Abstract
Background
This study aimed to investigate the effects of an oropharyngeal motor training programme on children with Obstructive Sleep Apnea Syndrome (OSAS) in Hong Kong.
Methods
In this retrospective study, we reviewed the outcomes of 10 children with OSAS who had received an oropharyngeal motor training programme in Occupational Therapy Department of an acute hospital in Hong Kong over a 1-year programme. Each participant attended an individual oropharyngeal motor training programme plus a follow-up session after 2 months. The training programme consisted of 10 individual mobilization exercises involving the orofacial and pharyngeal area for 45 minutes. Each exercise had to be repeated for 10 times. Three outcome measures were chosen to study the effectiveness of the training programme including tongue strength, tongue endurance level and orofacial function. Tongue strength and tongue endurance level were assessed using the Iowa Oral Pressure Instrument (IOPI). The Nordic Orofacial Test-Screening (NOT-S) Assessment was used to assess the orofacial function. Seven out of 10 participants completed the training programme and attended the follow-up session after two months.
Results
The tongue strength and the scores of NOT-S of the 7 participants were found to have significant improvement after training. However, there was no significant difference in tongue endurance level.
Conclusion
The findings of this study support the role of occupational therapist in oromotor training modalities to improve the respiratory function for children with OSAS in Hong Kong. Copyright © 2017, Hong Kong Occupational Therapy Association. Published by Elsevier (Singapore) Pte Ltd. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Keywords: Obstructive sleep apnea syndrome, Children, Oropharyngeal motor training, Tongue strength
Introduction
Current traditional management of obstructive sleep apnea syndrome (OSAS) includes non-invasive ventilation, e.g. Continuous Positive Airway Pressure Therapy (CPAP), surgical treatment e.g. adenotonsillectomy and tongue suspension, and non-surgical treatment e.g. the use of oral appliance (An & Ranson, 2011; Capdevila, Kheirandish-Gozal, Dayyat & Gozal, 2008; Rosen, 2004).
Recent evidences revealed that the orofacial developmental disorders in children with OSAS may be caused by orofacial anatomic abnormalities which result in upper airway obstruction, these abnormalities included high arch palate, hypotonic tongue and lips muscles (Clark, O'Brien, Calleja, & Corrie, 2009; Guimarães, Drager, Genta, Marcondes, & Lorenzi-Filho, 2009; Huang & Guilleminault, 2013). Findings of several studies have indicated that oropharyngeal motor training programme could be useful to improve the muscle tone of the tongue, throat, and face, which could increase the anatomical space of the orofacial structures and hence, reduce obstruction to the airway (Huang & Guilleminault, 2013; Leme, Barbosa, & Gavião, 2012; Logemann, 2008; Potter & Short, 2009; Randerath, Galetke, Domanski, Weitkunat, & Ruhle, 2004; Varjão, 2012).
An oropharyngeal motor training programme has been used by a group of occupational therapists in Taiwan to reduce obstructive sleep apnea and symptoms of sleep disordered breathing in children such as snoring and mouth breathing (Huang & Guilleminault, 2013). This pilot study adopted the oropharyngeal motor training programme from Taiwan (Huang & Guilleminault, 2013) to be used in Hong Kong for children with OSAS. This case study aimed to investigate retrospectively the effects of this oropharyngeal motor training programme for children with OSAS in Hong Kong.
Methods
Participants
Ten children, aged 6–18 years, diagnosed with OSAS, were referred from the Paediatric Sleep Clinic to Occupational Therapy Department for oropharyngeal motor training in an acute hospital in Hong Kong. Data of this study was collected over one year from January to December 2014. Participants had received oropharyngeal motor training during the above period. All participants had their pretraining Apnea—hypopnea Index (AHI) greater than 1.0 as confirmed by the Polysomnography (PSG).
Procedure
An occupational therapist in the hospital, who had received prior training in this area, provided an individual session of the oropharyngeal motor training programme to all the participants. The training aimed to correct the improper function of the tongue and facial muscles. This training was a re-education training in order to strengthen the tongue and oral-facial muscles by teaching individuals on how to reposition muscles to the appropriate position. Assessments were conducted at two time points: (a) before training, and (b) 2 months post-training.
The training programme consisted of 10 individual mobilization exercises involving orofacial and pharyngeal area that required 45 minutes to complete. Each exercise had to be repeated for 10 times. The 10 exercises were:
Exercise 1: Pushing Up The Tongue
Exercise 2: Touching Nose
Exercise 3: Touching Chin
Exercise 4: Pushing Tongue Right and Left
Exercise 5: Folding Tongue
Exercise 6: Clicking the Tongue
Exercise 7: Pushing Tongue Against Spoon
Exercise 8: Holding A Spoon
Exercise 9: Holding Button with Lips
Exercise 10: Gargling
During the training session, the Occupational Therapist went through all the exercise items with participants and an instruction sheet was provided to them for home programme. A daily time log was also given to each participant to record their compliance to the home programme. Each participant was then followed up in two months' time.
