Abstract
Objective/Background
Most parents of children with autism spectrum disorder (ASD) have difficulties with the selective eating behaviour of their children. This study aimed to develop a newly designed intervention programme on improving selective eating behaviour for parents of children with ASD and evaluate its effectiveness.
Methods
The participants were 23 parents of children (aged 3–6 years) with ASD. The education programme included a session that addressed approaches to improve selective eating and attitudes at meal times, with a discussion. The intervention aimed to identify the underlying factors and approaches to improve selective eating in children and the self-efficacy of parents.
Results
Significant differences were observed before and after the intervention in the degree of difficulty perceived by parents, their degree of self-efficacy, the number of recommendations conducted by them, their subjective view of the degree of dietary imbalance, and the number of food items consumed by their children.
Conclusion
We developed an interventional programme for parents of children with ASD and this programme was found to be useful. It is important for occupational therapists to consider the factors and approaches for selective eating in children with ASD in order to provide early intervention for their parents.
Keywords: Autism spectrum disorder, Selective eating, Programme
Introduction
The Centers for Disease Control and Prevention (CDC) estimated that one in 68 children among multiple communities in the United States has autism spectrum disorder (ASD). This new estimate is approximately 30% higher than previous estimates of 2012 (Wingate et al., 2014). In Japan, it is estimated that prevalence rate of autism in children up to 5 years of age was 3.5% (Kamio, Kawamata, Nakai, & Mishima, 2015). According to DSM-5, ASD is a lifelong neurodevelopmental disorder characterised by impaired social communication combined with restrictive and repetitive patterns of behaviour and interest. Impairments in sensory processing are also very common (American Psychiatric Association, 2013).
Parents of children with ASD report that they have difficulties with the daily activities, behaviours, and communication abilities of their children. The other concerns that parents often express involve the eating habits of their children during meals (Bicer & Alsaffar, 2013; Williams, Dalrymple, & Neal, 2000), and this can create stress in the household (Anderson, Must, Curtin, & Bandini, 2012; Rogers, Magill-Evans, & Rempel, 2012). Moreover, children with ASD are often highly selective eaters with very limited food acceptance (Cermak, Curtin, & Bandini, 2010).
In fact, an estimated 58%–67% of parents of children with ASD experience the selective eating behaviours of their children in countries such as Japan (Bicer & Alsaffar, 2013; Kerwin, Eicher, & Gelsinger, 2005; Tateyama, Miyajima, & Shimizu, 2013; Williams et al., 2000). Several studies have compared dietary variety among children with ASD, those with normal cognitive development, and those with other developmental disabilities, and these studies concluded that the dietary variety is lower in children with ASD and that these children are more likely to refuse food (Bandini et al., 2010; Marshall, Hill, Ziviani, & Dodrill, 2013; Williams, Hendy, & Knecht, 2008; Zimmer et al., 2012). Early childhood is the period when children experience new foods, tastes, and textures. Young children who consistently refuse to eat or to try a variety of foods are frequently described as ‘picky eaters’ by their parents (Legge, 2002; Tomchek & Dunn, 2007; Twachtman-Reilly, Amaral, & Zebrowski, 2008). Although selective eating is not uncommon in young children with normal development, selective eating in children with ASD may extend beyond the early childhood period. Selective eating patterns are five times more likely in children with ASD than in children with typical neurological development (Sharp et al., 2013). Selective eating tends to be more pronounced, start earlier, and extend over a longer period in children with ASD than in other children. In our pre-study investigation, more than 80% of the parents of young children with ASD reported that selective eating resulted in parental difficulties (Miyajima, Tateyama, Hirao, Nakaoka, & Higaki, 2014).
Food selectivity can become a significant problem because it can be associated with inadequate nutrition owing to the limited nutritional intake of a restricted diet (Cornish, 1998; Dovey, Staples, Gibson, & Halford, 2008; Herndon, DiGuiseppi, Johnson, Leiferman, & Reynolds, 2009; Lockner, Crowe, & Skipper, 2008; Raiten & Massaro, 1986; Schmitt, Heiss, & Campbell, 2008; Williams et al., 2000). Several studies have reported that children with ASD may be at greater risk for nutritional deficits as a result of limited dietary variety; however, these findings are not conclusive (Emond, Emmett, Steer, & Golding, 2010; Hyman et al., 2012; Zimmer et al., 2012). Food selectivity is a frequent problem in children with ASD, and the child's unusual eating patterns can significantly stress the family (Groden et al., 2001; Legee, 2002). If children have selective eating patterns, their parents often do not know how to deal with the situation, and this easily results in stress. Most parents of children who have poor eating habits tend to have lower self-efficacy because of stress and the daily loss of confidence. Therefore, it is important to understand the self-efficacy of parents, as this might help improve a child's food acceptance (Miyajima, Tateyama, Hirao, Nakaoka, & Higaki, 2016).
In response to this problem, researchers have recognised the need for assessment and treatment of selective eating (Johnson et al., 2014; Kral, Erikson, Souders, & Pinto-Martin, 2013; Sharp et al., 2013). Cermak et al. (2010) discussed the need for parents to understand food selectivity and the importance to address the needs of children with ASD who demonstrate substantial food selectivity, because feeding problems are complex and often multi-faceted. To solve the problem of selective eating in children with ASD, it is important to gain a deeper understanding of the various factors that contribute to food selectivity and address them in order to develop holistic interventions for this problem (Tanner et al., 2015).
