Abstract
Purpose:
To investigate the use of electronic patient-reported outcomes (PROs) to assess symptoms and how they can provide opportunities to clinicians to address symptoms in a timely manner to improve clinical care. As part of a larger study to evaluate whether providing standardized symptom reports to the medical team would decrease the time to treatment of reported symptoms in hematopoietic stem-cell transplant recipients, we assessed nurses’ and providers’ perceptions of electronic symptom reporting.
Methods:
Semistructured interviews of RNs, MDs, NPs and PAs were conducted at an academic cancer center in the southeastern United States. Nurses’ and providers’ perceptions of electronic symptom reporting were explored. Interviews were audio-recorded, transcribed, and coded by two investigators to identify major themes.
Results:
Fourteen RNs and seven providers (MDs, PAs, and NPs) participated in the interviews. Three main themes emerged from the interviews: electronic symptom reporting may improve assessment and care, integrating symptom reporting into nurse workflow presents difficulties, and there are barriers for completion of surveys.
Conclusion:
The majority of nurses and providers believed that the inclusion of electronic symptom reporting in bone marrow transplantation inpatient units has the potential to improve care but that barriers to implementation remain.
INTRODUCTION
Patient-reported outcomes (PROs) are instrumental in improving care to decrease symptom burden, improve patient outcomes, and increase survival.1,2 PROs refer to “any report on the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else.”3(p2) Systematic, comprehensive PRO collection is typically not part of routine nursing assessment or provider rounds in bone marrow transplantation units (BMTU); instead, clinicians typically query patients about specific symptoms during daily brief clinical encounters (ie, patient rounds).4-6 Using standardized electronic PRO surveys allows clinicians a broad inventory of symptoms they can use to identify and address severity and frequency of unrecognized symptoms.
Patients hospitalized for high-dose chemotherapy as part of preparation for hematopoietic stem-cell transplantation (HSCT) experience significant symptom burden interfering with quality of life7-9 and would likely benefit from standardized PRO reporting. Reporting these symptom changes to clinicians in a timely manner may result in more frequent, rapid improvements in clinical care (eg, medication adjustment, consultation with subspecialty services), which may lead to overall reduction in peak symptom burden. In outpatient care for cancer, patients completing PROs as part of routine care have higher satisfaction with care, reduced emergency room visits for uncontrolled symptoms, and better symptoms and survival.10-14 Clinicians use PRO information to direct care; however, little is known for adults treated in an inpatient unit. A critical first step in practice change is to understand HSCT clinicians’ perceptions of acceptability and usefulness of using PROs during inpatient rounds. We aimed to explore nurses’ and providers’ perceptions about using PROs to guide plan of care for patients undergoing HSCT.
METHODS
Parent Study
The current study is a part of a larger parent study conducted at the University of North Carolina at Chapel Hill (UNC) BMTU from July 2014 to June 2017. The primary aim of the parent study focused on evaluating use of electronic patient symptom reporting to reduce symptom burden during HSCT. At a single academic medical center, patients were randomly assigned to daily symptom reporting with PROs during hospitalization (n = 76) or usual care (symptom elicitation at discretion of clinician; n = 38).
Nurses instructed patients to complete a brief PRO survey daily on their iPhone or iPad (intervention group). Patient-Reported Outcomes Common Terminology for Adverse Events (PRO-CTCAE) items were used to assess 16 common HSCT symptoms. The recall period on PRO-CTCAE was changed from “last 7 days” to “now” to accommodate daily symptom reporting. The survey was available to be completed from 12:00 pm to 10:00 pm. This time period was selected because it occurs after morning rounds and may better capture symptoms experienced as the day progresses.
Nurses received an e-mail notification whenever patients were randomly assigned to daily symptom reporting and completed an electronic PRO during hospitalization. Each morning, an e-mail containing a link to a study home page was sent to the nurse caring for individual intervention patients. Nurses were required to use their secure institutional log-in to access patient reports (Fig 1). These reports show all symptoms queried in the survey; the most distressing symptoms are ranked at the top and the least distressing symptoms at the bottom. PRO-CTCAE commonly reported symptoms of those undergoing HSCT included shortness of breath, pain, vomiting, diarrhea, nausea, mouth/throat sores, constipation, cough, insomnia, heartburn, rash, decreased appetite, fatigue, anxiety, sad/unhappy feelings, nothing could cheer me up.
