Abstract
Background
In Australia there is commitment to developing interventions that will ‘Close the Gap’ between the health and welfare of Indigenous and non-Indigenous Australians and recognition that early childhood interventions offer the greatest potential for long term change. Nurse led sustained home visiting programs are considered an effective way to deliver a health and parenting service, however there is little international or Australian evidence that demonstrates the effectiveness of these programs for Aboriginal infants. This protocol describes the Bulundidi Gudaga Study, a quasi-experimental design, comparing three cohorts of families from the Macarthur region in south western Sydney to explore the effectiveness of the Maternal Early Childhood Sustained Home-visiting (MECSH) program for Aboriginal families.
Methods
Mothers were recruited when booking into the local hospital for perinatal care and families are followed up until child is age 4 years. Participants are from three distinct cohorts: Aboriginal MECSH intervention cohort (Group A), Non-Aboriginal MECSH intervention cohort (Group B) and Aboriginal non-intervention cohort (Group C). Eligible mothers were those identified as at risk during the Safe Start assessment conducted by antenatal clinic midwives. Mothers in Group A were eligible if they were pregnant with an Aboriginal infant. Mothers in Group B were eligible if they were pregnant with a non-Aboriginal infant. Mothers in Group C are part of the Gudaga descriptive cohort study and were recruited between October 2005 and May 2007. The difference in duration of breastfeeding, child body mass index, and child development outcomes at 18 months and 4 years of age will be measured as primary outcomes. We will also evaluate the intervention effect on secondary measures including: child dental health; the way the program is received; patterns of child health and illness; patterns of maternal health, health knowledge and behaviours; family and environmental conditions; and service usage for mothers and families.
Discussion
Involving local Aboriginal research and intervention staff and investing in established relationships between the research team and the local Aboriginal community is enabling this study to generate evidence regarding the effectiveness of interventions that are feasible to implement and sustainable in the context of Aboriginal communities and local service systems.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12616001721493 Registered 14 Dec 2016. Retrospectively registered.
Keywords: Australian Aboriginal families, Home visiting, Early intervention, Child development, Community health services, Perinatal care, Postnatal care, Primary prevention, Parenting education, MECSH program
Background
Indigenous children in Australia have some of the poorest health and welfare outcomes in the OECD [1]. In Australia there is a commitment to developing interventions that will ‘Close the Gap’ between the health and welfare of Indigenous and non-Indigenous Australians [2] and recognition that early childhood interventions offer the greatest potential for long term change [3]. Early childhood home visiting has been adopted as a key strategy. However the applicability and effectiveness of home visiting interventions has not been demonstrated with Indigenous families, particularly in urban environments.
Over the past decades, a number of interventions have been developed to improve birth outcomes for Indigenous infants. For example, in the Strong Women Strong Babies Strong Culture program in the Northern Territory senior community women visited pregnant Indigenous women to improve attendance at antenatal services and maternal health knowledge and behaviour, with mixed results in four communities [4, 5]. The Ngua Gundi program in Rockhampton, Queensland, provided antenatal home visiting, some postnatal home visiting and support for postnatal groups [6], and whilst there is evaluation evidence that the women liked the program, outcomes have not been published. Also in Queensland the evaluation of the Townsville Mums and Bubs program [7] provides an integrated model of antenatal shared care and has demonstrated improved early presentation for antenatal care, increased number of antenatal visits, and reduced rate of pre-term births, however, birth weight and rates of perinatal mortality were unchanged. The NSW Aboriginal Maternal Infant Health Strategy [8] employs a midwife and Aboriginal Health Worker to provide community-based antenatal services for Aboriginal women, and has demonstrated results similar to the Townsville program. In contrast to the antenatal focus of these programs, the South Australian Family Home Visiting program includes targeting of inter alia families of Indigenous infants and commences postnatally, continuing to child-age 2 years. This service, delivered by mainstream (non-Indigenous) child health nurses has been shown to be acceptable to families and achieved some positive outcomes in parent feelings of attachment and parental role satisfaction [9]. None of these programs, however, provides the continuity of care through pregnancy, infancy and early childhood that has been demonstrated to be effective in trials of sustained nurse home visiting (SNHV) in non-Indigenous populations [10].
Home visiting programs comprising intensive, structured and sustained visits by professionals (usually nurses) commencing antenatally and continuing over the first two years of life show promise in promoting child health and family functioning, and ameliorating disadvantage. When supported by SNHV, trials (predominantly overseas with non-Indigenous communities) have shown a positive effect on parenting attitudes and behaviours and on child cognitive and socioemotional outcomes [11]. This international evidence, however, comes mainly from tightly controlled efficacy trials; much less has been documented about the effectiveness of such programs in practice in the Australian context.
SNHV is now a key government strategy to ‘Close the Gap’ in life expectancy between Indigenous and non-Indigenous Australians with both State and Federal governments investing in improved maternal and child health services for Indigenous families. For example, the Federal Government has invested over $37 million in implementing the Nurse Family Partnership model [12] for Aboriginal families, which has been subject to a formative evaluation only. There is little international or Australian evidence that demonstrates the effectiveness of SNHV for Indigenous infants.
The Maternal (formerly Miller) Early Childhood Sustained Home-visiting (MECSH) program is an Australian-developed structured program of sustained nurse home visiting commencing antenatally and continuing through to child-age 2 years. MECSH is focused on: children’s health and development; parental aspirations for themselves and their child/ren, and a structured child development parent education program. A key strategy is continuity of the nurse home visitor. A randomised trial of the MECSH program, delivered by child health nurses within the context of existing community health service structures, has demonstrated effectiveness in improving the health, health behaviours and the quality of the home environment for children’s development of mothers assessed antenatally as having risk of poorer maternal and/or child outcomes living in a disadvantaged multicultural community in south western Sydney, New South Wales (NSW), Australia. Seventeen (8.5%) of the children in the MECSH trial were from Aboriginal families (note: ‘Aboriginal’ is the preferred term for description of Indigenous persons in NSW). The mothers of Aboriginal children who received the MECSH intervention were highly satisfied with the program, had a rate of retention in the study equivalent to mothers of non-Aboriginal children, and, although not statistically demonstrable, reported positive outcomes in duration of breastfeeding and child development at 18 months compared with Aboriginal mothers in the comparison, non-intervention group. These data suggest that the MECSH program may be an appropriate strategy to improve the health and development of Aboriginal children. The current study is applying this experience gained from the MECSH study, together with the knowledge of the issues for families of Aboriginal infants in an urban community gained from the Gudaga cohort study [13], to determine whether SNHV is effective in “Closing the Gap” for urban Aboriginal families, measuring both proximal outcomes during and at the conclusion of the intervention at child age 2 years, and also longer-term post-intervention outcomes during the pre-school years.