A number of explanations for food selectivity have been proposed (Whiteley, Rodgers, & Shattock, 2000). Among these, Williams et al. (2000) stated that the most likely factors to influence food selectivity reported by parents were food texture (69%), appearance (58%), taste (45%), smell (36%), and temperature (22%). In the literature, feeding problems have been associated with various factors, including repetitive behaviour, anxiety, and sensory reactivity (Johnson et al., 2014).
Therefore, in our pilot study involving an interview and questionnaire survey, we investigated not only the factors of food preferences but also the approaches for selective eating in children with ASD. We focused more on why these children preferred rather than on why they disliked certain food. We wanted to use the term “food preferences” rather than “food selectivity” because when we evaluated selective eating, we used the factors of preferences (i.e. temperature or size). In addition, we clarified the association between the factors and approaches; approaches corresponding to the factors (Miyajima et al., 2014). The factors of food preferences reported by parents included 57 items, which were divided into the following three categories: sensory functions (taste, texture, appearance, sound, smell, and temperature; 80%), oral functions (chewing and swallowing; 11%), and cognitive functions (habituation, forecast, and obsession; 9%). The approaches for selective eating reported by parents included 50 items, which are divided into the following four categories: oral, sensory, cognitive, and environmental functions. These represented ‘make chewing and swallowing easier’, ‘change the sensory stimulation they hate’, ‘try new kinds of foods’, and ‘support them in a consistent way’ (Tateyama et al., 2013).
The complicated presentation of children can lead to difficulties in determining the most effective interventions to tackle the problem of selective eating (Tanner et al., 2015). To the best of our knowledge, no study in the literature has investigated interventions focused on an education programme for the parents of children with ASD, which involve the abovementioned factors and approaches. If an occupational therapist can provide ideas about approaches corresponding to the factors of food preferences to the parents of children with ASD through a course, the parents might be able to obtain information for implementing techniques that prevent selective eating and improve the dietary habits of their children.
The present study aimed to evaluate the effectiveness of the programme that was designed to provide information to the parents of children with ASD about the factors of food preferences and approaches for coping with the problems of selective eating.
Methods
Participants
The study participants were Japanese-speaking parents of young children with ASD aged between 3–6 years old; they were recruited from two outpatient developmental support centres in Osaka prefecture. Developmental support centres are available to preschool children with special needs for providing therapy and teaching parents about the impairments of their children in Japan (Ministry of Health, Labour and Welfare, 2011).
In Japan, children who have some developmental problems are assessed with medical examinations; however, ASD is diagnosed later in Japan than in other countries, because of social and cultural differences. For example, children often undergo a medical examination prior to entering school in the US, but many Japanese children are examined after entering school.
The eligibility criteria were as follows: the parent (1) has attended all the programmes in the study including two sessions and two discussions; (2) has a child diagnosed with ASD or a child who scored of more than 15 points in the Social Communication Questionnaire (SCQ) (Kuroda, Inada, & Uchiyama, 2013, p. 7; Rutter, Bailey, & Lord, 2003); and (3) has experienced difficulties with their children's selective eating behaviours.
The parents of their children who were admitted to a hospital, changed to a new nursery school or kindergarten, or changed corresponding address recently, and parents who had any personal reason to withdraw from the study, were excluded from this study.
The study protocol was approved by the Research Ethics Committee of the Graduate School of Comprehensive Rehabilitation, Osaka Prefecture University prior to data collection (no.: 2013–210). Informed consent was obtained from each parent and the director of each participating centre. All procedures performed in this study involving human participants were in accordance with the ethical standards of the Institutional and/or National Research Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Examination and Measurement Methods
This study was a single-group, self-controlled trial that compared variables at baseline, and before and after the intervention (Katz, Kihara, & Kihara, 2013, pp. 1–13). The baseline and intervention periods were 2 months respectively (Fig. 1). Baseline measurements were used to evaluate the effectiveness of the programme and gather baseline information regarding the participants before the session and discussion.
Figure 1.
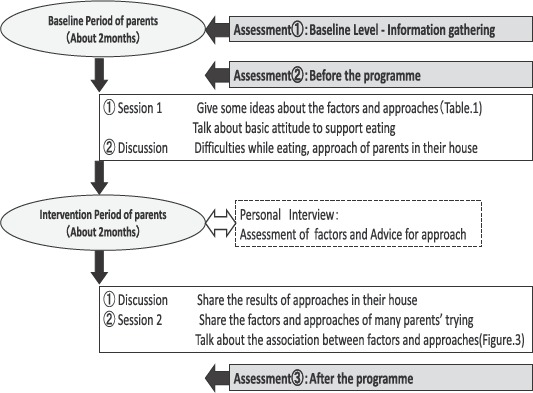
Research design and the interventional program content.
A questionnaire was distributed before and after each session to find out the parental attitudes regarding the selective eating and dietary habits of their children with ASD. At the same time, the developmental age and developmental quotient (DQ) of the children with ASD were determined by using the Kyodaishiki developmental schedule (Koyama, Osada, Tsujii, & Kurita, 2009). The Kyodaishiki developmental schedule is a standardised test used quite often in Japan. DQ has the highest correlation with IQ, and the assessment has been validated (Koyama, Osada, Tobari, & Takeda, 2003; Koyama et al., 2009). The information about parents' knowledge on approaches and the factors of food preference was collected at the baseline measurement. The outcome measures were measured at three time-points: (1) baseline(2 months prior to the intervention), (2) before the intervention, and (3) after the intervention. The outcome measures in this study are described below.
