Abstract
Background/Objective
Mindfulness-based intervention has received more clinical interest and empirical support for individuals with ADHD especially to improve attention. However, no systematic review has been done to analyze and compare the effectiveness of mindfulness-based intervention on individuals with ADHD in different age groups. This review examined its effectiveness for individuals (children, adolescents and adults) with ADHD to improve attention.
Methods
In 7 databases, totally of 152 studies were identified; 9 met the inclusion and exclusion criteria and were reviewed. Five of the studies recruited adults as the participants, two recruited adolescents as the participants, one recruited both adults and adolescents as the participants and one recruited children as the participants.
Results
It was found that mindfulness-based intervention was comparatively more popularly used in adults with ADHD to improve attention, and the improvement was significant.
Conclusion
It is still unclear whether mindfulness-based intervention is effective for children and adolescence with ADHD due to limited studies available and the limitations of the study design in the reviewed studies. Therefore, more research in the future is required to answer the question.
Keywords: Mindfulness, ADHD, Attention deficits
ADHD is a neurobiological disorder described by symptoms of inattention, hyperactivity and/or impulsivity (APA, 2013). According to the U.S. Centers for Disease Control and Prevention (CDC), 7.8% of children aged between 4 and 17 years have been diagnosed with ADHD. From the National Comorbidity Survey Replication, 4.4% of US adults aged between 18 and 44 years have matched the DSM-IV criteria for ADHD (Anonymous, 2008). Findings show that symptoms of ADHD are different between children, adolescents and adults. Inattention will be more evident while hyperactivity tends to decrease with age (Galéra et al., 2012).
Among the treatment approaches for improving attention in people with ADHD, pharmacotherapy, such as stimulant medication, is the mainstay choice as it is associated with a remarkable response rate, though many patients still suffer from the impairing residual symptoms despite treatment (Modesto-Lowe, Farahmand, Chaplin, & Sarro, 2015). Also, there are patients who wish to reduce the use of medications and look for alternative approaches (Mitchell, Zylowska, & Kollins, 2015).
Nonpharmacological treatment options are therefore increasingly preferred. However, there has been insufficient research on the effectiveness of nonpharmacological treatment options which treat inattention in adults with ADHD (Mitchell et al., 2015). For children and adolescents with ADHD, although nonpharmacological treatment options such as cognitive behavioral treatments and behavioral parent management training are available, they lack empirical support for their application (Van der Oord, Bögels, & Peijnenburg, 2012). Therefore, the need in developing nonpharmacological approaches to augment ADHD treatments has aroused interest in mindfulness-based intervention (MBI) (Modesto-Lowe et al., 2015).
Mindfulness-based intervention has been widely used and shown benefits in adults who suffer from stress, depression, pain and illness (Hofmann, Sawyer, Witt, & Oh, 2010). The concept of MBI is based on Buddhist tradition and Western knowledge of psychology (Van de Weijer-Bergsma, Formsma, de Bruin, & Bögels, 2012). MBI is to adopt a nonjudgmental attention towards one's experience(s) in the present moment (Kabat-Zinn, 1990). Bishop and colleagues (2004) proposed that there are two major components in MBI: (1) Self-regulation of attention — it refers to the observing and attending to the moment-to-moment changes of thoughts, feelings, and sensations. Sustained attention would be required to maintain the focus of attention and the awareness of present moment; (2) Orientation to experience — it is to maintain a curiosity about where the mind wanders, and being experientially open to the reality of the present moment. Based on these concepts, MBI can be viewed as a self-regulatory practice of our attention. This practice involves lowering arousal and controlling attention to the present moment with an open and nonjudgmental mind. Therefore, it appears that MBI can provide benefit for individuals with attention problems such as ADHD.