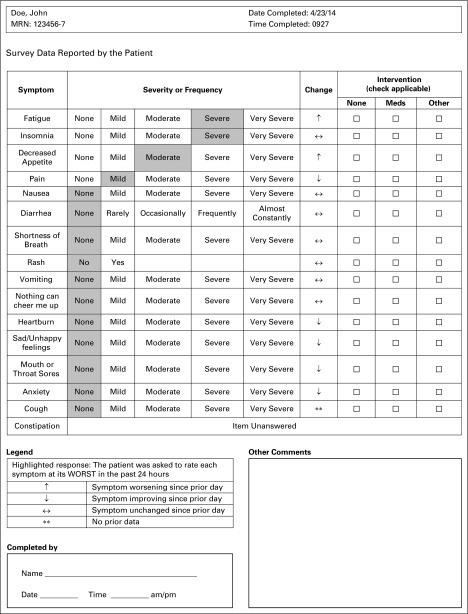
Fig 1.
Survey data reported by the patient.
When patients completed the electronic survey (70% completion rate), the nurse would receive an e-mail of patient reports. The nurse would print and present the report at morning rounds. Providers used the report to guide conversations with patients during rounds and help direct plan of care.
Setting and Participants
The focus of this article is to report on a concurrent qualitative study conducted at the UNC BMTU. Nurses and providers who had delivered care to patients enrolled in the aforementioned study were purposively recruited to participate. Nurses and providers were eligible if they had cared for patients undergoing HSCT during the parent study period. Forty-four nurses and 16 BMTU providers met inclusion criteria. Participants provided written informed consent.
Procedures
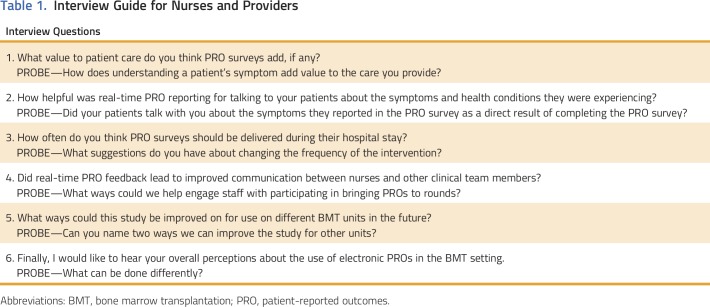
Interview data were collected from August 2017 to September 2017 by a trained interviewer (E.C.). Each nurse and provider was interviewed once. Semistructured interviews were audio-recorded and conducted in person on the BMTU to explore nurses’ and providers’ perceptions of using electronic PROs to obtain symptom data. Interview questions (Table 1) were derived from the research team and current literature. Participants could express other thoughts that were not included in the interview questions. The interviewer began with open-ended questions and followed with probe questions.
Table 1.
Interview Guide for Nurses and Providers
Data Management and Analysis
Interviews were transcribed by a professional transcription agency. Atlas was used for the content analysis procedure to analyze interview data.15 Two researchers (A.L.B., R.H.) read transcriptions to derive codes. One researcher (A.L.B.) highlighted words in the transcripts that illustrated key concepts, and R.H. made notes about her thoughts related to each group of highlighted words. Through this process, codes emerged and were given labels reflective of concepts or themes. Two coders reviewed and discussed labels to group codes into related categories. Major themes were identified through these processes. Each major theme was then defined, and corresponding exemplar quotes were identified.
The trustworthiness of analysis procedures and findings was addressed by making an audit trail to record data collection, coding, and analysis decisions. The interviewer, who was one of the data coders, made reflexive memos after each interview. These memos were reviewed together with the audio recordings to discern linkages, gaps, and questions.
The study coordinator entered demographic data, and 10% of the data entered were checked by the primary investigator for quality assurance and found to be 100% correct. The second coder (A.L.B.) was familiar with the aims of the study, did not interview the nurses or providers, and coded 100% of the data. When the two coders did not agree on their initial code, code negotiation and transcript review occurred.16 Their initial agreement in coding was only 47%, but that increased to 100% after code negotiation. Workflow and technology subcodes accounted for the initial discrepancy in coding. Both coders added codes that were not in the initial code book that required additional discussion.