The changes to parental attitudes were assessed using: (1) The degree of difficulty experienced by the parents was assessed using a visual analogue scale (VAS; 0–100 points) (Bijure, Silver, & Gallagher, 2001), (2) The degree of self-efficacy of the parents was evaluated using the Self-efficacy Assessment for Parents of Children with Selective Eating (SAPS) scale, with a scoring system of 12–60 points (12 items), and (3) The number of recommendations implemented by parents (50 items; Table 1).
Table 1.
Assessment of Content: Introduction of a Parental Course—Factor and Approach.
| Factors of Food Preferences (57 items) | |||
| Oral | Chew | 1) small size | 5) hard |
| Swallow | 3) easy to swallow | 6) difficult to swallow | |
| Sensory | Taste, Flavour | 8) sweet | 14) flavours mixed in the mouth |
| Smell | 15) strong smell | 16) scentless | |
| Texture | 20) flaky | 31) gummy | |
| Temperature | 32) hot | 34) lukewarm | |
| Sound | 36) crunchy | 39) fibrous | |
| Appearance | 42) colourful | 46) monotoned | |
| Cognition | Prediction | 52) predictable, unsurprising | 56) unpredictable |
| Familiar | 53) everyday food | 55) same bland | |
| Obsessed | 54) obsessed, particular | 57) hate everything except favourite food | |
| Approach for Selective Eating (50 items) | |||
| Oral | Make it easier to chew and swallow | 3) make food bite size, consistent firmness | |
| Sensory | Change the dislike sensory elements | 5) grind and mix, add soup, or sliminate fibre | |
| Not to mix sensory elements | 9) stop each bite and avoid mixing the flavour and texture | ||
| Use the flavoured sensory elements | 11) change to favoured flavours and tastes | ||
| Cognition | Introduce new ingredient | 20) serve anyway even they cannot eat | |
| Decide the size and amount as might be expected | 22) show small amount on a spoon | ||
| Experience together as might be expected | 26) cook the food together and show the process | ||
| Decide the roles as might be expected | 28) clarify each step and process | ||
| Let not notice ingredients of the meal | 34) mix with favourite food without noticing | ||
| Environment | Help eating in the consistent way | 38) always helped by the same person | |
| Do not force to eat and recognize their efforts | 39) praise and recognize their efforts | ||
| Create a pleasant atmosphere | 41) show and share a pleasant atmosphere for themselves | ||
| Take advantage of the obsession and make the same environment | 44) prepare the same bland (B flavour of A company) | ||
| Experience different places and environments | 49) eat at different places for many times | ||
The SAPS scale consists of 12 items and is divided into three areas: (1) basic attitudes to eating, (2) factors underlying likes and dislikes, and (3) compliance to recommendations for selective eating (Miyajima et al., 2016; Tateyama & Miyajima, 2015). Each item was measured according to how confident the parents are to pursue the necessary actions for improving the child's food acceptance. A Likert scale (Likert, 1932) was used for the responses to questions, with higher scores representing higher self-efficacy.
The changes in the eating patterns of children with ASD were assessed using: (1) The number of foods that the child chose to eat (47 items), and (2) The parents' subjective view of the degree of dietary imbalance (VAS; 0–100 points).
The 47 items of food included carbohydrate-rich foods, liquids, fish, meat, vegetables, beans, eggs, seaweed, mushrooms, and potatoes, etc. We also assessed the factors for the favourite foods through a 57-item questionnaire (Miyajima et al., 2014), and the approaches for selective eating were assessed through a 50-item questionnaire (Miyajima et al., 2014; Tateyama & Miyajima, 2015) which had been used in a pilot study before (Table 1).
Content of Intervention
The developmental support centres in Japan conduct seminars regularly to parents of children with ASD, and the intervention was part of this regular service (Fig. 2).
Figure 2.
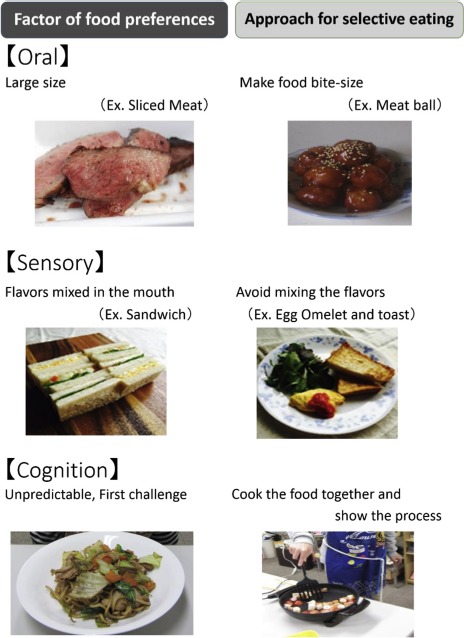
Introduction of a parental program — factor and approach (part of the presentation).
This programme intended to help parents to take care of their children and provide opportunities for them to learn how to cope with selective eating. This programme also intended to change the environment between parents and children by making an intervention for the parents based on the Person Environment Occupation model. In occupational therapy for children with developmental disorders, child care support for parents is very important (Karashima, 2008, pp. 39–43).