Recently, MBI becomes increasingly accepted as an intervention approach to individuals with ADHD, especially concerning the symptoms of inattention. There are some potential reasons. The first reason is MBI involves focused attention on a selected object (e.g. Breath sensation), and subsequently broadens the attention towards a steady monitoring of anything that arises from sensory, mental or emotional states (Smalley et al., 2009). Through this practice, people learn to control their attention to focus on the present experience rather than other objects and gradually a kind of attention called conflict attention is developed (Tang et al., 2007). As individuals with ADHD are found to have a lower level of conflict attention (Smalley et al., 2009), the application of MBI to individuals with ADHD is supported. The second reason is neuroimage studies found neuroplastic changes in the brain areas supporting attention in individuals with ADHD after MBI (Lutz, Slagter, Dunne, & Davidson, 2008). Although MBI emphasizes focusing attention on present experience (i.e., focus attention), the specific neural systems associated with conflict monitoring (e.g. dorsal anterior cingulate cortex), sustained attention (e.g. right frontal and parietal areas) and selective attention (e.g. the temporal-parietal junction and ventro-lateral prefrontal cortex) were found to fire spontaneously during mindfulness practice (Lutz et al., 2008), suggesting the benefit of MBI was evident not only at behavioral but also at neural level. This further substantiates the potential application of MBI to improve attention in individuals with ADHD.
There are various types of MBI used in ADHD. However, one common component among them is the practice of self-regulation of attention. For examples, mindfulness-based cognitive therapy (MBCT) is the combination of cognitive behavioral therapy and mindfulness. It emphasizes sustained attention training and believes that if someone is able to control his/her internal state, it can enable insight and adaptation of maladaptive cognitions and behaviors underlying psychiatric symptoms (Schoenberg et al., 2014). Mindful awareness practices (MAP) involves intentionally bringing one's attention to the present moment and experience, meditation is the main component of MAP (Bueno et al., 2015). Mindfulness-based stress reduction (MBSR) training is a method of using meditation and yoga to increase the awareness of and reduce stress. Through this practice, one learns to observe his/her reactions to life's stressors (Kabat-Zinn, 1990).
ADHD is a neurobiological disorder which is not only found in children but also in adolescents and adults. Clinical findings show that the pattern of ADHD symptoms would change with age, with hyperactivity-impulsivity is more significant than inattention in childhood but inattention would become more evident than hyperactivity-impulsivity in adulthood (Galéra et al., 2012). Although evidence shows that mindfulness-based training is effective for improving attention in adults with ADHD (Mitchell et al., 2013), because of the changes in the severity of inattention along the developmental pathway of ADHD individuals, it is possible that such kind of intervention would have different training benefits on attention for ADHD individuals at different developmental stages. To date, there is only one systematic review focusing on the effectiveness of MBI on adults with ADHD (Mitchell et al., 2015) but the effectiveness of MBI on individuals with ADHD in different age groups, especially in the aspect of attention, has not been examined. In order to better understand the clinical value of mindfulness-based training on improving attention in the ADHD population, this systematic review aimed to examine the effectiveness of mindfulness-based training on improving attention in ADHD individuals at three different developmental stages, i.e. childhood, adolescence, and adulthood.
Methodology
Literature Search
Literature review was done to locate published papers and research studies investigating mindfulness training for children, adolescents and adults with ADHD. The keywords search for the literature was performed from seven electronic databases, including PubMED, ScienceDirect, Medline, PsyclNFO, CINAHL, Frontiers and SAGE. The keywords used were Attention Deficit Hyperactive Disorder, ADHD, mindfulness, meditation and attention. Boolean operators ‘OR’, ‘*”, ‘AND’ were also used to capture potential studies. In addition, hand search of the reference lists of included articles was done by the review team which consisted of five postgraduate students and one faculty member in the field of rehabilitation. The search process was presented in Fig. 1.
Figure 1.
