Abstract
Background
Small scale shared housing arrangements (SHAs) is a deinstitutionalized model of care designed to resemble a typical home of <10 people and are increasingly available for persons with neurocognitive disorders of the Alzheimer's and related types (NCD). However, there is little aggregate evidence of their effect on persons with NCD thus, a literature review was performed.
Methods
Database searches were conducted across CINAHL Complete, OTseeker, PubMed, Ovid, Academic One File, ProQuest Nursing and Allied Health, the World Wide Web and Google Scholar using the several key words that included neurocognitive disorders, Alzheimer's, dementia, quality of life, well-being, occupational performance, activities of daily living, small scale shared housing, sheltered housing and group homes. Bibliographic references from final articles were also examined. Selection criteria involved three steps: screening perspective articles by title and abstract, assessing full text for eligibility and finally, reviewing full-texts.
Results
16 studies were selected for final review where most found the association of SHAs with various occupational performance indicators unique to the NCD population better than or equal to controls (traditional models of long term care). A small minority of studies had mixed or inconclusive results. No study found SHAs necessarily worse than controls.
Conclusion
The SHA model has many benefits for person's with NCD and may be especially advantageous for those in the early stages of the disease process. The occupational therapy profession should continue to raise awareness of SHAs and consider ecological theory as a valid basis for their expansion.
Keywords: Alzheimer's Disease, shared housing, quality of life
Introduction
Background
Numerous issues are confronting the provision of long-term rehabilitative care (LTC) and its effect on quality of life (QpL) for those with neurocognitive disorders of the Alzheimer's and related types (NCDs); given that physical health and function are its intended outcomes, LTC (a parasol term for nursing homes, assisted living, skilled nursing, and similar facilities) has come to be associated with isolation from the community, loss of autonomy, poor occupational performance, and reduced QpL (Teleniusm, Engedal, & Bergland, 2013). Ideally designed to be a living environment first and a workplace second, much criticism has been directed towards the authoritarian, technological, and hierarchical manner in which institutional care is delivered in these settings as most are cold, impersonal, and designed according to a hospital blueprint focused on its efficiency as a workplace rather than the “livability” or occupational performance of its residents (Cutler, Kane, Degenholtz, Miller, & Grant, 2006; Lundgren, 2000; Samus et al., 2005). Many have also found that the supportive nature of LTC, which is meant to be an intervention to enhance participation, in fact, does not suit them and residents often fail to thrive, representing a major paradox for many choosing to live there when they are no longer able to meet the occupational demands of their home environment. To provide more effective occupational therapy services to this underserved and challenged population, awareness about the present limitations of LTC and possible solutions should be discussed as new and promising models of service delivery are now available such as small-scale shared housing arrangements (SHAs), which is a deinstitutionalized model of living that resembles a typical home that accommodates <10 people. Classified as “nursing homes” with highly trained staff, a growing body of research emphasizes the benefits of these unique living arrangements over traditional LTC models, which may have ä100 residents, as several studies have noted improved QpL, better activity of daily living (ADL) performance, and healthier cognitive outcomes (de Rooij et al., 2012; Funaki, Kaneko, & Okamura, 2005; Nakanishi, Nakashimi, & Sawamura, 2012; Smit, de Lange, Willemse, & Pot, 2012; Suzuki, Kanamori, Yasuda, & Oshiro, 2008). The occupational therapy profession has a critical role to play and should be an active partner in the debate concerning the challenges that face LTC and possible solutions such as the implementation of SHAs. This can be achieved through a concerted effort by occupational therapy professionals to raise the awareness of SHAs as they engage in the several forms of service delivery unique to the profession such as direct service provision (i.e., working directly with clients, family, and caregivers), educational, which includes informing various constituents of the nature of issues facing the profession, as well as policy development, which consists of working with management, the public, and government in shaping opinion (Dorrestein & Hocking, 2010).
SHAs are not necessarily new and made their debut in the early 1980s in Scandinavian countries, Japan, and Germany. Representing a novel concept in NCD care at that time, they now account for >25% of all nursing home care in the Netherlands and as of 2008 represented 18% of the total 6,000 special care nursing homes in Japan (Nakanishi et al., 2012; Verbeek et al., 2010). In Germany, there are also >1,400 SHAs, with 460 of them situated in Berlin (Gräske, Meyer, Worch, & Wolf-Ostermann, 2015). Governed as nursing homes, there are many adjectives used to describe these settings, such as shared housing, sheltered housing, or group homes, as well as several trademarked descriptors, of which the most notable may be the “Green House Project” in the United States, which has 185 facilities in 28 states (Pomeroy et al., 2011; Scher-Mclean, 2015). The architectural prototype of this style of care includes multiple small houses clustered in residential-styled neighbourhoods or designed as apartments, which are additions to continuing care retirement communities, or may be incorporated into redesigned segments of assisted living facilities and nursing homes to resemble a typical home (Rabig, 2012). Their core domains embrace the establishment of a family-like environment, the inclusion of relatives, a community orientation, the safeguarding of care provision, along with core principles of well-being as well as self-determination and autonomy and most importantly a “homelike” feel (Gräske, Fischer, Kuhlmey, & Wolf-Ostermann, 2012). Key design components of newly built and proposed units include an emphasis on normal daily routines and environmental details that support occupational performance and QoL. This is achieved by having a floor plan of a characteristic dwelling, private rooms, and bathrooms, a “great room” or large living room, access to outdoors/nature, and in some communities, a fireplace. There is also the integration of pets as well as community meals, with staff who act as central figures that assume the role of universal worker, attending to food preparation, laundry, personal care, habilitation, and general promotion of occupation (Loe & Moore, 2012). In addition, in SHAs day-to-day decisions are typically made by residents themselves or in conjunction with staff, which has shown to have the potential to empower both.