This study is thus generating Australian evidence regarding the effectiveness of interventions that are feasible to implement and sustainable in the context of the local service systems. The interventions aim to reduce the impact of social and environmental factors predisposing urban Aboriginal infants and children to ill health and reducing their life potential. This study is the first study internationally to examine the immediate and longer-term effectiveness of a comprehensive SNHV program commencing antenatally and continuing to child-age 2 years for families of Indigenous infants, with follow-up to child age 4 years.
Research question and hypotheses
Primary research question
What are the differences in length of time breastfeeding, child development at 18 months, and child body mass index (BMI) and developmental outcomes at 4 years of age between Aboriginal children of vulnerable mothers (at risk of poorer maternal and child health and development outcomes) receiving SNHV (Group A) and
non-Aboriginal children of a matched contemporary cohort of vulnerable mothers receiving SNHV (Group B)?
an historical cohort of Aboriginal children of vulnerable mothers who did not receive SNHV intervention (Group C)?
Hypotheses
There will be no significant differences in the primary outcomes between Aboriginal children of vulnerable mothers receiving SNHV (Group A) and non-Aboriginal children in a matched contemporary cohort receiving SNHV (Group B).
- There will be a difference between Aboriginal children of vulnerable mothers receiving SNHV (Group A) and Aboriginal children in the historical cohort who did not receive SNHV (Group C) of more than:
-
(i)5 weeks duration of breastfeeding, and
-
(ii)5 points in the age standardised Griffiths [14] Quotient (GQ) measure of child development at 18 months compared with Group C GQ measured at 12 months.
-
(iii)15% difference in proportion of children overweight/obese at 4 years.
-
(iv)5 points difference in the Griffiths Quotient (GQ) at 4 years; and 0.5SD difference in child vocabulary development at 4 years.
-
(i)
Secondary research questions
What are the differences in program implementation for, and the way the program is received by mothers and families of Aboriginal and non-Aboriginal children receiving SNHV?
What are the patterns of health and illness for Aboriginal compared with non-Aboriginal children of mothers receiving SNHV, and compared with Aboriginal children who do not receive intervention?
What are the patterns of maternal health and health knowledge and behaviours, family and environmental conditions and service usage for mothers and families of Aboriginal compared with non-Aboriginal children receiving SNHV, and compared with Aboriginal children who do not receive intervention?
Methods/Design
Setting
The study is being conducted in the Macarthur region of south-western Sydney, Australia. The Macarthur region (Campbelltown, Camden and Wollondilly local government areas) has one of the largest Aboriginal populations in New South Wales (NSW) comprising 8337 people: 3.3% of the regional population of 254,219 and 4.0% of the state Aboriginal population [15].
Conceptual framework
The study applies an ecological framework, recognising that the health, development and wellbeing of children is the product of complex interacting factors at the individual, family and community level [16]. Interventions that seek to achieve the outcome of healthier children need to also address the health of parents (particularly mothers), family and social functioning, and the environment. The intervention and research also recognises Aboriginal frameworks for reciprocity, respect, equality and responsibility; recognising that the researchers, SNHV program providers and the families all contribute; and that contribution is respected, recognised and valued. The study is conducted in a culturally safe environment through the involvement of Aboriginal research and intervention staff and behaviour that maintains coherence of Aboriginal values and cultures [17, 18], and investment in established relationships between the research team and the local Aboriginal community [19].
Trial design
The study uses a quasi-experimental design comparing three cohorts of families to explore the effectiveness of SNHV for Aboriginal families. The study design recognises that the use of a randomised control group design is inappropriate in the context of this research. There was apprehension within the Aboriginal community about randomisation associated with equity and the investigators wished to demonstrate a respect for the views of the local Aboriginal community [18], based on discussions with local Aboriginal representatives.
Participants, eligibility criteria and recruitment
Eligibility and recruitment of intervention groups (Groups A and B)
In this study, eligible mothers were those identified as at risk using criteria identified through the responses given by the expectant mother at the routine Safe Start [20] assessment conducted by antenatal clinic midwives for all mothers booking into the local hospital for perinatal care. Mothers in Group A were eligible if they were pregnant with an Aboriginal infant, that is, they or the baby’s father identified as an Aboriginal person, and had one or more of the following vulnerability factors identified from the routine assessment:
maternal age under 20 years;
unsupported parent determined as those mothers who were not married or living with a partner;
late antenatal care (after 20 weeks);
major stressors in the past 12 months determined by a positive response to the question “Have you had any major stressors, changes or losses recently?”;
current or history of mental health problem or disorder determined by the mother reporting current or past treatment for emotional problems;
current probable psychosocial distress determined by an Edinburgh Depression Scale [21] score of 10 or more;
relationship issues with the mother’s parents if they report that they were hurt or abused as a child in any way;
current substance misuse determined by a positive response to questions about the use of prohibited substances and/or alcohol;
history of domestic violence based on reports that they get so angry that they hit or hurt their partner, that their partner or anyone else hits them, hurts them or makes them afraid.
Mothers in Group B were eligible if they were pregnant with a non-Aboriginal infant, that is, neither they nor the baby’s father identified as an Aboriginal person, and had one or more of the vulnerability factors described above. In order to match the demographic profile of Groups A and B, the recruitment of Group B commenced after Group A, with the intent of, as much as possible, matching participants on age and suburb of residence: Group A was recruited between October 2011 and March 2013, and Group B between January 2013 and December 2013.
Mothers who had insufficient English-language proficiency to undertake the antenatal risk assessment in English (that is, those who required the use of a translated assessment instrument or an interpreter) were ineligible to participate. All mothers in the area not eligible to be recruited to participate in the study or eligible mothers who declined to participate received usual care.
Contact details of all eligible mothers were collected by the Senior Research Officer on a weekly basis and entered onto a database. The project officer then telephoned each eligible mother to ask for verbal consent to visit them at home to explain the study in detail and written consent to participate in the study was obtained. The demographic and risk profile of the three study groups is presented in Table 1.
Table 1.