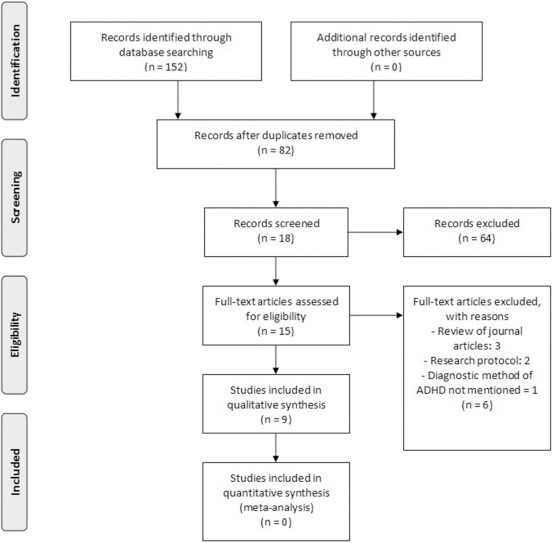
Flowchart of search strategy based on PRISMA flow diagram
Inclusion and Exclusion Criteria
Studies were included when they met the following criteria:
-
•
Participants: individuals with ADHD diagnosed by DSM-IV (APA, 1994).
-
•
Intervention: Mindfulness-based training, such as Mindfulness Based Cognitive Training (MBCT), Mindful Awareness Practices (MAP), Mindfulness-Based Stress Reduction (MBSR), etc.
-
•
Outcome measures: outcomes in attention performance/inattention symptom
-
•
Study design: rated as level 3, single case control or studies, or higher levels such as randomized control trials, according to the Centre for Evidence Based Medicine (CEBM, 2009) hierarchy or studies.
-
•
Studies were published in recent 10 years between 2007 and 2016.
-
•
Studies were excluded if full text was not available or they were not published in English.
Data Extraction
The review team screened and selected the included literature based on the title, publication year, methodology, types of participants, outcome measures and the intervention of the studies together. Disagreement on the decision between team members was resolved through discussion. In addition, the reasons for excluding studies were recorded. After selecting the relevant literature, two group members were responsible for classifying the studies into three categories based on the age of the participants (i.e., children, adolescents, and adults) – a person older than 19 is classified as an adult; a person aged from 10 to 19 is classified as an adolescent; a person is classified as a child if under 10 (World Health Organization, 2013).
Results
Study Identification
The initial search identified 152 articles for review. Based on the inclusion and exclusion criteria, nine studies examining mindfulness-based interventions with the outcome measures including attention performance/inattention symptom were included. This process is specified in Fig. 1.
Summary of Study Details
Out of the nine included studies, five articles involved adults as the participants, one article involved both adults and adolescents as the participants, two articles involved adolescents as the participants and one article involved children as the participants. Table 1 summarizes study details including (a) study design; (b) research objectives; (c) number of participants; (d) age of participants; (e) gender; (f) outcome measures; (g) intervention and; (h) intervention outcomes.
Table 1.
Summary of the study details.
