Abstract
Teledermatology is a useful alternative where specialized dermatological assistance is not available and has been used successfully to support health professionals in a wide range of settings worldwide, in either an asynchronous store-and-forward format or a real-time video conferencing format. Teledermoscopy, which includes dermoscopic images in the teleconsultation, is another addition that improves remote assessments of pigmented lesions. A more recent variant is mobile teledermoscopy, which uses a smartphone to deliver the same type of service.
Teledermoscopy’s greatest strength may be as a triage and monitoring tool, as it can reduce the number of unnecessary referrals, wait times, and the cost of providing and receiving dermatological care. While face-to-face (FTF) care remains the gold standard for diagnosis, drawbacks of not using FTF care as the primary method can be mitigated if teleconsultants are willing to refer to FTF care whenever there is uncertainty. Teledermatology has generally been well accepted by patients and practitioners alike.
Barriers to the large-scale use of teledermatology remain. Assigning medicolegal responsibility and instituting a reimbursement system are critical to promoting widespread use by medical professionals, while privacy and security features and a mechanism to link teleconsultations to patients’ existing health records are essential to maximize patient benefit. Direct-to-consumer services also need attention from regulators to ensure that consumers can enjoy the benefits of telemedicine without the dangers of unregulated or untested platforms.
Keywords: teledermatology, teledermoscopy, mobile teledermoscopy, melanoma, skin cancer
Introduction
One of the earliest telemedicine specialties, teledermatology is now integrated into several public health systems [1–3] and has been used to support military personnel on deployment [4], staff on commercial ships [5], and care providers in nursing homes [6]. Teledermoscopy is also increasingly popular, using images taken with a digital dermatoscope or a standard digital camera with a dermoscopic attachment with magnification and polarized light, to show the lesion in more detail. Studies of teledermatology have assessed its usefulness in triage and referral by primary care providers (PCPs), consultation with patients or health professionals in remote or medically undersupplied locations, and monitoring patients with chronic skin conditions [6]. Teledermatology can also be a useful educational tool for dermatologists and other health care providers, who can send an image of a difficult rash or lesion to a more experienced colleague for diagnostic assistance and instruction [7–10].
Teledermatology can be delivered as a real-time video consultation (RT-TD) or as an asynchronous store-and-forward (SAF) service. Mobile teledermatology and teledermoscopy are extensions of these services, where a smartphone is used with or without a dermatoscopic attachment, to deliver the same type of service from a pocket-sized device. While RT-TD consultations have the advantage of allowing the teleconsultant to ask clarifying questions and providing direct instructions and education to the patient, the image quality of the video is usually inferior to static images used in SAF consultations. Teledermoscopy in particular relies on SAF technology, as its main usefulness lies in the superior detail and clarity of dermatoscopic images over clinical images. In addition, SAF consultations allow the teleconsultant to work at a time convenient to them, which is especially useful for consultations in different time zones.
Methods
We searched the PubMed database for reviews and original articles, restricted to human research published in English between 2015 and 2017. The search terms dermatolog*, dermoscop*, dermatoscop*, teledermatolog*, teledermoscop*, teledermatoscop*, remote consult, and remote consultation were combined in the appropriate method for PubMed. Studies were included if the primary focus was on teledermatology or teledermoscopy; studies focusing on computer-assisted diagnosis or teledermatopathology were excluded.
Results
A 2018 [6] literature review of teledermatology use found that the majority of studies were published in the US, UK, and Europe, with several studies conducted in Brazil, Australia, New Zealand, and Turkey, and fewer elsewhere in the world. Recent studies continue to examine teledermatology for a wide variety of disorders (Table 1); teledermoscopy has been mostly studied for assessing melanocytic and keratinocytic lesions [11–25].
TABLE 1.
Conditions Examined by Teledermatology
| Condition | References |
|---|---|
| Acne | [26–40] |
| Acneiform/drug eruption | [1,41–48] |
| Alopecia | [32,33,37,39,41,42,44] |
| Benign lesions including nevi, seborrheic keratoses, hemangiomas, and scars | [11–16,19–23,27,32,33,35, 38–41,44–46,48–61] |
| Premalignant neoplasms | [15,16,20,22,38–42,46,49, 50,52,58,60] |
| Malignant neoplasms | [1,11–22,32,35,38,40,41, 44–46,48–53,55–58,60–66] |
| Atypical or dysplastic nevi | [15,16,20–22,24,25,33,60] |
| Papulosquamous dermatoses | [31–36,38,39,41,42,44–48,58,59,67] |
| Dermatitis/eczema | [1,28,31–49,67,68] |
| Inflammatory conditions | [26,27,31,35,45,48,56–58] |
| Infections | [1,26,28,31,32,34–37,40, 42–48,56–59] |
| Hair or nail conditions | [26,27,44,49,59] |
| Wounds | [42,44] |
| Other | [1,21,26–29,31,32,34,42,43, 46–48,53,57–59,67,69,70] |
Accuracy and Interobserver Concordance
Most studies show comparable diagnostic accuracy between teledermatology and face-to-face (FTF) care [55,64,66,71,72], although 3 earlier studies reviewed by Lee and English [71] found teledermatology either significantly superior [9] or inferior [73,74]. More specifically, Finnane et al [75] reviewed accuracy of diagnosis for skin cancer; most studies showed that FTF consultations were more accurate than teledermatology (67%–85% vs 51%–85%); however, some studies found teledermatology was more accurate.
Interobserver agreement between FTF consultants and teledermatologists ranged from 45% to 96% for diagnosis [33,38,42,48,58,61,67] and 66% to 96% for management recommendations, rising to 80% to 90% for skin cancer management [58,61,71]. Between referring PCPs and teledermatologists, interobserver diagnostic agreement ranges from 21% to 60% [34,45,46,49,59,65], suggesting that teledermatology provides useful assistance to PCPs who lack specialist dermatological training. Still images can also be combined with video (called hybrid teledermatology); one study found that this improved management accuracy compared to assessments with still images alone (87.6% vs 71.7%, respectively). This may be because the video provides additional information about the patient’s behavior not captured by the referring doctor’s history [27].
An important recent study examined teledermatology interobserver concordance rates in patients with either Fitzpatrick I–III or IV–VI skin types. Concordance between FTF and teledermatology diagnosis and management were the same in both lighter and darker skin groups, suggesting that teledermatology is reliable for diagnosis in patients of all Fitzpatrick skin types [41].
