Short abstract
Objectives
To evaluate home blood pressure (HBP) measurements during pregnancy and postpartum and investigate differences between singleton and twin pregnancies.
Methods
This prospective study involved normotensive, pregnant women who were planning to give birth at Saitama Medical Centre, Saitama, Japan between September 2013 and March 2017. HBP and pulse rate were measured twice daily and clinical blood pressure values were determined from patient records.
Results
HBP values were available from 101 participants; 69 women with singleton and 32 women with twin pregnancies. Systolic BP was statistically significantly higher in twin pregnancies from 23 weeks of gestation until 8 weeks after delivery compared with singleton pregnancies. Pulse rate was also statistically significantly higher between 11 and 30 weeks gestation in women with twin pregnancies compared with those with singleton pregnancies.
Conclusions
BP monitoring is important in the management of twin pregnancies, especially during the later gestational weeks and postpartum period and HBP would facilitate this monitoring.
Keywords: Blood pressure monitoring, home blood pressure, pulse rate, twin pregnancy, pregnancy
Introduction
Blood pressure (BP) is routinely monitored during pregnancy. In recent years, researchers evaluating ambulatory (ABP) and home BP (HBP) measurements have demonstrated that these parameters are more strongly associated with organ damage and long term prognoses compared with clinical BP data.1–3 Indeed, many of the guidelines used for patients with hypertension, including those in Japan, specify that BP measurements should be monitored using ABP or HBP.4–6
Several factors affect BP and include, time of measurement, seasonality, age, sex and body mass index (BMI).7,8 In pregnant women gestational age is also a factor and BP measurements have been shown to decline gradually as the pregnancy progresses with lowest values at approximately 18–20 weeks gestation after which values gradually increase.9–14
In a previous study, we examined HBP variations during pregnancy and postpartum (6 months after delivery) in women with singleton pregnancies. 15 To our knowledge, there is a paucity of data comparing the differences between singleton and twin pregnancies in maternal BP. These data are important since maternal cardiac output has been shown to be higher during a twin pregnancy compared with a singleton pregnancy.16,17 Moreover, twin pregnancy is thought to be associated with an increased risk of hypertensive disorders. 18 Therefore, this present study was designed to evaluate HBP and pulse rate from early pregnancy to 6 months after delivery and compare findings between singleton and twin pregnancies.
Methods
This prospective study involved pregnant women who were planning to give birth at Saitama Medical Centre, Saitama Medical University, Saitama, Japan between September 2013 and March 2017. The study was explained to all women of early gestational age (i.e., approximately 8 – 10 weeks) and enrolled those who provided written informed consent to participate. Eligible participants included women with singleton or twin pregnancies who were able to perform HBP measurements for more than three months and deliver their infants during the study period. Women without diseases known to affect blood pressure (e.g., chronic hypertension, thyroid disease, impaired glucose tolerance, kidney disease, and collagen disease) and without hypertensive disorders in pregnancy were classified as normotensive. The definitions and classifications proposed by the Japan Society of Obstetrics and Gynaecology were used to define hypertensive disorders of pregnancy in this current study 19 (Table 1).
Table 1.
Definitions and classification of hypertensive disorders in pregnancy according to the Japanese Society of Obstetrics and Gynaecology (modified from reference 19 ).