The programme consisted of two 40-min sessions and two discussions for the parents of children with ASD. The session was about the factors underlying selective eating and approaches to improve selective eating and attitudes at meal times. The aims of the programme were: (1) to learn the basic attitudes towards eating; (2) to elucidate factors influencing food preferences; and (3) to implement new approaches to tackle selective eating. Personal interviews were conducted upon request. The sessions included presentations on the results of previous investigations (Miyajima et al., 2014).
In session 1, parents were introduced to 57-factor items and 50 -approach items identified by analysing qualitatively the interviews after checking the assessment results (Table 1). This helped in providing a different point of view to parents and enhanced their awareness of the issues associated with ASD. For example, if the oral factor for disliking sliced meat was because it was hard to chew, we suggested to make the food bite size, such as a meat ball, as the approach. If the sensory factor for disliking a sandwich was because of having mixed flavours in the mouth, we suggested to avoid mixing the flavours, such as giving egg omelette and toast separately, as the approach. If the cognition factor for disliking the food for the first time was unpredictable, we suggested to cook the food together and show the process as the approach.
Next, basic attitudes towards eating were discussed and a report from a person with ASD was presented. The parents were then divided into small groups to discuss personal experiences and identify factors underlying the culinary likes and dislikes of their children. Later, various approaches to address the identified factors were discussed and the participants were encouraged to implement these new approaches at home.
Before session 2, we conducted another discussion with the same small group to allow parents to share the results of incorporating the approaches identified in the session 1. Small, detailed steps were recommended to maintain implementation of the approaches that were successful. The parents also examined about why some of their approaches were unsuccessful, and they were encouraged to try different methods or to implement the changes in smaller steps.
Later, the factors and recommendations from a previous study (Miyajima et al., 2014) were introduced to the parents in the session 2 so that they could obtain maximum benefit from the interventional programme. In addition, a lecture on the association between factors and approaches was given (Fig. 3).
Figure 3.
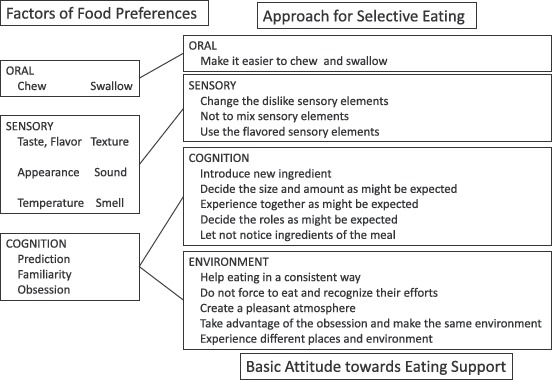
Association of food preferences and the food selectivity approach used in the program.
An additional session or a personal interview, as requested by parents, was conducted between the session 1 and session 2 within 2 months. Each interview lasted for about 40 minutes, and an occupational therapist answered questions about dietary status. The parents reassessed the information regarding food preference factors of their children after the interview.
Analysis
All data analyses were performed using SPSS statistical software (version 22; IBM Corp., Armonk, NY, USA). Baseline factors were recorded 2 months before the intervention and re-evaluated 2 months after the intervention. Data were collected for parents of children with ASD who had difficulties with selective eating and parents who participated in all the sessions.
Normality was assessed using the Shapiro—Wilk test. The differences between the periods were analysed by either: (a) a one-way analysis of variance or (b) the Friedman test, depending on the nature of the data ( Table 3 ). The Bonferroni test was used where multiple comparisons were indicated. A p-value of <0.05 was considered statistically significant.
Table 3.
Self-reported Compliance with Recommendations Before and After the Intervention.
| Measurement items | Means | Range | Unit | Assessment ① baseline level | Assessment ② before | Assessment ③ after | p | ||
|---|---|---|---|---|---|---|---|---|---|
| Difficulty | degree of difficulty | VAS | 0–100 | points | 54.13 ± 25.05 | 54.65 ± 25.01 | 37.22 ± 24.54 | 0.000b | *** |
| Self-efficacy | total | SAPS: total | 12–60 | points | 39.3 ± 6.92 | 39.3 ± 6.92 | 44.65 ± 6.64 | 0.018a | * |
| 1. attitude | NO 1–3 | 3–15 | points | 9.52 ± 2.59 | 9.52 ± 2.59 | 10.35 ± 2.19 | 0.018a | * | |
| 2. factor | NO 4–7 | 4–20 | 14.48 ± 3.10 | 14.48 ± 3.10 | 16.39 ± 2.84 | 0.002a | ** | ||
| 3. approach | NO 8–12 | 5–25 | 15.31 ± 3.74 | 15.31 ± 3.74 | 17.95 ± 3.07 | 0.000b | *** | ||
| Approach | practicing now | 50 items | 0–50 | items | 18.22 ± 6.91 | 18.39 ± 6.89 | 25.39 ± 7.73 | 0.000a | *** |
| tried already | 26 ± 9.52 | 26.17 ± 9.56 | 33.13 ± 7.63 | 0.003a | ** | ||||
| Diet condition | eatable food | 47 items | 0–47 | items | 32.13 ± 11.61 | 32.48 ± 11.68 | 35.04 ± 12.00 | 0.000b | *** |
| - no need attempts | 20.26 ± 10.83 | 20.52 ± 10.79 | 25.17 ± 13.04 | 0.004a | ** | ||||
| - need attempts | 11.87 ± 6.49 | 11.96 ± 6.43 | 10.04 ± 6.89 | 0.164a | ns | ||||
| uneatable food | 14.87 ± 10.83 | 14.52 ± 10.79 | 11.79 ± 13.04 | 0.000b | *** | ||||
| Subjective view | dietary unbalance | VAS | 0–100 | points | 57.78 ± 23.95 | 58.09 ± 24.28 | 44.43 ± 29.46 | 0.000b | *** |
VAS = visual analogue scale; SAPS = Self-efficacy Assessment for Parents of Children with Selective Eating.