Demographic and vulnerability profile
| Group A | Group B | Group C | |
|---|---|---|---|
| Demographic (n) | 149 | 80 | 132 |
| Mean age (SD) at parturition | 25.97 (6.17) | 27.96 (7.10) | 25.39 (6.27) |
| Median age (years) | 25.5 | 27.5 | 24.3 |
| Age range (years) | 15–44 | 16–41 | 16–42 |
| First time mother n (%) | 51 (34.2) | 38 (47.5) | 43 (32.6) |
| Living in lowest Socio-Economic Index for Areas (SEIFA) n (%) | 77 (51.7) | 28 (35.0) | 79 (59.8) |
| Vulnerabilities at maternity booking (Safe Start assessment) | |||
| Age < 20 years n (%) | 29 (19.5) | 11 (13.8) | 35 (26.7) |
| Not married or living with partner n (%a) (Data missing: A = 5%, B = 6%, C = 10%) | 34 (22.8) | 17 (21.3) | 72 (54.5) |
| Late antenatal care n (%a) (Data missing: A = 3% B = 15% C = 20%) | 41 (27.5) | 26 (32.5) | 31 (23.5) |
| Major stressor n (%a) (Data missing: A = 4% B = 6% C = 7%) | 77 (51.7) | 71 (88.8) | 52 (39.4) |
| Mental health issue requiring treatment n (%a) (Data missing: A = 3% B = 20% C = 10%) | 71 (47.7) | 49 (61.3) | 31 (23.5) |
| EDS ≥10 at booking n (%a) (Data missing: A = 4% B = 2.5% C = 14%) | 34 (22.8) | 43 (53.8) | 26 (19.7) |
| Abused as child n (%a) (Data missing: A = 7% B = 48% C = 8%) | 45 (30.2) | 15 (18.8) | 32 (24.2) |
| Substance misuse n (%a) (Data missing: A = 79% B = 9% C = 11%) | 17 (11.5) | 8 (10.3) | 17 (12.9) |
| Family violence n (%a) (Data missing: A = 34% B = 41% C = 8%) | 6 (4.0) | 10 (12.5) | 26 (19.7) |
| Number of risks, mean (SD) | 2.49 (1.36) | 3.29 (1.37) | 2.57 (1.61) |
| Risk range | 1–6 | 1–7 | 1–7 |
| Median number of risks | 2 | 3 | 2 |
aPresence of vulnerability recorded as percentage of total group N
Eligibility and recruitment of Aboriginal non-intervention group (Group C)
The Gudaga cohort (n = 149) was recruited between October 2005 and May 2007. Recruitment was conducted in the postnatal ward of Campbelltown Hospital [13]. All infants whose mothers identified them as having an Aboriginal mother or father were eligible to participate. The subset of families in the Gudaga cohort who were assessed at the routine assessment by midwives antenatally as having one or more of the above listed vulnerability factors are included in the historical non-intervention group (n = 132).
Sample size in relation to study effect sizes
Recruitment of 149 participants (Group A) and 80 (Group B) was achieved. A sample size of 75 participants per intervention Group A, Group B and 132 participants in the non-intervention Group C has power of 0.80 at the 95% level to detect a 5 point difference in the Griffiths Quotient (GQ), and a 5 week longer duration in breastfeeding.
The effect size of 5 weeks duration in breastfeeding is based on the Group C data that showed at 2–3 weeks postnatally (n = 122) only 38.6% of mothers were still breastfeeding. The MECSH study demonstrated that mothers of Aboriginal children who received the SNHV intervention breastfed for an average of 14 weeks compared with 8 weeks for mothers of Aboriginal children in the non-intervention control group.
Results for the broader Gudaga cohort show that 36.9% of children were overweight/obese at 24 months [22]. Evidence suggests that the proportion of overweight/obese children in the cohort will rise in the preschool years [23]. It is expected that the intervention will reduce the proportion of overweight/obesity by at least 17% in the immediate prior-to-school period.
The effect size of 5 points in the GQ is also based on data from the Group C cohort that showed a mean GQ of 95.35 (SD 10.4) compared with the population norm mean of 100.5 (SD 11.8) and also unpublished data from the MECSH study that demonstrated that Aboriginal children who received the SNHV intervention (n = 7) reported a mean mental development score of 101.0 compared with 96.3 for Aboriginal children in the non-intervention control group.
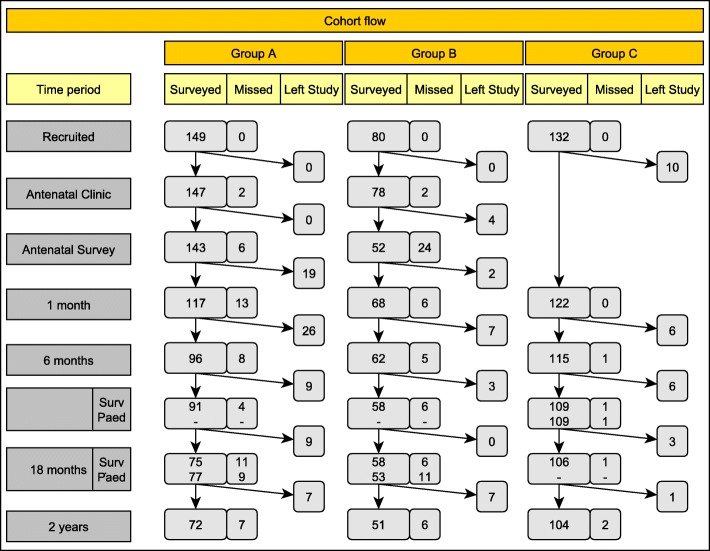
Retention and attrition
The retention of participants in the trial to child-age 2 years is presented in Fig. 1. Retention of Group C to child age 4 years was 75% (n = 99). Active retention strategies have been and continue to be in place including: asking mothers to provide the name and phone number of two relatives or friends who could be contacted by the researchers to reach them; providing mothers with details of the research team to advise of changes in contact details; sending thank you notes and relevant holiday greeting cards to all participants [24]; using project officers experienced in interviewing families in their own home and trained in the sensitive administration of the data collection tools. Importantly, the project officers employed to work with the Aboriginal families (Group A) are local Aboriginal women and all project officers wear a uniform clearly identifying them with the program. Each time a data collection visit is made a health pack including a small gift for the mother and baby is provided as a thank you for her time. The small gifts included in the health packs are specifically designed to engender a sense of involvement in the project. Further, the research team work closely with the local Aboriginal community through the Aboriginal community controlled medical service, the local community chose an Aboriginal name for the program (Bulundidi Gudaga, meaning happy baby from healthy pregnancy in the local language), and information about the program was and continues to be extensively disseminated within the community.
Fig. 1.
