Abstract
Naringenin (NGN) is a natural flavonoid that exerts antiinflammatory, antioxidant and cardioprotective effects. The present study investigated the effects of NGN on left ventricular hypertrophy in rats with NG-nitro-L-arginine methyl ester (L-NAME)-induced hypertension, and sought to determine the underlying mechanism of action. The rats received the following by gavage daily for 56 days: L-NAME (50 mg/kg/day) + NGN (100 mg/kg/day), L-NAME (50 mg/kg/day) + saline, or saline + saline. Blood pressure, heart rate and body weight were recorded. Left ventricular hypertrophy was assessed by echocardiography and hematoxylin-eosin staining. Angiotensin II (Ang II) and angiotensin-converting enzyme 1 (ACE1), which serve a pivotal role in cardiac remodeling, were evaluated by ELISA, reverse transcription-quantitative polymerase chain reaction and western blot analysis. NGN had no significant effect on body weight, heart rate or blood pressure. The extent of left ventricular hypertrophy in the L-NAME + NGN group was lower than in the L-NAME + saline group on day 56. NGN decreased Ang II and ACE1 protein levels in myocardial tissues. In conclusion, Ang II and ACE1 expression in cardiac tissue was inhibited by NGN in L-NAME-treated rats, which may contribute to the inhibitory effects of NGN on left ventricular hypertrophy that is induced by pressure overload.
Keywords: left ventricular hypertrophy, naringenin, NG-nitro-L-arginine methyl ester, angiotensin-converting enzyme 1, angiotensin II
Introduction
Left ventricular hypertrophy is a common complication, even in mild hypertension, and is detected in up to 36% of patients globally (1). Left ventricular hypertrophy is generally regarded as an adaptive response to chronic pressure overload. It is also a gateway to pathogenesis and heart failure. Concentric hypertrophy is an early remodeling event that often precedes myocardial dilatation that can progress to eccentric hypertrophy and global pump failure. Preventing and reversing the development of cardiac hypertrophy may be an effective therapeutic strategy for the treatment of hypertension with heart failure, resulting in an improved prognosis (2).
The renin-angiotensin-aldosterone system (RAS), especially angiotensin-converting enzyme 1 (ACE1) and angiotensin II (Ang II), plays an important role in the pathophysiology of left ventricular remodeling. Under physiological conditions, ACE1 expression in the heart is relatively low and mainly localized in the endothelium of the coronary artery and myocardial endometrium (3). The expression of ACE1 is upregulated in models of heart damage that is induced by stress overload, volume overload, myocardial infarction, and heart failure (4). Under pathological conditions, both cardiomyocytes and fibroblasts express ACE1 protein. Although the RAS plays a supportive role in hemodynamics, sustained activation of the RAS can lead to heart disease, including heart deterioration and failure (5). Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers are applied clinically to manage pathological cardiac hypertrophy (6).
Naringenin (NGN) is a flavonoid that is found in citrus fruits (e.g., grapefruit) and Chinese herbs (e.g., C. aurantium) (7), and its cardioprotective effect has been recently reported. Epidemiological studies have found a correlation between higher flavonoid intake from fruits and vegetables and a lower risk of developing cardiovascular disease (8). NGN has been shown to alleviate myocardial ischemia/reperfusion injury and protect against doxorubicin-induced cardiac toxicity (9,10). However, remaining unclear is whether NGN mitigates the development of pressure overload-induced cardiac hypertrophy in its early stage and delays the progression of heart failure.
In the present study, NG -nitro-L-arginine methyl ester (L-NAME) was used to induce cardiac hypertrophy in Sprague-Dawley rats. We sought to determine whether NGN is able to exert a protective effect against left ventricular hypertrophy. We also sought to identify the possible mechanisms that underlie these effects. Additionally, we investigated whether NGN influences activation of the RAS, which is overactivated by pressure overload.