Average ± standard deviation (SD).
*p < 0.05, **p < 0.01, ***p < 0.001.
Data were analysed by using SPSS22.0, a: One factor repeated measure ANOVA, b: Friedman test, due to the nature of data by the test of normality assessed with the Shapiro—Wilk test.
Differences in mean values were assessed with Bonferroni multiple comparison procedure.
Results
Participant and Diet Condition Characteristics
Forty-nine participants attended the session 1. Fourteen (28.6%) out of the 49 participants were unable to attend the session 2 due to working, personal business or illness of their children. A total of 35 participants attended all the programmes. Of these 35 participants, 20 of them had children diagnosed with ASD. In addition, on assessment using the SCQ, we identified four children with cut-off scores of more than 15 points, and they were included in the analysis. Of those 24 selected parents, 23 reported difficulties owing to selective eating in their children. Hence, a total of 23 participants (46.9%) were finally included in this study. Table 2 summarises the characteristics of the participating children and parents, and the parents' perception of the dietary balance of their children.
Table 2.
Characteristics of the Participants and Dietary Status (n = 23).
| Characteristics of participants (n = 23) | |||
|---|---|---|---|
| Parents | |||
| Age | 20–29 | 2 | 9% |
| 30–39 | 9 | 39% | |
| 40–49 | 12 | 52% | |
| Gender | male | 0 | 0% |
| female | 23 | 100% | |
| Children | |||
| Age | 3 years old | 9 | 39% |
| 4 years old | 8 | 35% | |
| 5 years old | 4 | 17% | |
| 6 years old | 2 | 9% | |
| average ± SD | 52.83 ± 12.1 months | ||
| Gender | boy | 18 | 78% |
| girl | 5 | 22% | |
| Diagnosis | ASD | 19 | 83% |
| SCQ (more than 15 points) | 4 | 17% | |
| Development agea | 0 year old | 2 | 9% |
| 1 year old | 6 | 26% | |
| 2 years old | 5 | 22% | |
| 3 years old | 2 | 9% | |
| 4 years old | 1 | 4% | |
| unclear/unadministered | 7 | 30% | |
| Development Quotient (DQ)a | 0–19 the most severe | 0 | 0% |
| 20–34 severe | 1 | 4% | |
| 35–49 moderate | 8 | 35% | |
| 50–69 mild | 4 | 17% | |
| 70–border | 2 | 9% | |
| unclear/unadministered | 8 | 35% | |
| Diet condition of participants (n = 23) | |||
| Degree of difficulty | great | 6 | 26% |
| normal | 9 | 39% | |
| few | 8 | 35% | |
| none | 0 | 0% | |
| Dietary unbalance (subjective view) | very unbalanced | 7 | 31% |
| unbalanced | 9 | 38% | |
| few unbalanced | 7 | 31% | |
| none | 0 | 0% | |
| Eatable food items before intervention (in 47 items) | 1–10 | 5 | 21% |
| 11–20 | 7 | 31% | |
| 21–30 | 7 | 31% | |
| more than 31 | 4 | 17% | |
Kyodaishiki developmental schedule.
Of the 23 parents included in the analysis, two were aged 20–29 years, nine were aged 30–39 years, and 12 were aged 40–49 years. These 23 parents had 23 preschool-aged children (mean age, 52.83 ± 12.10 months), including nine children aged 3 years, eight aged 4 years, four aged 5 years, and two aged 6 years. The ratio of boys to girls was 18:5, which was similar to the sex ratio of ASD reported by Wingate et al. (2014). Of the 23 children, 19 were diagnosed with ASD (including pervasive developmental disorder or autism) and four were undiagnosed but had SCO scores of >15 points (the ASD cut-off score). All 23 parents reported difficulties at mealtime and suspected that the diets of their children were imbalanced. Table 3 shows these results.
An occupational therapist interviewed 12 of the 23 (52.2%) parents, who requested advice. Of the 12 parents, five had children who consumed less than 10 different food items. The occupational therapist advised the parents on how to best approach their concerns.
Degree of Difficulty Perceived by Parents
The degree of difficulty perceived by parents was measured using a VAS (0–100 points). Statistical analysis revealed that the VAS score significantly decreased by 17.87 points from 54.65 to 37.22 after the intervention (p < .001).
Degree of Self-Efficacy of the Parents
The degree of self-efficacy of the parents was measured using the SAPS (12–60 points), which showed that the total score significantly increased by 5.35 points from 39.3 to 44.65 after the intervention (p = .018).