Recruitment and retention flowchart
Intervention
Intervention groups (Groups A and B)
The intervention groups received the MECSH program [25] provided by the local public community health service. The program consisted of at least 25 home visits (actual number of visits determined by need) primarily by the same program nurse, commencing at (on average) 26 weeks gestation and continuing through the first 2 years post birth. The nurse was supported by a social worker, and all nurses working with Aboriginal families were also supported by Aboriginal Health Workers. All intervention staff (nurses, Aboriginal health workers and social worker) received additional training in the program model and cultural competency. The MECSH program home visits were standardised as follows:
A minimum of three antenatal home visits and postnatal visits within one week of birth, and then at least weekly until 6 weeks; second weekly until 12 weeks; monthly to 6 months; bi-monthly until 2 years. The content of each home visit was individually tailored to the mother’s needs, skills, strengths, capacity, and cultural needs.
Structured child development parent education program: Parents as Teachers [26].
Explicit strategies to facilitate access to Aboriginal and non-Aboriginal early childhood health services, volunteer home visiting services and family support services within the Macarthur area.
Encouragement for families to attend group activities and link into community activities in the local area.
Historical Aboriginal non-intervention group (Group C)
The non-intervention group received usual care for families in the Macarthur area, that is:
Antenatal care according to NSW Health maternity care and Safe Start [20] guidelines and protocols;
One postnatal home visit by a nurse from the regular child and family nursing service (within 2 weeks of baby’s birth);
Additional postnatal home or clinic visits with the regular child and family nursing service as indicated by protocols in usual care;
Volunteer home visiting services and family support services within the local area, as available.
Hence the key differences in the intervention were: home visiting commencing antenatally; continuity of care by the same nurse throughout the 2½ year program; care provided by nurses with additional individualised training in the program model; standardised structured antenatal and postnatal home visiting program to the child’s second birthday; dedicated social worker; dedicated Aboriginal Health Workers (Group A only); structured child development parent education program; group activities and proactive strategies to establish links to community activities.
Program adaptation, implementation and monitoring
The MECSH program was adapted to provide a culturally appropriate intervention for Aboriginal families. In 2008, a Health Impact Assessment (HIA) [27] was undertaken in consultation with the local Aboriginal community, the Aboriginal medical service and the community health service, to identify and mitigate any aspects of the MECSH intervention that may impact negatively on Aboriginal families. For example, the HIA recommended that an Aboriginal Health Worker be present at the initial contact between the nurse and each Aboriginal family, and continue to visit and support the families and nurses throughout the intervention.
Program documentation (minutes of staff meetings, procedures and protocols, training) were continually reviewed to identify: barriers and facilitators to the uptake and retention in the intervention program, cultural adaptation, workforce skills training, and monitoring of supervision needs and workload; actively promoting links between health home visiting, child protection services, and non-government agencies. Nurses completed checklists on completion of each home visit, detailing the interventions and tasks undertaken. The collated data were used to identify the content of interventions related to the age of the child for Aboriginal and non-Aboriginal families, and to provide ongoing quality feedback to the intervention team.
Data collection, management and analysis
Data collection by trained project officers is undertaken at recruitment antenatally (Groups A and B only), and then at 1, 6, 12, 18, 24, 36 and 48 months postnatally. On each occasion, a 30 min face-to-face questionnaire is completed by the child’s primary carer (usually mother). At 18 and 48 months the children attend a health and development assessment conducted by a paediatrician at the local hospital. Where needed, transport to the hospital or a home-based assessment is provided. At 48 months the children’s dental health will be assessed by a trained dental therapist at the local community health centre or the child’s home.
Data coding, security and monitoring
The participants’ identity is protected by assigning a unique ID number to each primary carer/child dyad. Questionnaire data were recorded on paper forms for surveys up to 18 months with all paper based information filed under the participants ID number in locked filing cabinets in a secure building. Questionnaire data for 18 months onwards are recorded electronically using a secure online data entry platform and database with the data entered via tablets on site by the project officers in collaboration with the parents. The online platform provides data collection, backup and security services with the data collected and recorded using study ID numbers only. Health, development and dental assessment data are scored by the assessor on paper forms and stored in a secure building. All study data are input into a SPSS database and stored on a secure, password protected network accessible only by research staff. The study did not employ a data monitoring committee as the intervention has minimal risks. Data monitoring was conducted with the project officers reporting weekly to the project manager with any issues for discussion and documentation.
Critical events
At each contact the occurrence of any of the following events is noted: maternal death, child death, or child placement in out-of-home care. Descriptive analyses will be undertaken as the incidence of these events is low in the Australian population.
Outcomes
Primary and secondary outcomes are detailed in Table 2. Where appropriate, measures have been validated and/or benchmarked against the routine data collections of NSW Health (Child Health Survey) and national data collections (such as National Perinatal Statistics).
Table 2.