Demographic data (eg, years as an RN, MD, NP, or PA) were collected on the participants and managed using REDCap.17 Descriptive statistics were calculated for all demographic variables using SPSS version 22.0 (SPSS, Chicago, IL). The UNC Lineberger Comprehensive Cancer Center Protocol Review Board and the UNC Institutional Review Board approved this study. Participants did not receive incentives.
RESULTS
Participants
A total of 14 nurses and seven providers (MD, NP, and PA), with a mean age of 33.4 (± 7.9) and 43.86 (± 11.9) years, respectively, participated in semistructured interviews. The nursing staff was primarily female (85.7%) and white (92.9%), with an average of 2.3 (± 1.86) years experience of working in BMT. The majority of nurses held a BSN degree (71.4%) and had an average of 9.5 (± 10.19) years of experience working in BMT. The majority of providers were white (85.7%) and board certified, with an average of 9.5 (± 10.19) years of experience working in BMT.
Themes
Three main themes emerged: electronic symptom reporting may improve assessment and care, integrating symptom reporting into nurse workflow presents difficulties, and clinicians perceived that patients commonly experienced barriers to completing PROs. Three subthemes emerged: electronic PROs improve quality of care, there are communication gaps, and timing and frequency of nurse/provider interventions are important.
Electronic Symptom Reporting May Improve Assessment and Care
Nurses and providers found that the electronic tool improved overall symptom assessment and emphasized the importance of continual assessment and management. In many instances, nurses and providers learned that patients were experiencing symptoms that their assessment practices did not identify. Nursing staff believed that the surveys added value to symptom assessment and management because of their objective and self-reported nature. However, three nurses (out of 14) believed surveys were redundant, because nurses routinely assess symptoms.
PROs improve quality of care
Eleven nurses found the survey effective as an additional tool for assessing patient symptoms. Because patients are hospitalized for 2 to 4 weeks, they inevitably have new nurses at different points in their treatment. Three nurses believed that the surveys were a good starting point to building rapport with new patients who might not feel comfortable discussing the severity of their symptoms with someone they have just met. The objective list of symptoms was also mentioned as a good way to “gather one’s thoughts” during rounds or when assessing patients. Two nurses mentioned the advantage of the surveys being open from 12:00 pm to 10:00 pm. This time period is important, because it is missed by earlier assessment during rounds, and patients might experience symptoms as the day progresses. Surveys enable providers to follow up during the night shift.
Other nurses found the survey less useful and believed if they were building rapport with patients and assessing them thoroughly, they should already know about issues before a survey is completed. One nurse mentioned that if a patient does not fill out their survey until later in the day, by the time they are assessed in the morning, the answers given might be irrelevant. The window into patients’ perceptions of their symptoms was cited as a strength of using surveys as a symptom assessment tool. Two nurses expressed similar experiences with differences between their assessment of a patient’s symptoms and the patient’s own perspective of their symptoms. These misaligned perceptions included which symptoms were most bothersome and severe. One nurse spoke of how perceptions about the presenting symptoms themselves can differ: “Well mucositis, to me, is the worst thing you could have while you’re here, but the patient’s more distressed about their nausea or another symptom, so they report that higher, so you get the patient’s subjective part of it as well, which is good.”
Because of this insight, nurses and providers appreciated the benefit of an electronic tool to improve assessment and care. Improving the symptom experience for the patient undergoing HSCT is the key role of the nurse and provider. One nurse said, “I didn’t even know this person was experiencing this particular symptom, but it was something that was mentioned in the survey. So then that’s how it came up. I’ve seen some instances where it added value to rounds. I think it’s always best when we treat the patient based on their symptoms and progression per their report as opposed to how we’ve been experiencing their symptoms because it’s not always the same.” Another nurse shared that “one time my patient was not reporting pain to the provider. He was reporting severe pain on the survey, and I was like, ‘You said you were in a lot of pain yesterday, but today you’re saying you told the provider you weren’t in any pain.’ They were like, ‘Yes, I just don’t want to look like I’m…’—they were being stoic.” The symptom tool provides opportunity for clarity and encourages the patient to share symptoms they might not have otherwise shared.