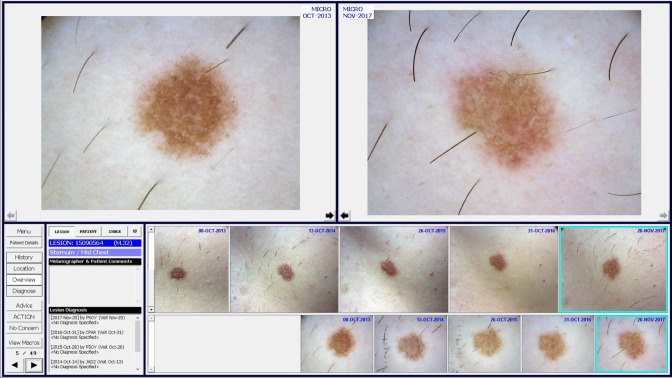
As is the case in FTF dermatology, including dermatoscopic images (Figure 1) in a teleconsultation appears to improve the reliability of telediagnoses, reportedly improving both sensitivity (0.93–1.0 with teledermatology vs 0.6–1.0 without) and specificity (0.85–0.97 vs 0.72–0.81) [14,55,64]. While including dermoscopy added 1 to 2 minutes to a consultation, 9 minutes (95% CI 8.3–9.5) with dermoscopy vs 7 minutes (95% CI 6.7–7.6) without dermoscopy, the teleconsultant’s evaluation time was almost the same for both groups, at 1.09 minutes (95% CI 1.04–1.14) with dermoscopy and 1.02 minutes (95% CI 1.0–1.04) without [14]. Other studies have found that interobserver concordance when using teledermoscopy is moderate (Fleiss kappa = 0.52) [16] to excellent (prevalence-adjusted, bias-adjusted kappa = 95) [12], with the exception of very difficult lesions [18].
Figure 1.
A dermoscopic image provides greater clarity and detail for melanocytic lesions. [Copyright: ©2018 Lee et al.]
Triaging
Numerous studies found that SAF teledermatology is highly effective as a triaging tool. It can reduce FTF referrals by 31% to 88%, surgery waiting times, and the number of no-shows at FTF clinics [11,13,14,29,31,32,35,42,46,53–57,64,67,71,76–80], although some studies report no difference in time to treatment [51] or number of secondary referrals [52].
Teledermatology can also improve access to dermatological care in lower income groups, such as Medicaid enrollees in the US [39]. Inclusion of dermatoscopic images also improves triaging decisions, including shorter waiting times and low number needed to excise for both melanomas (1.59) and other skin cancers (1.32) [13,42]. In a study comparing paper referrals without dermatoscopic images to digital referrals including dermoscopy, 43% of patients with benign lesions in the teledermoscopy arm were returned to a PCP without a FTF dermatologist appointment, compared to 1% from the paper referrals arm [16]. Inclusion of dermatoscopic images can also allow more cancers to be booked directly to surgery [16,50,64].
One drawback to the reduced number of patients being referred to FTF appointments is the risk of so-called “unimaged melanomas.” These lesions are not initially noted by the referring PCP but rather discovered by the dermatologist as an incidental part of the FTF examination. With reduced FTF appointments, there is a real risk of these lesions going unnoticed [62,63]. However, the reverse can also be true: one study focusing on aesthetic dermatology concerns also identified 5 skin cancers and 2 actinic keratoses by teledermatology [38].
Cost Effectiveness
While some studies found teledermatology to be more expensive than conventional care, in most studies teledermatology was equivalent or more economical [6,13,14,54,67,71,81,82]. Teledermatology consultations usually took longer than FTF consultations [14,83], but economic benefits for the health system stemmed from fewer FTF specialist referrals, and for patients from reduced travel time, costs, and time away from work and faster delivery of treatments [57,72,77,84,85]. RT-TD is generally more expensive than SAF modalities due to more expensive video conferencing technology and difficulty organizing suitable times for multiple clinicians, but can still be more cost-effective than FTF visits, particularly when the patient lives a long way from specialist dermatology care [26,72]. Cost-effectiveness studies have been limited by addressing only a few economic principles in each study; randomized clinical trials and other studies that include a comprehensive economic evaluation are still needed [77].
In terms of quality of life (QoL), there are relatively few studies about the effectiveness of teledermatology for improving QoL. A 2015 review found that teledermatology does improve QoL due to improvements in disease severity [86], but the only 2 studies comparing SAF teledermatology to FTF dermatology found that teledermatology and FTF care were equally effective at improving patients’ QoL [68,86].
User Attitudes
Patient and doctor attitudes to teledermatology are generally reported as neutral to good, with patients in rural areas often more positive than urban areas [26,35,38,52,54,57,59,60,72,82,87–91]. A study in which each participant was assessed FTF, by SAF and by RT-TD found that while patients preferred FTF assessment, they were still generally satisfied with teledermatology, and were evenly divided between preferring SAF and RT-TD [92]. Drivers of patient satisfaction included convenience, less travel, shorter waiting times, lower cost, and good quality of health care [21,26,87,92]. Some areas of patient dissatisfaction with teledermatology include poor follow-up or communication by their referring physician, feeling uncomfortable being photographed, or wishing to directly ask the teledermatologist questions [59,72,87]. Referring health care providers generally found teledermatology easy to use but were sometimes concerned about the service’s ability to meet patient demand, technical complications, and an increased workload. Consulting dermatologists were also concerned about the lack of ability to palpate lesions, reliability of teledermatology, legal liability, and financial reimbursement [21,57,80,87–90,92]. A survey of attitudes to teledermoscopy particularly found that 71% of dermatologists surveyed were in favor of PCPs using teledermatology to seek advice, provided there was dermoscopy training for the PCPs, or in the case of long travel distances or long waiting times [93].