The following is a breakdown in each domain: 1) Basic attitudes to eating: three items increased from 9.52 to 10.35 points (p = .018); 2) Factors of likes and dislikes: four items increased from 14.48 to 16.39 points (p = .002); and 3) Correspondence to selective eating: five items increased from 15.31 to 17.95 points (p < .001). The average gain scores in these three areas were 0.28, 0.48, and 0.53 points, respectively, with the most significant increase in ‘correspondence to selective eating’ (p = .018).
Number of Recommendations Carried out by Parents
There was a significant increase in the number of recommendations carried out by parents (increase of 7.00 items from 18.39 to 25.39) and the number of approaches attempted by parents (increase of 7.39 items from 26.17 to 33.13) (both, p < .01). The most common approaches among parents of children with ASD were ‘change the hated texture’ (10 parents), ‘change to favoured texture’ (10 parents), ‘gradually mix favoured texture’ (10 parents), and ‘change to favoured flavours and tastes’ (nine parents). Of these classifications, the greatest change in compliance with regard to sensory function was ‘change the hated sensory elements’ and ‘use of favoured sensory elements'. In the open questions of the questionnaire, parents described their approaches as ‘I made the food bite-size to be eaten easily’ as an oral function; ‘I changed to softened food’ as a sensory function; ‘I served the same menu for the family,’ “I increased the volume of disliked food without letting the child know’, and ‘I cooked together and showed the child the cooking process’ as cognitive functions; and ‘I tried to eat at different places many times’ as an environment function.
Some successful examples were ‘I fried the fish’, ‘I cut the vegetables to a small size’, ‘I changed the vegetables used in the soup’, and ‘I mixed small carrots in gravy and hamburger patty’.
Number of Foods that Children found Acceptable
Among the 47 listed food items, the number of food items that children consumed significantly increased by 4.35 from 20.52 to 25.17 items (p = .004) after the intervention. On the other hand, the number of unaccepted food items significantly decreased by 2.73 from 14.52 to 11.79 items after the intervention (p < .001).
Parents' Subjective View of the Degree of Dietary Imbalance
The parents' subjective view of the degree of dietary imbalance was measured using a VAS, which showed a significant decrease of 13.65 points from 58.09 to 44.43 points after the intervention (p < .001).
Discussion
There were significant differences in all outcome measures before and after the intervention. Therefore, it is important that occupational therapists understand the factors and approaches for selective eating in children with ASD in order to provide early intervention for their parents.
The results of this study showed that the number of recommendations carried out by the parents increased after the intervention. This is possibly because the parents of children with ASD understood the factors of food preferences addressed in the programme, and they were influenced to implement these approaches to improve selective eating. Meanwhile, the degree of difficulty perceived by parents decreased, while self-efficacy improved after the intervention.
As expected, the parents' subjective view of the degree of dietary imbalance and the number of food items acceptable to the children improved after the intervention, and these perceptions are expected to maintain across time. In spite of the short period of this intervention (2 months), the intervention not only improved the parents' subjective view of the degree of dietary imbalance but also increased the number of food items that the children found acceptable. We believe that this result is a direct consequence of the improved communication among the parents in small groups, which enabled the parents to become familiar with the various factors underlying food preferences of their children and motivated them to try new approaches according to the responses of their children. The group dynamics motivated the parents and allowed them to address their challenges without stress. The results of this study show that increasing the number of approaches by parents can increase the number of food items acceptable to children with ASD. Furthermore, although the intervention was short, increasing the number of approaches can improve the degree of difficulty and self-efficacy perceived by parents. Further development of this programme will assist occupational therapists to develop implementation strategies to improving the variety of food preferences acceptable to children with ASD. Parents can also find out the best approach for their children based on various factors and identify the most feasible approach according to their family dynamics.
Limitations
An important limitation of this study was the definition of selective eating, as food selectivity has not been operationally defined in a consistent manner. One reason for the limited studies on the effects of selective eating is the lack of consistent application of an operational definition (Kelly et al., 2015). In this study, parents mentioned that a limited diet (selective eating) was a problem. However, after participating in this study, the parents reported a significant improvement in the perceived degree of difficulty associated with selective eating, self-efficacy, and the number of approaches for selective eating. On the other hand, there was no significant change in the degree of dietary imbalance or the number of food items acceptable to their children. Hence, the results of this study demonstrated that the proposed programme was useful as an introductory programme for parents who experience difficulty with regard to selective eating in their children and that it resulted in short-term improvements in the quality of life of both the parents and children.
Many parents had difficulties following the recommendations to improve selective eating in their children with ASD, which resulted in a decrease in the number of parents who participated in each session, and this might be a challenge in the future. Nonetheless, the findings of this study revealed that parents who participated in the programme benefited from the sessions and discussions. Therefore, we suggest enrolling parents at an earlier stage to familiarise them with the problems associated with implementation of new approaches designed to expand the variety and number of food items consumed by their children. In our next trial, we will continue this study with additional approaches. Furthermore, it is very difficult to address the issue in some children who demonstrate strong selective eating, such as those who choose only one or two food items. For such cases, we suggest longer-term intervention with one-to-one approaches.
Conclusion
In conclusion, we developed an interventional programme for parents of children with ASD and this programme was found to be useful. It is important for occupational therapists to consider the factors and approaches for selective eating in children with ASD in order to provide early intervention for their parents.
Acknowledgements
The authors wish to thank the developmental support centres for their support in this study and the families and children who participated in this study. The authors also wish to thank the members of the Osaka Prefecture University and Shijyonawate-gakuen University for their contribution in this study. The authors would like to thank Yoko Bourne, Yukiko Miyajima, and Enago (www.enago.jp), for the English language review.