| Studies | Research design | Research objectives | Number of participants | Age (years) (range, mean) | Gender (number (male, female) | ) Outcome measures | Intervention | Intervention outcomes |
|---|---|---|---|---|---|---|---|---|
| Zylowska et al. (2008) | Quasi-experimental design: one group pre-post test | To test the practicability of an 8-week mind-fullness training program for adults and adolescents with ADHD | 32 (24 adults and 8 adolescents) | Adult:/, 48.5 Adolescent:/, 15.6 | 12, 20 | ADHD Rating Scale IV (for adults); SNAP-IV scale (for adolescents); Attention Network Test (ANT) | MAPs for ADHD: 8 weekly 2.5-h sessions of mindfulness training and daily at-home practice | Significant improvements in self-reported attention and measures of attentional conflict were found |
| Mitchell et al. (2013) | RCTs | To evaluate the preliminary value of a group-based mindfulness meditation training for ADHD adults | 20 | Control:/, 36.22 Intervention:/, 40.55 | 8, 12 | self-report and un-blinded clinician rating versions of the Current ADHD Symptoms Scale; ecological momentary assessment (EMA) completed via electronic diary | MAPs for ADHD: 8 weekly 2.5-h sessions of mindfulness training and daily at-home practice | Significant reduction of inattention symptom was found |
| Edel et al. (2017) | Quasi-experimental design: two group pre test post test design | To compare mindfulness-based training program and skills group training in reducing ADHD symptoms and improving mindfulness and self-efficacy | 91 | Mindfulness-based training group (MBTG):/33.8 Dialectical behavioral therapy (DBT)- oriented skills training group (STG):/, 36.7 | 55, 36 | WRI; four self-designed Likert-type scales | -DBT-oriented skills training: 13 weekly 2-h sessions - Mindfulness-based Training: 13 weekly 2-h sessions | Similar reduction of inattention symptom in both groups with the effect sizes were in the small-to-medium range; 30.8% of the MBTG participants and 11.5% of the STG participants had a decrease in inattention symptoms ≥ 30% |
| Schoenberg et al. (2014) | RCTs | To examine whether MBCT would enhance the ERP amplitudes indexing the performance biomarkers of adults with ADHD | 50 | Wait-list Control: 22–50, 33.9 Intervention: 19–53, 39.5a | 21, 23a | Conners' Adult ADHD Self-rating Scale (CAARS-S: SV) | MBCT adapted for individuals with ADHD: 12 weekly 3-h sessions of MBCT and at-home self-practice | Significant reduction of attention symptom was found |
| Hepark et al. (2015) | RCTs | To examine the effectiveness of mindfulness as a treatment for ADHD adults | 103 | Wait-list Control:/, 36.5 Intervention:/, 35.2 | 47, 56 | Conners' Adult ADHD Rating Scale Investigator Rating Version (CAARS-INV); Conners' Adult ADHD Self-rating Scale (CAARS-S: SV) | MBCT adapted for individuals with ADHD: 12 weekly session and 30-min home practice daily | Significant reduction of self-rated and investigator-rated inattention symptom were found |
| Bueno et al. (2015) | Quasi-experimental design: two group pre test post test design | To examine whether mindful awareness practices (MAP) can improve in QoL, attention and mood, in ADHD adult | 68 | Control:/, 31.7 Intervention:/, 31.2 | 30, 30bb | Adult ADHD Self-Report Scale (ASRS); Attention/ Attentional Network Test (ANT); Conner's Continuous Performance Test (CPT II) | MAP for ADHD: 8 weekly 2.5-h sessions of group program and home practice | Significant improvement in sustained attention (ANT) and detectability (CPT II) were found |
| van der Weijer-Bergsma et al. (2012) | Quasi-experimental design: one group pre-post test | To evaluate the effectiveness of an 8-week mindfulness training for 11–15 years old ADHD adolescents and parallel mindful parenting training for their parents | 10 adolescents (19 parents) | 11–15, 13.4 | 5, 5 | Youth Self Report (YSR), Child Behavior Checklist (CBCL), Teacher Report Form (TRF), Mindful Attention and Awareness Scale (MAAS), Amsterdam Neuropsychological Tasks (ANT) | (Adopted from van der Oord et al.): 8 weekly 1.5-h group sessions and home practice; parallel 8 weekly MP training for their parents | Self-report as well as father- and teacher-report showed improvement in adolescent's attention; improvement in adolescent's actual performance on attention tests were also found |
| Haydicky et al. (2015) | Quasi-experimental design: one group pre-post test | To evaluate the effectiveness of an adaptation of a MBCT intervention for 13-18 years old with ADHD and their parents | 18 adolescents (17 parents) | 13–18, 15.5 | 13, 5 | Parent and Adolescent self-report of Conners—3rd Edition | MYmind (adopted from MBCT): 8 weekly 1.5-h group sessions and home practice; parallel 8 weekly training for their parents | Parent-report showed reduction in the adolescents' attention problems; however, adolescents did not report any improvements in attention after training |
| van der Oord et al. (2012) | Quasi-experimental design: waitlist control group | To evaluate the effectiveness of an 8-week mindfulness training for 8–12 years old ADHD children and parallel mindful parenting training for parents | 22 children (22 parents) | 8–12, 9.7 | 16, 6 | The parent and teacher version of the Disruptive Behavior Disorder Rating Scale (DBDRS) | Adopted from MBCT and MBSR: 8 weekly 90-min group sessions and homework; parallel parent training | Parent-rating showed significant reduction in children's inattention from pre-to post test and from pre- to follow-up test; teacher-rating showed reduction in children's inattention from pre-to post test only |
Six data were lost.