Barriers to Routine Use
There are a number of barriers to the effective use of teledermatology. Reimbursement is a major issue to integrating teledermatology into the health care system, as is defining who is ultimately medically responsible for diagnosis and treatment decisions; these issues are complicated further if the referring doctor and consultant are in different jurisdictions [1,3,72,84,88,94,95]. Privacy and security while transmitting patient images and information are critical, as well as integration into electronic health records for maximum effectiveness [3,42,43,84,94,96]. International standards for encryption and data protection, such as International Organization for Standardization (ISO) standards ISO/TS 13131:2014 on telehealth services [97] or ISO/IEC 27001:2013 on information technology security [98], should be consulted when setting up a teledermatology service. Finally, referring health care providers will require training on what elements of the patient’s history are useful to the teledermatologist, appropriate image acquisition, especially how to use a dermatoscope effectively, and on effectively using the selected teledermatology platform [72,84,99] (see example in Figure 2).
Figure 2.
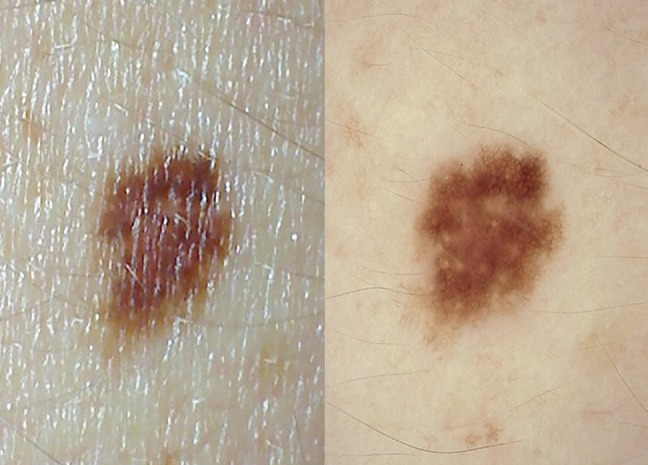
Sequential monitoring of a clinically dysplastic nevus using the MoleMap teledermoscopy platform. The 2 larger images in the top row compare dermoscopic images of the same lesion taken 4 years apart. The images in the middle row are clinical images of the same lesions taken over 4 years, and the images in the bottom row are the corresponding dermoscopic images. (Supplied by authors; H. Peter Soyer is a shareholder and consultant of MoleMap Pty Ltd.) [Copyright: ©2018 Lee et al.]
There are successful models for new services to draw on, including the Dutch health care system, where teledermatology is fully reimbursed and integrated in the health system, with electronic records available to all system users [3]; the teledermatology service of the US Veterans Health Administration [100]; an NGO-led teledermatology service in Toledo, Belize, where a collaboration between the Medical College of Wisconsin and Hillside Healthcare International has addressed technological requirements, training for PCPs, and ongoing adjustments to the service to optimize its usability [101]; and the Australian Tele-Derm National service, which provides consultations and education to rural and remote general practitioners [49].
Mobile Teledermatology and Teledermoscopy
Mobile teledermatology is the use of a smartphone to take and send images and information to a teleconsultant; mobile teledermoscopy is performed with a smartphone that has a dermoscopic attachment (Figure 3), usually in conjunction with an app to facilitate SAF teledermatology. This emerging technology is particularly useful for ongoing monitoring of chronic conditions that require frequent follow-up and changes to optimize treatment. In addition, in developing countries, mobile phone networks are well developed and often more reliable than other electronic communications [45,84].
Figure 3.

Mobile teledermoscopy with a Handyscope dermoscopic attachment (FotoFinder Systems GmbH, Bad Birnbach, Germany). [©2018 FotoFinder Systems]
A survey of Australian dermatologists and dermatology trainees found that mobile teledermatology was common, with more than 50% saying they sent or received clinical images using a smartphone at least weekly (rising to 89% of junior practitioners) [102]. However, it was also poorly regulated, with limited security measures, documentation of patient consent, or transfer of images to a patient’s permanent medical record. Dermatologists reported taking mobile phone images to obtain advice from a colleague, monitor patient progress, communicate with the patient’s other doctors, and for educational purposes [102]. Similarly, 47% of British dermatologists surveyed had used a mobile to take images for teledermatology, and 75% of these were aware of guidelines on data storage and transfer [89].
There are few studies comparing diagnostic and management concordance between mobile teledermoscopy and FTF assessment, but existing studies are generally positive, with 81% to 91% full or partial diagnostic concordance [40,48,58]. A German study found that accuracy of the clinical diagnosis, as compared to histopathological diagnosis, was 72.2% for FTF and 55.6% for teledermatologists [40].
Several studies suggest that PCP and dermatology staffs are able to capture good-quality images with a mobile phone [55,58]. Of note, a study of PCPs found they were able to provide mobile teledermoscopy images of similar quality to images taken in a dermatology department despite having little training in dermoscopy [11,15].
Images taken by study participants themselves are generally of sufficient quality for teleconsultations. A study of mobile dermoscopy with instructions on skin self-examination found that the images were generally good quality, with substantial agreement between mobile teledermoscopy and FTF diagnoses (kappa = 0.9), although 22% of participants did not choose to image lesions that were later selected for imaging by the clinician [22]. Similarly, a study of parent-taken images for a pediatric dermatology service found there was good correlation between telediagnoses and in-person diagnoses (82%) [33]. Another study of high school students found that 98% were able to take good-quality overview images of another person, and 66% were able to take in-focus dermoscopic images on the first try [23].
Mobile teledermoscopy is also a useful triaging tool for PCPs, having been used successfully in mass screening events [20], in underserved areas remote from FTF dermatologists [103], and for reducing waiting time for surgery compared to paper referrals [11].
Mobile teledermatology has also been explored as a relatively low-cost way to extend dermatological assistance to rural health services. A study of a service in Uganda and Guatemala, with US-based dermatologists, found that 89% of the teledermatology consultations changed the treatment plan initially suggested by the PCP, with the added benefit of PCPs improving their diagnostic accuracy over the course of the study [44].
Finally, there is an increasing number of direct-to-consumer website- or app-based dermatology services, which can be very popular with patients: a trial of one app for pediatric dermatology found 83% of parents said that, had the app been unavailable, they would have sought FTF appointments with a PCP, an urgent care clinic, or a dermatologist [28]. Review of such services in 2014–2015 found that there were up to 29 available to US patients, with some restricting their advice to acne or anti-aging, while others were treating patients for any condition [29, 104,105]. There is also a number of services aimed at pediatric patients [106]. As for general teledermatology, this form of mobile teledermatology can substantially reduce the waiting period to access care, but services are poorly regulated, frequently do not require proper verification of patient identity, and provide little continuity of care or integration with the patient’s official medical record [29,105–107]. However, there are examples that avoid these pitfalls, usually by being associated with a regulated health care provider, such as the Stanford Health Care eCare Direct program [91] or a trial giving direct-to-consumer access to existing members of a commercial health plan [36].