Outcome Measures
In order to study the effectiveness of the oropharyngeal motor training programme, three outcome parameters were chosen: orofacial function, tongue strength and tongue endurance level. The orofacial function of the participants was assessed by the Nordic Orofacial Test-Screening (NOT-S) Assessment (Leme et al., 2012), while the tongue strength and tongue endurance level were assessed using the Iowa Oral Pressure Instrument (IOPI) (Potter & Short, 2009). They were conducted by a trained occupational therapist.
Nordic Orofacial Test-Screening (NOT-S) Assessment
The NOT-S assessment was used for patients aged 3 years or above who had difficulties to speak, chew or swallow. It was developed by the Mun-H-Center in Sweden with a total score of 12 (Leme et al., 2012). It includes two parts, the NOT-S interview session and the NOT-S examination session. The NOT-S interview consists of six sections: sensory function, breathing, habits, chewing and swallowing, drooling, and dryness of the mouth. The NOT-S examination consists of six sections: face at rest, nose breathing, facial expression, masticatory muscle and jaw function, oral motor function, and speech (Leme et al., 2012). The illustrated manual was used during the examination. If an individual answers yes or unable to fulfill the requirement of the examination tasks, the corresponding item will be scored as 1 mark. The NOT-S total score would vary from 0 to 12 (Leme et al., 2012). The higher the NOT-S score, the worse would be the orofacial dysfunction of the person.
Iowa Oral Pressure Instrument (IOPI)
The IOPI is an objective instrument to measure one's tongue and lip strength and endurance (Potter & Short, 2009). It contains a portable machine, a connecting tube and a tongue bulb. In order to measure a person's tongue strength and endurance, the tongue bulb is placed in the patient's mouth just behind the alveolar ridge. The tongue strength is measured in kilopascals (kPa), while the endurance level is measured in seconds (s) (Potter & Short, 2009).
Statistical Analysis
All collected data was analyzed by SPSS 22.0. In order to identify the effects of the oropharyngeal motor training programme, primary outcomes of tongue strength, tongue endurance level and NOT-S scores were chosen. Due to the small sample size and with the result of normality tests, non-parametric test — related-samples Wilcoxon Signed Rank test, was chosen for pre/post comparison in the statistical analysis. A p value of 0.05 or less was considered to be statistically significant.
Results
There were seven out of 10 participants, aged 7 to 18 years old, completed the training programme and attended the follow-up session after 2 months. Before the training, five of them had received adenotonsillectomy whilst the other two did not receive any surgery (Table 1).
Table 1.
Demographic of Participants (n = 7)
| Variable | Number | |
|---|---|---|
| Gender | ||
| Male | 6 | |
| Female | 1 | |
| Age (Years) | Mean = 12.86 (SD = 4.95) | |
| 7 | 2 | |
| 11 | 1 | |
| 12 | 1 | |
| 16 | 1 | |
| 18 | 2 | |
| Received adenotonsillectomy before | 5 | |
| AHI (>1.0) | 7 | Mean = 7.92 (SD = 12.15) |
AHI = Apnea-hypopnea Index.
The mean difference in tongue strength of the 7 participants after training programme was found to be statistically significant (p = 0.18) ( Table 2 ), however, there was no significant difference in the mean tongue endurance after training (p = 0.203) ( Table 2 ).
Table 2.
Results of Comparison of Training
| Pre-training | Post-training | p | |
|---|---|---|---|
| Tongue strength (kPa) | Mean = 38.00, SD = 12.11 | Mean = 48.29, SD = 11.38 | 0.018* |
| Tongue endurance (second) | Mean = 6.43, SD = 3.60 | Mean = 8.71, SD = 5.12 | 0.203 |
| NOT-S total score | Mean = 5.29, SD = 2.50 | Mean = 3.14, SD = 2.73 | 0.026* |
NOT-S = Nordic Orofacial Test-Screening.
p < 0.05.
The median of differences between in NOT-S total score showed that there was significant improvement before and after training (p = 0.026) (Table 2, Figs. 1 and 2).
Figure 1.

Training results of NOT-S interview performance among seven participants.
Figure 2.
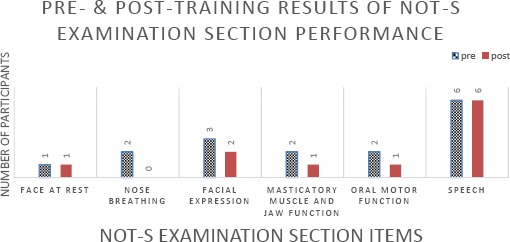
Training results of NOT-S examination performance among seven participants.