| Definition | |
|---|---|
| Hypertensive disorder of pregnancy | Cases in which hypertension develops; those with a systolic blood pressure of ≥140 mmHg and a diastolic blood pressure of ≥90 mmHg from the 20th week of pregnancy until 12 weeks after delivery, or cases in which hypertension is accompanied by proteinuria (≥300 mg/day) where both of these symptoms are not caused by accidental complications of pregnancy. |
| Classification of disease types | Cases in which hypertension develops and is accompanied by proteinuria after the 20th week of pregnancy and recovers to normal by 12 weeks after delivery. |
| Preeclampsia | Cases in which hypertension develops after the 20th week of pregnancy and recovers to normal by 12 weeks after delivery. |
| Gestational hypertension Superimposed preeclampsia | a) Cases in which chronic hypertension exists before the 20th week of pregnancy and is accompanied by proteinuria after the 20th week of pregnancy. |
| b) Cases in which chronic hypertension and proteinuria exist before the 20th week of pregnancy and either or both of the symptoms become exacerbated after the 20th week of pregnancy. | |
| c) Cases in which renal disease presenting with proteinuria only exists before the 20th week of pregnancy and hypertension develops after the 20th week of pregnancy. |
Participants measured their HBP twice daily after enrolment (i.e., approximately 10 weeks of gestation) to six months after delivery using automatic sphygmomanometers (Omron HEM-7251G, OMRON HEALTHCARE Co., Ltd. Kyoto, Japan). This model of sphygmomanometer has been demonstrated to have an adequately high precision based on the mean differences between the device and mercury readings for systolic and diastolic BP (-0.6 ± 4.7 and -0.2 ± 4.4 mmHg, respectively). 20 HBP measurements were performed according to the Japanese Society of Hypertension 2014 guideline. 4 According to the guidelines, BP was measured on the upper arm by maintaining the arm-cuff position at heart level after a 1–2 min rest period with the participant in a seated position. The first HBP was measured between 0400 and 1000 hours and was within one hour of awakening, after urination and before breakfast. The second HBP measurement was taken between 1500 and 0300 hours before bedtime.
Anonymized identification numbers, dates, systolic and diastolic BP values, pulse rates, room temperatures, times of measurements, fit of the arm cuff, and any movement during measurement were recorded and automatically transferred to a dedicated server managed by OMRON HEALTHCARE Co., Ltd. Kyoto, Japan, using a third generation universal mobile telecommunications system (Medical LINK, OMRON HEALTHCARE). 15 The server was accessed through the internet and data were downloaded for analysis. Identification codes and personal information were protected and only the principal investigator (H.S.) could view this information. Clinical BP data was obtained from patient records and had been measured usually once at each clinic visit, every 1–2 weeks, using an automated sphygmomanometer (BR-203RV II B; OMRON HEALTHCARE Co., Ltd. Kyoto, Japan) which has high accuracy compared with mercurial sphygmomanometers. 21 If two BP readings had been recorded, then the mean value was used for the analysis. Data were obtained from patient records by two investigators (S.E. and Y.O.).
The study protocol was approved by the ethical committee (IRB number; 764) of Saitama Medical Centre, Saitama Medical University and was performed in accordance with the principles of the Declaration of Helsinki.
Statistical analyses
Statistical analyses were performed using JMP software (version 10.0.2; SAS Institute Inc., Cary, NC, USA) and a P<0.05 was considered statistically significant.
Some participants only measured HBP once an occasion and so the first measurement was used in the analyses. To account for the circadian rhythm of BP, 12 guidelines suggest using mean BP values taken over several days4–6 and so according to these recommendations weekly mean values were used in the analyses. Data that had been compromised due to poor fit of the arm cuff and/or movement during the measurement were excluded from the analysis. Student's t-test was used to compare data from singleton and twin pregnancies. Each gestational week was compared but for the postpartum period analysis periods were separated into <4 weeks, 5–8 weeks and 9–12 weeks after delivery. The Steel-Dwass test and Tukey-Kramar test were used to compare data from singleton, dichorionic-diamniotic (DD) twin and monochorionic-diamniotic (MD) twin pregnancies.