Ongoing Monitoring
One major advantage of mobile teledermatology is that patients themselves may collect images for short-term monitoring, without requiring a FTF appointment. A study of 29 patients found that 97% were able to collect suitable baseline and follow-up images of nevi with a mobile dermatoscope, with a good diagnostic concordance (kappa = 0.87) between FTF consultations and teledermatology [24]. A study of a smartphone SAF service for facial laser resurfacing patients, allowing them to send daily images of their skin to monitor healing after the procedure, found that patients using the service required fewer FTF consultations. As well as detecting any adverse reactions requiring medical treatment, the teleconsultant was able to reassure participants about reactions that were an expected part of the healing process, such as swelling, exudation, or crusting [69]. A randomized control trial examining ongoing monitoring of isotretinoin acne treatment also found that the mobile teledermatology patients had equivalent treatment success and fewer adverse events than the FTF patients [30].
User Attitudes
There are few studies of consumer or professional acceptance of mobile teledermatology and dermoscopy, but existing studies indicate favorable attitudes. Patients generally expressed satisfaction with mobile services, citing improved waiting times, convenience, comfort, reassurance, and privacy [24,30,69]. One study found that a high number of participants believe that mobile teledermoscopy would improve their skin self-examinations for cancer and motivate them to check their skin more often [19], and in other studies parents were willing to use a pediatric teledermatology service for their children [28,33]. Participants generally reported feeling comfortable and competent with taking dermoscopic images after minimal instructions [19,23].
Drawbacks were requiring assistance to image hard-to-reach areas like the back [19], uncertainty about privacy and accuracy [69], uncertainty about completely trusting a telediagnosis [19], and uncertainty about whether insurance would cover such a service [24]. A discrete choice survey of mobile teledermoscopy patients found that patients preferred involvement of a doctor to skin self-examinations, but also strongly preferred having their concerning lesions assessed by a dermatologist rather than a GP, which is more easily achieved via mobile teledermoscopy [108].
There are very few studies of clinician attitudes about mobile teledermatology. A survey of nurses in Arizona, which included an introduction to mobile teledermoscopy, example images, and case studies, found that although most had not used mobile teledermoscopy, they perceived it to have the ability to improve diagnosis and positively affect their practice, with moderate scores for perceived ease of use. However, this study may be influenced by self-selection bias [109].
Barriers to Use of Mobile Teledermatology
While modern smartphones enable patients to take and forward their own images, patient-acquired images have drawbacks such as teleconsultants having difficulty confirming patient identity and coordinating with PCPs [72]. The proliferation of poorly regulated direct-to-consumer teledermatology apps may also have adverse outcomes for consumers who rely on them rather than professional, individual medical advice, particularly where the service relies on algorithms to diagnose or suggest treatment plans, without oversight by a trained health care provider [29,106,107,110].
Conclusions
Teledermatology is a useful alternative where specialized dermatological assistance is not available, and has generally been accepted by patients and practitioners alike. Its greatest strength may be as a triage and/or monitoring tool, in both underserved areas and busy metropolitan dermatology clinics, by reducing both the number of unnecessary referrals and wait times. While FTF care remains the gold standard for diagnosis, this drawback can be mitigated if teleconsultants are willing to refer to FTF care whenever there is uncertainty.
Despite these advantages, barriers remain to incorporating teledermatology into large-scale use. Privacy and security features are essential to any telemedicine system, and teledermatology records need to be linked to patients’ health records for maximum effectiveness. Assigning medicolegal responsibility and instituting a reimbursement system are also critical to persuading greater numbers of health professionals to use teledermatology. Direct-to-consumer services also need attention from regulators to ensure that consumers can enjoy the benefits of telemedicine without the dangers of unregulated or untested platforms.
Footnotes
Funding: This funding was supported by the Australian National Health and Medical Research Council (Centre for Research Excellence for the Study of Naevi APP1099021).
Competing interests: Prof. H. Peter Soyer is a shareholder of e-derm consult GmbH and MoleMap by Dermatologists Ltd Pty. He provides teledermatological reports regularly for both companies. Ms. Katie J. Lee and Dr. Anna Finnane have no conflicts of interest to disclose.
References
- 1.Finnane A, Siller G, Mujcic R, Soyer HP. The growth of a skin emergency teledermatology service from 2008 to 2014. Australas J Dermatol. 2016;57(1):14–18. doi: 10.1111/ajd.12411. [DOI] [PubMed] [Google Scholar]
- 2.Vega S, Marciscano I, Holcomb M, et al. Army–Republic of Panama Initiative. Testing a top-down strategy for establishing a sustainable telemedicine program in a developing country: the Arizona telemedicine program-US Army–Republic of Panama Initiative. Telemed J E Health. 2013;19(10):746–753. doi: 10.1089/tmj.2013.0025. [DOI] [PubMed] [Google Scholar]