Occupational therapy is at a unique crossroad with those who suffer from NCD as the number of cases in the United States is expected to rise dramatically by the year 2050, with estimates suggesting 14 million people to be affected by the disease, of which 7.0 million will be >85 years (Hebert, Weuve, Scherr, & Evans, 2013). This is almost triple the current 5.5 million cases estimated by Mayeux and Stern (2012). A number of factors are contributing to this phenomenon and most can be ascribed to the changing demographic where the population is expected to increase 27% from 314 million in 2012 to 400 million by 2050 (Ortman, Velkoff, & Hogan, 2014). Studies also estimate that the population aged ä65 will reach 83 million, up significantly from the current 43.1 million representing the fastest growing segment of the U.S. population (He, Sangupta, Velkoff, & Debarros, 2005; Ortman et al., 2014). People are living longer as well. Life expectancy in the year 2030 is projected to be 79.3 years for men and 83.7 years for women, whereas the year 2000 estimates were only 74.1 years for men and 79.3 years for women (U.S. Census Bureau, 2012a, 2012b, p. 77). The trend in the decline in mortality rates has also translated into sizeable increases in survival at older ages. For example, in the United States, the probability of a 65-year-old surviving to age 85 doubled between 1970 and 2005, from about 20% in 1970 to 40% in 2005, which has equated into changes in causes of death, particularly those that effect octogenarians (80–89 years) and nonagenarians (90–99 years) where today major neurocognitive disorders of the Alzheimer's type now represent the sixth leading cause of death (24.7/ 100,000; Bell & Miller, 2005; U.S. Census Bureau, 2012c, p. 91). That number increases to the fifth leading cause of death for those aged 75–84 years (176.7/100,000) and for those ä85 it becomes the fourth leading cause of death at a rate of 849.1/100,000 (U.S. Census Bureau, 2012c, p. 91).
Literature review
The looming NCD crisis proposed by the anticipated shift from 5 million to 14 million cases by 2050 is creating a unique opportunity for today's occupational therapy professionals to not only affect but also guide the debate relative to the expansion of the SHA model of care, as construction of new LTC beds is projected to expand at an annual compound growth rate of 8% over the next decade. Thus, significantly additions are projected to be made to the current 15,700 nursing homes and 22,200 assisted living and similar residential care communities currently in the United States (Basu, 2014; Harris-Kojetin, Sengupta, Park-Lee, & Valverde, 2013). One accepted way to raise awareness of the model among those associated with the profession is through the dissemination of research. However, as bodies of evidence continue to grow through publication, there is the challenge of aggregating that information not only to answer clinical questions but also to provide a vision for the profession as well, and therefore, a literature review (LR) was undertaken. A well-designed LR can identify central issues important to clinicians, explore research methods that have been used successfully elsewhere, identify “gaps” in the current state of evidence, as well as conceptualize both “new” and important theoretical underpinnings to advance the adoption of best evidence-based practices (Classen & Alvarez, 2015; Russell, 2005; Whittemore & Knafl, 2005). Studies were eligible (Table 1) for inclusion if they were published in a peer-reviewed journal between 2004 and 2016 and contained original research involving a critical appraisal of the topic of NCD, SHAs, and one of the many occupational performance indicators unique to the NCD population, which according to Lawton (1994) include competent cognitive functioning, the ability to perform ADLs, and to engage in meaningful use of time and social behaviour, as well as a favourable balance between positive emotion and absence of negative emotional outcomes (Chaudhury, 2003; Berwig, Leicht, Hartwig, & Gertz, 2011).
Table 1.
Characteristics of Selected Articles for the Literature Review.
| Study | Research design | Sample information | Outcome measures | Environmental features | Major findings |
|---|---|---|---|---|---|
| Kok, van Heuvelen, Berg, and Scherder (2016) | Longitudinal Controlled intervention study | n = 15; mean age, 83.1 y; 0.69 female; mean MMSE of 8.59 (Dutch version) | RBMT, 8-Word Test, Trail Making Test A and B, Clox 1 and 2, Geriatric Depression Scale, s-Boston Naming Test, GIT, IQCODE, etc. | n = 67, residing in SHAs of seven to eight people and n = 48, residing in special care units of 15 –30 with up to four persons/bedroom | No significant differences between the two groups were found. However, the majority of effect sizes favoured SHAs over controls not vice versa. In particular, RBMT-face / picture recognition, GIT-figure recognition Trail Making-B, and IQCODE-N. All other measures showed no or only small effect. |
| Kasai, Meguro, Akanuma, and Yamaguchi (2015) | Group comparison, matched pair design | n = 74; mean age, 81.2 y; 0.81 female mean MMSE of 14.1 | BEHAVE-AD, Long-Term Care Level (Care and ADL level), Japanese version of the MMSE | 37 group home SHA dwellings (nine/unit) and 37 community dwelling individuals | SHA patients had significantly fewer symptoms of delusions, aggression, disturbances and anxieties, and phobias when MMSE and ADL care were controlled. |
| Wolf-Ostermann, Worch, Meyer, and Gräske (2014) | Cluster randomized longitudinal design | n = 31; mean age, 77.5 y; 0.74 female, mean MMSE of 11.3 | A developed set of quality indicators, QualiDem | 34 small-scale shared housing arrangements (SHA), six to eight people | No statistical difference between the intervention and control groups on QualiDem accept “feeling at home” (90.2 and 80.3). Mean MMSE scores were better than the control group. |
| Smit, Willemse, de Lange, and Pot (2014) | Direct observational study | n = 57; 0.87 female residing in dementia-specific facilities | Dementia Care Mapping (DCM) | Cross-sectional study of 10 facilities, six with less than eight people/ residence | High mean “well-being” values (+1.5) during expressive, reminiscence, intellectual, and vocational skills. Small facilities ranked (1, 2, 6, 7, 8, 10). |
| Verbeek et al. (2014) | Longitudinal quasi-experimental study | n = 259; mean age, 82.7 y; 0.75 female; mean MMSE < 11 | Neuropsychiatric Inventory-Nursing Home, Cohen –Mansfield Inventory, Cornell Scale for Depression in Dementia, Index of Social Engagement | 28 small-scale shared houses (6–8 people), 21 traditional nursing homes (>20 people) | Small-scale units had less use of physical restraints and less use of psychotropic drugs, more physical Nonaggressive behaviour (aimless wandering, etc.) and more aberrant motor behaviour |
| Wolf-Ostermann, Worch, Fischer, Wulff, and Gräske (2012) | Single-group cohort | n = 56; mean age, 82.5 y; 0.77 female, mean MMSE 13.3 | Barthel Index, NPI-NH, QualiDem, and MMSE | 34 resident of SHAs, 22 residents of special care units, and new admits | During 1 y follow-up, SHA values for most dimensions improved for QoL; ratings between the two settings were marginal except for “care relationship.” |
| de Rooij et al. (2012) | Quasi-experimental, four-group comparison | n = 179; mean age, 85 y; 0.79 female mean S-MMSE 6.5 | QualiDem, NPI-NH, Revised Index of Social Interaction | 98 SHA and 81 nursing homes in Belgium and the Netherlands | Residents of small-scale housing had higher scores on “social relations,” “positive affect,” and “having something to do.” Suggesting some positive benefits. |