Study measures
| Measures | Rationale | Collection Schedule | Instrument | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Postnatal Month | ||||||||||||
| A | 1 | 6 | 12 | 18 | 24 | 36 | 48 | |||||
| Primary Outcomes | Breastfeeding | Important for health/development, poor in Aboriginal children [33]. | ● | ● | ● | Parental questionnaire (CHS items 37,39) collated at 12 months [34]. | ||||||
| Body mass index | Childhood obesity is increasing. Home visiting interventions have had impact, although not sustained over time [35]. | ● | ● | Child weight and height; BMI = kg/m2. | ||||||||
| Child development | Studies reporting significantly lower levels of performance for Indigenous children compared to their non-Indigenous counterparts on cognitive and language tasks at school entry [36, 37]. | ● | ● | Griffiths child developmental assessment [14]. | ||||||||
| Child vocabulary development | ● | Peabody Picture Vocabulary Test – 4th Edition [38]. | ||||||||||
| Secondary Outcomes | Child | Child birthweight | Low birth weight more prevalent in Aboriginal children [33]. | ● | Birth weight recorded in perinatal statistics. | |||||||
| Child health | Child health is associated with health in later life [39]. | ● | ● | ● | ● | ● | ● | ● | General health (CHS item 97) [34]; Paediatric assessment (18 months). | |||
| Child dental health | Dental disease is an important cause of potentially preventable hospitalisations particularly for young Aboriginal children age 0–4 [40]. | ● | Dental assessment (dmft: decayed, missing and filled primary teeth); Significant Caries Index (SiC). | |||||||||
| Illnesses and injury | Aboriginal children have increased hospital admissions for respiratory illness, ear disease, gastroenteritis [41, 42]. | ● | ● | ● | ● | ● | ● | ● | Parental questionnaire; Paediatric assessment (18 months); Hospital data collections. Collated at 24 and 48 months. |
|||
| Age at first solids | Disadvantaged mothers more likely to introduce solids too early [43]. | ● | ● | Parental questionnaire (CHS items 48–49), collated at 12 months) [34]. | ||||||||
| Age appropriate immunisation | Contact with health professionals is influential in immunisation [44]. | ● | ● | ● | ● | Parental questionnaire validated by Child Personal Health Record (Blue Book) [45]. | ||||||
| Mother | Maternal enablement | Enabling mother is a key principle of SNHV [10, 46, 47]. | ● | Modified Patient Enablement Instrument (Groups A and B only) [48]. | ||||||||
| Parental child developmental enablement | Parental enablement of their child’s development is a key purpose of the intervention. | ● | ● | ● | ● | Modified Patient Enablement Instrument (Groups A and B only) [48]. | ||||||
| Knowledge of SIDS risk factors | Disadvantaged families less likely to act to reduce risk of SIDS [49]. | ● | ● | Parental questionnaire [50]. | ||||||||
| Maternal health | Associated with child health. | ● | ● | 12-Item Short Form Health Survey (SF-12) [51]. | ||||||||
| Maternal smoking | Risk factor for adverse perinatal outcomes [33]. | ● | ● | ● | ● | ● | ● | ● | ● | Fagerstrom test for nicotine dependence [52]. | ||
| Family | Maternal social support | Positively influences families, parents, children [53]. | ● | ● | ● | ● | ● | ● | ● | ● | Parental questionnaire (CHS items 191–196) [34]. | |
| Family functioning | Affects health and wellbeing of children [53]. | ● | ● | ● | ● | ● | ● | ● | ● | McMaster Family Assessment Device [54]. | ||
| Home | Home environment | Stimulating environment associated with infant development [55]. | ● | ● | ● | HOME Inventory [56]. | ||||||
| Household smoking | Increases risk of child respiratory problems [57]. | ● | ● | ● | ● | ● | ● | ● | ● | Parental questionnaire (CHS items 291–294) [34]. | ||
| Service use | Use of and satisfaction with services | Parenting programs are effective in improving child behaviour [58]. | ● | ● | ● | ● | ● | ● | ● | ● | Parental questionnaire (CHS items 15, 18, 178–189, 285, 290) [34]. | |
| Mother satisfaction with home visiting service | Mothers are more likely to make use of services that are accessible and acceptable [59]. | ● | ● | ● | ● | ● | Parental questionnaire (Modified PSQ-18 Groups A and B only) [50]; Program retention. | |||||
Statistical methods
Microsoft Access is used to manage the data collection. The data will be extracted and analyses conducted using the latest version of SPSS. Descriptive analyses will be used to profile the characteristics of each Group. Although stratification will be applied during the recruitment processes for Group B, it is recognised that the three groups may differ on the distribution of demographic and risk factors impacting on treatment effects. To account for group differences in baseline demographic and risk profiles, propensity score analysis will be used to balance the differences in groups before treatment [28, 29].
Families recruited into Groups A and B are retained in the study regardless of whether they continued to receive the intervention. All analyses will be intention to treat. Comparison of the adjusted treatment effects for primary outcomes (duration [number of weeks] of breastfeeding, child development and educational development) will be made using t-tests, comparing outcomes of (1) Aboriginal children who did (Group A) and did not receive SNHV (Group C), and (2) Aboriginal and non-Aboriginal children receiving SNHV (Group A compared with Group B). Patterns of difference in secondary outcomes between the three groups will be analysed using Chi-Square test for proportions (categorical data) and ANOVA (continuous data), together with 95% confidence intervals. Multilevel analyses will be used for analyses of secondary outcomes collected at multiple time points (e.g., maternal health), with time at level 1 and the repeated outcome at level 2. Multiple regression analyses will be used to identify the impact of secondary measures as potential mediators or moderators of effects on the primary outcomes, for example, the impact of social support on the duration of breastfeeding, and the impact of the quality of the home environment and maternal health on child development.
Discussion
This study is the first Australian trial of the effectiveness of sustained nurse home visiting for families of Aboriginal infants, and one of few conducted worldwide with Indigenous communities. Comparison with an historical non-intervention cohort of Aboriginal infants will allow assessment of the effectiveness of the intervention compared with usual care. In addition, enrolment of a contemporary study cohort of families of non-Aboriginal infants who also received sustained nurse home visiting provided by the same local health service provider in the same community will allow assessment of whether this intervention can ‘close the gap’ that exists in the health and development of Australian Indigenous and non-Indigenous children.
The intervention was based in the local public community health service and utilised the mainstream child and family health nurses and social workers, with the addition of Aboriginal Health Workers for the Aboriginal families receiving the intervention. By trialing the effectiveness of mainstream service provision for this population, the program is more likely to be replicable at the whole of population level than programs relying on provision by only Indigenous staff, who are considerably underrepresented in Australian child and family health professions.
The research is being conducted in partnership with the local service providers and Aboriginal community, who will support the communication of the study results through professional and community events, policy briefings and joint publications.
A significant limitation of the study was the number of families recruited to participate. Participation was limited by the maximum caseload that could be assigned to the number of trained program nurses. This limitation on recruitment numbers was further exacerbated by poorer than predicted retention rates in the intervention cohorts, and the Aboriginal intervention cohort in particular. Unfortunately, intervention participation could only be maintained for those who continually resided in the local area for the duration of the study, unlike the historical non-intervention group whose participation was not associated with an intervention. As has been the case with other home visiting research [30], attrition mainly occurred early in the research, predominantly in the antenatal period and the first month post-birth. This loss of participants was particularly high for the Aboriginal intervention group (Group A), with an overall loss of 30% of participants at those times. There is evidence [31] that in urban locations the Indigenous population is more mobile than the non-Indigenous population, and that Indigenous women are most mobile in young adulthood up to 30 years of age; the main age group in this study. The loss of participants in the perinatal period may reflect such mobility. The much higher retention rate in the historic cohort (80% at child-age 2 years) may also reflect postnatal study recruitment, rather than antenatal recruitment as in the case of the intervention groups, and therefore may not be fully indicative of the number of Aboriginal women presenting for antenatal care in the recruiting hospital. The low rates of participation at each data point may reduce the power of the study to detect small and moderate effects of the intervention. This may be moderated by the collection of the same data items at multiple data points, which should facilitate imputation of values for data points missed by individual participants and the use of multilevel analyses, however, this will remain a limitation for cross-sectional analyses.
