 0.697 | ||
| Anterior descending branch | 19 (55.9) | 18 (48.6) | ||
| Right coronary artery | 13 (38.2) | 15(40.5) | ||
| Circumflex | 2(5.9) | 4 (10.8) | ||
| Platelet count (103/mm3) | 207±85 | 205±48 | 0.135 | 0.902 |
| Glutamic pyruvic transaminase (U/l) | 74±36 | 63±31 | 0.425 | 0.369 |
| Serum creatinine (µmmol/l) | 87±22 | 77±18 | 0.326 | 0.518 |
| Low density lipoprotein (mmol/l) | 3.07±1.03 | 3.00±0.97 | 0.107 | 0.798 |
| High sensitive C reactive protein (mg/l) | 8.01±4.42 | 8.38±4.49 | 0.124 | 0.757 |
| Use time of tirofiban (h) | 20.9±9.5 | 22.4±9.8 | 0.213 | 0.664 |
Research methods
The coronary artery was opened as per standardized protocols by the surgical and nursing team. They were treated with pre-operative oral doses of aspirin 300 mg and clopidogrel 300 mg, post-operative oral doses of aspirin 100 mg/day and clopidogrel 75 mg/day. Further, intra-operative and post-operative short-term low dose treatment was of tirofiban (5 µg/kg/h).
Remote ischemic post-conditioning: The observation group used the cuff-of sphygmomanometer to tightly wrap the left arm of the patient, inflated to 200 mmHg and maintained for 5 min, and then deflated to 0 mmHg. The condition was maintained for 5 min. This was one cycle, and a total of four cycles were performed. The control group also used the sphygmo-manometer for inflation up to 10 mmHg for 5 min, and was then deflated to 0 mmHg. Similarly, 4 cycles were carried out.
Observation index
Before PCI, the moment of intervention, 24 and 48 h after PCI, respectively, flow cytometer was used to detect the platelet alpha granule membrane glycoprotein (CD62P) and the percentages of activated IIb/IIIa (PAC-1). The maximum platelet aggregation rate induced by adenosine diphosphate (ADP) and arachidonic acid (AA), were measured by light transmittance aggrometer. The incidence of major adverse cardiac events (MACE) was compared between the two groups during the follow-up period of 6 months. Venous blood samples 4–5 ml were collected from patients with 3.8% sodium citrate (1:9) anticoagulation. Platelet rich plasma took 200 × g centrifugation for 10 min. Platelet-poor plasma was centrifuged at 1,300 × g for 15 min. Platelet count of platelet rich plasma was adjusted to 3 times × 1011/l.
Determination of CD62P and PAC-1
A total of 20 µl platelet-rich plasma was added to 5 µl FITC-labeled CD62P (BioLegend, San Diego, CA, USA) and incubated for 15 min at 37°C in the dark. A total of 5 µl platelet rich plasma was added to 10 µl FITC-labeled PAC-1 (Becton-Dickinson, San Diego, CA, USA) and was then incubated for 15 min at 37°C in the dark. Flow cytometer (Beckman XL; Beckman Coulter, Inc., Brea, CA, USA) was used for measurements.
Platelet maximum aggregation rate
Platelet rich plasma was incubated at 37°C for 10 min. 10 µM ADP and 0.5 µM AA were used to induce platelet aggregation. The reagents were purchased from Jiangsu Biyuntian Biotechnology Co., Ltd. (Jiangsu, China).
Statistical analysis
SPSS 20.0 software (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Measurement data were expressed by mean ± standard deviation. Comparison between two groups was tested by independent sample t-test. Analysis of variance with Fisher's exact post hoc test of repeated measures was used for percentage of CD62P and PAC-1 comparison at different time-points. Countable data were expressed by the number of cases or (%). Comparisons among groups were by χ2 method. P<0.05 indicated that the difference was statistically significant.
Results
Determination of CD62P and PAC-1
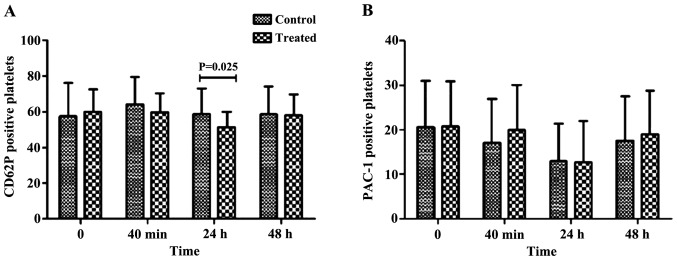
The percentage of CD62P (24 h after PCI) in the observation group was significantly lower than that in the control group (P<0.05). There was no difference at other time-points (P>0.05). Moreover, there was no statistical difference in the percentages of PAC-1 in both the groups at each time-point (P>0.05), (Table II; Fig. 1).