Materials and methods
Animal care and use
All of the studies followed the guidelines of the Animal Care and Use Committee of Peking University. The animal protocol was approved by the Animal Ethical and Welfare Committee at China-Japan Friendship Hospital (Beijing, China). Male Sprague-Dawley rats (160–180 g) were purchased from Beijing Vital River Laboratory Animal Technology Company (Beijing, China) and maintained in a specific pathogen-free facility under a 12/12 h light/dark cycle with controlled room temperature and free access to standard chow and water. Three groups of rats (n=10 per group) received the following by gavage daily for 8 weeks: L-NAME (50 mg/kg) + NGN (100 mg/kg), L-NAME (50 mg/kg) + saline, or saline + saline. L-NAME and NGN were purchased from Sigma-Aldrich; Merck KGaA (Darmstadt, Germany).
Blood pressure measurement
Arterial systolic blood pressure and heart rate were measured in conscious, restrained rats using a noninvasive computerized tail-cuff system (Beijing Softron Biotechnology Co., Ltd, Beijing, China). Measurements were performed every week, beginning 1 day before intragastric administration. Blood pressure was calculated for each rat as the average of three separate measurements in each session.
Echocardiography
Transthoracic echocardiography (Vevo 2100 image system, FUJIFILM VisualSonics, Toronto, Canada) was performed before the rats were sacrificed. Under anesthesia by an intraperitoneal injection of 45 mg/kg sodium pentobarbital, the rats were fixed on their backs. Chest fur was shaved, and the skin was cleaned. The rats were examined on day 56 after drug administration to monitor IVSth and LVPWth using a miniature M-mode ultrasound probe.
Histology and immunohistochemistry
Paraformaldehyde-fixed tissue was embedded in paraffin and processed, and 6-µm sections were stained with hematoxylin-eosin or Masson's Trichrome. Additional sections were immunostained using an indirect horseradish peroxidase immunoperoxidase method and specific antibody for the antigen of ACE1 (Abcam, Cambridge, MA, USA). Negative controls for immunostaining consisted of replacing each of the primary antibodies with an equivalent concentration of irrelevant rabbit polyclonal antibody. At least three different specimens were analyzed. The myocardial tissue staining results were analyzed using ImageJ image analysis software (National Institutes of Health, Bethesda, MD, USA).
Enzyme-linked immunosorbent assay
The concentrations of Ang II in blood samples and myocardial tissues were analyzed using a rat Ang II ELISA kit (Cusabio Biotech Co., Ltd., Wuhan, China) according to the manufacture's instructions. Absorbance at 450 nm was read using a Multi-Mode Microplate Reader (SpectraMax M2; MTX Lab Systems, Bradenton, FL, USA).
Reverse-transcription-quantitative polymerase chain reaction
Total RNA from the left ventricular was isolated using Trizol reagent (Applygen Technologies, Inc., Beijing, China). RNA then was quantified by Nanodrop (Thermo Fisher Scientific, Inc., Waltham, MA, USA) and samples were included when the 260/280 nm ratio was >1.6. cDNA was reverse-transcribed using a reverse transcription system (Promega Corporation, Madison, WI, USA). Real-time polymerase chain reaction (PCR) was performed using TransStart Green qPCR Supermix (TransGen Biotech, Beijing, China) and all samples were amplified in duplicate. The PCR reaction were carried out using the ABI Prism 7500 Sequence Detector (Applied Biosystems; Thermo Fisher Scientific Inc.). All of the amplification reactions underwent 35 cycles (initial stage at 95°C for 5 min, followed by a three-step cycle at 95°C for 30 sec, 58°C for 30 sec, and 72°C for 30 sec). The accuracy of the PCR products was confirmed by sequencing the amplicons. Fold changes in expression were calculated using 2−(ΔCt1−ΔCt2), where ΔCt represents the difference between the threshold cycle (Ct) for each target gene and housekeeping β-actin mRNA transcript levels.
The primers used were as follows: AGT (forward, ACACCCCTGCTACAGTCCAC; reverse, TTTTCTGGGCAGCAAGAACT), ACE1 (forward, CAGGGGTCCAAGTTCCACGTT; reverse, GCCACTGCTTACTGTAGCCCAA), ACE2 (forward, GAATGCGACCATCAAGCG; reverse, CAAGCCCAGAGCCTACGA), AT1R (forward, GGAAACAGCTTGGTGGTGAT; reverse, CACACTGGCGTAGAGGTTGA), β-actin (forward, GAGACCTTCAACACCCCAGCC; reverse, TCGGGGCATCGGAACCGCTCA).