Eight data were lost.
Participants
All together 400 participants were involved in these nine included studies. Among them, 342 were adults, 36 were adolescents and 22 were children. Besides, about half of the adults, 58% of the adolescents and 73% of the children were male. For the details of the demographics of the participants refer to Table 1 .
Qualitative Summary of the Studies
Due to the small number of identified studies in this review as well as these studies were substantially heterogeneous in terms of study design, a quantitative data synthesis was not possible. Therefore, a narrative, qualitative summary based on the three age groups was done.
Adults
There were six studies using MBI to improve inattention symptoms in adults with ADHD. While three of them were Randomized Control Trials (RCTs), the rest were two-group pre-posttest design without randomization. Three variants of mindfulness-based training, MBCT, MAP and MBSR, were used in these studies. The results of the two RCT studies which used MBCT as an intervention showed significant reduction in attention problems (Hepark et al., 2015; Schoenberg et al., 2014). Besides, significant reduction of inattention symptom was found after MAP in three studies, in which two were in quasi experimental design (Bueno et al., 2015; Zylowska et al., 2008) and another was RCT (Mitchell et al., 2013). The last study compared the training effects of two mindfulness-based programmes, mindfulness-based training (MBTG) and dialectical behavior therapy-oriented skill training (STG), on the inattention symptoms of ADHD adults (Edel, Hölter, Wassink, & Juckel, 2014). Findings yielded similar reduction of inattention symptoms in both groups, with the effect sizes were in the small-to-medium range. Additionally, 30.8% of the MBTG participants and 11.5% of the STG participants had a decrease in inattention symptoms ≥30%. Generally, the findings of these six studies provided support for the benefits of mindfulness-based training for improving attention in adults with ADHD.
Adolescents
In totally, three articles were found which included adolescents as participants and one of them included both adults and adolescents as participants (Zylowska et al, 2008). All three studies were quasi-experimental and utilized one group pre- and post-test design. The training interventions were adopted from MAP, MBCT and MBSR respectively.
The findings of these three studies revealed that although there were no differences in their attention between pre- and post-training in adolescents in Haydicky, Shecter, Wiener, & Ducharme (2015) study, significant improvements in their attention after either MAP or MBCT were reported by both parents and teachers in all three studies (Haydicky et al., 2015; van der Oord et al., 2012; Zylowska et al., 2008). On the whole, these three studies supported that mindfulness-based training is of clinical value for adolescents with ADHD.
Children
Only one article targeting children with ADHD was included in this review. In Van der Oord et al.'s study (2012), a quasi-random design with a wait-list control group was used. The study involved a group training for children and a parallel training for their parents. This mindfulness training was adopted from MBCT and MBSR. The results showed significant reduction in children's inattention from pre- to post-test and from pre-test to follow-up as reported by parents. For teacher-report, reduction in children's inattention was found only from pre-to post-test.
Discussion
An appropriate behavioral intervention approach is important for improving the attention deficits in individuals with ADHD. As mindfulness-based training has become widely used recently, there is a need to examine whether this type of training is effective in improving attention deficits for individuals with ADHD, in particular whether this kind of intervention would have similar training benefits for ADHD individuals at different developmental stage.