| Nakanishi, Nakashimi, and Sawamura (2012) | Two-group cross-sectional design | n = 1,366; mean age, 86.5 y; 0.83 female, the intervention group had known NCD | Quality of Life Instrument for Japanese Elderly with Dementia (QLDJ) | Intervention group (n = 616; 173 SHAs) Control group (n = 750; 174 traditional LTC) | Residents in SHA living facilities had a better QoL (interacting with surroundings, expressing oneself, less negative behaviour) and higher total QoL. |
| Smit, de Lange, Willemse, and Pot (2012) | Cross-sectional study | n = 1,327; mean age, 83.5 y; 0.77 female, mean Katz ADL Inventory Score 5.41 | Resident Assessment Minimum Data Set, Neuropsychiatric Inventory Questionnaire, Katz Inventory | Large-scale nursing homes (n = 27), homes for the aged (n = 17), nursing home where SHA care is provided (n = 31), SHA close to a mother facility (n = 35), stand-alone SHAs (n = 26) | Facilities with more SHA characteristics were more involved in task-related activities, outdoor and leisure activities, physical exercise, and interaction with others. No differences were found in activities such as religion, creativity, intellectual, or activities with senses. |
| Verbeek et al. (2010) | Cross-sectional study | n = 769; mean age, 82.5 y; 0.72 female, mean Cognitive Performance Scale score 4.2 | Activities of Daily Living subscale of the Resident Assessment Minimum Data Set | n = 183; eight people or less, small-scale unit, n = 586; regular n = 586; regular psych-geriatric or nursing home | Residents of small-scale units had higher functional status and cognitive performance when compared with psych-geriatric units. |
| Suzuki, Kanamori, Yasuda, and Oshiro (2008) | Two-group comparison, longitudinal design | n = 26; mean age, 82 y; matched cohort mean MMSE 16.9 | Gottfries–Bråne–Steen Scale (GBS). Disability Assessment for Dementia | n = 13 SHAs with maximum nine people, n = 13 from a traditional unit with a maximum of 117 people | MMSE SHA scores remained stable, whereas those for the control group declined; GBS scores were similar for both groups. DAD-ADL-specific scores for SHAs showed significant improvement. |
| te Boekhorst, Depla, de Lange, Pot, and Eefsting (2009) | Quasi-experimental group comparison | n = 164; mean age, 82.5 y; 0.80 female, mean MMSE 12.4 | Interview for the Deterioration of Daily Living Activities in Dementia, Revised Memory and Behavior Problems Checklist, NPI-Q, RISE, DQoL, QualiDem | n = 67; four to six people living in SHAs, n = 97; <20 living in traditional facilities | Residents of GHs needed less help with ADLs, were more socially engaged, had a better sense of aesthetics, and had more to do. No differences were found in cognitive status or behavioural problems. |
| Kane, Lum, Cutler, Degenholtz, and Yu (2007) | Quasi-experimental group | n = 120; mean age, 85.7 y; 0.81 female, mean Minimum Data Set 3.23 (range, 0–6) | 11 self-report QoL domains of five self-report ADL and six IADL domains on self-report “satisfaction” and “emotional well-being” scale, 24 Quality Indicators for the Minimum Data Set | Four SHAs with 10 people in each. n = 20 with known NCD, control group (n = 80) from traditional facility >65 beds | Controlling baseline characteristics significant differences favoured SHAs over controls. SHAs had higher QoL on nine of 11 items (Control 1) and four of 11 items in (Control 2); however, none of the items were lower in Control 2. |
| Funaki, Kaneko, and Okamura, (2005) | Single-group cohort Longitudinal study | n = 25; mean age, 81.2 y; 0.72 female, mean Hasegawa Dementia Scale (revised) 10.6 | Quality of Life Questionnaire for Dementia, Lawton IADL, Housekeeping Task Test Items, GBS Scale, Troublesome Behavior Scale | n = 25; living in five units in two SHA homes, tested at baseline and 3 mo later | Slight improvement in QoL was seen at 3 mo after entering an SHA across many domains but none were statistically relevant except “housekeeping tasks.” |
| Reimer, Slaughter, Donaldson, Currie, and Eliasziw (2004) | Group comparison matched cohort | n = 185; mean age, 81.7 y; 0.74 female; mean Global Deterioration Score, 6.0 | Cohen–Mansfield Agitation Inventory, Multidimensional Observation Scale of Elderly Subjects, Apparent Affect Rating Scale, FAST Scale, the Pleasant Events Scale | n = 62; six ecological SHA-type units with 10 people in an SCU n = 123 from single traditional, and multiple traditional facilities | QoL was ä in ecological SHA-type dwellings than traditional facilities. Better ADL functioning increased interest and less anxiety and fear were also noted. No differences in cognitive function were noted. |
Note. ADL = activity of daily living; BEHAVE-AD = Behavioral Pathology in Alzheimer's Disease Rating Scale; DAD = Disability Assessment for Dementia Scale; DCM = Dementia Care Mapping; DQoL = Dementia Quality of Life; FAST = Functional Assessment Staging Test; GH = Group Home; GIT = Groningen intelligence test; lADLs = instrumental activities of daily living; IQCODE = Informant Questionnaire on Cognitive Decline in the Elderly; LTC = long-term rehabilitative care; MMSE = Mini-Mental State Examination; NCD = neurocognitive disorders of the Alzheimer's and related types; NPI-NH = Neuropsychiatric Inventory-Nursing Home version; NPI-Q = Neuropsychiatric Inventory-Questionnaire; QLDJ = Quality of Life Instrument for Japanese Elderly with Dementia; QoL = quality of life; RBMT = Rivermead Behavioral Memory Test; RISE = Revised Index of Social Engagement; SCU = special care unit; SHAs = shared housing arrangements.
Methods
A database search was conducted across CINAHL Complete, OTseeker, PubMed, Ovid, Academic OneFile, ProQuest Nursing and Allied Health, the World Wide Web, as well as Google Scholar using the following keywords: neurocognitive disorder(s), Alzheimer's, dementia, fronto-temporal, Lewy body(ies), vascular, quality of life, well-being, occupational performance, activities of daily living, ADLs, small scale shared housing, SHAs, special care facility, sheltered housing, and group home. Bibliographic references from final articles were also examined to provide further insight into the topic. The comprehensive search returned >4,000 articles, of which 240 citations met initial inclusion criteria. Stepwise screening of the 240 articles yielded 85 papers that were inspected in detail and graded on their ability to meet designated conditions outlined by Beerens, Zwakhalen, Verbeek, Ruwaard, and Hamers (2012), which judges an article according to (a) adequate sample size in relation to predictors, (b) use of valid and reliable measures, (c) use of appropriate statistical testing, and (d) discussion and conclusion in line with the results, (e) appropriate description of sampling method, (f) clear description of inclusion and exclusion criteria, (g) appropriate description of participants, (h) appropriate description of cases lost to follow-up, and (i) description of cut-off point for clinical relevance. After careful review of the 85 articles, it was determined that 16 would be included in the final review. Some reasons for exclusion were unreliable methodology; the primary focus was on staff, family or caregiver, or on environmental design. Other reasons included being postoccupancy evaluations, descriptive analyses, or intervention protocols (Figure 1).