Western blot analysis
Extracts of rat tissue were collected using tissue lysis buffer (Beyotime Institute of Biotechnology, Haimen, China) plus 1 mM phenylmethylsulfonyl fluoride. Total protein was quantified using a bicinchoninic acid protein assay (Pierce; Thermo Fisher Scientific, Inc.). Proteins were separated by 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis and electrophoretically transferred to nitrocellulose membranes. The membranes were blocked with PBS and Tween 20 containing 5% non-fat dry milk to prevent nonspecific antibody binding. Equal protein loading was determined using specific antibodies for the antigens of GAPDH (CWBiotech, Beijing, China), ACE1, AT1R and AT2R (Abcam, Cambridge, MA, USA), washed, and incubated with an appropriate IRDye800-conjugated secondary antibody (Rockland, Gilbertsville, PA, USA). Specific immunofluorescence bands were detected and analyzed using the Odyssey infrared imaging system and software (LI-COR Biosciences, Lincoln, NE, USA).
Statistical analysis
All of the results are expressed as the mean ± SEM or representative original data for 10 animals per treatment group. The statistical analysis was performed using Prism v.5.0 software (GraphPad Software, Inc., La Jolla, CA, USA). Significant differences were assessed using one-way analysis of variance followed by the Student-Newman-Keuls post hoc test or two-way analysis of variance followed by the Bonferroni post hoc test. P<0.05 was considered to indicate a statistically significant difference.
Results
Comparison of systolic blood pressure in L-NAME alone, L-NAME + NGN, and control groups
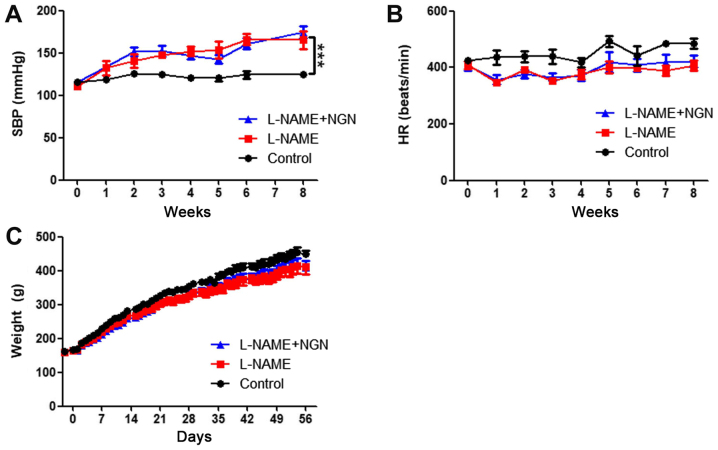
To investigate the protective effect of NGN against cardiac hypertrophy, we first developed a rat model of hypertension by administering 50 mg/kg L-NAME by gavage. As shown in Fig. 1A, L-NAME produced modest effects on blood pressure. Systolic blood pressure increased beginning in the third week after L-NAME administration and reached 175.0±6.9 mmHg at 8 weeks compared with 125.2±1.9 mmHg in the control group (P<0.001). No significant difference in systolic blood pressure was found between the L-NAME and L-NAME + NGN groups. NGN and L-NAME had no significant effects on body weight or heart rate (Fig. 1B and C).
Figure 1.
NGN does not significantly affect systolic blood pressure, HR or body weight in rats with L-NAME-induced hypertension. (A) Systolic blood pressure, (B) HR and (C) body weight were recorded in the control, L-NAME and L-NAME + NGN groups (n=10 per group). The data are expressed as the mean ± standard error of the mean. ***P<0.001. NGN, naringenin; SBP, systolic blood pressure; HR, heart rate; L-NAME, NG-nitro-L-arginine methyl ester.
