Abstract
Rationale
Leptomeningeal metastasis (LM) is an important cause of mortality in patients with non-small cell lung cancer (NSCLC). As the symptoms of LM and its early clinical manifestations are nonspecific, early diagnosis of LM is difficult. However, there are few treatment options for LM, which leads to a poor prognosis; thus, increased clinical attention is necessary. The effects of most systemic chemotherapies on metastatic brain tumors (brain metastases and LMs) are limited as they cannot pass the blood–brain barrier; therefore, whole-brain radiation therapy is a therapeutic option. Osimertinib is a potent and irreversible third-generation oral epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI). It binds to EGFR with high affinity when the EGFR T790M mutation is present together with sensitizing mutations. The clinical efficacy of osimertinib in NSCLC patients carrying the T790M mutation has been demonstrated in clinical trial NCT02468661. Intrathecal injection of chemotherapeutic drugs can be directed to a specific lesion. Temozolomide is one such drug, and its effect has been confirmed.
Patient and interventions
We treated a 38-year-old patient with NSCLC who carried the EGFR L858R mutation. We administered a combination of oral osimertinib and oral temozolomide plus an intrathecal injection of cytarabine and whole-brain radiation therapy for symptomatic multiple brain metastases.
Outcomes
The patient showed a marked response to this combination therapy. To date (after ~18 months), no recurrence or new lesions have been observed and he is asymptomatic. His disease-free survival surpasses that achieved with any monotherapy for LM.
Lessons
This is the first report to demonstrate the response to combination therapy in an NSCLC patient with LM. These findings indicate the potential utility of chemotherapy combined with radiotherapy combined with targeted therapy combined with local treatment, as each treatment acts via a different mechanism, enhancing their therapeutic effects.
Keywords: intrathecal injection, meningeal metastasis osimertinib, non-small cell lung cancer, temozolomide, WBRT
Introduction
Metastatic brain tumors include brain metastasis and leptomeningeal metastasis (LM). Brain metastases most frequently occur in the cerebral hemispheres, followed by the cerebellum and brainstem.1 LMs are less common than brain metastases, and 5%–10% of patients with non-small cell lung cancer (NSCLC) will develop LM,2 and 20% of these patients will already have LM when their lung cancer is first diagnosed.1 Approximately 50% of NSCLC patients with LM carry a mutation in the epidermal growth factor receptor (EGFR).3 With the discovery of targeted drug therapies and improvements in the treatment of lung cancer patients, patient survival has increased; thus, the number of patients diagnosed with meningeal metastasis has also increased.4
Osimertinib mesylate (AZD9291, Tagrisso™, Astra-Zeneca Pharmaceuticals, Cambridge, UK) is an oral mono-anilino-pyrimidine small molecule that has shown promise as a mutant-selective EGFR tyrosine kinase inhibitor (TKI). Osimertinib has shown potent activity against advanced NSCLC positive for the EGFR T790M mutation (EGFRm).5 Osimertinib penetrates the blood–brain barrier (BBB) and its effects have been encouraging. Its activity and reasonable tolerability were observed at a dose of 160 mg qd in patients with LM from EGFRm NSCLC following a median treatment duration of 6.0 months. Evaluation of this agent is ongoing;5,6 (ClinicalTrials.gov identifier: NCT02228369). Temozolomide (TMZ) is a new oral alkylating agent which crosses the BBB and has demonstrated a survival benefit in high-grade glioma treatment when administered concurrently with adjuvant radiotherapy.7 A subgroup analysis showed that the treatment of NSCLC patients with whole-brain radiation therapy (WBRT) combined with TMZ had a significantly superior objective response rate (ORR; RR =1.38) to that of WBRT alone (RR =1.34, P<0.00001).8 WBRT is one of the therapeutic options for LM. Although it may damage neurocognitive functions,9 it is the preferred option, especially for patients with symptomatic multiple brain metastases.10
Intrathecal drug therapy
Intrathecal chemotherapy remains the standard treatment for lung cancer patients with leptomeningeal disease and has a good risk profile. The chemotherapeutic drugs are delivered intrathecally.11 Chemotherapeutic drugs administered by intrathecal injection include methotrexate, cytarabine, and thiotepa.12 Cytarabine was selected to treat the patient in this study.