In speaking of electronic PROs, one provider said: “The potential for providers understanding in a more quantifiable way how the patient is doing in those kind of nursing-centered aspects is really valuable. I think one of the things that’s been challenging with nursing is that a large portion of the quality is qualitative, and trying to quantify it is important.”
PROs improves communication gaps
Nurses viewed the surveys as a communication tool allowing patients to report their subjective experiences in a standardized, objective way on their own time. Nurses also believed that electronic survey delivery removed some of the psychosocial barriers to symptom reporting, such as appearing stoic for family or providers or being uncomfortable about physical symptom conversations (ie, diarrhea). Five nurses cited instances where symptoms were incongruent with statements made during morning rounds. Another nurse said, “Some people are embarrassed to ask or they don’t just [ask] about something because they don’t want to trouble us.” The providers highlighted the surveys’ usefulness as a tool for bridging the communication gap between patients and providers. A common statement among providers was that patients underreport their symptoms or report things differently: “I feel that if they tell us stuff that indicates that what we’re doing is not working, and they don’t want to disappoint us…but it’s clear and when you query folks themselves in a patient-reported manner, what they report is a bit different.”
One nurse believed surveys could help fill communication gaps in the transplantation process. “We’re putting them through the transplant process pretty fast. I’ve noticed a trend of it being harder for them to really get the information, all of that information, and so you tell somebody, well this chemo’s going to do this you, it’s going to cause some peripheral neuropathy. They kind of expect that so they don’t even report it a lot of times.” One nurse mentioned patients underreporting symptoms because of expectations: “I’ve noticed a lot of our patients are like, oh well you told me that was going to happen. Yes, but I still need to know about it so we can manage it.”
Integrating Symptom Reporting Into Nurse Workflow
Nurses were responsible for providing PRO survey findings for discussion at morning rounds. During this study, this was an additional task for nurses who often struggled with changes because of the varying number of patients who were in the study. This was an added responsibility to their already demanding patient workloads. Nurses expressed that it was easy to forget these additional tasks, particularly reminding the patient to complete the symptom assessment before the electronic system closed. If the night shift nurse printed the form, then the day shift nurse could share it in morning rounds. More than 50% of patients were asleep by 10:00 pm, and nurses were not comfortable waking patients to ask them to complete the symptom assessment. One nurse explained, “Once we forgot to remind the patient, it just didn’t get done.” To counteract the lack of integration, nurses and providers suggested further simplifying the survey to fewer items, offering different modes of data completion (phone, interactive voice response), or offering incentives for data completion. A common statement among nurses and providers was “it needs to be a much simpler process in order to be successful.” Interviewees mentioned standardized surveys as a useful tool for nursing staff to quantify quality of care and as a device for nurses to add patient input to rounds.
Barriers for Completion of Surveys
Interview data from nurses and providers revealed that patients often did not complete the symptom survey. Common reasons were that patients simply forgot even when prompted, symptoms were too severe, and they did not feel well. For example, one nurse said, “When they actually start feeling worse…is when they are least likely to fill it out.”
One nurse commented, “They agree to be on the study when they come in, when they’re feeling fine, and they think that they’re going to have all that energy, all this free time, and then when they actually start feeling worse than we would like, when they’re least likely to complete their surveys.”
Timing and frequency of survey completion are concerns. Twelve nurses agreed that daily surveys were important because “the patients’ needs and symptoms vary from day to day.” One nurse believed that although the surveys are a tool for tracking symptomology, they would not affect care, because “we treat all symptom management kind of the same so based on the patient, not necessarily what they report because they won’t always report everything.” The nurses’ opinions about frequency of how often surveys should be administered ranged from daily, two to three times a week, once patients had received their transplants, or at the onset of symptoms. Providers agreed with nurses about how frequently surveys should be delivered. All providers mentioning frequency agreed that daily symptom surveys were best. One provider’s preference was to start once symptoms begin; another suggested stopping once symptoms resolve or reach a level adequate for coping. Opinions about the timing and frequency of how often symptoms should be assessed and managed are mixed, but future work is needed to explore this further.