- 3.Tensen E, van der Heijden JP, Jaspers MW, Witkamp L. Two decades of teledermatology: current status and integration in national healthcare systems. Curr Dermatol Rep. 2016;5(2):96–104. doi: 10.1007/s13671-016-0136-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hwang JS, Lappan CM, Sperling LC, Meyerle JH. Utilization of telemedicine in the U S. military in a deployed setting. Mil Med. 2014;179(11):1347–1353. doi: 10.7205/MILMED-D-14-00115. [DOI] [PubMed] [Google Scholar]
- 5.Dahl E. Briefing notes on maritime teledermatology. Int Marit Health. 2014;65(2):61–64. doi: 10.5603/IMH.2014.0014. [DOI] [PubMed] [Google Scholar]
- 6.Trettel A, Eissing L, Augustin M. Telemedicine in dermatology: findings and experiences worldwide – a systematic literature review. J Eur Acad Dermatol Venereol. 2018;32(2):215–224. doi: 10.1111/jdv.14341. [DOI] [PubMed] [Google Scholar]
- 7.Coates DF, Soyer HP. Teledermoscopy and computer-assisted diagnosis. In: Marghoob AA, Malvehy J, Braun R, editors. Atlas of Dermoscopy. 2nd ed. London: Independence: Informa Healthcare; 2012. pp. 362–365. [Google Scholar]
- 8.Boyers LN, Schultz A, Baceviciene R, et al. Teledermatology as an educational tool for teaching dermatology to residents and medical students. Telemed J E Health. 2015;21(4):312–314. doi: 10.1089/tmj.2014.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lozzi GP, Soyer HP, Massone C, et al. The additive value of second opinion teleconsulting in the management of patients with challenging inflammatory, neoplastic skin diseases: a best practice model in dermatology? J Eur Acad Dermatol Venereol. 2007;21(1):30–34. doi: 10.1111/j.1468-3083.2006.01846.x. [DOI] [PubMed] [Google Scholar]
- 10.Nelson CA, Wanat KA, Roth RR, James WD, Kovarik CL, Takeshita J. Teledermatology as pedagogy: diagnostic and management concordance between resident and attending dermatologists. J Am Acad Dermatol. 2015;72(3):555–557. doi: 10.1016/j.jaad.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Börve A, Dahlén Gyllencreutz J, Terstappen K, et al. Smartphone teledermoscopy referrals: a novel process for improved triage of skin cancer patients. Acta Derm Venereol. 2015;95(2):186–190. doi: 10.2340/00015555-1906. [DOI] [PubMed] [Google Scholar]
- 12.Arzberger E, Curiel-Lewandrowski C, Blum A, et al. Teledermoscopy in high-risk melanoma patients: a comparative study of face-to-face and teledermatology visits. Acta Derm Venereol. 2016;96(6):779–783. doi: 10.2340/00015555-2344. [DOI] [PubMed] [Google Scholar]
- 13.Congalton AT, Oakley AM, Rademaker M, Bramley D, Martin RC. Successful melanoma triage by a virtual lesion clinic (teledermoscopy) J Eur Acad Dermatol Venereol. 2015;29(12):2423–2428. doi: 10.1111/jdv.13309. [DOI] [PubMed] [Google Scholar]
- 14.Ferrándiz L, Ojeda-Vila T, Corrales A, et al. Internet-based skin cancer screening using clinical images alone or in conjunction with dermoscopic images: A randomized teledermoscopy trial. J Am Acad Dermatol. 2017;76(4):676–682. doi: 10.1016/j.jaad.2016.10.041. [DOI] [PubMed] [Google Scholar]
- 15.Dahlén Gyllencreutz J, Johansson Backman E, Terstappen K, Paoli J. Teledermoscopy images acquired in primary health care and hospital settings - a comparative study of image quality. J Eur Acad Dermatol Venereol. 2018;32(6):1038–1043. doi: 10.1111/jdv.14565. [DOI] [PubMed] [Google Scholar]
- 16.Dahlén Gyllencreutz J, Paoli J, Bjellerup M, et al. Diagnostic agreement and interobserver concordance with teledermoscopy referrals. J Eur Acad Dermatol Venereol. 2017;31(5):898–903. doi: 10.1111/jdv.14147. [DOI] [PubMed] [Google Scholar]
- 17.Daniel CL, Armstrong GT, Keske RR, et al. Advancing Survivors’ Knowledge (ASK) about skin cancer study: study protocol for a randomized controlled trial. Trials. 2015;16(1):109. doi: 10.1186/s13063-015-0637-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Giorgi V, Gori A, Savarese I, et al. Teledermoscopy in doubtful melanocytic lesions: is it really useful? Int J Dermatol. 2016;55(10):1119–1123. doi: 10.1111/ijd.13281. [DOI] [PubMed] [Google Scholar]
- 19.Horsham C, Loescher LJ, Whiteman DC, Soyer HP, Janda M. Consumer acceptance of patient-performed mobile teledermoscopy for the early detection of melanoma. Br J Dermatol. 2016;175(6):1301–1310. doi: 10.1111/bjd.14630. [DOI] [PubMed] [Google Scholar]
- 20.Hue L, Makhloufi S, Sall N’Diaye P, et al. Real-time mobile teledermoscopy for skin cancer screening targeting an agricultural population: an experiment on 289 patients in France. J Eur Acad Dermatol Venereol. 2016;30(1):20–24. doi: 10.1111/jdv.13404. [DOI] [PubMed] [Google Scholar]
- 21.Kenney AS, Yiannias JA, Raghu TS, David PS, Chang YH, Greig HE. Measures of satisfaction for providers and patients using same day teledermoscopy consultation. Int J Dermatol. 2016;55(7):781–785. doi: 10.1111/ijd.12892. [DOI] [PubMed] [Google Scholar]
- 22.Manahan MN, Soyer HP, Loescher LJ, et al. A pilot trial of mobile, patient-performed teledermoscopy. Br J Dermatol. 2015;172(4):1072–1080. doi: 10.1111/bjd.13550. [DOI] [PubMed] [Google Scholar]
- 23.Marchetti MA, Fonseca M, Dusza SW, et al. Dermatoscopic imaging of skin lesions by high school students: a cross-sectional pilot study. Dermatol Pract Concept. 2015;5(1):11–28. doi: 10.5826/dpc.0501a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu X, Oliveria SA, Yagerman S, et al. Feasibility and efficacy of patient-initiated mobile teledermoscopy for short-term monitoring of clinically atypical nevi. JAMA Dermatol. 2015;151(5):489–496. doi: 10.1001/jamadermatol.2014.3837. [DOI] [PubMed] [Google Scholar]