Discussion
We had conducted this case study to explore the effects of an oropharyngeal motor training programme for children with OSAS in Hong Kong. The results showed that a 2-month training programme was useful in increasing their tongue strength from 6% to 76%.
According to results of the Nordic Orofacial Test-Screening (NOT-S) Assessment, six out of 7 participants showed improvement in orofacial function after the training in various aspects, including shorter chewing time during feeding (NOT-S interview item IV: less than or equal to 30 minutes to eat a main meal) and promoting the habit of nose breathing instead of mouth breathing while at rest (NOT-S examination item 2: able to take 5 breaths in succession through the nose).
The verbal feedbacks from both the parents and the participants showed that the training was useful in improving their oromotor function during feeding, which is one of the important activities of daily living (ADL) concerned by occupational therapists. As this is a new training programme in occupational therapy in Hong Kong, this finding implies oropharyngeal training will be a new training technique that should be advocated by occupational therapists to improve oral feeding function and reduce breathing difficulties during sleeping in children with OSAS.
According to the present findings of our study, we found that this oropharyngeal motor training programme could improve the symptoms of children with OSAS such as oromotor function including chewing and feeding and reducing mouth breathing. These findings are similar to findings of other overseas training programmes in Brazil and Taiwan as children with OSAS are found to have abnormal orofacial growth due to orofacial hypotonia (Guimarães et al. (2009); Huang and Guilleminault (2013)), where persistent abnormal tongue position and presence of mouth breathing were often found during PSG. After repetitive orofacial exercises, a normal orofacial musculature as well as oromotor function can be induced.
There were several limitations in this case study. Our sample size was too small and owing to the resources limitation, the reported training effects had not been further confirmed with the Apnea—hypopnea Index (AHI) by Polysomnography (PSG) at the later follow-up period. Therefore, further research with a larger sample size and the arrangement of a follow-up PSG after the training programme is necessary in order to investigate the effects of generalization to a larger population as well as reducing symptoms of Apnea across a longer time period.
Acknowledgements
We would like to give a special acknowledgement to Dr. Daniel K. K. Ng, Kwong Wah Hospital, for the support of the training programme.
Funding/Support:
No funding and financial disclosures were reported by the authors of this paper.
Conflicts of interest:
All contributing authors declare that they have no conflicts of interest.
References
- An S.-L., & Ranson C. (2011). Obstructive sleep apnea for the dental hygienist: Overview and parameters for interprofessional practice. Canadian Journal of Dental Hygiene, 45(4), 238–252. [Google Scholar]
- Capdevila O. S., Kheirandish-Gozal L., Dayyat E., & Gozal D. (2008). Pediatric obstructive sleep apnea complications, management, and long-term outcomes. Proceedings of the American Thoracic Society, 5, 274–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark H. M., O'Brien K., Calleja A., & Corrie S. N. (2009). Effects of directional exercise on lingual strength. Journal of Speech Language and Hearing Research, 52(4), 1034–1047. [DOI] [PubMed] [Google Scholar]
- Guimarães K. C., Drager L. F., Genta P. R., Marcondes B. F., & Lorenzi-Filho G. (2009). Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. American Journal of Respiratory and Critical Care Medicine, 179(10), 962–966. [DOI] [PubMed] [Google Scholar]
- Huang Y., & Guilleminault C. (2013). Pediatric obstructive sleep apnea and the critical role of oral-facial growth: Evidences. Frontiers in Neurology, 3, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leme M. S., Barbosa T. D., & Gavião M. B. (2012). Assessment of orofacial functions in Brazilian children using the nordic orofacial test-screening (NOT-S). Revista Odonto Ciência, 27(2), 108–114. [Google Scholar]
- Logemann J. A. (2008). Treatment of oral and pharyngeal dysphagia. Physical Medicine and Rehabilitation Clinics of North America, 19(4), 803–816. [DOI] [PubMed] [Google Scholar]
- Potter N. L., & Short R. (2009). Maximal tongue strength in typically developing children and adolescents. Dysphagia, 24(4), 391–397. [DOI] [PubMed] [Google Scholar]
- Randerath W. J., Galetke W., Domanski U., Weitkunat R., & Ruhle K. (2004). Tongue-muscle training by intraoral electrical neurostimulation in patients with obstructive sleep apnea. Sleep, 27(2), 254–259. [DOI] [PubMed] [Google Scholar]
- Rosen C. L. (2004). Obstructive sleep apnea syndrome in children: Controversies in diagnosis and treatment. The Pediatric Clinics of North America, 51, 153–167. [DOI] [PubMed] [Google Scholar]
- Varjão F. M. (2012). Myofunctional therapy as an aid to prosthodontic treatment after hemiglossectomy: A clinical report. The Journal of Prosthetic Dentistry, 107(5), 284–287. [DOI] [PubMed] [Google Scholar]