This systematic review examined clinical evidence on the effectiveness of mindfulness-based interventions on improving attention in children, adolescents, and adults with ADHD. Nine studies, including three RCTs, four one-group quasi-experimental designs, one two-group quasi-experimental design and one one-group wait-list control quasi-experimental design, were included in this review.
There were six studies concerning adults with ADHD. The results all showed significant improvement in attention in this age group. Moreover, three of the studies were randomized control trials, posing a strong evidence that the positive results were due to treatment effect. This result echoes with the previous systematic review by Mitchell et al. (2015) that mindfulness-based intervention is an effective treatment approach for ADHD in adulthood to improve attention deficits. For adolescents with ADHD, three studies concerning the effectiveness of mindfulness-based intervention were included in this review. Again the findings of these three studies provided preliminary evidence that MBI has benefits for adolescents with ADHD. Finally, there was only one study concerning the effectiveness of mindfulness-based intervention on children with ADHD was included in this review. The results showed a significant improvement in attention in the children based on the parent-rated and teacher-rated Disruptive Behavior Disorder Rating Scale (DBDRS).
This systematic review supported that MBI has clinical value for individuals with ADHD regardless of their developmental stages, however, some considerations should be taken before a conclusion can be drawn. Mitchell and colleagues (2015) mentioned in their systematic review that there are still some concerns about the studies on MBI for individuals with ADHD, they are the sample size and composition, randomization, long-term follow-up assessments, blinded clinician assessments, active treatment comparison groups, training of instructors, and adherence to manualized treatment materials. These concerns are valid and important, however, based on this current systematic review, at least three more issues that we need to know before we can draw a clear conclusion on the effectiveness of MBI in ADHD population. First, when considering the content of the MBI programmes used in the studies in this systematic review, some studies involves the basic mindfulness training plus home practice (Mitchell et al., 2013) while one study used the basic mindfulness training only (Edel et al., 2017). Since both types of training contents showed significant reduction in inattention symptoms, it is unsure whether home practice is a necessary component in MBI. In light of it, future studies should consider the use of a well-defined treatment protocol so that it is easier to tease out the effect of each component to the treatment outcomes. In addition, if the treatment components are clearly specified, other studies can adopt the same protocol so that between-studies comparisons can be done. Second, when considering the intensity of the various mindfulness-based trainings, different number of training sessions and training duration for each session are involved in different training programmes. For example, MAP usually involves 8 weekly 2.5-h sessions while MBCT consists of 12 weekly 3-h sessions plus at-home self-practice. Under this condition, although both programmes showed benefits for individuals with ADHD, it is unclear whether or not MAP is more effective training than MBCT for improving attention as it involves less total hours of training compared to MBCT. Along the same line, it is unable to know whether there is an optimal training dosage for improving attention when conducting MBI in ADHD individuals. In view of it, more studies that focus on comparing the training effects between different MBI programmes and studies on the effects of different training intensities are warranted. Third, when taking the outcome measures used in the studies in this systematic review into account, majority of the studies used rating scales to report the pre- and post-training changes. Although this is a common rating approach, the reported ratings may be biased as parents and teachers were not blinded to the training condition of the participants. If the actual performance of participants on attentional tasks can be considered as an outcome measure in future studies, it can provide objective information about whether MBI has benefits or not and give additional information about whether MBI leads to a specific pattern of improvements in attention in individuals with ADHD.