- 25.Argenziano G, Soyer HP, Chimenti S, et al. Dermoscopy of pigmented skin lesions: results of a consensus meeting via the Internet. J Am Acad Dermatol. 2003;48(5):679–693. doi: 10.1067/mjd.2003.281. [DOI] [PubMed] [Google Scholar]
- 26.Al Quran HA, Khader YS, Ellauzi ZM, Shdaifat A. Effect of real-time teledermatology on diagnosis, treatment and clinical improvement. J Telemed Telecare. 2015;21(2):93–99. doi: 10.1177/1357633X14566572. [DOI] [PubMed] [Google Scholar]
- 27.Feigenbaum DF, Boscardin CK, Frieden IJ, Mathes EFD. Can you see me now? Video supplementation for pediatric teledermatology cases. Pediatr Dermatol. 2017;34(5):566–571. doi: 10.1111/pde.13210. [DOI] [PubMed] [Google Scholar]
- 28.Fiks AG, Fleisher L, Berrigan L, et al. Usability, acceptability, and impact of a pediatric teledermatology mobile health application. Telemed J E Health. 2018;24(3):236–245. doi: 10.1089/tmj.2017.0075. [DOI] [PubMed] [Google Scholar]
- 29.Fogel AL, Sarin KY. A survey of direct-to-consumer teledermatology services available to US patients: explosive growth, opportunities and controversy. J Telemed Telecare. 2017;23(1):19–25. doi: 10.1177/1357633X15624044. [DOI] [PubMed] [Google Scholar]
- 30.Frühauf J, Kröck S, Quehenberger F, et al. Mobile teledermatology helping patients control high-need acne: a randomized controlled trial. J Eur Acad Dermatol Venereol. 2015;29(5):919–924. doi: 10.1111/jdv.12723. [DOI] [PubMed] [Google Scholar]
- 31.Nair AR, Nair PA. Teledermatology: a possible reality in rural India. Int J Dermatol. 2015;54(3):375–376. doi: 10.1111/ijd.12624. [DOI] [PubMed] [Google Scholar]
- 32.Naka F, Lu J, Porto A, Villagra J, Wu ZH, Anderson D. Impact of dermatology eConsults on access to care and skin cancer screening in underserved populations: A model for teledermatology services in community health centers. J Am Acad Dermatol. 2018;78(2):293–302. doi: 10.1016/j.jaad.2017.09.017. [DOI] [PubMed] [Google Scholar]
- 33.O’Connor DM, Jew OS, Perman MJ, Castelo-Soccio LA, Winston FK, McMahon PJ. Diagnostic accuracy of pediatric teledermatology using parent-submitted photographs: a randomized clinical trial. JAMA Dermatol. 2017;153(12):1243–1248. doi: 10.1001/jamadermatol.2017.4280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patro BK, Tripathy JP, De D, Sinha S, Singh A, Kanwar AJ. Diagnostic agreement between a primary care physician and a teledermatologist for common dermatological conditions in North India. Indian Dermatol Online J. 2015;6(1):21–26. doi: 10.4103/2229-5178.148927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Piette E, Nougairède M, Vuong V, Crickx B, Tran VT. Impact of a store-and-forward teledermatology intervention versus usual care on delay before beginning treatment: A pragmatic cluster-randomized trial in ambulatory care. J Telemed Telecare. 2017;23(8):725–732. doi: 10.1177/1357633X16663328. [DOI] [PubMed] [Google Scholar]
- 36.Rajda J, Seraly MP, Fernandes J, et al. Impact of direct to consumer store-and-forward teledermatology on access to care, satisfaction, utilization, and costs in a commercial health plan population. Telemed J E Health. 2018;24(2):166–169. doi: 10.1089/tmj.2017.0078. [DOI] [PubMed] [Google Scholar]
- 37.Seol JE, Park SH, Kim H. Analysis of live interactive teledermatologic consultations for prisoners in Korea for 3 years. J Telemed Telecare. 2017 doi: 10.1177/1357633X17732095. 1357633x17732095. [DOI] [PubMed] [Google Scholar]
- 38.Tian B. Tele-aesthetics in South Asia. J Cosmet Dermatol. 2017;16(1):21–25. doi: 10.1111/jocd.12257. [DOI] [PubMed] [Google Scholar]
- 39.Uscher-Pines L, Malsberger R, Burgette L, Mulcahy A, Mehrotra A. Effect of teledermatology on access to dermatology care among Medicaid enrollees. JAMA Dermatol. 2016;152(8):905–912. doi: 10.1001/jamadermatol.2016.0938. [DOI] [PubMed] [Google Scholar]
- 40.Zink A, Kolbinger A, Leibl M, et al. The value of teledermatology using a mobile app compared to conventional dermatology. Eur J Dermatol. 2017;27(4):429–431. doi: 10.1684/ejd.2017.3044. [DOI] [PubMed] [Google Scholar]
- 41.Altieri L, Hu J, Nguyen A, et al. Interobserver reliability of teledermatology across all Fitzpatrick skin types. J Telemed Telecare. 2017;23(1):68–73. doi: 10.1177/1357633X15621226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carter ZA, Goldman S, Anderson K, et al. Creation of an internal teledermatology store-and-forward system in an existing electronic health record: a pilot study in a safety-net public health and hospital system. JAMA Dermatol. 2017;153(7):644–650. doi: 10.1001/jamadermatol.2017.0204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Finnane AR, Siller G, Soyer HP. Teledermatologists’ management of emergency skin conditions. Med J Aust. 2015;203(7):286. doi: 10.5694/mja15.00362. [DOI] [PubMed] [Google Scholar]
- 44.Greisman L, Nguyen TM, Mann RE, et al. Feasibility and cost of a medical student proxy-based mobile teledermatology consult service with Kisoro, Uganda, and Lake Atitlán, Guatemala. Int J Dermatol. 2015;54(6):685–692. doi: 10.1111/ijd.12708. [DOI] [PubMed] [Google Scholar]
- 45.Lipoff JB, Cobos G, Kaddu S, Kovarik CL. The Africa Teledermatology Project: A retrospective case review of 1229 consultations from sub-Saharan Africa. J Am Acad Dermatol. 2015;72(6):1084–1085. doi: 10.1016/j.jaad.2015.02.1119. [DOI] [PubMed] [Google Scholar]
- 46.Nelson CA, Takeshita J, Wanat KA, et al. Impact of store-and-forward (SAF) teledermatology on outpatient dermatologic care: A prospective study in an underserved urban primary care setting. J Am Acad Dermatol. 2016;74(3):484–90.e1. doi: 10.1016/j.jaad.2015.09.058. [DOI] [PubMed] [Google Scholar]