Case
Four years ago, a 38-year-old man with no history of smoking or other diseases underwent upper-lobe wedge resection of the left lung for early-stage NSCLC. Positron emission tomography–computed tomography (CT) showed left upper-lobe mass lesions, increased abnormal glucose metabolism, and malignant lesions. Surgery was undertaken on July 19, 2013, during which, a hard-textured mass on the superior anterior segment of the upper lobe was detected, which was closely adhered to the parietal and visceral pleura, and was ~4×3×3 cm3 in size. About 300 mL of bloody pleural effusion was also present. The diaphragm surface was covered with masses of different sizes, the largest of which was ~3×3×3 cm3. The lesions could not be completely resected, and left upper-lobe wedge resection was performed. The pathological diagnosis of frozen sections showed a well-differentiated to moderately differentiated adenocarcinoma. The postoperative pathological diagnosis also indicated a well-differentiated to moderately differentiated adenocarcinoma (Figure 1). An EGFR gene analysis showed L858R (+), but KRAS gene mutation was negative.
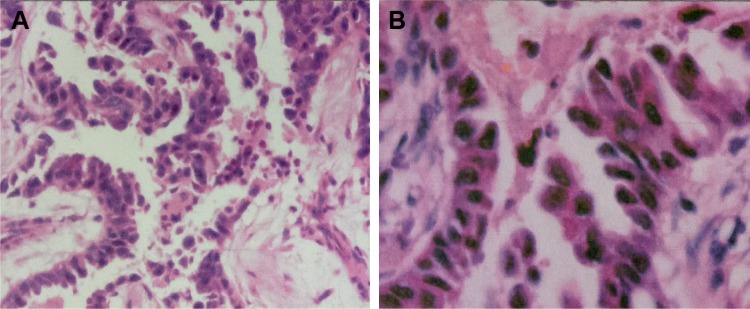
Figure 1.
Hematoxylin and eosin staining of a tumor section (×200). Pathological light microscopic results (A), well-differentiated to moderately differentiated adenocarcinoma seen in the upper lobe and pleura of the left lung (B).
After surgery, 150 mg of erlotinib per day was administered for 1 year. Follow-up CT showed that the pulmonary nodules were larger than previously detected by CT. The patient then received 4 courses of systemic chemotherapy. During the first course, 0.8 g of pemetrexed on day 1 and 40 mg of cisplatin on days 1–3 were administered. Reexamination with CT showed a light shadow under the left pleura. A bone scan and craniocerebral MRI showed no abnormalities. The patient received 150 mg of Tarceva® (OSI Pharmaceuticals, LLC, Northbrook, IL, USA an affiliate of Astellas Pharma US, Inc., Northbrook, IL, USA) per day for 8 months. Follow-up CT revealed that the left pulmonary nodules had increased in size, with a maximum diameter of ~1.2 cm. Due to disease progression, 1 g of pemetrexed and 500 mg of carboplatin were administered, which induced a degree II gastrointestinal reaction and grade I hematological toxicity. The efficacy of chemotherapy was rated as a partial response after 2 courses and stable disease after 4 courses.
Approximately 1.5 years ago, the patient reported headache and dizziness, with intermittent symptoms of nausea, vomiting, weakness, hand numbness, and tongue numbness. A craniocerebral MRI showed multiple meningeal metastatic lesions. Cerebrospinal fluid cytology showed a few atypical cells. Lung cancer and meningeal metastases were diagnosed due to the patient’s symptoms, MRI findings, and cerebrospinal fluid cytology, and 250 mg of TMZ per day was administered for 5 days. Cytarabine was administered 6 times by intrathecal injection, at a frequency of twice per week. During the same period, WBRT was administered with an intensity of Dt50Gy/25f for 3 weeks, at a frequency of 5 days per week. On day 5 after chemotherapy, the patient’s symptoms of dizziness and nausea decreased rapidly.
On day 10 after radiotherapy, headache severity and nausea symptoms increased, but they were immediately relieved following intravenous administration of corticosteroids. The patient’s symptoms of dizziness, nausea, and headache disappeared. AZD9291 has been administered up to the present time as fourth-line therapy. The patient had no headache or fatigue following this combination therapy. The examination of the brain fluid after 2 intrathecal injection showed that there were no atypical cells
Follow-up MRI showed that all lesions had disappeared from the bilateral cerebellar regions (Figure 2) and the right frontal lobe (Figures 3 and 4) 6 months after the combination therapy. CT showed that the lesion in the lower lobe of the right lung had disappeared (Figure 5) and the lesions in the upper lobe of the left lung had reduced.