Results
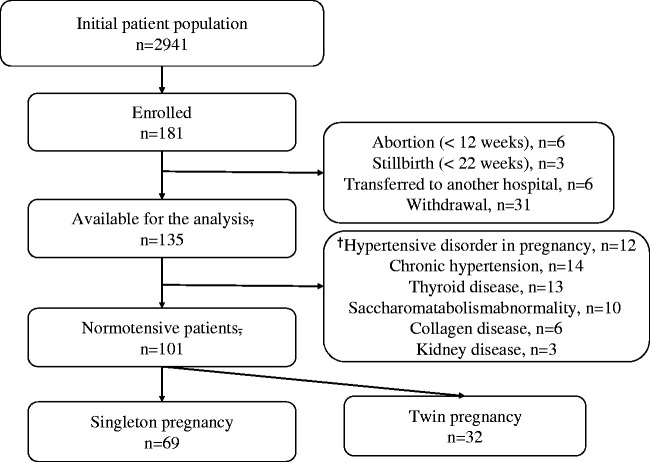
Of the 2941 women screened for the study, 181 were enrolled, of whom 101 (69 singleton, 32 twin pregnancies) were normotensive and so were eligible for the study. A flowchart of study participants is shown in Figure 1. Demographic and gestational characterises of the participants are shown in Table 2. In total, 24,329 records of HBP were obtained, 12,393 records from the morning period and 11,936 records from the evening period.
Figure 1.
Flowchart of the study subjects. † Some participants had more than one disorder. †
Table 2.
Demographic and gestational characteristics of the normotensive participants.
| Characteristic | Singleton pregnancy n = 69 | Twin pregnancy n = 32 |
|
|---|---|---|---|
| DD (n = 20) | MD (n = 12) | ||
| Age, years | 35.21±4.72 | 36.35±3.95 | 34.25±4.27 |
| BMI before pregnancy, kg/m2 | 21.73±4.05 | 23.48±4.93 | 20.55±2.15 |
| Gestational age at delivery, median (range) | 38 weeks, 4 days (31 weeks, 1 days–41 weeks, 1 day) | 37 weeks, 0 days*(35 weeks, 2 days–37 weeks, 3 days) | 36 weeks, 5 days*(29 weeks, 0 days–37 weeks,3 days) |
| Birth weight, g | 2923±521 | 2397±279** | 2156±374** |
| SD value of the birth weight Parity | 0.12±1.23 | −0.56±0.78** | −0.98±0.77** |
| Primipara | 43 (62.3) | 11 (55.0) | 6 (50.0) |
| Multipara | 26 (37.7) | 9 (45.0) | 6 (50.0) |
Values are shown as mean ± SD, or n (%)
DD: dichorionic-diamniotic; MD: monochorionic-diamniotic; SD: standard deviation, BMI, body mass index
*P<0.05 Steel-Dwass test
**P<0.05 Tukey-Kramar test
Interestingly, gestational age at delivery was statistically significantly (P<0.05) younger and birth weight statistically significantly (P<0.05) lower in the twin pregnancy group compared with the singleton pregnancy group (Table 2). No differences in maternal background were observed between singleton, dichorionic-diamniotic (DD) twin and monochorionic-diamniotic (MD) twin pregnancies.
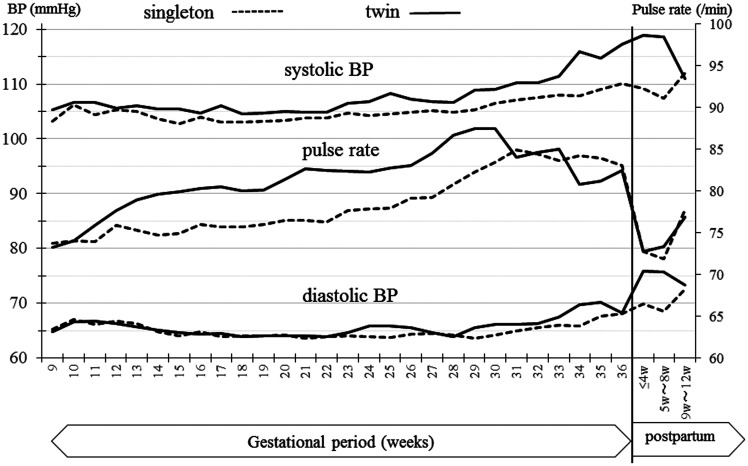
HBP and pulse rate measurements throughout the pregnancies and postpartum period are shown in Figure 2. For the singleton and twin pregnancy groups, HBP values declined during early pregnancy with the lowest values occurring mid-pregnancy. Thereafter, values increased gradually as the gestational age progressed.