Figure 1.
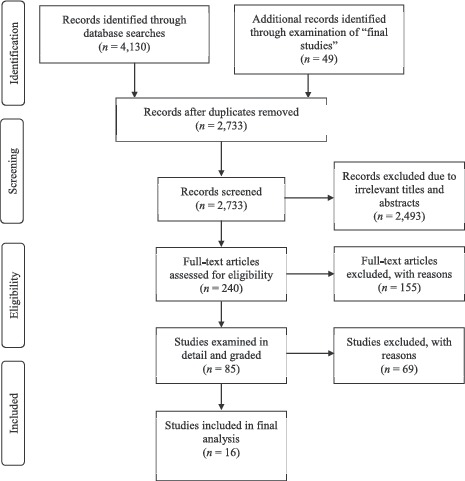
Flow diagram of studies included in final review.
Analysis of final articles
Arguably, most people would prefer to age in place but often there is a need for medical, physical, and occupational therapy services beyond the scope of the home that can only be delivered in a rehabilitative setting when an individual is no longer able to meet the occupational demands of their living environment. Advocating what setting is most appropriate for client and client populations is an important aspect of the profession because a transition to a new environment can affect established roles, as well as routines and meaningful occupations (Mulry, 2012). Using QoL as an indicator, which for the NCD population is a multidimensional concept, several studies found QoL to be better for those clients residing in SHAs when compared with traditional facilities, although QpL can be vague and ill-defined for those with NCD because accurate assessment of one's own QpL is predicated on intact cognitive processes and the ability to retrieve and integrate information into a wider context as well as on awareness of one's life circumstances. Using the Activity Pursuit Patterns subscale from the Resident Assessment Instrument Minimum Data Set a study by Smit et al. (2012) indicated that residents of facilities with more group living home-care characteristics, such as (a) living rooms with a homelike atmosphere, (b) dinner prepared in the kitchen of the home or unit, (c) nursing staff involved in day-to-day chores such as housekeeping, and (d) an environment that supported movement such that the resident could get out of bed whenever they wanted, were more involved in task-related activities, outdoor activities, leisure activities, physical exercise, and interaction with others when compared with traditional LTC settings. Another study found that those facilities that engaged their residents in occupations on a frequent basis more often had a homelike atmosphere, supported social interaction through the environment, and had a decentralized activity program such that activities were chosen through bargaining with the client (Smit et al., 2014). Using the Quality of Life Instrument for Japanese Elderly with Dementia scale as the main outcome, Nakanishi et al. (2012) found that QoL was better for those in SHAs when compared with traditional nursing units as results revealed that “interaction with surroundings” subscale scores and “self-expression” were greater for those residing in SHAs. Funaki et al. (2005) evaluated individuals using the Housekeeping Task Test Item Scale upon entering SHAs and found meaningful change over a 3-month time frame for housekeeping tasks, suggesting that a homelike environment may support the reacquisition of established procedural roles. Using the Disability Assessment for Dementia Scale, Suzuki et al. (2008) found improvement on several ADL items such as hygiene, dressing, eating, meal preparation, finance, correspondence, housework, using the telephone, and going on an outing when compared with traditional facilities. A study of four traditional nursing homes and 12 SHAs in Belgium and the Netherlands using the Revised Index of Social Engagement as the main outcome measure found that residents of the Netherlands SHAs had better social relationships and the indictor of “having something to do” was also better as individuals were more inclined to help with group tasks and perform more personal activities (de Rooij et al., 2012). The same study found that “caregiver relations” and “negative affect” remained stable in small-scale settings according to results of the QUALIDEM, whereas they decreased significantly in traditional LTC settings (de Rooij et al.). The Belgian sample, by contrast, found fewer significant differences in scores between the two settings; however, “negative affect,” was better among residents in small-scale settings. The Belgian sample also found that depressive symptoms, as measured by the Cornell Scale for Depression in Dementia, were higher for traditional units than for small-scale unit settings (de Rooij et al.).
A hallmark of the disablement process posed by NCD often includes an array of heterogeneous neuropsychiatric symptoms such as delusions, hallucinations, agitation, aggression, depression, apathy, euphoria, anxiety, disinhibition, irritability, and aberrant motor behaviour, which may necessitate the need for the prescription of psychotropic drugs, and as much as 69% of all nursing home residents are prescribed at least some type of medication (Galik and Resnick, 2013; Smeets et al., 2013). However, the negative outcomes associated with psychotropic drugs and physical and psychosocial functions have been noted and several studies have shown that their use causes an increased risk of falls, lower self-efficacy, poorer QpL, the presence of aberrant motor movements, sleeping disorders, a higher incidence of stroke, pneumonia, use of physical restraints, and mortality (van der Spek et al., 2013). There is also some evidence to suggest that medication may be contraindicated for those with NCD as they have been shown to use drugs longer and more frequently than general populations. Thus, it is arguable that psychotropic drug use may not only be related to person factors but also to environmental factors. A study by Verbeek et al. (2014) found that the use of psychotropic drugs and physical restraints were much less in SHAs when compared with traditional LTC units. Although their study noted that resident behaviour in SHAs displayed more physically nonaggressive behaviour (such as aimless wandering) and aberrant motor behaviour, this may not necessarily be a negative finding as it may indicate that residents had the environmental and biochemical freedom for such activity (Riemer, Slaughter, Donaldson, Currie, & Eliasziw, 2004). A similar study by te Boekhorst, Depla, de Lange, Pot, and Eefsting (2009) found no significant difference in the use of psychotropic drugs as approximately 65% of both groups were prescribed one or more psychotropic drugs, which is within established findings; however, only 10% of SHA residents were prescribed physical restraints, whereas 50% of those residing in traditional LTC were prescribed restraints.