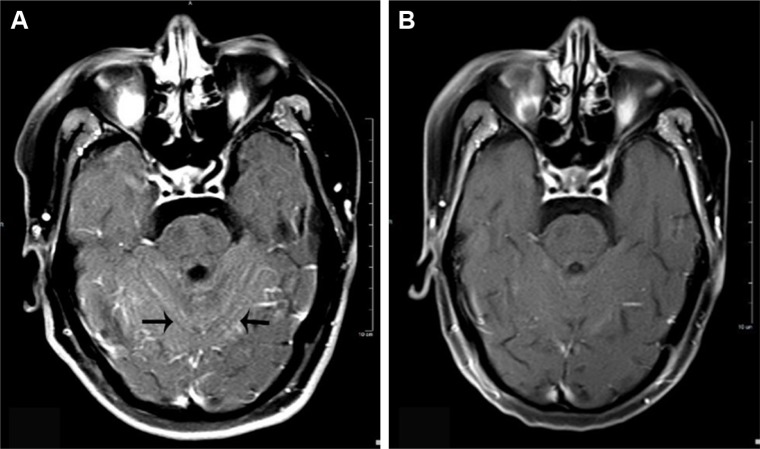
Figure 2.
Axial craniocerebral MRI.
Notes: (A) Before treatment, bilateral cerebellar sulcus line-like enhancement (black arrows) was seen. (B) After treatment, line-like enhancement had disappeared.
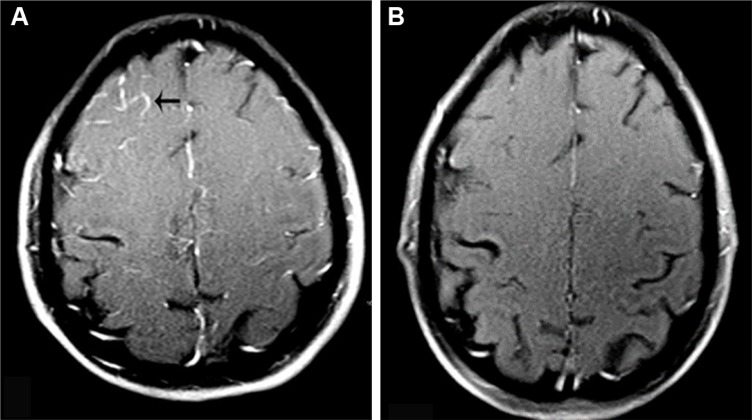
Figure 3.
Axial craniocerebral MRI.
Notes: (A) Before treatment, line-like enhancement was seen in the right frontal lobe of the brain (black arrows). (B) After treatment, the line-like enhancement had disappeared.
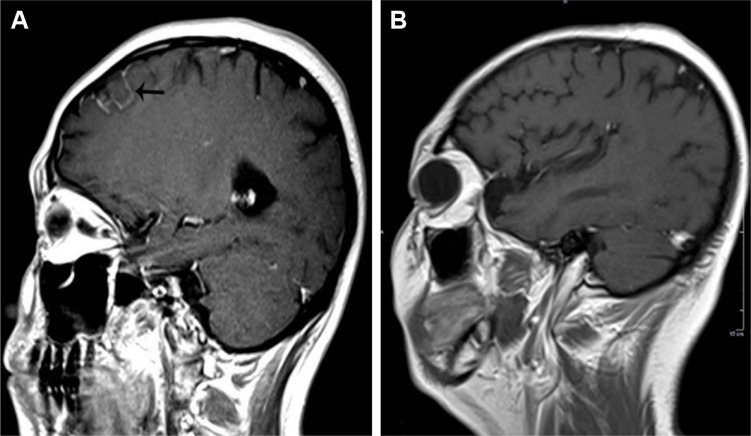
Figure 4.
Sagittal craniocerebral MRI.
Notes: (A) Before treatment, right lobe brain sulci visible line-like enhancement was seen (black arrow). (B) After treatment, the line-like enhancement had disappeared.