Apart from the above-mentioned three issues, there are some other areas that future studies should consider. ADHD has various subtypes and the severity of different ADHD symptoms would be different among these subtypes. Although it appears that MBI has benefits for ADHD individuals, it is unclear whether any ADHD subtypes would benefit more from MBI. In order to know the answer for this issue, future studies should consider investigating the training effect of MBI on the various ADHD subtypes. MBI was originally used in adult populations, it is a relatively new treatment approach for children. Because of this background, majority of the identified studies in this systematic review focused on adults and only one study is on children. Under this condition, it is premature to make any conclusions on the clinical application of MBI in children with ADHD. There is no doubt that more studies are needed to test the effectiveness of MBI on improving attention in children with ADHD. However, more specifically, as MBI involves high cognitive demands, studies on investigating whether MBI is a “child-friendly” treatment approach is also indicated. Wall (2005) mentioned that children needed more assistance for internalizing the concepts of mindfulness than adults. In other words, the effectiveness of MBI in children could be affected by an external help offered to them during the training. Future studies should consider modifying the adult version of MBI and providing parent/ teacher guidance and environmental set up for children during training and practice.
Finally, it is noteworthy that there were some limitations in this review. First, one of the participant selection criteria was participants in the reviewed studies should fulfil the DSM-IV diagnostic criteria of ADHD. This criterion excluded those individuals who had the diagnosis based on other DSM editions (e.g., DSM III or DSM lll-R), leading to a smaller number of studies that could be identified during the literature search process, in particular those studies on adults. Although a negative consequence on the total number of identified studies was induced, if the same diagnostic criteria were used for different age groups, a relatively more consistent clinical characteristics profile of participants can be warranted and helped controlling the confounding effect of mixed participants' characteristics. Second, only articles published in English were included in this review, this criterion might restrict the number of relevant studies identified, lowering the power of generalization of the study results. Third, one of the selection criteria set for the literature search was “outcomes in attention performance/inattention symptoms”. As many studies used ADHD symptoms, depressive and anxiety symptoms, and/or mindfulness skills as the outcome measures, outcomes in attention performance/inattention symptoms may be too focused and restrict the quantity of studies that can be identified. However, inattention is a major symptom in ADHD individuals and the essence of MBI is to practice self-regulation of attention, improvements in attention should be more direct and explicit than other outcome measures. Moreover, it may also provide further information about the associations between the underlying mechanisms of intervention and the treatment outcomes. Therefore, attention is preferred as the primary outcome measure in this systematic review.
Conclusions
This systematic review examined the evidence for effectiveness of mindfulness-based interventions in children, adolescents and adults with ADHD. For adults with ADHD, mindfulness-based intervention improves attention deficits significantly, however, due to limited research studies, it is hard to make conclusion for adolescents and children with ADHD. Moreover, for the small quantity of references papers, it is hard to conclude that whether mindfulness-based interventions are more effective in a particular age group.
It is recommended that future studies should consider using attention as the primary outcome and other variables as the secondary outcomes and consider the quality of home-based mindfulness practice for the children and adolescents.
References
- American Psychiatric Association (APA). (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Arlinton, VA: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlinton, VA: American Psychiatric Association. [Google Scholar]
- Anonymous (Ed.). (2008). Shire to present additional scientific data on ADHD treatment Portfolio at American Psychiatric Association Annual Meeting. New York. [Google Scholar]
- Bishop S. R., Lau M., Shapiro S., Carlson L., Anderson N. D., Carmody J. et al. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241. [Google Scholar]
- Bueno V. F., Kozasa E. H., da Silva M. A., Alves T. M., Louzã M. R., & Pompéia S. (2015). Mindfulness meditation improves mood, quality of life, and attention in adults with attention deficit hyperactivity disorder. BioMed Research International, 2015, 962857 10.1155/2015/962857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre for Evidence Based Medicine (CEBM). (2009). Oxford centre for evidence-based medicine: Levels of evidence. Retrieved from: http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/.