Table II.
Determination of CD62P and PAC-1 (%).
| Group | Control group (n=34) | Treatment group (n=37) | t-test | P-value |
|---|---|---|---|---|
| CD62P | ||||
| Before PCI | 57.6±18.5 | 59.9±12.5 | 0.365 | 0.583 |
| The moment of intervention | 64.2±15.3 | 59.6±10.5 | 0.693 | 0.199 |
| 24 h after PCI | 58.5±14.6 | 51.1±8.6 | 5.236 | 0.025 |
| 48 h after PCI | 58.6±15.5 | 57.9±11.7 | 0.187 | 0.853 |
| PAC-1 | ||||
| Before PCI | 20.6±10.3 | 20.8±10.1 | 0.065 | 0.972 |
| The moment of intervention | 17.1±9.8 | 19.9±10.1 | 0.587 | 0.571 |
| 24 h after PCI | 12.9±8.4 | 12.6±9.4 | 0.132 | 0.911 |
| 4 h after PCI | 17.5±10.0 | 18.9±9.7 | 0.365 | 0.721 |
CD62P, alpha granule membrane glycoprotein; PCI, percutaneous coronary intervention.
Figure 1.
The percentage of CD62P and PAC-1 detected by flow cytometry. (A) The percentage of CD62P 24 h after PCI in the observation group was significantly lower than that in the control group after PCI (P<0.05). (B) There was no difference in other time-points (P>0.05). There was no statistical difference in the percentage of PAC-1 in the groups at any time-point (P>0.05). CD62P, alpha granule membrane glycoprotein; PCI, percutaneous coronary intervention.
Determination of the maximum platelet aggregation rate
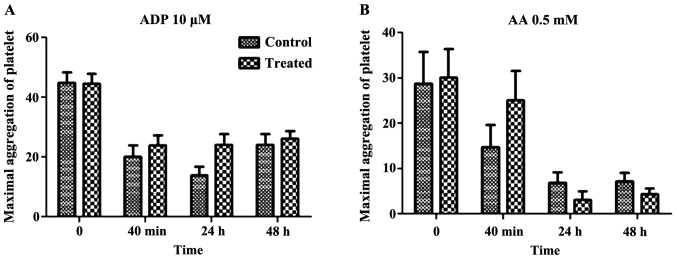
There was no significant difference in maximum platelet aggregation rate induced by ADP and AA at different time-points (P>0.05). The two groups reached the lowest 24 h after PCI, and recovered 48 h after PCI (Table III; Fig. 2).
Table III.
Determination of the maximum platelet aggregation rate (%).
| Group | Control group (n=34) | Treatment group (n=37) | t-test | P-value |
|---|---|---|---|---|
| ADP | ||||
| Before PCI | 44.8±6.4 | 44.6±6.3 | 0.047 | 0.953 |
| The moment of intervention | 20.0±6.9 | 23.8±6.3 | 0.623 | 0.458 |
| 24 h after PCI | 13.8±5.9 | 21.0±6.5 | 0.421 | 0.679 |
| 48 h after PCI | 24.0±6.5 | 26.1±5.6 | 0.359 | 0.621 |
| AA | ||||
| Before PCI | 28.7±7.0 | 30.1±6.2 | 0.212 | 0.881 |
| The moment of intervention | 14.7±4.9 | 25.1±6.5 | 0.724 | 0.210 |
| 24 h after PCI | 5.8±2.3 | 3.0±1.9 | 0.863 | 0.132 |
| 48 h after PCI | 7.1±1.9 | 5.2±1.3 | 0.659 | 0.222 |
ADP, adenosine diphosphate; PCI, percutaneous coronary intervention.
Figure 2.
Maximum platelet aggregation rate detected by turbidimetry. There was no significant difference in maximum platelet aggregation rate induced by (A) ADP and (B) AA at different time-points (P>0.05). The two groups were at the lowest level 24 h after PCI, and recovered 48 h after PCI. PCI, percutaneous coronary intervention; ADP, adenosine diphosphate; AA, arachidonic acid.
Comparison of MACE
The incidence of MACE in the observation group was lower than that in the control group and the difference was statistically significant (P<0.05) (Table IV).
Table IV.
Comparison of MACE [cases (%)].
| Group | Target vessel reconstruction | Recurrent myocardia infarction | Congestive heart failure | Rehospitalization | Sudden cardiac death | Overall incidence |
|---|---|---|---|---|---|---|
| Control group (n=34) | 1 | 2 | 2 | 3 | 1 | 9 (26.5) |
| Treatment group (n=37) | 0 | 1 | 1 | 1 | 0 | 3 (8.1) |
| χ2 | 4.254 | |||||
| P-value | 0.039 |
MACE, major adverse cardiac events.