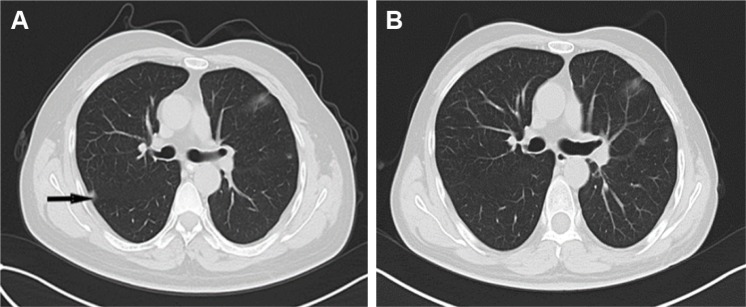
Figure 5.
CT of the lung.
Notes: (A) Before treatment, small nodules were seen in the lower right lung. (B) After treatment, the small nodules had disappeared.
Abbreviation: CT, computed tomography.
Regular follow-up, which has included imaging every 3 months (CT/MRI), has identified no new lesions.
Neurocognitive dysfunction has been identified after whole-brain radiation and chemotherapy.8,9 However, our patient only experienced a slight decrease in recent memory, comprehension, and occasionally a slight decrease in hearing ability, which did not affect his normal daily life.
Ethics statement
This case report was approved by the Medical Ethics Committee of the Shaanxi Provincial Cancer Hospital Affiliated to Medical School Xi’an Jiaotong University. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Discussion
Lung cancer is accompanied by LM in 3.8% of cases.13 Although there has been no randomized controlled trial on lung cancer-associated LM, references on this phenomenon are available in some case studies.
Our patient had an Eastern Cooperative Oncology Group score of 0, and gene analysis detected the EFGR mutation L858R; thus, we administered combined therapy for LM, including oral chemotherapy, intrathecal chemotherapy, and WBRT, in a targeted sequential manner. The patient has survived for 18 months since the diagnosis of LM, without relapse or progression. The survival of cancer patients with LM treated with any monotherapy is 3–10 months.14 Therefore, the survival period of our patient exceeds that achieved with any single treatment and in any other reported case. Other solid tumors with LM, such as breast cancer and gynecological tumors, also have poor prognoses and limited survival.15–17
The use of 4 types of therapy administered sequentially was only possible due to the good physical condition of the patient, which suggested that he could tolerate any adverse effects. During the course of WBRT, the patient developed obvious headache, but this disappeared after dehydration and treatment with glucocorticoids. Fatigue persisted for a relatively long period, which may be attributable to osimertinib.15 After chemotherapy and WBRT, the symptoms of headache, nausea, and fatigue disappeared.
The different elements of the combination therapy had different mechanisms of action, not only against existing lesions but also against potential lesions. The combination therapy extended the patient’s disease-free survival and overall survival, reduced disease recurrence, and improved his quality of life. A retrospective study showed that in patients who received modern systemic therapy for LM that included chemotherapy or a TKI, the mean overall survival was 6 months (95% CI, 3–12) after LM diagnosis. Patients who received modern systemic therapy for LM had a reduced risk of death (hazard ratio, 0.24; P=0.007).18
We chose TMZ treatment as it has been reported that its administration alone or combined with other chemotherapeutic drugs, together with sequential WBRT or concurrent WBRT, improved the disease control rate in patients with intracranial metastatic lesions, thus providing a new treatment option for NSCLC patients with brain metastases.1,2,9 Phase II clinical trials have shown that TMZ is safe and effective in patients with brain metastases, but because the sample sizes were small,2 a large-scale Phase III trial is required to verify its therapeutic effects.
Intrathecal chemotherapy can reduce the neurotoxicity of chemotherapeutic drugs, and symptoms can be relieved when it is combined with glucocorticoids; therefore, it is an important treatment option for patients with LM of NSCLC. However, there is no clear evidence at present of the efficacy of intrathecal chemotherapy in patients with LM of NSCLC.
Another explanation for the longer survival of our patient is that he carries the EGFR mutation L858R. AZD9291 is a targeted drug that plays an important role in cancer control as it can pass through the BBB. Therefore, our patient has received AZD9291 as ongoing maintenance therapy. Several cases of LM treated with osimertinib have been reported. Koba et al19 observed a rapid response to osimertinib, within 2 weeks of its administration in patients with brain metastases. Hata et al20 observed that osimertinib efficiently passes the BBB. Yang et al5 reported that osimertinib showed a good Kpuu, brain value (puu: plasma unbound ratio) of 0.39, greater than those of other available EGFR-TKIs. Kpuu, brain is well established as a good predictor of BBB permeability, and values >0.3 indicate good diffusion across the BBB.21 Therefore, from this research, we conclude that osimertinib played an important role in the treatment of our patient.