The last major theme of the LR revolves around cognitive impairment where its diagnosis suggests evidence of significant decline from a previous level of performance in one or more domains such as complex attention, executive function, learning and memory, language, perceptual-motor, or social cognition such that those deficits interfere with ADL engagement that has preferably been documented through standardized neuropsychological testing (American Psychiatric Association, 2013). Using the Mini-Mental State Examination (MMSE) score as the primary outcome measure, which is considered by some to be a “gold standard” of cognitive testing, a matched cohort study showed cognitive function being maintained in residents of SHAs as mean MMSE scores of 17.40 were observed after 1 month, 3 months, and 12 months. In comparison, residents of traditional LTC had a baseline score of 16.40, which decreased to 13.10 after 12 months (Suzuki et al., 2008). A longitudinal cluster-randomized design of 34 SHAs in Berlin showed a decrease in the mean MMSE score for residents of traditional LTC facilities from 12.7 to 10.6, whereas scores in the intervention group (those in SHAs) improved from 11.3 to 12.0 (Wolf-Ostermann, Worch, Meyer, & Gräske, 2014). A third study by Kok, van Heuvelen, Berg, and Scherder (2016) found only marginal differences in MMSE scores that favoured SHAs over LTC models; however, a significant effect size was noted with regard to Trail Making Test-B scores at 4.5 versus 1.5, respectively. Smaller effect sizes were also noted in Rivermead Behavioural Memory subtest scores for face and picture recognition, although other test scores used in the study were inconclusive. Finally, a purposefully built 60-bed facility with six bungalows of 10 people each that followed an ecologic model of care that accentuated a homelike atmosphere was, like the study discussed earlier, typical of the few “mixed results” findings of the LR, which also showed no significant differences in cognitive function when compared with multiple LTC facilities that typically had long corridors with a nursing station at the end, and large noisy dining rooms, as each cohort declined at the same rate. However, the decline in competence in ADLs and affect as reported by family members and staff on the Functional Assessment Staging Test scale and the Apparent Affect Rating Scale, respectively, were not as pronounced in the purposeful built facility as in control groups (Reimer et al., 2004).
Results
Findings of the LR propose that SHAs have many advantages for the NCD population when compared with traditional LTC facilities as most studies found incremental improvement across many performance indicators unique to the NCD population. Although none showed definitively that they were better than controls, there was a tendency in the direction of better performance (objectively assessed and subjectively observed) in most studies (Kok et al., 2016). A small minority of studies (≤3) had results that were mixed or inconclusive, but none found them to be overtly worse than controls, suggesting that the results of the LR were not only worthwhile but also that these living arrangements be considered more sincerely as the first choice for the client with NCD if available. Results also elude to the fact that SHAs may be particularly valuable for those in the early stages of the disease process where ADL roles are familiar, which is in contrast to placement in other types of LTC where the learning curve may be difficult to overcome for the compromised individual. One unfortunate result of the LR was that only one study specific to the United States was included in the final review, suggesting that the current level of research emanating from the United States is limited. Reasons for this vary, and however unfortunate, it necessitates the need for those associated with the profession to continue to raise awareness about the topic. The upside is that the gap in current evidence creates an opportunity for researchers and occupational therapy students to explore.
Ecological framework
The occupational therapy profession and other stakeholders should approach the proposed development of SHAs from the understanding of an ecological model because it recognizes that disability created the moment a person with a pathological condition or injury interacts with an environment that does not support occupational performance because occupation, for those with NCD, is known to affect a person's well-being including positive affect, less depressive symptoms, elevated interest and alertness, less boredom, higher nutrition intake, and decreased use of psychotropic medications (Table 2). By contrast, the lack of engagement in occupations is known to be related to adverse outcomes such as loss of physical function, social isolation, neuropsychiatric symptoms, and poor QpL (Smit et al., 2012; Stark, 2001). By attributing a loss of performance potential to environmental barriers in LTC, the environment becomes a significant factor in the disability creation process and viewing the issue from ecological theory, the decline in functional abilities associated with the process of disablement will shift from an emphasis on impairments to a focus on the environmental demands that may exceed an individual's capacity, suggesting that a person's degree of disability cannot be determined solely by the levels of pathologies, impairments, or functional limitations but must include the extent to which the environment constrains a particular potentially disabling condition (Law, 1991; Patla & Shumway-Cook, 1999; Stark, 2004). Hence, the ecological framework argues that a person's disability should not be defined by the number of tasks that a person can or cannot perform but rather the range of environmental contexts under which tasks are carried out (Patla & Shumway-Cook, 1999).
Table 2.
Ecological Theory Relevant to the Profession of Occupational Therapy.
| Frame of reference | Authors | Summary |
|---|---|---|
| Ecological systems model | Howe and Briggs (1982) | Examines individuals and their environments; considered a continuous process of interaction affecting each through mutual feedback. Function is evaluated in terms of a person's effectiveness in achieving goals through their interactions in the ecosystem and states of health and illness are seen as reflections of ecological adaptation. |
| Person-Environment Occupation Performance model | Christiansen and Baum (1985) as discussed in Baum and Christiansen (2005) | Explores intrinsic “person” factors such as psychological, biological, cognitive, and spiritual, as well as environmental factors considered extrinsic to the person, such as social support, economic systems, culture, the built environment, and technology that either support or restrict the person's performance of activities, tasks, and roles, and how these various components relate and interact with each other to foster performance. |
| Ecology of Human Performance Framework | Dunn, Brown, and McGuigan (1994) | Framework for considering the relationship of person, task, and context, and how the interactions between these three impact activity of daily living and instrumental activity of daily living performance. Interventions are considered through establishing or restoring skills and abilities, altering the contexts in which a person operates, adapting or modifying tasks and environments to foster performance, as well as preventing loss of function and creating opportunities to increase performance. |