Funding/Support:
No financial or material support of any kind was received for the work described in this article.
Conflicts of interest:
All contributing authors declare that they have no conflicts of interest.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Anderson S. E., Must A., Curtin C., & Bandini L. G. (2012). Meals in our household: Reliability and initial validation of a questionnaire to assess child mealtime behaviors and family mealtime environments. Journal of the Academy of Nutrition and Dietetics, 112(2), 276–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandini L. G., Anderson S. E., Curtin C., Cermak S., Evans E. W., Scampini R. et al. (2010). Food selectivity in children with autism spectrum disorders and typically developing children. Journal of Pediatrics, 157(2), 259–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bicer A. H., & Alsaffar A. A. (2013). Body mass index, dietary intake and feeding problems of Turkish children with autism spectrum disorder (ASD). Research in Developmental Disabilities, 34(11), 3978–3987. [DOI] [PubMed] [Google Scholar]
- Bijure P. E., Silver W. E., & Gallagher J. (2001). Reliability of the visual analog scale for measurement of acute pain. Academic Emergency Medicine, 8(12), 1153–1157. [DOI] [PubMed] [Google Scholar]
- Cermak S. A., Curtin C., & Bandini L. G. (2010). Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of American Diet Association, 110(2), 238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornish E. (1998). A balanced approach towards healthy eating in autism. Journal of Human Nutrition and Dietetics, 11(6), 501–509. [Google Scholar]
- Dovey T. M., Staples P. A., Gibson E. L., & Halford J. C. (2008). Food neophobia and 'picky/fussy' eating in children: A review. Appetite, 50(2–3), 181–193. [DOI] [PubMed] [Google Scholar]
- Emond A., Emmett P., Steer C., & Golding J. (2010). Feeding symptoms, dietary patterns and growth in young children with autism spectrum disorders. Pediatrics, 126(2), e337–e342. [DOI] [PubMed] [Google Scholar]
- Groden J., Diller A., Bausman M., Velicer W., Norman G., & Cautela J. (2001). The development of a stress survey schedule for persons with autism and other developmental disabilities. Journal of Autism and Developmental Disorders, 31(2), 207–217. [DOI] [PubMed] [Google Scholar]
- Herndon A. C., DiGuiseppi C., Johnson S. L., Leiferman J., & Reynolds A. (2009). Does nutritional intake differ between children with autism spectrum disorders and children with typical development. Journal of Autism and Developmental Disorders, 39(2), 212–222. [DOI] [PubMed] [Google Scholar]
- Hyman S. L., Stewart P. A., Schimidt B., Cain U., Lemcke N., Foley J. T. et al. (2012). Nutrient intake from food in children with autism. Pediatrics, 130(2), S145–S153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson C. R., Turner K., Stewart P. A., Schmidt B., Shui A., Macklin E. et al. (2014). Relationships between feeding problems, behavioral characteristics and nutritional quality in children with ASD. Journal of Autism and Developmental Disorders, 44(9), 2175–2184. [DOI] [PubMed] [Google Scholar]
- Kamio Y., Kawamata T., Nakai S., & Mishima K. (2015). Prevalence of developmental disorders in children before and after preschool and its developmental changes, regional-based cross-sectional and longitudinal studies. Comprehensive research report of Grant-in-Aid for Scientific Research grant http://mhlw-grants.niph.go.jp/niph/search/NIDD02.do?resrchNum=201317044A Accessed 20.04.17.
- Karashima C. (2008). Activities of daily living for children with developmental disorders and adults/families. Tokyo: Miwa Bookstore. [Google Scholar]
- Katz M. H., Kihara M., & Kihara M. (2013). Evaluating clinical and public health interventions, a practical guide to study design and statistics, Tokyo. [Google Scholar]
- Kelly T., Jane C. S., Marcia N. N., Karen R. S., Colleen S., & Amy R. D. (2015). Behavioral and physiological factors associated with selective eating in children with autism spectrum disorder. American Journal of Occupational Therapy, 69(6), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerwin M. E., Eicher P. S., & Gelsinger J. (2005). Parental report of eating problems and gastrointestinal symptoms in children with pervasive developmental disorders. Children's Health Care, 34(3), 217–234. [Google Scholar]
- Koyama T., Osada H., Tobari M., & Takeda T. (2003). Clinical significance of developmental quotient (DQ) in developmental assessment of children with pervasive developmental disorders. Japanese Journal of clinical psychiatry, 32(9), 1081–1087. [Google Scholar]
- Koyama T., Osada H., Tsujii H., & Kurita H. (2009). Utility of the Kyoto Scale of Psychological Development in cognitive assessment of children with pervasive developmental disorders. Psychiatry and Clinical Neurosciences, 63(2), 241–243. [DOI] [PubMed] [Google Scholar]
- Kral T. V. E., Erikson W. T., Souders M. C., & Pinto-Martin J. A. (2013). Eating behaviors, diet quality and gastrointestinal symptoms in children with autism spectrum disorders: A brief review. Journal of Pediatric Nursing, 28(6), 548–556. [DOI] [PubMed] [Google Scholar]