Figure 2.
Home blood pressure (HBP) and pulse rates during pregnancy and in the postpartum period in normotensive women. The solid lines show the mean values for the systolic/diastolic BP and pulse rate at each gestational week during twin pregnancies and the dotted lines show the same variables for singleton pregnancies.
With the exception of weeks, 9, 10, 12, 13, 16, 21, and 22, systolic HBP values were statistically significantly higher in the twin pregnancy group than in the singleton pregnancy group for all other weeks. Compared with systolic HBP, there were fewer gestational weeks when diastolic HBP showed differences between singleton and twin pregnancy groups. However, between 24 weeks gestation and 8 weeks post-partum, diastolic HBP values were statistically significantly higher in the twin compared with the singleton pregnancy group. There were no differences between singleton and twin pregnancy groups in HBP values 9–12 weeks after delivery (Figure 2).
Pulse rates increased over the gestational period for both types of pregnancy. For singleton pregnancies, pulse rates were highest at 31 weeks gestation and for twin pregnancies they were highest at 30 weeks gestation. Over gestation weeks 11 to 30, pulse rates were statistically significantly higher in the twin pregnancy group compared with the singleton pregnancy group.
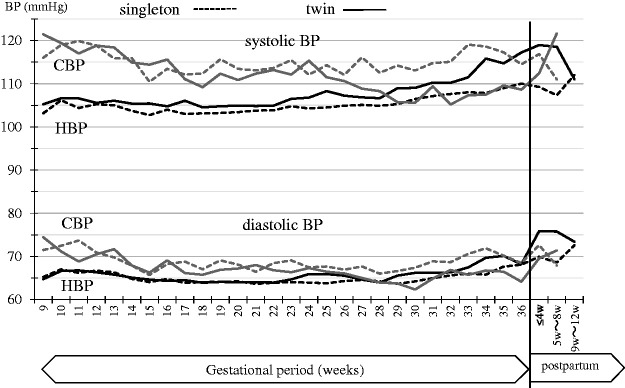
Clinic BP values tended to be higher than HBP values (Figure 3). For women with singleton pregnancies, the pattern of CBP and HBP values were similar. However, CBP and HBP values differed statistically significantly in women with twin pregnancies. For the twin pregnancy group, systolic CBP values decreased as gestational age increased whereas HBP values tended to be level until mid-pregnancy after which time they increased.
Figure 3.
Home blood pressure (HBP) and clinic blood pressure (CBP) values during pregnancy and postpartum period in normotensive women. The solid black lines represent the mean values for systolic/diastolic HBP at each gestational week during twin pregnancy, while dotted black lines represent the same values during singleton pregnancy. Solid grey lines represent the mean values for systolic/diastolic CBP at each gestational week during twin pregnancy, while dotted grey lines represent the same values during singleton pregnancy.
Discussion
In Japan, the incidence of twin births has increased over recent years. 22 In 2010, data from the Ministry of Health, Labour and Welfare indicate that the number of twin births, including live births and stillbirths was 9.6/1000 births. 22 Twin pregnancy is associated with an increased risk of hypertensive disorders including preeclampsia,15,23 therefore longitudinal and careful management of BP during gestation is important. Several guidelines recommend HBP measurements for monitoring BP in pregnancy 4–6,24 In this current study, a large amount of HBP data from early pregnancy to several weeks postpartum were analysed and findings compared between singleton and twin pregnancies.
Variations in HBP and pulse rate during singleton and twin pregnancies were similar to previously reported findings.9–15 Importantly, after 23 weeks gestation, the systolic HBP values during twin pregnancies were statistically significantly higher than those in the singleton pregnancies and this pattern continued until 8 weeks after delivery. In a previous study, researchers observed that BP began to rise after 30 weeks gestation during twin pregnancies. 25 Together, these studies strongly suggest that women with twin pregnancies are at increased risk for high BP as gestational age increases. Furthermore, pulse rates during the twin pregnancies were significantly higher than those during the singleton pregnancies between 11 and 30 weeks gestation.