- 47.Nguyen A, Tran D, Uemura M, Bardin RL, Shitabata PK. Practical and sustainable teledermatology and teledermatopathology: specialty care in Cameroon Africa. J Clin Aesthet Dermatol. 2017;10(1):47–56. [PMC free article] [PubMed] [Google Scholar]
- 48.Okita AL, Molina Tinoco LJ, Patatas OH, et al. Use of smartphones in telemedicine: comparative study between standard and teledermatological evaluation of high-complex care hospital inpatients. Telemed J E Health. 2016;22(9):755–760. doi: 10.1089/tmj.2015.0086. [DOI] [PubMed] [Google Scholar]
- 49.Byrom L, Lucas L, Sheedy V, et al. Tele-Derm National: a decade of teledermatology in rural and remote Australia. Aust J Rural Health. 2016;24(3):193–199. doi: 10.1111/ajr.12248. [DOI] [PubMed] [Google Scholar]
- 50.Cotes ME, Albers LN, Sargen M, Chen SC. Diagnostic accuracy of teledermatology for nonmelanoma skin cancer: can patients be referred directly for surgical management? J Am Acad Dermatol. 2017 doi: 10.1016/j.jaad.2017.09.029. S0190–9622(17)32434–9. [DOI] [PubMed] [Google Scholar]
- 51.Creighton-Smith M, Murgia RD, III, Konnikov N, Dornelles A, Garber C, Nguyen BT. Incidence of melanoma and keratinocytic carcinomas in patients evaluated by store-and-forward teledermatology vs. dermatology clinic. Int J Dermatol. 2017;56(10):1026–1031. doi: 10.1111/ijd.13672. [DOI] [PubMed] [Google Scholar]
- 52.Ford JA, Pereira A. Does teledermatology reduces secondary care referrals and is it acceptable to patients and doctors?: a service evaluation. J Eval Clin Pract. 2015;21(4):710–716. doi: 10.1111/jep.12373. [DOI] [PubMed] [Google Scholar]
- 53.Leavitt ER, Kessler S, Pun S, et al. Teledermatology as a tool to improve access to care for medically underserved populations: A retrospective descriptive study. J Am Acad Dermatol. 2016;75(6):1259–1261. doi: 10.1016/j.jaad.2016.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Livingstone J, Solomon J. An assessment of the cost-effectiveness, safety of referral and patient satisfaction of a general practice teledermatology service. London J Prim Care (Abingdon) 2015;7(2):31–35. doi: 10.1080/17571472.2015.11493433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Markun S, Scherz N, Rosemann T, Tandjung R, Braun RP. Mobile teledermatology for skin cancer screening: a diagnostic accuracy study. Medicine (Baltimore) 2017;96(10):e6278. doi: 10.1097/MD.0000000000006278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Martin I, Aphivantrakul PP, Chen KH, Chen SC. Adherence to teledermatology recommendations by primary health care professionals: strategies for improving follow-up on teledermatology recommendations. JAMA Dermatol. 2015;151(10):1130–1132. doi: 10.1001/jamadermatol.2015.1884. [DOI] [PubMed] [Google Scholar]
- 57.McGoey ST, Oakley A, Rademaker M. Waikato Teledermatology: a pilot project for improving access in New Zealand. J Telemed Telecare. 2015;21(7):414–419. doi: 10.1177/1357633X15583216. [DOI] [PubMed] [Google Scholar]
- 58.Nami N, Massone C, Rubegni P, Cevenini G, Fimiani M, Hofmann-Wellenhof R. Concordance and time estimation of store-and-forward mobile teledermatology compared to classical face-to-face consultation. Acta Derm Venereol. 2015;95(1):35–39. doi: 10.2340/00015555-1876. [DOI] [PubMed] [Google Scholar]
- 59.Saleh N, Abdel Hay R, Hegazy R, Hussein M, Gomaa D. Can teledermatology be a useful diagnostic tool in dermatology practice in remote areas? An Egyptian experience with 600 patients. J Telemed Telecare. 2017;23(2):233–238. doi: 10.1177/1357633X16633944. [DOI] [PubMed] [Google Scholar]
- 60.Tandjung R, Badertscher N, Kleiner N, et al. Feasibility and diagnostic accuracy of teledermatology in Swiss primary care: process analysis of a randomized controlled trial. J Eval Clin Pract. 2015;21(2):326–331. doi: 10.1111/jep.12323. [DOI] [PubMed] [Google Scholar]
- 61.Warshaw EM, Gravely AA, Nelson DB. Reliability of store and forward teledermatology for skin neoplasms. J Am Acad Dermatol. 2015;72(3):426–435. doi: 10.1016/j.jaad.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 62.Gendreau JL, Gemelas J, Wang M, et al. Unimaged melanomas in store-and-forward teledermatology. Telemed J E Health. 2017;23(6):517–520. doi: 10.1089/tmj.2016.0170. [DOI] [PubMed] [Google Scholar]
- 63.Keleshian V, Ortega-Loayza AG, Tarkington P. Incidental skin malignancies in teledermatology and in-person cohorts in the Veterans Affairs Health System. J Am Acad Dermatol. 2017;77(5):965–966. doi: 10.1016/j.jaad.2017.01.027. [DOI] [PubMed] [Google Scholar]
- 64.Moreno-Ramírez D, Argenziano G. Teledermatology and mobile applications in the management of patients with skin lesions. Acta Derm Venereol. 2017 doi: 10.2340/00015555-2718. [DOI] [PubMed] [Google Scholar]
- 65.Piccoli MF, Amorim BD, Wagner HM, Nunes DH. Teledermatology protocol for screening of skin cancer. An Bras Dermatol. 2015;90(2):202–210. doi: 10.1590/abd1806-4841.20153163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang M, Gendreau JL, Gemelas J, et al. Diagnosis and management of malignant melanoma in store-and-forward teledermatology. Telemed J E Health. 2017;23(11):877–880. doi: 10.1089/tmj.2017.0009. [DOI] [PubMed] [Google Scholar]
- 67.Seghers AC, Seng KH, Chio MT, Chia E, Ng SK, Tang MB. A prospective study on the use of teledermatology in psychiatric patients with chronic skin diseases. Australas J Dermatol. 2015;56(3):170–174. doi: 10.1111/ajd.12297. [DOI] [PubMed] [Google Scholar]
- 68.Kornmehl H, Singh S, Johnson MA, Armstrong AW. Direct-access online care for the management of atopic dermatitis: a randomized clinical trial examining patient quality of life. Telemed J E Health. 2017;23(9):726–732. doi: 10.1089/tmj.2016.0249. [DOI] [PubMed] [Google Scholar]