Inferences about outcome differences between the Aboriginal and non-Aboriginal intervention groups may also be affected by the differences in the demographic and risk profile of the participating families. It was possible to match Groups A and B on maternal age, but not on suburb of residence, with Group A (like historic Group C) more likely to live in low socio-economic areas. There were also considerable issues of inconsistency in the routine Safe Start [20] assessment conducted by antenatal clinic midwives in either the asking, or recording of risk factors and vulnerabilities between the groups. Group B (non-Aboriginal intervention group) were much less likely to have an answer recorded regarding whether they had been abused as a child, or about mental health issues, whilst Group A (Aboriginal intervention group) were less likely to have data recorded about substance misuse. There also seems to have been a temporal change in recording of family violence with both current groups (A and B) being less likely to have these data recorded than the historic group (C Aboriginal non-intervention group). Propensity scoring will be used to correct recorded differences. For the purposes of identifying families to be offered the intervention, however, the assumption was made that non-recording of the vulnerability factor was an indicator of the absence of the risk. It is not possible to know whether the mother was not asked or whether she was asked and the factor was absent and hence not recorded.
The ‘Bulundidi Gudaga’ trial has been designed to provide Australian evidence of whether a sustained nurse home visiting intervention, adapted to meet the needs and preferences of an urban Aboriginal population and delivered by local public community health services, can improve outcomes for Aboriginal children and their families, and close the gap between them and their non-Aboriginal contemporaries. Although limited by the sample size and study retention and participation rates, it is envisaged that the comprehensive, culturally adapted intervention will support significant child health and development improvements that are sustained beyond the 2 year intervention to child age 4 years.
Acknowledgements
We would like to acknowledge the local Aboriginal community and participating families, the intervention, management and leadership team from the Local Health District, the research team involved in the data collection: Cheryl Jane Anderson, Natasha Bucknall and Sheryl Scharkie, project staff Jennifer Knight, Emma Elcombe for statistical assistance and Fiona Byrne for editorial support.
Funding
The research has been funded by the Australian National Health and Medical Research Council (NHMRC) project grants 630520, 510171 and 300439; CAGES Foundation (2015–2016) and the Vincent Fairfax Family Foundation to continue the study until child age 4 years (2017–2019).
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author LK. The data are not publicly available due to ownership of the data by the Aboriginal community.
Abbreviations
- BMI
Body Mass Index
- CHS
Child Health Survey
- GQ
Griffiths Quotient
- HIA
Health Impact Assessment
- HOME
Home Observation for Measurement of the Environment
- MECSH
Maternal Early Childhood Sustained Home-visiting
- NSW
New South Wales, Australia
- OECD
Organisation for Economic Co-operation and Development (OECD)
- PSQ
Patient Satisfaction Questionnaire
- SIDS
Sudden Infant Death Syndrome
- SNHV
Sustained Nurse Home Visiting
Authors’ contributions
LK led the study design and intervention, interpreted the data and drafted the manuscript. RG EC LJP CM EH MH AG HM contributed to the conception and design of the study, the revising of the manuscript, and read and approved the final version.
The study is approved by the South Western Sydney Local Health District Human Research Ethics Committee (HREC/10/LPOOL/98, HREC/15/LPOOL/361), the Aboriginal Health and Medical Research Council of NSW (739/10), UNSW Australia (HC10429) and Western Sydney University (RH12261).
The project officer telephoned each eligible mother to ask for verbal consent to visit them at home to explain the study in detail and written consent to participate in the study was obtained. In accordance with the guidelines of the Australian National Statement on Ethical Conduct in Human Research [32], ethics permission was granted to recruit participants over the age of 14 years with their own consent.
Not applicable.
The MECSH® program is a registered trademark of UNSW Australia and from 2016 for the duration of 5 years is being sublicensed to Western Sydney University. The authors declare that they have no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Lynn Kemp, Phone: +61 2 8738 9387, Email: Lynn.Kemp@westernsydney.edu.au.
Rebekah Grace, Email: R.Grace2@westernsydney.edu.au.
Elizabeth Comino, Email: e.comino@unsw.edu.au.
Lisa Jackson Pulver, Email: Lisa.Jackson-Pulver@westernsydney.edu.au.
Catherine McMahon, Email: cathy.mcmahon@mq.edu.au.
Elizabeth Harris, Email: e.harris@unsw.edu.au.
Mark Harris, Email: m.f.harris@unsw.edu.au.
Ajesh George, Email: A.George@westernsydney.edu.au.
Holly A. Mack, Email: H.Mack@westernsydney.edu.au
References
- 1.Australian Research Alliance for Children and Youth (ARACY). Report card 2018: The wellbeing of young Australians. Braddon, ACT: ARACY; 2018. http://www.aracy.org.au/projects/report-card-the-wellbeing-of-young-australians. Accessed 26 July 2018.
- 2.Commonwealth of Australia. Closing the gap: Prime Minister's report 2015. Canberra: Department of the Prime Minister and Cabinet; 2015.
- 3.World Health Organization Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health: Commission on Social Determinants of Health final report. Geneva: Commission on Social Determinants of Health, World Health Organization; 2008.
- 4.Mackerras D. Birthweight changes in the pilot phase of the strong women strong babies strong culture program in the Northern Territory. Aust N Z J Public Health. 2001;25(1):34–40. doi: 10.1111/j.1467-842X.2001.tb00547.x. [DOI] [PubMed] [Google Scholar]
- 5.Tursan D'Espaignet E, Measey ML, Carnegie MA, Mackerras D. Monitoring the 'Strong women, strong babies, strong culture Program': the first eight years. J Paediatr Child Health. 2003;39(9):668–672. doi: 10.1046/j.1440-1754.2003.00272.x. [DOI] [PubMed] [Google Scholar]
- 6.Dorman R. Ngua gundi (mother and child) program. Aborig Isl Health Work J. 1997;21(5):2–6. [PubMed] [Google Scholar]
- 7.Panaretto KS, Lee HM, Mitchell MR, Larkins SL, Manessis V, Buettner PG, Watson D. Impact of a collaborative shared antenatal care program for urban indigenous women: a prospective cohort study. Med J Aust. 2005;182(10):514–519. doi: 10.5694/j.1326-5377.2005.tb00017.x. [DOI] [PubMed] [Google Scholar]
- 8.NSW Department of Health. NSW Aboriginal Maternal and Infant Health Strategy Evaluation: Final Report. [North Sydney]: NSW Health; 2005. http://www.health.nsw.gov.au/kidsfamilies/MCFhealth/Documents/nsw-aboriginal-maternal-infant-strategy-evaluation.pdf. Accessed 21 Feb 2017.