Discussion
The results of the present study showed that the percentage of CD62P after 24 h of PCI, in the observation group was significantly lower than that in the control group. Further, there was no difference in other time-points. Also, there was no significant difference in maximum platelet aggregation rate induced by ADP and AA at different time-points. The incidence of MACE in the observation group was lower than that of the control group. Thus, it could be suggested that remote ischemic post-conditioning has the ability to reduce the incidence of MACE in patients with AMI after primary PCI treatment. Furthermore, this may be related to the improvement of platelet CD62P activation. Earlier studies (11,12) revealed that remote ischemic post-conditioning could increase the release of reactive oxygen species, adenosine, bradykinin, opioids and other factors. These factors in turn activated intracellular tyrosine kinase (TK), MEK1/2, PIK3, AKT, ERK1/2, so as to upregulate RISK reperfusion injury protective enzyme pathway (13,14). These factors could have mediated the downstream target molecules such as eNOS, GC in order to activate potassium ATP channel (15), and may have collectively caused inhibition of mitochondrial permeability transition pore (mPTP) opening (16). However, the specific mechanism needs further confirmation.
CD62P and PAC-1 are considered as the markers of platelet activation. PAC-1 is considered as a GPIIb/III complex fibrinogen receptor. After platelet activation, GPIIb/IIIa receptor activity expression is the final path to induce platelet aggregation. Thus, PAC-1 is also considered to be an early marker of platelet activation (17). On the other hand, CD62P is expressed in plasma alpha granules in resting state, when platelets and endothelial cells are stimulated by thrombin, histamine and oxygen free radicals. It has been considered as a specific marker of late platelet activation (18). The results of the present study showed that remote ischemic post-conditioning could decrease the expression of CD62P in platelets but had no effect on the expression of PAC-1. The reason could be primarily the treatment of the patients with triple antiplatelet therapy (aspirin + clopidogrel + tirofiban), and especially tirofiban was antagonist of the platelet GPIIb/IIIa receptor. This had a great influence on the expression of PAC-1. Secondly, the statistical difference of CD62P expression after 24 h may be the delayed protective effect of ischemic post-conditioning, and the early influence on platelet function may be masked by antiplatelet drugs. Thirdly, CD62P was a late specific marker of platelet activation, so there was a statistical difference between the two groups after 24 h.
Aspirin, clopidogrel and tirofiban affected platelet aggregation rates. Moreover, it was indicated that the remote ischemic post-conditioning had an effect on platelet activity, but its effect was far weaker than that of antiplatelet drugs. All of the participants in this study had the first occurrence of AMI, excluding the effect of ischemic pre-conditioning on the study results. Remote ischemic post-conditioning could further reduce platelet activity in patients with AMI, and could play a synergistic role with antiplatelet drugs. The prime drawback of the present study was the small sample size. Moreover, the mechanism of remote ischemic post-conditioning effect on platelet function was not analyzed in-depth. Subjects receiving multiple antiplatelet therapies may have an impact on the outcome of the study.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Al Shammeri O, Garcia L. Thrombolysis in the age of primary percutaneous coronary intervention: Mini-review and meta-analysis of early PCI. Int J Health Sci (Qassim) 2013;7:91–100. doi: 10.12816/0006026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hausenloy DJ, Barrabes JA, Bøtker HE, Davidson SM, Di Lisa F, Downey J, Engstrom T, Ferdinandy P, Carbrera-Fuentes HA, Heusch G, et al. Ischaemic conditioning and targeting reperfusion injury: A 30 year voyage of discovery. Basic Res Cardiol. 2016;111:70. doi: 10.1007/s00395-016-0588-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao XJ, Liu XL, He GX, Xu HP. Effects of single-dose atorvastatin on interleukin-6, interferon gamma, and myocardial no-reflow in a rabbit model of acute myocardial infarction and reperfusion. Braz J Med Biol Res. 2014;47:245–251. doi: 10.1590/1414-431X20132999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li H, Jiang Z, Liu X, Yang Z. Higher plasma level of STIM1, OPG are correlated with stent restenosis after PCI. Int J Clin Exp Med. 2015;8:21089–21097. [PMC free article] [PubMed] [Google Scholar]