- Edel M. A., Hölter T., Wassink K., & Juckel G. (2017). A comparison of mindfulness-based group training and skills group training in adults with ADHD: An open study. Journal of attention disorders, 21(6), 533–539. [DOI] [PubMed] [Google Scholar]
- Galéra C., Bouvard M.-P., Lagarde E., Michel G., Touchette E., Fombonne E. et al. (2012). Childhood attention problems and socioeconomic status in adulthood: 18-year follow-up. The British Journal of Psychiatry, 201(1), 20–25. 10.1192/bjp.bp.111.102491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haydicky J., Shecter C., Wiener J., & Ducharme J. M. (2015). Evaluation of MBCT for adolescents with ADHD and their parents: impact on individual and family functioning. Journal of Child and Family Studies, 24(1), 76–94. [Google Scholar]
- Hepark S., Janssen L., de Vries A., Schoenberg P. L., Donders R., Kan C. C. et al. (2015). The efficacy of adapted MBCT on core symptoms and executive functioning in adults with ADHD: A preliminary randomized controlled trial. Journal of Attention Disorders, 1087054715613587. [DOI] [PubMed] [Google Scholar]
- Hofmann S. G., Sawyer A.T., Witt A. A., & Oh D. (2010). The effect of mindfulness- based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Deltacorte Press. [Google Scholar]
- Lutz A., Slagter H. A., Dunne J. D., & Davidson R. J. (2008). Attention regulation and monitoring in meditation. Trends in Cognitive Sciences, 12(4), 163–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell J. T., McIntyre E. M., English J. S., Dennis M. F., Beckham J. C., & Kollins S. H. (2013). A pilot trial of mindfulness meditation training for attention-deficit/hyperactivity disorder in adulthood: Impact on core symptoms, executive functioning, and emotion dysregulation. Journal of Attention Disorders. 10.1177/1087054713513328. Advance online publication. [DOI] [PMC free article] [PubMed]
- Mitchell J. T., Zylowska L., & Kollins S. H. (2015). Mindfulness meditation training for attention-deficit/hyperactivity disorder in adulthood: Current empirical support, treatment overview, and future directions. Cognitive and Behavioral Practice, 22(2), 172–191. 10.1016/j.cbpra.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modesto-Lowe V., Farahmand P., Chaplin M., & Sarro L. (2015). Does mindfulness meditation improve attention in attention deficit hyperactivity disorder? World Journal of Psychiatry, 5(4), 397–403. 10.5498/wjp.v5.i4.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenberg P. L., Hepark S., Kan C. C., Barendregt H. P., Buitelaar J. K., & Speckens A. E. (2014). Effects of mindfulness-based cognitive therapy on neurophysiological correlates of performance monitoring in adult attention-deficit/hyperactivity disorder. Clinical Neurophysiology, 125(7), 1407–1416. [DOI] [PubMed] [Google Scholar]
- Smalley S. L., Loo S. K., Hale T. S., Shrestha A., McGough J., Flook L. et al. (2009). Mindfulness and attention deficit/-hyperactivity disorder. Journal of Clinical Psychology, 65(10), 1087–1098. 10.1002/jclp.20618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y. Y., Ma Y., Wang J., Fan Y., Feng S., Lu Q. et al. (2007). Short-term meditation training improves attention and self-regulation. Proceedings of the National Academy of Sciences, 104(43), 17152–17156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Weijer-Bergsma E., Formsma A. R., de Bruin E. I., & Bögels S. M. (2012). The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. Journal of Child and Family Studies, 21(5), 775–787. 10.1007/s10826-011-9531-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Oord S., Bögels S. M., & Peijnenburg D. (2012). The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. Journal of Child and Family Studies, 21(1), 139–147. 10.1007/s10826-011-9457-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall R. B. (2005). Tai chi and mindfulness-based stress reduction in a Boston public middle school. Journal of Pediatric Health Care, 19(4), 230–237. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2013). Definition of key terms. Retrieved from: http://www.who.int/hiv/pub/guidelines/arv2013/intro/keyterms/en/.
- Zylowska L., Ackerman D. L., Yang M. H., Futrell J. L., Horton N. L., Hale T. S. et al. (2008). Mindfulness meditation training in adults and adolescents with ADHD a feasibility study. Journal of Attention Disorders, 11(6), 737–746. [DOI] [PubMed] [Google Scholar]