Perhaps the differences between singleton and twin pregnancies may be associated with differences in the circulating blood volume in the two types of pregnancy. For example, maternal stroke volume and left ventricular mass are greater in women with twin pregnancies compared with those with singleton pregnancies. 16 Furthermore, mean arterial pressure and global time to shortening increase progressively in twin pregnancies after mid-pregnancy. 17 In addition, in the 20th, 28th, and 32nd week of pregnancy, plasma levels of atrial natriuretic peptide (ANP) have been reported to be lower in twin pregnancy compared with singleton pregnancy. 17 ANP exerts a diuretic effect and so its decrease may explain the reason for blood volume being greater in twin than in singleton pregnancies in the middle stages of pregnancy.
The differences observed in this study between clinic BP and HBP might have been due to the small number of clinic BP records available compared with the large amount of HBP data. Although 24,329 recordings of HBP data were obtained, the number of CBP measurements was far lower because recordings had only been made every 1-2 weeks. We observed that gestational age at delivery and birth weight were significantly lower in the twin pregnancy group compared with the singleton pregnancy group and we intend to investigate these findings at a later date.
The study had several limitations. For example, as previously mentioned, there was a disparity between clinic BP and HBP data in the number of recordings. Moreover, data were only available for 32 women with twin pregnancies compared with 69 women with singleton pregnancies and so restricted the generalizability of the results. In addition, HBP measurements were continued for only two to three months postpartum and not six months as specified in the study design. Further, long term studies involving more women are required to substantiate our findings. However, maintaining long term compliance in young women without complications may be difficult because of changes in their daily routine associated with having a new baby.
In conclusion, BP monitoring is important in the management of twin pregnancies, especially during the later gestational weeks and postpartum period and this present study shows that HBP assessments would facilitate the monitoring.
Declaration of conflicting interests
The authors declare that there are no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 1998; 16: 971–975. [DOI] [PubMed] [Google Scholar]
- 2.Her AY, Kim YH, Rim SJ, et al. Home blood pressure is the predictor of subclinical target organ damage like ambulatory blood pressure monitoring in untreated hypertensive patients. Anadolu Kardiyol Derg 2014; 14: 711–718. [DOI] [PubMed] [Google Scholar]
- 3.Karpettas N, Destounis A, Kollias A, et al. Prediction of treatment-induced changes in target-organ damage using changes in clinic, home and ambulatory blood pressure. Hypertens Res. 2014; 37: 543–547. [DOI] [PubMed] [Google Scholar]
- 4.Shimamoto K, Ando K, Fujita T, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH2014). Hypertens Res 2014; 37: 253–392. [DOI] [PubMed] [Google Scholar]
- 5.Imai Y, Kario K, Shimada K, et al. ; Japanese society of hypertension committee for guidelines for self-monitoring of blood pressure at home. The Japanese society of hypertension guidelines for self-monitoring of blood pressure at home (second edition). Hypertens Res 2012; 35: 777–795. [DOI] [PubMed] [Google Scholar]
- 6.Pickering TG, Hall JE, Appel LJ, et al. ; Recommendations for blood pressure measurement in humans: an AHA Scientific Statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. J Clin Hypertens (Greenwich) 2005; 7: 102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kato T, Kikuya M, Ohkubo T, et al. Factors associated with day-by-day variability of self-measured blood pressure at home: The Ohasama Study. Am J Hypertens 2010; 23: 980–986. [DOI] [PubMed] [Google Scholar]