- 5.Serebruany V, Malinin A, Aradi D, Kuliczkowski W, Norgard NB, Boden WE. The in vitro effects of niacin on platelet biomarkers in human volunteers. Thromb Haemost. 2010;104:311–317. doi: 10.1160/TH10-01-0015. [DOI] [PubMed] [Google Scholar]
- 6.Boukhris M, Bousselmi R, Tomasello SD, Elhadj ZI, Azzarelli S, Marzà F, Galassi AR. Mechanical post-conditioning in STEMI patients undergoing primary percutaneous coronary intervention. J Saudi Heart Assoc. 2015;27:192–200. doi: 10.1016/j.jsha.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu J, Sun S, Lu X, Hu X, Yang M, Tang W. Remote ischemic pre-and postconditioning improve postresuscitation myocardial and cerebral function in a rat model of cardiac arrest and resuscitation. Crit Care Med. 2015;43:2053–2056. doi: 10.1097/CCM.0000000000000684. [DOI] [PubMed] [Google Scholar]
- 8.Scalone G, Aurigemma C, Tomai F, Corvo P, Battipaglia I, Lanza GA, Crea F. Effect of pre-infarction angina on platelet reactivity in acute myocardial infarction. Int J Cardiol. 2013;167:51–56. doi: 10.1016/j.ijcard.2011.11.085. [DOI] [PubMed] [Google Scholar]
- 9.Wang N, Wang GS, Yu HY, Mi L, Guo LJ, Gao W. Myocardial protection of remote ischemic postconditioning during primary percutaneous coronary intervention in patients with acute ST-segment elevation myocardial infarction. Beijing Da Xue Xue Bao. 2014;46:838–843. (In Chinese) [PubMed] [Google Scholar]
- 10.Lavi S, DAlfonso S, Diamantouros P, Camuglia A, Garg P, Teefy P, Jablonsky G, Sridhar K, Lavi R. Remote ischemic postconditioning during percutaneous coronary interventions: Remote ischemic postconditioning-percutaneous coronary intervention randomized trial. Circ Cardiovasc Interv. 2014;7:225–232. doi: 10.1161/CIRCINTERVENTIONS.113.000948. [DOI] [PubMed] [Google Scholar]
- 11.Wei M, Xin P, Li S, Tao J, Li Y, Li J, Liu M, Li J, Zhu W, Redington AN. Repeated remote ischemic postconditioning protects against adverse left ventricular remodeling and improves survival in a rat model of myocardial infarction. Circ Res. 2011;108:1220–1225. doi: 10.1161/CIRCRESAHA.110.236190. [DOI] [PubMed] [Google Scholar]
- 12.Xiong J, Liao X, Xue FS, Yuan YJ, Wang Q, Liu JH. Remote ischemia conditioning-an endogenous cardioprotective strategy from outside the heart. Chin Med J (Engl) 2011;124:2209–2215. [PubMed] [Google Scholar]
- 13.Xu J, Sun S, Lu X, Hu X, Yang M, Tang W. Remote ischemic pre- and postconditioning improve postresuscitation myocardial and cerebral function in a rat model of cardiac arrest and resuscitation. Crit Care Med. 2015;43:e12–e18. doi: 10.1097/CCM.0000000000000684. [DOI] [PubMed] [Google Scholar]
- 14.Heusch G, Bøtker HE, Przyklenk K, Redington A, Yellon D. Remote ischemic conditioning. J Am Coll Cardiol. 2015;65:177–195. doi: 10.1016/j.jacc.2014.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Battipaglia I, Scalone G, Milo M, Di Franco A, Lanza GA, Crea F. Upper arm intermittent ischaemia reduces exercise-related increase of platelet reactivity in patients with obstructive coronary artery disease. Heart. 2011;97:1298–1303. doi: 10.1136/hrt.2011.226415. [DOI] [PubMed] [Google Scholar]
- 16.Stazi A, Scalone G, Laurito M, Milo M, Pelargonio G, Narducci ML, Parrinello R, Figliozzi S, Bencardino G, Perna F, et al. Effect of remote ischemic preconditioning on platelet activation and reactivity induced by ablation for atrial fibrillation. Circulation. 2014;129:11–17. doi: 10.1161/CIRCULATIONAHA.113.005336. [DOI] [PubMed] [Google Scholar]
- 17.Coller BS, Shattil SJ. The GPIIb/IIIa (integrin αIIbβ3) odyssey: A technology-driven saga of a receptor with twists, turns, and even a bend. Blood. 2008;112:3011–3025. doi: 10.1182/blood-2008-06-077891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Werkum JW, Gerritsen WBM, Kelder JC, Hackeng CM, Ernst SM, Deneer VHM, Suttorp MJ, Rensing BJWM, Plokker HWM, Ten Berg JM. Inhibition of platelet function by abciximab or high-dose tirofiban in patients with STEMI undergoing primary PCI: A randomised trial. Neth Heart J. 2007;15:375–381. doi: 10.1007/BF03086018. [DOI] [PMC free article] [PubMed] [Google Scholar]