Effects of NGN on indices of cardiac hypertrophy in rats
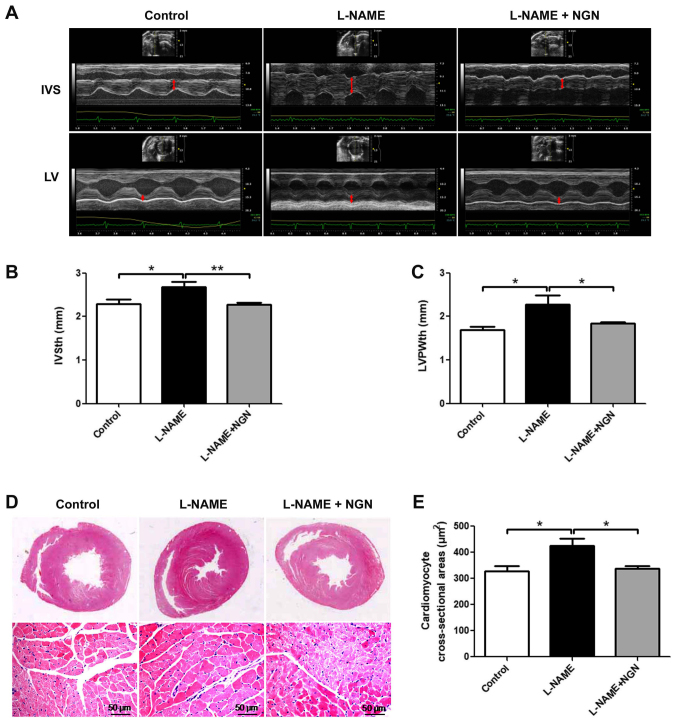
To evaluate the effect of NGN on cardiac remodeling, the wall thickness of the left ventricular was assessed by echocardiography, and morphological changes in myocardial tissue were assessed by hematoxylin-eosin staining. As shown in Fig. 2, the L-NAME group exhibited increases in interventricular septal thickness (IVSth), left ventricular posterior wall thickness (LVPWth), cardiomyocyte cross-sectional area (all P<0.05), and concentric hypertrophy compared with the control group. These effects were partially attenuated in the L-NAME + NGN group. No significant differences in myocardial fibrosis were observed among the three groups (data not shown).
Figure 2.
NGN attenuated left ventricular hypertrophy in rats with L-NAME-induced hypertension. (A) Representative images of M-mode echocardiography in rats 8 weeks after L-NAME administration. Red bidirectional arrows indicate the thickness of the interventricular septum or left ventricular posterior wall. Analysis of the thickness of the (B) interventricular septum and (C) left ventricular posterior wall as determined by M-mode echocardiography. (D) Whole-heart section (upper panels) and cardiomyocyte cross-section stained with hematoxylin-eosin (lower panels) 8 weeks after L-NAME administration. (E) Microscopic analysis of cardiomyocyte cross-sections n=10. The data are expressed as the mean ± standard error of the mean. *P<0.05, **P<0.01. NGN, naringenin; IVS, interventricular septum; LV, left ventricular; IVSth, interventricular septal thickness; LVPWth, left ventricular posterior wall thickness; L-NAME, NG-nitro-L-arginine methyl ester.
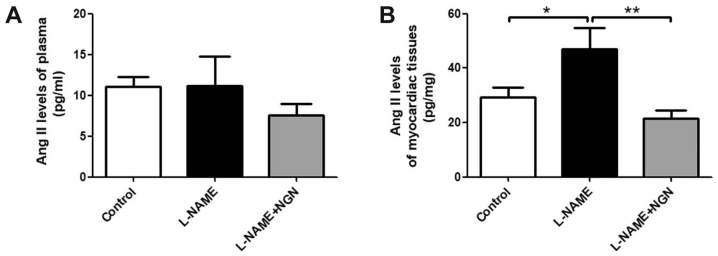
Effects of NGN on Ang II levels in plasma and myocardial tissue in rats
Ang II is a key molecule in myocardial remodeling. We detected Ang II levels in plasma and myocardial tissue in the three groups of rats by enzyme-linked immunosorbent assay (ELISA). Myocardial Ang II levels were significantly elevated in the L-NAME group compared with the control group (P<0.05; Fig. 3A). NGN reversed the L-NAME-induced elevation of Ang II levels in hypertensive cardiac tissue (P<0.05; Fig. 3A). No significant differences in serum Ang II levels were found among the three groups (Fig. 3B).