DISCUSSION
BMT providers and nurses valued electronic assessment of symptoms. Nurses and providers reported improved communication with patients about symptoms. Clinicians perceived that standardized PRO reporting identified more symptoms during rounds than typical clinical interactions and that symptoms were better managed. Our findings are consistent with extant literature showing that clinicians underestimate symptoms.13,18-20 BMT clinicians reported benefits for using PROs during inpatient care consistent with outpatient care: building rapport with patients21 to increase understanding patients’ perceptions of symptoms.2,9,21 Most PRO implementation has been in outpatient cancer care, but inpatient care has unique barriers; implementation strategies need to be tailored to an inpatient unit’s needs, barriers, and workflow.
A tailored implementation plan for PROs needs to target multiple levels22,23 on the basis of barriers interviewees identified at the unit, nursing workflow, and patient levels. At the unit level, a common theme was integrating symptom reporting into the electronic health record (EHR). The health care system where the interviews took place is currently pilot testing using the EHR to administer PROs in outpatient units, with rollout to inpatient units occurring later. Health care systems have struggled to integrate PROs within EHRs, because EHRs lack essential functionality for PROs (eg, PRO visual representation).
At the nursing workflow level, barriers included nurses forgetting to remind patients or not wanting to wake patients to complete the PRO before the survey closed at 10:00 pm. Clinician suggestions to address these barriers were simplifying the process of completing the questionnaire or offering patients incentives to reduce need for reminders. A potential solution is to change the nursing workflow so nurses are alerted immediately to distressing symptoms. For instance, if a patient reports severe pain or nausea, an automated alert could be sent to the nurse. Nurses could follow up immediately, and perhaps a more immediate feedback loop would reinforce patients to complete the PRO.
At the patient level, the primary barrier was missing data because of high symptom burden, which is similar in other studies.11,12 Inpatient interviews may help to determine barriers to PRO completion, timing and frequency of PROs, alerts to nurses, and which questions are the most meaningful. Future solutions may be to automate reminders and change how patients complete the PRO (eg, landline-based interactive voice response, smart TV).
This study has some limitations. First, this single-site study focused on interviewing a small number of nurses and providers in an inpatient BMT unit and was limited by diversity of race/ethnicity and sex (although it was representative of the units’ clinicians). Second, the varying number of patients in the study at any given time might have affected the nurses’ and providers’ ability to remember details of the study about patients they cared for during the study period. Last, the symptom report was completed the night before morning rounds, and symptoms can fluctuate from time of survey to morning rounds. Despite these limitations, this study was novel in its exploration of nurses’ and providers’ perceptions of electronic PROs in a high symptom burden population.
One strength is that all providers and nurses interviewed had used the study’s symptom report and could discuss challenges, barriers, and suggestions for future work of an electronic tool. The qualitative design allowed authors to comprehensively explore nurses’ and providers’ experiences by gaining a deeper understanding of their perceptions of the symptom tool.
In conclusion, the majority of nurses and providers believed the inclusion of electronic symptom reporting in BMT units has the potential to improve care, but barriers to implementation remain. Additional multisite studies, increased numbers of nurses and providers to offer their perceptions, and patient perceptions are needed. Future work is needed to explore how workflow would change if this tool were implemented in the EHR.
ACKNOWLEDGMENT
Supported by National Cancer Institute Grant No. 5K12CA120780-07 (A.L.B.) and University Cancer Research Fund Grant No. UL1RR025747 from University of North Carolina at Chapel Hill (A.L.B., W.W.).