- 9.Sawyer MG, Frost L, Bowering K, Lynch J. Effectiveness of nurse home-visiting for disadvantaged families: results of a natural experiment. BMJ Open. 2013;3:e002720. doi: 10.1136/bmjopen-2013-002720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olds DL, Sadler L, Kitzman H. Programs for parents of infants and toddlers: recent evidence from randomized trials. J Child Psychol Psychiatry Allied Discip. 2007;48(3–4):355–391. doi: 10.1111/j.1469-7610.2006.01702.x. [DOI] [PubMed] [Google Scholar]
- 11.Sweet MA, Appelbaum MI. Is home visiting an effective strategy? A meta-analytic review of home visiting programs for families with young children. Child Dev. 2004;75(5):1435–1456. doi: 10.1111/j.1467-8624.2004.00750.x. [DOI] [PubMed] [Google Scholar]
- 12.Olds DL. The nurse-family partnership: an evidence-based preventive intervention. Infant Ment Health J. 2006;27(1):5–25. doi: 10.1002/imhj.20077. [DOI] [PubMed] [Google Scholar]
- 13.Comino E, Craig P, Harris E, McDermott D, Harris M, Henry R, Jackson Pulver L, Kemp L, Knight J. The Gudaga study: establishing an Aboriginal birth cohort in an urban community. Aust N Z J Public Health. 2010;34(S1):S9–17. doi: 10.1111/j.1753-6405.2010.00546.x. [DOI] [PubMed] [Google Scholar]
- 14.Griffiths R, Huntley M. The Griffiths mental development scales (from birth to 2 years): manual. Henley-on-Thames: The Test Agency; 1996. [Google Scholar]
- 15.Australian Bureau of Statistics. Estimates of Aboriginal and Torres Strait Islander Australians, June 2011, 'Table 1, Estimated resident Aboriginal and Torres Strait Islander and non-Indigenous populations, Local Government Areas, Australia', data cube: Excel spreadsheet, cat no. 3238.0.55.001. Canberra, ACT: ABS; 2013. http://www.abs.gov.au/ausstats/abs@.nsf/mf/3238.0.55.001. Accessed 16 Mar 2017.
- 16.Jack G. Ecological influences on parenting and child development. Br J Soc Work. 2000;30(6):703–720. doi: 10.1093/bjsw/30.6.703. [DOI] [Google Scholar]
- 17.National Health and Medical Research Council. The NHMRC road map: A strategic framework for improving Aboriginal and Torres Strait Islander health through research. Canberra: NHMRC; 2002. [DOI] [PubMed]
- 18.National Health and Medical Research Council. Values and ethics: guidelines for ethical conduct in Aboriginal and Torres Strait Islander health research. Canberra: NHMRC; 2003.
- 19.Comino EJ, Knight J, Grace R, Kemp L, Wright DC. The Gudaga research program: a case study in undertaking research with an urban Aboriginal community. Aust Soc Work. 2016;69(4):443–55. doi: 10.1080/0312407X.2015.1131842. [DOI] [Google Scholar]
- 20.NSW Department of Health. NSW Health/Families NSW Supporting Families Early Package - Supporting Families Early Safe Start Strategic Policy. Sydney: NSW Health; 2010. http://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2010_016.pdf. Accessed 16 Mar 2017.
- 21.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 22.Webster V, Denney-Wilson E, Knight J, Comino E. Describing the growth and rapid weight gain of urban Australian Aboriginal infants. J Paediatr Child Health. 2013;49(4):303–8. [DOI] [PubMed]
- 23.Wake M, Hardy P, Canterford L, Sawyer M, Carlin JB. Overweight, obesity and girth of Australian preschoolers: prevalence and socio-economic correlates. Int J Obes. 2007;31(7):1044–1051. doi: 10.1038/sj.ijo.0803503. [DOI] [PubMed] [Google Scholar]
- 24.McKenzie M, Tulsky JP, Long HL, Chesney M, Moss A. Tracking and follow-up of marginalized populations: a review. J Health Care Poor Underserved. 1999;10(4):409–429. doi: 10.1353/hpu.2010.0697. [DOI] [PubMed] [Google Scholar]
- 25.Kemp L, Harris E, McMahon C, Matthey S, Vimpani G, Anderson T, Schmied V, Aslam H, Zapart S. Child and family outcomes of a long-term nurse home visitation program: a randomised controlled trial. Arch Dis Child. 2011;96(6):533–540. doi: 10.1136/adc.2010.196279. [DOI] [PubMed] [Google Scholar]
- 26.Wagner MM, Clayton SL. The parents as teachers program: results from two demonstrations. Futur Child. 1999;9(1):91–115. doi: 10.2307/1602723. [DOI] [PubMed] [Google Scholar]
- 27.European Centre for Health Policy Health Impact Assessment: Main concepts and suggested approach—The Gothenburg Consensus Paper. Brussels: WHO Regional Office for Europe; 1999. http://webarchive.nationalarchives.gov.uk/20170106084428/http://www.apho.org.uk/resource/item.aspx?RID=44163. Accessed 26 July 2018.
- 28.Pearl J. Causality: models, reasoning, and inference. 2. Cambridge: Cambridge University Press; 2009. [Google Scholar]
- 29.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. doi: 10.1093/biomet/70.1.41. [DOI] [Google Scholar]
- 30.Kemp L, Harris E, McMahon C, Matthey S, Vimpani G, Anderson T, Schmied V. Miller early childhood sustained home-visiting (MECSH) trial: design, method and sample description. BMC Public Health. 2008;8:424. doi: 10.1186/1471-2458-8-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Biddle N, Prout S. Indigenous temporary mobility: an analysis of the 2006 Census Snapshot. Canberra: Australian National University Centre for Aboriginal Economic Policy Research; 2009. CAEPR Working Paper No 55/2009. http://caepr.cass.anu.edu.au/sites/default/files/docs/CAEPRWP55_0.pdf. Accessed 26 July 2018.
- 32.National Health and Medical Research Council Australian Research Council Australian Vice-Chancellors' Committee. National Statement on Ethical Conduct in Human Research 2007 (updated May 2015). Canberra: Australian Government; 2007. https://www.nhmrc.gov.au/guidelines-publications/e72. Accessed 14 Jun 2017.
- 33.Australian Research Alliance for Children and Youth (ARACY), Allen Consulting Group. The wellbeing of young Australians: technical report. Woden, ACT: ARACY; 2008.