Figure 3.
NGN decreased Ang II levels in myocardial tissue in rats with L-NAME-induced hypertension. Ang II levels in the (A) plasma and (B) myocardial tissue in the control, L-NAME, and L-NAME + NGN groups 8 weeks after L-NAME administration n=10. The data are expressed as mean ± standard error of the mean. *P<0.05, **P<0.01. NGN, naringenin; Ang II, angiotensin II; L-NAME, NG-nitro-L-arginine methyl ester.
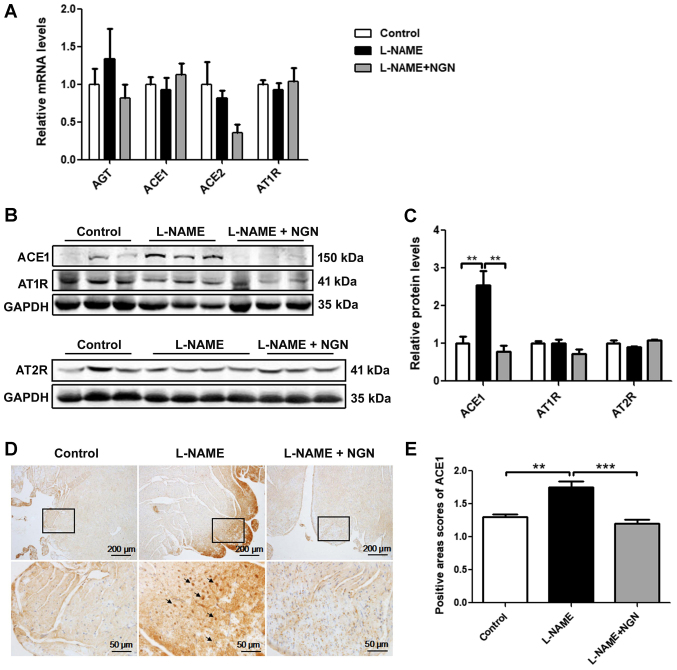
Comparison of ACE1 expression in myocardial tissue
To clarify the mechanism of the elevation of Ang II levels, ACE1 mRNA and protein were detected in myocardial tissue in the L-NAME, L-NAME + NGN, and control groups by real-time polymerase chain reaction (PCR), Western blot, and immunohistochemistry. No significant difference in ACE1 mRNA expression was found among the three groups (Fig. 4A). The protein expression of ACE1 in the L-NAME group was significantly higher than in the control group (P<0.05). Compared with the L-NAME group, ACE1 protein expression significantly decreased in the L-NAME + NGN group (P<0.05; Fig. 4B and C). Immunohistochemistry showed that ACE1 protein levels were significantly higher in the subendocardial and epicardial myocardium in the L-NAME group than in the control and L-NAME + NGN groups (Fig. 4D and E). No significant difference in angiotensinogen, ACE2, AT1R and AT2R mRNA or protein expression was found among the three groups (Fig. 4A-C).
Figure 4.
NGN inhibited ACE1 protein expression in myocardial tissue in rats with L-NAME-induced hypertension. (A) Analysis of angiotensinogen, ACE1, ACE2 and AT1R mRNA expression by reverse transcription-quantitative polymerase chain reaction in myocardial tissue from rats treated with vehicle (control), L-NAME, or L-NAME + NGN for 8 weeks. (B) Representative western blots of ACE1, AT1R and AT2R in myocardial tissue from rats in the control, L-NAME, and L-NAME + NGN groups 8 weeks after L-NAME administration. (C) Analysis of ACE1, AT1R and AT2R protein expression by western blot analysis. (D) Immunohistochemistry was used to detect ACE1 in serial paraffin sections of myocardial tissue from rats with L-NAME-induced hypertension. The insets show high-magnification images of the rectangular areas in each panel. The black arrowheads indicate strong ACE1 expression. (E) Analysis of ACE1 protein expression by immunohistochemistry n=10. The data are expressed as mean ± standard error of the mean. **P<0.01, ***P<0.001. NGN, naringenin; ACE, angiotensin-converting enzyme; AGT, angiotensinogen; AT1R, angiotensin II receptor type 1; AT2R, angiotensin II receptor type 2; L-NAME, NG-nitro-L-arginine methyl ester.