Which methods can be used for further therapy if a mutant EGFR gene mutates again, indicating resistance to osimertinib? It has been reported that patients will acquire resistance to osimertinib therapy after a median treatment period of 9.6 months.22 The EGFR C797S mutation is reported to be a major mechanism (6/15; 40%) of resistance to osimertinib;23 thus, it is not surprising that patients become resistant to osimertinib. However, it is unclear whether we should recommend a fourth-generation EGFR-TKI that can overcome the resistance mediated by C797S or local radiotherapy. Therefore, a combination of intrathecal chemotherapy, WBRT, osimertinib, and TMZ is the best treatment choice for patients with LM (and Eastern Cooperative Oncology Group scores of 0–2) carrying the EGFR mutation T790M.24
Although we combined 4 different treatment mechanisms to extend our patient’s disease-free survival and overall survival, our research has some limitations as it includes only 1 case study of NSCLC meningeal metastases. Multicenter, randomized, double-blind observational studies are required to verify our treatment outcome and provide more evidence to benefit patients with meningeal metastases from NSCLC or solid tumor meningeal metastases.
Acknowledgments
The authors thank the patient for his participation and his agreement to the publication of the report.
Footnotes
Authors contribution
All authors contributed toward data analysis, drafting, and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Eichler AF, Loeffler JS. Multidisciplinary management of brain metastases. Oncologist. 2007;12(7):884–898. doi: 10.1634/theoncologist.12-7-884. [DOI] [PubMed] [Google Scholar]
- 2.Addeo R, De Rosa C, Faiola V, et al. Phase 2 trial of temozolomide using protracted low-dose and whole-brain radiotherapy for nonsmall cell lung cancer and breast cancer patients with brain metastases. Cancer. 2008;113(9):2524–2531. doi: 10.1002/cncr.23859. [DOI] [PubMed] [Google Scholar]
- 3.Ballard P, Yates JW, Yang Z, et al. Preclinical comparison of osimertinib with other EGFR-TKIs in EGFR-mutant NSCLC brain metastases models, and early evidence of clinical brain metastases activity. Clin Cancer Res. 2016;22(20):5130–5140. doi: 10.1158/1078-0432.CCR-16-0399. [DOI] [PubMed] [Google Scholar]
- 4.Eichler AF, Kahle KT, Wang DL, et al. EGFR mutation status and survival after diagnosis of brain metastasis in nonsmall cell lung cancer. Neuro Oncol. 2010;12(11):1193–1199. doi: 10.1093/neuonc/noq076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang JCH, Kim DW, Kim SW, et al. Osimertinib activity in patients (pts) with leptomeningeal (LM) disease from non-small cell lung cancer (NSCLC): updated results from BLOOM, a phase I study. Am Soc Clin Oncol. 2016;34(Suppl 15):9002. [Google Scholar]
- 6.Yang JCH, Cho BC, Kim DW, et al. Osimertinib for patients (pts) with leptomeningeal metastases (LM) from EGFR-mutant non-small cell lung cancer (NSCLC): updated results from the BLOOM study. Am Soc Clin Oncol. 2017;35(Suppl 15):2020. [Google Scholar]
- 7.Tian J, Luo Y, Xiang J, Tang J. Combined treatment for non-small cell lung cancer and breast cancer patients with brain metastases with whole brain radiotherapy and temozolomide: a systematic review and meta-analysis. J Neurooncol. 2017;135(2):217–227. doi: 10.1007/s11060-017-2572-z. [DOI] [PubMed] [Google Scholar]
- 8.Deng X, Zheng Z, Lin B, et al. The efficacy and roles of combining temozolomide with whole brain radiotherapy in protection neurocognitive function and improvement quality of life of non-small-cell lung cancer patients with brain metastases. BMC Cancer. 2017;17(1):42. doi: 10.1186/s12885-016-3017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li J, Bentzen SM, Li J, Renschler M, Mehta MP. Relationship between neurocognitive function and quality of life after whole-brain radiotherapy in patients with brain metastasis. Int J Radiat Oncol Biol Phys. 2008;71(1):64–70. doi: 10.1016/j.ijrobp.2007.09.059. [DOI] [PubMed] [Google Scholar]