AUTHOR CONTRIBUTIONS
Conception and design: Ashley Leak Bryant, Erin M. Coffman, Elizabeth Bullard, William A. Wood
Collection and assembly of data: Ashley Leak Bryant, Erin M. Coffman, Elizabeth Bullard, Joshua Bradley, William A. Wood
Data analysis and interpretation: Ashley Leak Bryant, Erin M. Coffman, Rachel Hirschey, Elizabeth Bullard, William A. Wood, Antonia V. Bennett
Administrative support: Erin Coffman, Elizabeth Bullard
Provision of study materials or patients: Elizabeth Bullard
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Experiences of Inpatient Bone Marrow Transplantation Nurses and Providers Using Electronic Symptom Reporting
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
Ashley Leak Bryant
No relationship to disclose
Erin M. Coffman
No relationship to disclose
Elizabeth Bullard
No relationship to disclose
Rachel Hirschey
No relationship to disclose
Joshua Bradley
No relationship to disclose
Angela Stover
No relationship to disclose
William A. Wood
Research Funding: Genentech (Inst)
Antonia Bennett
No relationship to disclose
REFERENCES
- 1.Basch E, Bennett A, Pietanza MC: Use of patient-reported outcomes to improve the predictive accuracy of clinician-reported adverse events. J Natl Cancer Inst 103:1808-1810, 2011 [DOI] [PubMed] [Google Scholar]
- 2.Basch E, Deal AM, Kris MG, et al. : Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J Clin Oncol 34:557-565, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. US Food and Drug Administration: Guidance for industry: patient-reported outcome measures: Use in medical product development to support labeling claims. Fed Regist 74:65132-65133, 2009. [Google Scholar]
- 4.Cleeland CS, Wang XS, Shi Q, et al. : Automated symptom alerts reduce postoperative symptom severity after cancer surgery: A randomized controlled clinical trial. J Clin Oncol 29:994-1000, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cleeland CS: Symptom burden: Multiple symptoms and their impact as patient-reported outcomes. J Natl Cancer Inst Monogr 2007:16-21, 2007 [DOI] [PubMed] [Google Scholar]
- 6.Anderson KO, Giralt SA, Mendoza TR, et al. : Symptom burden in patients undergoing autologous stem-cell transplantation. Bone Marrow Transplant 39:759-766, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Pidala J, Anasetti C, Jim H: Health-related quality of life following haematopoietic cell transplantation: Patient education, evaluation and intervention. Br J Haematol 148:373-385, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pidala J, Anasetti C, Jim H: Quality of life after allogeneic hematopoietic cell transplantation. Blood 114:7-19, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wood WA, Deal AM, Abernethy A, et al. : Feasibility of frequent patient-reported outcome surveillance in patients undergoing hematopoietic cell transplantation. Biol Blood Marrow Transplant 19:450-459, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howell D, Molloy S, Wilkinson K, et al. : Patient-reported outcomes in routine cancer clinical practice: A scoping review of use, impact on health outcomes, and implementation factors. Ann Oncol 26:1846-1858, 2015 [DOI] [PubMed] [Google Scholar]
- 11.Valderas JM, Kotzeva A, Espallargues M, et al. : The impact of measuring patient-reported outcomes in clinical practice: A systematic review of the literature. Qual Life Res 17:179-193, 2008 [DOI] [PubMed] [Google Scholar]
- 12.Chen J, Ou L, Hollis SJ: A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Serv Res 13:211, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kotronoulas G, Kearney N, Maguire R, et al. : What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. J Clin Oncol 32:1480-1501, 2014 [DOI] [PubMed] [Google Scholar]
- 14.Cooley ME, Blonquist TM, Catalano PJ, et al. : Feasibility of using algorithm-based clinical decision support for symptom assessment and management in lung cancer. J Pain Symptom Manage 49:13-26, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh HF, Shannon SE: Three approaches to qualitative content analysis. Qual Health Res 15:1277-1288, 2005 [DOI] [PubMed] [Google Scholar]
- 16.Patton M: Two Decades of Developments in Qualitative Inquiry: A Personal, Experiential Perspective, Volume 1 London, UK, Sage Publications, 2002 [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377-381, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atkinson TM, Li Y, Coffey CW, et al. : Reliability of adverse symptom event reporting by clinicians. Qual Life Res 21:1159-1164, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fromme EK, Eilers KM, Mori M, et al. : How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the Quality-of-Life Questionnaire C30. J Clin Oncol 22:3485-3490, 2004 [DOI] [PubMed] [Google Scholar]
- 20.Laugsand EA, Sprangers MA, Bjordal K, et al. : Health care providers underestimate symptom intensities of cancer patients: A multicenter European study. Health Qual Life Outcomes 8:104, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cooley ME, Nayak MM, Abrahm JL, et al. : Patient and caregiver perspectives on decision support for symptom and quality of life management during cancer treatment: Implications for eHealth. Psychooncology 26:1105-1112, 2017 [DOI] [PubMed] [Google Scholar]
- 22.Stover AM, Basch EM: The potential role of symptom questionnaires in palliative and supportive cancer care delivery. Curr Oncol Rep 19:12, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stover AM, Basch EM: Implementation of symptom questionnaires into oncology workflow. J Oncol Pract 12:859-862, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]