| Person-Environment Occupation Model | Lawet al. (1996) | Qualities of person constantly interact with and influence the environment to carry out occupational performance and the environment is seen as the context where occupation occurs. The three major components of the model (person, environment, and occupation) continually interact across time and space in ways that increase or diminish their congruence. The closer their congruence the better occupational performance. |
| Canadian Model of Occupational Performance (CMOP) | Law, Polatajko, Baptiste, and Townsend (1997) | CMOP examines the dynamic relation of person, his/ her environment, and occupations. The model uses a three-dimensional illustration that shows both the interdependence and interplay of person, environment, and occupation and argues that any change in one area will automatically affect the other two by supporting or inhibiting performance. Spirituality is considered central, which gives meaning to occupation. |
| World Health Organization (WHO) International Classification of Functioning, Disability and Health | WHO (2001) | Examines occupational engagement as it relates to (a) body functions, (b) body structures, and (c) activities and participation to encompass functioning at the level of body, the whole person, and the whole person as they relate to their environment (Jette, 2009). Recognizes disability as a multifaceted phenomenon whose cause may be entirely internal or external to the person (WHO, 2002). Views disablement as a composite of biological and social forces that arise out of the complex interaction between health conditions and personal and contextual factors such as the external environment consisting of social attitudes, architectural characteristics, as well as legal and social structures (WHO, 2002). |
| Canadian Model Occupational Performance and Engagement | Polatajko, Townsend, and Craik (2007) | (WHO, 2002). A further expansion of the CMOP model in which of engagement was added as it is considered an aspect of occupation. Core domain is performance, which occurs as a result of interplay between the individual who is a spiritual being, situated at the centre of the model represented by a triangle surrounded by the affective, physical, and cognitive representing person, as well as self-care, productivity, and leisure, which represents occupation, and the physical, cultural, institutional, and social representing the environment. The model also acknowledges the importance of spirituality, which is expressed through occupations. |
Conclusion
For individuals associated with the occupational therapy profession who are constrained by working environments that do not support client health and well-being, a desire for occupational justice exists. A concept that involves the recognition that an inequality in service delivery may be occurring and instills an aspiration for fairness and equal opportunity without discrimination based on disability and includes a social commitment to universal design and accessibility is necessary, enabling people with NCD to flourish to their greatest potential throughout their remaining lifespan (Townsend & Wilcock, 2004). In an occupationally just environment, these individuals have access to and participate in a wide range of occupations for health and social inclusion, share the decision-making power of their daily lives, and receive equal access for diverse participation in occupations (Townsend & Wilcock, 2004). Framing the “long-term care” debate for those with NCD in terms of occupational justice includes recognizing the spheres in which the occupational therapy practitioner and profession may exert influence, tacitly recognizing their ethical, moral, and civic commitment to identify the environmental and system barriers that may be preventing their clients from engaging in occupations to the fullest, that will promote health and QpL (Wolf, Ripat, Davis, Becker, & MacSwiggan, 2010). Requiring practitioners to change their modus operandi and to mobilize around a health advocacy agenda based on progressive thinking about long-term care environments can help to limit occupational injustice, which occurs when one is denied the physical, social, economic, and cultural resources or opportunities to engage in meaningful occupations and is related to occupational alienation, which occurs when people are required to participate in occupations that are meaningless (Nilsson & Townsend, 2010; Wolf et al., 2010). These issues may happen as a result of antiquated social and business policies or other forms of governance that influence how various and competing powers influence and restrict participation in the everyday occupations of underprivileged populations such as those with NCD (Nilsson & Townsend, 2010). The problems are not limited simply to occupational therapy as other health professionals witness injustice in the present long-term care system, and thus strong occupational therapy leadership could empower other health professions and inspire multidisciplinary approaches to support alternative models of service delivery such as SHAs to support health, well-being, and participation. By advancing a critical dialogue about the issues associated with current antiquated models of LTC and the positive benefits of SHAs, the occupational therapy profession will be fulfilling its own mandate of supporting occupation to the fullest for all (Chung, 2004; Nilsson & Townsend, 2010).
Limitations
Although this paper raises awareness of both the issues and opportunities that face the profession of occupational therapy as it relates to LTC for those with NCD, it is limited in its presentation of peer-reviewed research, suggesting that alternative means of gathering and presenting evidence might better advance the breadth and detail of the evidence to the clinician, administrator, or policy maker. For example, a systematic review (SR), which through its construct, delivers a more comprehensive analysis of the full range of literature of a subject. This is achieved by utilizing a rigorous and structured approach to searching, examining, appraising, and summarizing information not seen in the LR. The resulting SR method is thus more inclusive and less biased. Examination of the minutiae details of each database can be a meticulous and time-consuming process; for example, Medline bibliographic alone contains >22 million references, of which approximately 750,000 references were added in 2014 (Portney & Watkins, 2009; U.S. National Library of Medicine, 2015). Which is why, according to Arbesman and Lieberman (2011), the SR is considered level I evidence, whereas an LR is only level V. Any future research involving an SR or other “more rigorous” strategy such as a meta-analysis, which seeks to combine data from highly specific studies, such as randomized control trials, to improve the ability of the clinician to estimate “size” and “effect,” relative to the topic would also be valuable as the quantity and quality of evidence continue to grow concerning SHAs.
Conflicts of interest:
The author declares that no financial or material support of any kind was received for the work described in this article and has no conflicts of interest relevant to this article.
References
- American Psychiatric Association. (2013). Neurocognitive disorders. In: Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Arbesman M., & Lieberman D.. (2011). Methodology for the systematic reviews on occupational therapy for adults with Alzheimer's disease and related dementias. American Journal of Occupational Therapy, 65(5), 490–496. [DOI] [PubMed] [Google Scholar]
- Basu A.. (2014). Forecasting peak demand for senior housing. Construction Executive. Retrieved December 7, 2014, from. http://www.constructionexec.com/Articles/tabid/3837/entryid/2794/forecasting-peak-demand-for-senior-housing.aspx. [Google Scholar]