- 10.Ettinger DS, Wood DE, Akerley W, et al. Non-small cell lung cancer, version 6.2015. J Natl Compr Canc Netw. 2015;13(5):515–524. doi: 10.6004/jnccn.2015.0071. [DOI] [PubMed] [Google Scholar]
- 11.Remon J, Le Rhun E, Besse B. Leptomeningeal carcinomatosis in non-small cell lung cancer patients: A continuing challenge in the personalized treatment era. Cancer Treat Rev. 2017;53:128–137. doi: 10.1016/j.ctrv.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Xin-en H. Interpretation of China Experts Consensus on the Diagnosis and Treatment of Brain Metastases of Lung Cancer (2017 Version) J Int Transl Med. 2017;5(1):45–52. doi: 10.3779/j.issn.1009-3419.2017.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gion M, Remon J, Caramella C, Soria JC, Besse B. Symptomatic leptomeningeal metastasis improvement with nivolumab in advanced non-small cell lung cancer patient. Lung Cancer. 2017;108:72–74. doi: 10.1016/j.lungcan.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 14.Ota K, Shiraishi Y, Harada T, et al. OA08.02 phase II study of erlotinib in advanced non-small cell lung cancer patients with leptomeningeal metastasis (LOGIK1101) J Thorac Oncol. 2017;12(1):S271–S272. [Google Scholar]
- 15.Cordone I, Masi S, Summa V, et al. Overexpression of syndecan-1, MUC-1, and putative stem cell markers in breast cancer leptomeningeal metastasis: a cerebrospinal fluid flow cytometry study. Breast Cancer Res. 2017;19(1):46. doi: 10.1186/s13058-017-0827-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morikawa A, Jordan L, Rozner R, et al. Characteristics and outcomes of patients with breast cancer with leptomeningeal metastasis. Clin Breast Cancer. 2017;17(1):23–28. doi: 10.1016/j.clbc.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Toyoshima M, Tsuji K, Shigeta S, et al. Leptomeningeal metastasis from gynecologic cancers diagnosed by brain MRI. Clin Imaging. 2017;41:42–47. doi: 10.1016/j.clinimag.2016.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Riess JW, Nagpal S, Iv M, et al. Prolonged survival of patients with non–small-cell lung cancer with leptomeningeal carcinomatosis in the modern treatment era. Clin Lung Cancer. 2014;15(3):202–206. doi: 10.1016/j.cllc.2013.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koba T, Kijima T, Takimoto T, et al. Rapid intracranial response to osimertinib, without radiotherapy, in nonsmall cell lung cancer patients harboring the EGFR T790M mutation: two case reports. Medicine. 2017;96(6):e6087. doi: 10.1097/MD.0000000000006087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hata A, Katakami N, Yoshioka H, et al. Prognostic impact of central nervous system metastases after acquired resistance to EGFR-TKI: poorer prognosis associated with T790M-negative status and leptomeningeal metastases. Anticancer Res. 2015;35(2):1025–1031. [PubMed] [Google Scholar]
- 21.Varadharajan S, Winiwarter S, Carlsson L, et al. Exploring in silico prediction of the unbound brain-to-plasma drug concentration ratio: model validation, renewal, and interpretation. J Pharm Sci. 2015;104(3):1197–1206. doi: 10.1002/jps.24301. [DOI] [PubMed] [Google Scholar]
- 22.Jänne PA, Yang JCH, Kim DW, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med. 2015;372(18):1689–1699. doi: 10.1056/NEJMoa1411817. [DOI] [PubMed] [Google Scholar]
- 23.Thress KS, Paweletz CP, Felip E, et al. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non-small cell lung cancer harboring EGFR T790M. Nat Med. 2015;21(6):560–562. doi: 10.1038/nm.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee SJ, Lee JI, Nam DH, et al. Leptomeningeal carcinomatosis in non–small-cell lung cancer patients: impact on survival and correlated prognostic factors. J Thorac Oncol. 2013;8(2):185–191. doi: 10.1097/JTO.0b013e3182773f21. [DOI] [PubMed] [Google Scholar]