- 34.New South Wales Department of Health Centre for Epidemiology and Research New South Wales child health survey 2001. NSW Pub Health Bull. 2002;13(3):1–84. doi: 10.1071/nb02s22. [DOI] [PubMed] [Google Scholar]
- 35.Wen LM, Baur LA, Simpson JM, Xu H, Hayes AJ, Hardy LL, Williams M, Rissel C. Sustainability of effects of an early childhood obesity prevention trial over time: a further 3-year follow-up of the healthy beginnings trial. JAMA Pediatr. 2015;169(6):543–551. doi: 10.1001/jamapediatrics.2015.0258. [DOI] [PubMed] [Google Scholar]
- 36.Leigh A, Gong X. Estimating Cognitive Gaps between Indigenous and Non-Indigenous Australians. Canberra, ACT: Centre for Economic Policy Research, Australian National University; 2008. Discussion paper no 578. https://www.cbe.anu.edu.au/researchpapers/cepr/DP578.pdf. Accessed 16 Mar 2017.
- 37.McTurk N, Lea T, Robinson G, Nutton G, Carapetis JR. Defining and assessing the school readiness of Indigenous Australian children. Aust J Early Childhood. 2011;36(1):69-76.
- 38.Dunn LM, Dunn DM. PPVT-4: Peabody Picture Vocabulary Test. 4. San Antonio, TX: Pearson Assessments; 2007. [Google Scholar]
- 39.Najman JM, Aird R, Bor W, O'Callaghan M, Shuttlewood G, Williams GM. Socioeconomic inequalities in foetal and child health: a platform for adult health inequalities? A Better Start to Life. Brisbane: Queensland Health; 2000.
- 40.AIHW, Chrisopoulos S, Harford JE, Ellershaw A. Oral health and dental care in Australia: Key facts and figures 2015. Cat no DEN 229. Canberra: AIHW; 2016.
- 41.Trewin D, Madden R. The health and welfare of Australia's Aboriginal and Torres Strait Islander peoples 2005. Canberra: Australian Bureau of Statistics and Australian Institute of Health and Welfare; 2005.
- 42.Zubrick SK, Lawrence DM, Silburn SR, Blair E, Milroy H, Wilkes T, Eades S, D’Antoine H, Read A, Ishiguchi P, et al. The Western Australian Aboriginal child health survey: The health of Aboriginal children and young people. Perth: Telethon Institute for Child Health Research; 2004. [Google Scholar]
- 43.Williams HE, Carmichael A. Nutrition in the first year of life in a multi-ethnic poor socio-economic municipality in Melbourne. Aust Paediatr J. 1983;19(2):73–77. doi: 10.1111/j.1440-1754.1983.tb02061.x. [DOI] [PubMed] [Google Scholar]
- 44.Bazeley P, Kemp L. Childhood immunisation: the role of parents and service providers: a review of the literature. Canberra: Australian Government Publishing Service; 1994.
- 45.NSW Department of Health. Child Personal Health Record (Blue Book). Sydney: NSW Health; 2013. http://www.health.nsw.gov.au/kidsfamilies/MCFhealth/Publications/blue-book.pdf. Accessed 21 Feb 2017.
- 46.Davis H, Day C, Bidmead C. Working in partnership with parents: the parent adviser model. London: Harcourt Assessment; 2002. [Google Scholar]
- 47.Day C, Ellis M, Harris L. Family partnership model: reflective practice handbook. 2. London: Centre for Parent and Child Support, South London and Maudsley NHS Foundation Trust; 2015. [Google Scholar]
- 48.Howie JGR, Heaney DJ, Maxwell M, Walker JJ. A comparison of a patient enablement instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pr. 1998;15(2):165–171. doi: 10.1093/fampra/15.2.165. [DOI] [PubMed] [Google Scholar]
- 49.Paterson J, Tukuitonga C, Butler S, Williams M. Awareness of sudden infant death syndrome risk factors among mothers of Pacific infants in New Zealand. N Z Med J. 2002;115(1147):33–35. [PubMed] [Google Scholar]
- 50.Armstrong KL, Fraser JA, Dadds MR, Morris J. Promoting secure attachment, maternal mood and child health in a vulnerable population: a randomized controlled trial. J Paediatr Child Health. 2000;36(6):555–562. doi: 10.1046/j.1440-1754.2000.00591.x. [DOI] [PubMed] [Google Scholar]
- 51.Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 4. Lincoln: QualityMetric Incorporated; 2002. [Google Scholar]
- 52.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Br J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 53.New South Wales Child Protection Council . O'Donovan E: a framework for building a child-friendly society: strategies for preventing child abuse and neglect: summary document. Sydney: New South Wales Child Protection Council; 1998. [Google Scholar]
- 54.Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. J Marital Fam Ther. 1983;9(2):171–180. doi: 10.1111/j.1752-0606.1983.tb01497.x. [DOI] [Google Scholar]
- 55.Gertner S, Greenbaum CW, Sadeh A, Dolfin Z, Sirota L, Ben-Nun Y. Sleep-wake patterns in preterm infants and 6 month's home environment: implications for early cognitive development. Early Hum Dev. 2002;68(2):93–102. doi: 10.1016/S0378-3782(02)00018-X. [DOI] [PubMed] [Google Scholar]
- 56.Caldwell BM, Bradley RH. Home observation for measurement of the environment. Little Rock: Ar: University of Arkansas at Little Rock; 1984. [Google Scholar]
- 57.Floreani AA, Rennard SI. The role of cigarette smoke in the pathogenesis of asthma and as a trigger for acute symptoms. Curr Opin Pulm Med. 1999;5(1):38–46. doi: 10.1097/00063198-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 58.Barlow J, Bergman H, Kornor H, Wei Y, Bennett C. Group-based parent training programmes for improving emotional and behavioural adjustment in young children. Cochrane Database Syst Rev. 2016;(8):Cd003680. [DOI] [PMC free article] [PubMed]
- 59.Sivak L, Arney F, Lewig K. A pilot exploration of a family home visiting program for families of Aboriginal and Torres Strait Islander children: report and recommendations: perspectives of parents of Aboriginal children and organisational considerations. Magill: Australian Centre for Child Protection, University of South Australia; 2008. http://search.ror.unisa.edu.au/record/UNISA_ALMA11143309610001831/media/digital/open/9915911179001831/12143309600001831/13143306010001831/pdf. Accessed 26 July 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author LK. The data are not publicly available due to ownership of the data by the Aboriginal community.