- Baum C. M., & Christiansen C. H.. (2005). Person-environment-occupation-performance: An occupation-based framework for practice. In Christiansen C. H., Baum C. M., & Bass-Haugen J. (Eds.), Occupational therapy: Performance, participation, and well-being (3rd ed.). Thorofare, NJ: SLACK Incorporated. [Google Scholar]
- Beerens H., Zwakhalen S., Verbeek H., Ruwaard D., & Hamers J.. (2012). Factors associated with quality of life of people with dementia in long-term care facilities: A systematic review. International Journal of Nursing Studies, 50(9), 1259–1270. [DOI] [PubMed] [Google Scholar]
- Bell F., & Miller M. L.. (2005). Life tables for the United States Social Security Area, 1900–2100. Baltimore, MD: Social Security Administration, Office of the Chief Actuary. [Google Scholar]
- Berwig M., Leicht H., Hartwig K., & Gertz H. J.. (2011). Self-rated quality of life in mild cognitive impairment and Alzheimer's disease: The problem of affective distortion. GeroPsych: The Journal of Gerontopsychology and Geriatric Psychiatry, 24(1), 45–51. [Google Scholar]
- Classen S., & Alvarez L.. (2015). Editorial: Evidence-informed reviews—Moving occupational therapy practice and science forward. OTJR: Occupation, Participation and Health, 35(4), 199–203. [DOI] [PubMed] [Google Scholar]
- Chaudhury H.. (2003). Quality of life and place-therapy. Journal of Housing for the Elderly, 17, 85–103. [Google Scholar]
- Chung J. C. C.. (2004). Activity participation and well-being of people with dementia in long-term-care settings. OTJR: Occupation, Participation and Health, 24(1), 22–31. [Google Scholar]
- Cutler L., Kane R., Degenholtz H., Miller M., & Grant L.. (2006). Assessing and comparing physical environments for nursing home residents: Using new tools for greater research specificity. The Gerontologist, 46(1), 42–51. [DOI] [PubMed] [Google Scholar]
- de Rooij A., Luijkx K., Schaafsma J., Declercq A., Emmerink P., & Schols J.. (2012). Quality of life of residents with dementia in traditional versus small-scale long-term care settings: A quasi-experimental study. International Journal of Nursing Studies, 49(8), 931–940. [DOI] [PubMed] [Google Scholar]
- Dorrestein M., & Hocking C.. (2010). Maximising participation for older people: Scoping the occupational therapy role in residential care settings. New Zealand Journal of Occupational Therapy, 57(2), 49–55. [Google Scholar]
- Dunn W., Brown C., & McGuigan A.. (1994). The ecology of human performance: A framework for considering the effect of context. American Journal of Occupational Therapy, 48, 595–607. [DOI] [PubMed] [Google Scholar]
- Funaki Y., Kaneko F., & Okamura H.. (2005). Study on factors associated with changes in quality of life of demented elderly persons in group homes. Scandinavian Journal of Occupational Therapy, 12(1), 4–9. [DOI] [PubMed] [Google Scholar]
- Galik E., & Resnick B.. (2013). Psychotropic medication use and association with physical and psychosocial outcomes in nursing home residents. Journal of Psychiatric and Mental Health Nursing, 20, 244–252. [DOI] [PubMed] [Google Scholar]
- Gräske J., Fischer T., Kuhlmey A., & Wolf-Ostermann K.. (2012). Dementia-specific quality of life instruments and their appropriateness in shared-housing arrangements—A literature study. Geriatric Nursing, 33(3), 204–216. [DOI] [PubMed] [Google Scholar]
- Gräske J., Meyer S., Worch A., & Wolf-Ostermann K.. (2015). Family visits in shared-housing arrangements for residents with dementia—A cross-sectional study on the impact on residents’ quality of life. BMC Geriatrics, 15, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris-Kojetin L., Sengupta M., Park-Lee E., & Valverde R.. (2013). Long-term care services in the United States: 2013 overview. In: National health care statistics reports: No. 1 (pp. 32–35). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- He W., Sangupta M., Velkoff V. A., & Debarros K.. (2005). 65+ in the United States: 2005. Current population reports (P23–209). Washington, DC: U.S. Census Bureau. [Google Scholar]
- Hebert L., Weuve J., Scherr P., & Evans D.. (2013). Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology, 80(19), 1778–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe M., & Briggs A.. (1982). Ecological systems model for occupational therapy. American Journal of Occupational Therapy, 36(5), 322–327. [DOI] [PubMed] [Google Scholar]
- Jette A.. (2009). Toward a common language of disablement. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64A(11), 1165–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane R. A., Lum T. Y., Cutler L. J., Degenholtz H. B., & Yu T. C.. (2007). Resident outcomes in small-house nursing homes: A longitudinal evaluation of the initial green house program. Journal of the American Geriatrics Society, 55(6), 832–839. [DOI] [PubMed] [Google Scholar]
- Kasai M., Meguro K., Akanuma K., & Yamaguchi S.. (2015). Alzheimer's disease patients institutionalized in group homes run by long-term care insurance exhibit fewer symptoms of behavioural problems as evaluated by the Behavioural Pathology in Alzheimer's Disease Rating Scale. Psychogeriatrics, 15(2), 102–108. [DOI] [PubMed] [Google Scholar]
- Kok J., van Heuvelen M., Berg I., & Scherder E.. (2016). Small scale homelike special care units and traditional special care units: Effects on cognition in dementia; a longitudinal controlled intervention study. BMC Geriatrics, 16(1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law M.. (1991). The environment: A focus for occupational therapy: 1991 Muriel Driver Lecture. The Canadian Journal of Occupational Therapy, 58(4), 171–179. [DOI] [PubMed] [Google Scholar]
- Law M., Cooper B., Strong S., Stewart D., Rigby P., & Letts L.. (1996). The person-environment-occupation model: A transactive approach to occupational performance. Canadian journal of occupational therapy, 63(1), 9–23. [DOI] [PubMed] [Google Scholar]
- Law M., Polatajko H., Baptiste S., & Townsend E.. (1997). Core concepts of occupational therapy. In: Canadian Association of Occupational Therapists. Enabling occupation: An occupational therapy perspective (pp. 29–56). Ottawa, ON: CAOT Publications ACE. [Google Scholar]
- Lawton M. P.. (1994). Quality of life in Alzheimer disease. Alzheimer Disease & Associated Disorders, 8, 138–150. [PubMed] [Google Scholar]
- Loe M., & Moore C. D.. (2012). From nursing home to green house: Changing contexts of elder care in the United States. Journal of Applied Gerontology, 31(6), 755–763. [Google Scholar]
- Lundgren E.. (2000). Homelike housing for elderly people—Materialized ideology. Housing Theory and Society, 17, 109–120. [Google Scholar]
- Mayeux R., & Stern Y.. (2012). Epidemiology of Alzheimer disease. Cold Spring Harbor Perspectives in Medicine. 2(8), 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulry C. M.. (2012). Transitions to assisted living: A pilot study of residents’ occupational perspectives. Physical & Occupational Therapy in Geriatrics, 30(4), 328–343. [Google Scholar]
- Nakanishi M., Nakashimi T., & Sawamura K.. (2012). Quality of life of residents in a group living situation: An approach to creating small, homelike environments in traditional nursing homes in Japan. Japanese Journal of Public Health, 59(1), 3–10. [DOI] [PubMed] [Google Scholar]
- Nilsson I., & Townsend E.. (2010). Occupational justice—Bridging theory and practice. Scandinavian Journal of Occupational Therapy, 17(1), 57–63. [DOI] [PubMed] [Google Scholar]
- Ortman J. M., Velkoff V. A., & Hogan H.. (2014). An aging nation: The older population in the United States. Current population reports (P25–1140). Washington, DC: U.S. Census Bureau. [Google Scholar]