Discussion
The present study investigated the cardioprotective effect of NGN against pressure overload-induced left ventricular hypertrophy in rats and the underlying mechanism. The results showed that NGN had a protective effect on the heart by inhibiting the abnormal enlargement of cardiomyocytes and concentric myocardial hypertrophy that were induced by L-NAME. NGN also decreased ACE1 expression and Ang II content in cardiac tissue that were induced by pressure overload, suggesting that the inhibition of RAS overactivation in myocardial tissue might be related to the cardioprotective effect of NGN.
NGN is widely used in traditional Chinese medicine for its multiple pharmacological effects, including antiinflammatory and antioxidative actions (8,11,12). NGN has several purported beneficial cardiovascular effects and has been shown to prevent the growth of atherosclerotic plaques, improve vascular reactivity, inhibit platelet aggregation, decrease plasma lipids and lipoproteins, alleviate myocardial ischemia/reperfusion injury, and protect against doxorubicin-induced cardiac toxicity (8–10,13,14). A previous study reported that NGN supplementation improved hypertension in high-carbohydrate/high-fat-diet-fed obese rats (15). However, in the present study, NGN did not significantly lower the elevation of systolic blood pressure that was induced by L-NAME.
Left ventricular hypertrophy is characterized by an abnormal increase in left ventricular mass and the enlargement of cardiomyocytes, originating from an increase in myocyte size (16). Numerous clinical studies have indicated that left ventricular hypertrophy is an independent risk factor for coronary events, stroke, heart failure, peripheral arterial disease, and cardiovascular mortality in patients with hypertension (17,18). In the present study, we found that NGN treatment in rats with L-NAME-induced hypertension significantly inhibited cardiomyocyte enlargement and concentric cardiac hypertrophy.
Sustained RAS overactivation can lead to cardiovascular disease progression and deterioration, although the RAS exerts a supportive effect on hemodynamic blood (5). Furthermore, the RAS in tissues and organs plays an important role in disease development. Angiotensin-converting enzyme and Ang II play a pivotal role in the RAS, and their expression in the heart is relatively low under physiological conditions (3). In a rat model of cardiac remodeling that was triggered by myocardial infarction, cardiac metabolism was improved by low-dose ACE inhibitor treatment, which did not prevent hypertension (19). In the present study, Ang II levels and ACE1 expression in left ventricular tissue were upregulated in the L-NAME-treated group, and NGN inhibited this upregulation in cardiac tissues. This suggests one mechanism by which NGN protects against left ventricular remodeling. NGN had no significant effect on plasma Ang II levels, which was consistent with its effect on blood pressure.
In the present study, hypertensive cardiac hypertrophy was still in the compensatory phase after 8 weeks of L-NAME administration, with intermediate hypertension, centripetal left ventricular wall thickening, a smaller end-diastolic diameter, and no serious myocardial fibrosis. Our animal model simulates patients who are in the early stage of hypertensive heart damage that is caused by long-term mild-to-moderate hypertension. Zhang et al (20), reported that NGN attenuated cardiac hypertrophy and interstitial fibrosis that were induced by aortic banding in mice, which was consistent with the present results in rats. However, blood pressure was acute and malignant increased, and myocardial damage appeared to be serious in the aortic-banding mouse model. Zhang et al (20), found that the cardioprotective effect of NGN may be associated with inhibition of the phosphatidylinositol-4,5-bisphosphate 3-kinase/Akt, extracellular signal-regulated kinase, and c-Jun N-terminal kinase signaling pathways. Our results suggest that NGN plays a protective role against cardiac remodeling by decreasing the expression of ACE1 and Ang II in heart tissue.