- 8.Hosseini M, Baikpour M, Yousefifard M, et al. Blood pressure percentiles by age and body mass index for adults. EXCLI J 2015; 14: 465–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Macdonald-Wallis C, Tilling K, Fraser A, et al. Established preeclampsia risk factors are related to patterns of blood pressure change in normal term pregnancy: findings from the Avon longitudinal study of parents and children. J Hypertens 2011; 29: 1703–1711. [DOI] [PubMed] [Google Scholar]
- 10.Imai Y, Munakata M, Tsuji I, et al. Seasonal variation in blood pressure in normotensive women studied by home measurements. Clin Sci (Lond) 1996; 90: 55–60. [DOI] [PubMed] [Google Scholar]
- 11.Ochsenbein- Kölble N, Roos M, Gasser T, et al. Cross sectional study of automated blood pressure measurements throughout pregnancy. BJOG 2004; 111: 319–325. [DOI] [PubMed] [Google Scholar]
- 12.Metoki H, Ohkubo T, Watanabe Y, et al. Seasonal trends of blood pressure during pregnancy in Japan: the babies and their parents' longitudinal observation in Suzuki Memorial Hospital in Intrauterine Period study. J Hypertens 2008; 26: 2406–2413. [DOI] [PubMed] [Google Scholar]
- 13.Denolle T, Daniel JC, Calvez C, et al. Home blood pressure during normal pregnancy. Am J Hypertens 2005; 18(9, pt 1): 1178–1180. [DOI] [PubMed] [Google Scholar]
- 14.Metoki H, Ohkubo T, Obara T, et al. Daily serial hemodynamic data during pregnancy and seasonal variation: the BOSHI study. Clin Exp Hypertens 2012; 34: 290–296. [DOI] [PubMed] [Google Scholar]
- 15.Mikami Y, Takai Y, Era S, et al. Provisional criteria for the diagnosis of hypertension in pregnancy using home blood pressure measurement. Hypertens Res 2017; 40: 679–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kametas NA, McAuliffe F, Krampl E, et al. Maternal cardiac function in twin pregnancy. Obstet Gynecol 2003; 102: 806–815. [DOI] [PubMed] [Google Scholar]
- 17.Thomsen JK Fogh-Andersen N andJaszczak P.. Atrial natriuretic peptide, blood volume, aldosterone, and sodium excretion during twin pregnancy. Acta Obstet Gynecol Scand 1994; 73: 14–20. [DOI] [PubMed] [Google Scholar]
- 18.Taguchi T, Ishii K, Hayashi S, et al. Clinical features and prenatal risk factors for hypertensive disorders in twin pregnancies. J Obstet Gynaecol Res 2014; 40: 1584–1591. [DOI] [PubMed] [Google Scholar]
- 19.Seki H. The role of the renin-angiotensin system in the pathogenesis of preeclampsia - new insights into the renin- angiotensin system in preeclampsia. Med Hypotheses 2014; 82: 362–327. [DOI] [PubMed] [Google Scholar]
- 20.Takahashi H Yoshida M andYokoi T.. Validation of two automatic devices: Omron HEM-7252G-HP and Omron HEM-7251G for self-measurement of blood pressure according to the European Society of Hypertension International Protocol revision 2010 . Blood Press Monit 2015: 20: 286–290. [DOI] [PubMed] [Google Scholar]
- 21.Sekine M, Goto E, Ochiai H, et al. Examination of the white coat effect at the time of the blood pressure measurement in the hospital. Therapeutic Research 1997; 18: 118–121. [in Japanese] [Google Scholar]
- 22.Ministry of Health, Labour and Welfare. Annual Report of Vital Statistics of Population, main statistical tables 2010. http://www.mhlw.go.jp/toukei/saikin/hw/jinkou/suii10/. Accessed January 14, 2017.
- 23.Bartsch E, Medcalf KE, Park AL, et al. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies. BMJ 2016; 353: i1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension 2008; 52: 10–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fox NS, Roman AS, Hastings J, et al. Blood pressure changes across gestation in patients with twin pregnancies. J Matern Fetal Neonatal Med 2014; 27: 898–903. [DOI] [PubMed] [Google Scholar]