- Patla A. E., & Shumway-Cook A.. (1999). Dimensions of mobility: Defining the complexity and difficulty associated with community mobility. Journal of Aging and Physical Activity, 7(1), 7–19. [Google Scholar]
- Polatajko H. J., Townsend E. A., & Craik J.. (2007). Canadian model of occupational performance and engagement (CMOP-E). In Townsend E. A., & Polatajko H. J. (Eds.), Enabling occupation II: Advancing an occupational therapy vision of health, well-being, & justice through occupation (pp. 22–36). Ottawa, ON: CAOT Publications ACE. [Google Scholar]
- Pomeroy S., Scherer Y., Runkawatt V., lamsumang W., Lindemann J., & Resnick B.. (2011). Person–environment fit and functioning among older adults in a long-term care setting. Geriatric Nursing, 32(5), 368–378. [DOI] [PubMed] [Google Scholar]
- Portney L. G., & Watkins M. P.. (2009). Foundations of clinical research. Saddle River, NJ: Pearson Education, Inc. [Google Scholar]
- Rabig J.. (2012). Small house nursing homes (some are trademarked as Green Houses). In: Livable New York: Sustainable communities for all ages. New York: Division of Policy, Research, and Legislative Affairs, New York State Office for the Aging. [Google Scholar]
- Reimer M., Slaughter S., Donaldson C., Currie G., & Eliasziw M.. (2004). Special care facility compared with traditional environments for dementia care: A longitudinal study of quality of life. Journal of the American Geriatrics Society, 52(7), 1085–1092. [DOI] [PubMed] [Google Scholar]
- Russell C. L.. (2005). An overview of the integrative research review. Progress in transplantation, 15(1), 8–13. [DOI] [PubMed] [Google Scholar]
- Samus Q., Rosenblatt A., Steele C., Baker A., Harper M., Brandt J. et al. (2005). The association of neuropsychiatric symptoms and environment with quality of life in assisted living residents with dementia. The Gerontologist, 45(sp I), 19–26. [DOI] [PubMed] [Google Scholar]
- Scher-Mclean R.. (2015). 2015: A year of remarkable growth. Green house project blog. Retrieved February 9, 2016, from http://blog.thegreenhouseproject.org/2015highlights/. [Google Scholar]
- Smeets C., Smalbrugge M., Gerritsen D., Nelissen-Vrancken M., Wetzels R. B., van der Spek K. et al. (2013). Improving psychotropic drug prescription in nursing home patients with dementia: Design of a cluster randomized controlled trial. BMC Psychiatry, 13(280), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit D., de Lange J., Willemse B., & Pot A. M.. (2012). The relationship between small-scale care and activity involvement of residents with dementia. International Psychogeriatrics, 24(5), 722–732. [DOI] [PubMed] [Google Scholar]
- Smit D., Willemse B., de Lange J., & Pot A. M.. (2014). Well-being-enhancing occupation and organizational and environmental contributors in long-term dementia care facilities: an explorative study. International Psychogeriatrics, 26(01), 69–80. [DOI] [PubMed] [Google Scholar]
- Stark S.. (2001). Creating disability in the home: The role of environmental barriers in the United States. Disability and Society, 16(1), 37–49. [Google Scholar]
- Stark S.. (2004). Removing environmental barriers in the homes of older adults with disabilities improves occupational performance. OTJR: Occupation, Participation and Health, 24(1), 32–39. [Google Scholar]
- Suzuki M., Kanamori M., Yasuda M., & Oshiro H.. (2008). One-year follow-up study of elderly group-home residents with dementia. American Journal of Alzheimer's Disease and Other Dementias, 23(4), 334–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- te Boekhorst S., Depla M., de Lange J., Pot A. M., & Eefsting J.. (2009). The effects of group living homes on older people with dementia: A comparison with traditional nursing home care. International Journal of Geriatric Psychiatry, 24(9), 970–978. [DOI] [PubMed] [Google Scholar]
- Teleniusm E., Engedal K., & Bergland A.. (2013). Physical performance and quality of life of nursing-home residents with mild and moderate dementia. International Journal of Environmental Research and Public Health, 10(12), 6672–6686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend E., & Wilcock A.. (2004). Occupational justice and client centered practice: A dialogue in progress. The Canadian Journal of Occupational Therapy, 71(2), 75–87. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2012. a). 2012 National population projections: Summary tables. Table 10; projected life expectancy at birth by sex, race, and Hispanic origin for the United States: 2015 to 2060. Retrieved December 4, 2014, from: http://www.census.gov/population/projections/data/national/2012/summarytables.html.
- U.S. Census Bureau. (2012. b). Table 104; expectation of life at birth, 1970 to 2008, and projections, 2010 to 2020, births, deaths, marriages, and divorces. U.S. Census Bureau, Statistical Abstract of the United States: 2012 (131st ed., p. 77). Washington, DC: U.S. Census Bureau. [Google Scholar]
- U.S. Census Bureau. (2012. c). Table 122; deaths and death rates by leading causes of death and age: 2007, births, deaths, marriages, and divorces. U.S. Census Bureau, Statistical Abstract of the United States: 2012 (131st ed., p. 91). Washington, DC: U.S. Census Bureau. [Google Scholar]
- U.S. National Library of Medicine. (2015). Fact sheet: Medline. Retrieved September 6, 2015, from www.nlm.nih.gov/pubs/factsheets/medline.html. [Google Scholar]
- van der Spek K., Gerritsen D., Smalbrugge M., Nelissen-Vrancken M., Wetzels R., Smeets C. et al. (2013). PROPER I: Frequency and appropriateness of psychotropic drugs use in nursing home patients and its associations: A study protocol. BMC Psychiatry, 13(307), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbeek H., Zwakhalen S. M., van Rossum E., Ambergen T., Kempen G., & Hamers J.. (2010). Small-scale, homelike facilities versus regular psychogeriatric nursing home wards: A cross-sectional study into residents’ characteristics. BMC Health Services Research, 10(30), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbeek H., Zwakhalen S. M., van Rossum E., Ambergen T., Kempen G., & Hamers J.. (2014). Effects of small-scale, homelike facilities in dementia care on residents’ behavior, and use of physical restraints and psychotropic drugs: A quasi-experimental study. International Psychogeriatrics, 26(4), 657–668. [DOI] [PubMed] [Google Scholar]
- Whittemore R., & Knafl K.. (2005). The integrative review: Updated methodology. Journal of Advanced Nursing, 52(5), 546–553. [DOI] [PubMed] [Google Scholar]
- Wolf L., Ripat J., Davis E., Becker P., & MacSwiggan J.. (2010). Applying an occupational justice framework. Occupational Therapy Now, 12(1), 15–18. [Google Scholar]
- Wolf-Ostermann K., Worch A., Fischer T., Wulff I., & Gräske J.. (2012). Health outcomes and quality of life of residents of shared-housing arrangements compared to residents of special care units–results of the Berlin DeWeGE-study. Journal of clinical nursing, 21(21-22), 3047–3060. [DOI] [PubMed] [Google Scholar]
- Wolf-Ostermann K., Worch A., Meyer S., & Gräske J.. (2014). Quality of care and its impact on quality of life for care-dependent persons with dementia in shared-housing arrangements: Results of the Berlin WGQual-study. Applied Nursing Research, 27(1), 33–40. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2001). International classification of functioning, disability and health: ICF. Geneva: World Health Organization. [Google Scholar]
- World Health Organization. (2002). Towards a common language for functioning, disability and health: ICF the international classification of functioning, disability and health (p. 10). Geneva, Switzerland: World Health Organization. [Google Scholar]