In summary, the present study revealed a novel mechanism by which NGN exerts cardioprotective effects, namely by negatively regulating Ang II and ACE1 expression in cardiac tissues. NGN protected against left ventricular hypertrophy after long-term mild to moderate hypertension that was induced by L-NAME administration in rats. Increasing the intake of NGN-rich citrus fruits and vegetables may be beneficial for preventing hypertensive cardiac hypertrophy, and pharmacological NGN analogues may be applied clinically for the treatment of hypertensive cardiac hypertrophy.
Acknowledgements
Not applicable.
Glossary
Abbreviations
- L-NAME
NG-nitro-L-arginine methyl ester
- ACE
angiotensin-converting enzyme
- Ang II
angiotensin II
- RAS
renin-angiotensin-aldosterone system
- IVSth
interventricular septal thickness
- LVPWth
left ventricular posterior wall thickness
- NGN
narigenin
Funding
This work was supported by the National Natural Science Foundation of China (grant nos. 81500326, 91639110) and Beijing Natural Science Foundation (grant no. 7172195).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
YG was involved in drafting the manuscript. YG and JZ designed the study. YG, ZW, YZ, YL, SW, WS, JG and CY collected and analyzed the data. YG, YW, WK and JZ interpreted the data, collected the funding for this study and gave final approval of the version to be published. All authors reviewed the initial manuscript and revised it critically for important intellectual content.
Ethics approval and consent to participate
The animal protocol was approved by the Animal Ethical and Welfare Committee at China-Japan Friendship Hospital (Beijing, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Boonpeng H, Yusoff K. The utility of copy number variation (CNV) in studies of hypertension-related left ventricular hypertrophy (LVH): Rationale, potential and challenges. Mol Cytogenet. 2013;6:8. doi: 10.1186/1755-8166-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nayor M, Enserro DM, Vasan RS, Xanthakis V. Cardiovascular health status and incidence of heart failure in the framingham offspring study. Circ Heart Fail. 2016;9:e002416. doi: 10.1161/CIRCHEARTFAILURE.115.002416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamada H, Fabris B, Allen AM, Jackson B, Johnston CI, Mendelsohn AO. Localization of angiotensin converting enzyme in rat heart. Circ Res. 1991;68:141–149. doi: 10.1161/01.RES.68.1.141. [DOI] [PubMed] [Google Scholar]
- 4.Hirsch AT, Talsness CE, Schunkert H, Paul M, Dzau VJ. Tissue-specific activation of cardiac angiotensin converting enzyme in experimental heart failure. Circ Res. 1991;69:475–482. doi: 10.1161/01.RES.69.2.475. [DOI] [PubMed] [Google Scholar]
- 5.Borghi C, SIIA Task Force and Rossi F; SIF Task Force Role of the renin-angiotensin-aldosterone system and its pharmacological inhibitors in cardiovascular diseases: Complex and critical issues. High Blood Press Cardiovasc Prev. 2015;22:429–444. doi: 10.1007/s40292-015-0120-5. [DOI] [PubMed] [Google Scholar]
- 6.Hellawell JL, Margulies KB. Myocardial reverse remodeling. Cardiovasc Ther. 2012;30:172–181. doi: 10.1111/j.1755-5922.2010.00247.x. [DOI] [PubMed] [Google Scholar]
- 7.Lu Y, Zhang C, Bucheli P, Wei D. Citrus flavonoids in fruit and traditional Chinese medicinal food ingredients in China. Plant Foods Hum Nutr. 2006;61:57–65. doi: 10.1007/s11130-006-0014-8. [DOI] [PubMed] [Google Scholar]
- 8.Mulvihill EE, Burke AC, Huff MW. Citrus flavonoids as regulators of lipoprotein metabolism and atherosclerosis. Annu Rev Nutr. 2016;36:275–299. doi: 10.1146/annurev-nutr-071715-050718. [DOI] [PubMed] [Google Scholar]