- Kuroda M., Inada N., & Uchiyama T. (2013). Social communication questionnaire Japanese manual, Tokyo. [Google Scholar]
- Legge B. (2002). Can't eat, won't eat: Dietary difficulties and autistic spectrum disorders. London, UK: Jessica Kingsley Publishers. [Google Scholar]
- Likert R. (1932). A technique for the measurement of attitudes. Archives of Psychology, 22, 5–55. [Google Scholar]
- Lockner D. W., Crowe T. K., & Skipper B. J. (2008). Dietary intake and parents' perception of mealtime behaviors in preschool-age children with autism spectrum disorder and in typically developing children. Journal of American Dietary Association, 108(8), 1360–1363. [DOI] [PubMed] [Google Scholar]
- Marshall J., Hill R. J., Ziviani J., & Dodrill P. (2013). Features of feeding difficulty in children with autism spectrum disorder. International Journal of Speech-Language Pathology, 16(2), 151–158. [DOI] [PubMed] [Google Scholar]
- Miyajima A., Tateyama K., Hirao K., Nakaoka K., & Higaki K. (2016). Reliability and validity of self-efficacy assessment for parents of children with selective eating disorder (SAPS). Japanese Occupational Therapy Research, 35(2), 167–179. [Google Scholar]
- Miyajima A., Tateyama K., Hirao K., Nakaoka K., & Higaki K. (2014). An exploratory study on the factors of food preferences and approaches for selective eating in children with Autism Spectrum Disorder (ASD). Japanese Occupational Therapy Research, 33(2), 124–136. [Google Scholar]
- Ministry of Health, Labor and Welfare. (2011). Child Development Support Center and the business. (on line), Available from http://www.mhlw.go.jp/seisakunitsuite/bunya/hukushi_kaigo/shougaishahukushi/kaigi_shiryou/dl/20111101_02-03.pdf Accessed 08.06.17.
- Raiten D. J., & Massaro T. (1986). Perspectives on the nutritional ecology of autistic children. Journal of Autism and Developmental Disorders, 16(2), 133–143. [DOI] [PubMed] [Google Scholar]
- Rogers L. G., Magill-Evans J., & Rempel G. R. (2012). Mother's challenges in feeding their children with autism spectrum disorder - managing more than picky eating. Journal of Developmental and Physical Disabilities, 24(1), 19–33. [Google Scholar]
- Rutter M., Bailey A., & Lord C. (2003). Social communication questionnaire manual, U.S.A. [Google Scholar]
- Schmitt L., Heiss C. J., & Campbell E. E. (2008). A comparison of nutrient intake and eating behaviors of boys with and without autism. Topics in Clinical Nutrition, 23(1), 23–31. [Google Scholar]
- Sharp W. G., Berry R. C., McCracken C., Nuhu N. N., Marvel E., Saulnier C. A. et al. (2013). Feeding problems and nutrient intake in children with autism spectrum disorders: A metaanalysis and comprehensive review of the literature. Journal of Autism and Developmental Disorders, 43(9), 2159–2173. [DOI] [PubMed] [Google Scholar]
- Tanner K., Case-Smith J., Nahikian-Nelms M., Ratliff-Schaub K., Spees C., & Darragh A. R. (2015). Behavioral and physiological factors associated with selective eating in children with autism spectrum disorder. American Journal of Occupational Therapy, 69(6), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tateyama K., Miyajima A., & Shimizu H. (2013). A study on the factors of food preferences and approaches for selective eating in children with autism spectrum disorders (ASD). Urakami Foundation Memoirs, 20, 117–132. http://urakamizaidan.or.jp/hp/jisseki/2010/vol20urakamif-16tateyama.pdf Accessed 20.04.17. [Google Scholar]
- Tateyama K., & Miyajima A. (2015). Points of assessment and nutrition at school age. The Japanese Journal of Child Nursing, Monthly, 38(2), 212–217. [Google Scholar]
- Tomchek S. D., & Dunn W. (2007). Sensory processing in children with and without autism: A comparative study using the Short Sensory Profile. American Journal of Occupational Therapy, 61(2), 190–200. [DOI] [PubMed] [Google Scholar]
- Twachtman-Reilly J., Amaral S. C., & Zebrowski P. P. (2008). Addressing feeding disorders in children on the autism spectrum in school-based settings: Physiological and behavioral issues. Language Speech Hearing Service in Schools, 39(2), 261–272. [DOI] [PubMed] [Google Scholar]
- Whiteley P., Rodgers J., & Shattock P. (2000). Feeding patterns in autism. Autism, 4(2), 207–211. [Google Scholar]
- Williams K. E., Hendy H., & Knecht S. (2008). Parent feeding practices and child variables associated with childhood feeding problems. Journal of Developmental and Physical Disabilities, 20, 231–242. [Google Scholar]
- Williams P. G., Dalrymple N., & Neal J. (2000). Eating habits of children with autism. Pediatrics Nursing, 26, 259–264. [PubMed] [Google Scholar]
- Wingate M., Kirby R. S., Pettygrove S., Cunniff C., Schulz E., Chosh T. et al. (2014). Centers for Disease Control and Prevention. Prevalence of autism spectrum disorder among children aged 8 years–Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report, 63SS-2, 1–21. [PubMed] [Google Scholar]
- Zimmer M. H., Hart L. C., Manning-Courtney P., Murray D. S., Bing N. M., & Summer S. (2012). Food variety as a predictor nutritional status among children with autism. Journal of Autism and Developmental Disorders, 42(4), 549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]