- 9.Testai L, Martelli A, Cristofaro M, Breschi MC, Calderone V. Cardioprotective effects of different flavonoids against myocardial ischaemia/reperfusion injury in Langendorff-perfused rat hearts. J Pharm Pharmacol. 2013;65:750–756. doi: 10.1111/jphp.12032. [DOI] [PubMed] [Google Scholar]
- 10.Subburaman S, Ganesan K, Ramachandran M. Protective role of naringenin against doxorubicin-induced cardiotoxicity in a rat model: Histopathology and mRNA expression profile studies. J Environ Pathol Toxicol Oncol. 2014;33:363–376. doi: 10.1615/JEnvironPatholToxicolOncol.2014010625. [DOI] [PubMed] [Google Scholar]
- 11.Liu X, Wang N, Fan S, Zheng X, Yang Y, Zhu Y, Lu Y, Chen Q, Zhou H, Zheng J. The citrus flavonoid naringenin confers protection in a murine endotoxaemia model through AMPK-ATF3-dependent negative regulation of the TLR4 signalling pathway. Sci Rep. 2016;6:39735. doi: 10.1038/srep39735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang K, Chen Z, Huang L, Meng B, Zhou X, Wen X, Ren D. Naringenin reduces oxidative stress and improves mitochondrial dysfunction via activation of the Nrf2/ARE signaling pathway in neurons. Int J Mol Med. 2017;40:1582–1590. doi: 10.3892/ijmm.2017.3134. [DOI] [PubMed] [Google Scholar]
- 13.Ren B, Qin W, Wu F, Wang S, Pan C, Wang L, Zeng B, Ma S, Liang J. Apigenin and naringenin regulate glucose and lipid metabolism, and ameliorate vascular dysfunction in type 2 diabetic rats. Eur J Pharmacol. 2016;773:13–23. doi: 10.1016/j.ejphar.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Zaragozá C, Monserrat J, Mantecón C, Villaescusa L, Zaragozá F, Álvarez-Mon M. Antiplatelet activity of flavonoid and coumarin drugs. Vascul Pharmacol. 2016;87:139–149. doi: 10.1016/j.vph.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Alam MA, Kauter K, Brown L. Naringin improves diet-induced cardiovascular dysfunction and obesity in high carbohydrate, high fat diet-fed rats. Nutrients. 2013;5:637–650. doi: 10.3390/nu5030637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Samak M, Fatullayev J, Sabashnikov A, Zeriouh M, Schmack B, Farag M, Popov AF, Dohmen PM, Choi YH, Wahlers T, Weymann A. Cardiac hypertrophy: An introduction to molecular and cellular basis. Med Sci Monit Basic Res. 2016;22:75–79. doi: 10.12659/MSMBR.900437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerdts E, Okin PM, Boman K, Wachtell K, Nieminen MS, Dahlöf B, Devereux RB. Association of heart failure hospitalizations with combined electrocardiography and echocardiography criteria for left ventricular hypertrophy. Am J Hypertens. 2012;25:678–683. doi: 10.1038/ajh.2012.31. [DOI] [PubMed] [Google Scholar]
- 18.Aronow WS, Ahn C, Kronzon I, Koenigsberg M. Congestive heart failure, coronary events and atherothrombotic brain infarction in elderly blacks and whites with systemic hypertension and with and without echocardiographic and electrocardiographic evidence of left ventricular hypertrophy. Am J Cardiol. 1991;67:295–299. doi: 10.1016/0002-9149(91)90562-Y. [DOI] [PubMed] [Google Scholar]
- 19.Zhu YC, Zhu YZ, Gohlke P, Stauss HM, Unger T. Effects of angiotensin-converting enzyme inhibition and angiotensin II AT1 receptor antagonism on cardiac parameters in left ventricular hypertrophy. Am J Cardiol. 1997;80:110A–117A. doi: 10.1016/S0002-9149(97)00465-7. [DOI] [PubMed] [Google Scholar]
- 20.Zhang N, Yang Z, Yuan Y, Li F, Liu Y, Ma Z, Liao H, Bian Z, Zhang Y, Zhou H, et al. Naringenin attenuates pressure overload-induced cardiac hypertrophy. Exp Ther Med. 2015;10:2206–2212. doi: 10.3892/etm.2015.2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.