- 69.Chee SN, Lowe P, Lim A. Smartphone patient monitoring post-laser resurfacing. Australas J Dermatol. 2017;58(4):e216–e222. doi: 10.1111/ajd.12507. [DOI] [PubMed] [Google Scholar]
- 70.Grey KR, Hagen SL, Hylwa SA, Warshaw EM. Utility of store and forward teledermatology for skin patch test readings. Dermatitis. 2017;28(2):152–161. doi: 10.1097/DER.0000000000000258. [DOI] [PubMed] [Google Scholar]
- 71.Lee JJ, English JC., III Teledermatology: a review and update. Am J Clin Dermatol. 2018;19(2):253–260. doi: 10.1007/s40257-017-0317-6. [DOI] [PubMed] [Google Scholar]
- 72.Campagna M, Naka F, Lu J. Teledermatology: an updated overview of clinical applications and reimbursement policies. Int J Womens Dermatol. 2017;3(3):176–179. doi: 10.1016/j.ijwd.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Warshaw EM, Lederle FA, Grill JP, et al. Accuracy of teledermatology for nonpigmented neoplasms. J Am Acad Dermatol. 2009;60(4):579–588. doi: 10.1016/j.jaad.2008.11.892. [DOI] [PubMed] [Google Scholar]
- 74.Warshaw EM, Lederle FA, Grill JP, et al. Accuracy of teledermatology for pigmented neoplasms. J Am Acad Dermatol. 2009;61(5):753–765. doi: 10.1016/j.jaad.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 75.Finnane A, Dallest K, Janda M, Soyer HP. Teledermatology for the diagnosis and management of skin cancer: a systematic review. JAMA Dermatol. 2017;153(3):319–327. doi: 10.1001/jamadermatol.2016.4361. [DOI] [PubMed] [Google Scholar]
- 76.Bruce AF, Mallow JA, Theeke LA. The use of teledermoscopy in the accurate identification of cancerous skin lesions in the adult population: a systematic review. J Telemed Telecare. 2018;24(2):75–83. doi: 10.1177/1357633X16686770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Snoswell C, Finnane A, Janda M, Soyer HP, Whitty JA. Cost-effectiveness of store-and-forward teledermatology: a systematic review. JAMA Dermatol. 2016;152(6):702–708. doi: 10.1001/jamadermatol.2016.0525. [DOI] [PubMed] [Google Scholar]
- 78.Bezalel S, Fabri P, Park HS. Implementation of store-and-forward teledermatology and its associated effect on patient access in a Veterans Affairs dermatology clinic. JAMA Dermatol. 2015;151(5):556–557. doi: 10.1001/jamadermatol.2014.5272. [DOI] [PubMed] [Google Scholar]
- 79.Raugi GJ, Nelson W, Miethke M, et al. Teledermatology implementation in a VHA secondary treatment facility improves access to face-to-face care. Telemed J E Health. 2016;22(1):12–17. doi: 10.1089/tmj.2015.0036. [DOI] [PubMed] [Google Scholar]
- 80.Sharma P, Kovarik CL, Lipoff JB. Teledermatology as a means to improve access to inpatient dermatology care. J Telemed Telecare. 2016;22(5):304–310. doi: 10.1177/1357633X15603298. [DOI] [PubMed] [Google Scholar]
- 81.Datta SK, Warshaw EM, Edison KE, et al. Cost and utility analysis of a store-and-forward teledermatology referral system: a randomized clinical trial. JAMA Dermatol. 2015;151(12):1323–1329. doi: 10.1001/jamadermatol.2015.2362. [DOI] [PubMed] [Google Scholar]
- 82.Wootton R, Liu J, Bonnardot L, Venugopal R, Oakley A. Experience with quality assurance in two store-and-forward telemedicine networks. Front Public Health. 2015;3:261. doi: 10.3389/fpubh.2015.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fuertes-Guiró F, Girabent-Farrés M. Opportunity cost of the dermatologist’s consulting time in the economic evaluation of teledermatology. J Telemed Telecare. 2017;23(7):657–664. doi: 10.1177/1357633X16660876. [DOI] [PubMed] [Google Scholar]
- 84.Coates SJ, Kvedar J, Granstein RD. Teledermatology: from historical perspective to emerging techniques of the modern era: part II: emerging technologies in teledermatology, limitations and future directions. J Am Acad Dermatol. 2015;72(4):577–586. doi: 10.1016/j.jaad.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 85.Nguyen B, Murgia R, Creighton-Smith M, Dornelles A, Garber C, Konnikov N. Use of spatial mapping technology to characterize geographic and socioeconomic reach of teledermatology service. J Telemed Telecare. 2017;23(7):688–690. doi: 10.1177/1357633X16686778. [DOI] [PubMed] [Google Scholar]
- 86.Whited JD. Quality of life: a research gap in teledermatology. Int J Dermatol. 2015;54(10):1124–1128. doi: 10.1111/ijd.12909. [DOI] [PubMed] [Google Scholar]
- 87.Mounessa JS, Chapman S, Braunberger T, et al. A systematic review of satisfaction with teledermatology. J Telemed Telecare. 2018;24(4):263–270. doi: 10.1177/1357633X17696587. [DOI] [PubMed] [Google Scholar]
- 88.Fogel AL, Teng JM. Pediatric teledermatology: a survey of usage, perspectives, and practice. Pediatr Dermatol. 2015;32(3):363–368. doi: 10.1111/pde.12533. [DOI] [PubMed] [Google Scholar]
- 89.Mehrtens SH, Halpern SM. Changing use and attitudes towards teledermatology in the U K. over 10 years: results of the 2016 National Survey. Br J Dermatol. 2018;178(1):286–288. doi: 10.1111/bjd.15606. [DOI] [PubMed] [Google Scholar]
- 90.Ogbechie OA, Nambudiri VE, Vleugels RA. Teledermatology perception differences between urban primary care physicians and dermatologists. JAMA Dermatol. 2015;151(3):339–340. doi: 10.1001/jamadermatol.2014.3331. [DOI] [PubMed] [Google Scholar]
- 91.Pathipati AS, Ko JM. Implementation and evaluation of Stanford Health Care direct-care teledermatology program. SAGE Open Med. 2016;4 doi: 10.1177/2050312116659089. 2050312116659089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Marchell R, Locatis C, Burgess G, Maisiak R, Liu WL, Ackerman M. Patient and provider satisfaction with teledermatology. Telemed J E Health. 2017;23(8):684–690. doi: 10.1089/tmj.2016.0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kukutsch NA, Argenziano G, Bergman W. The opinion of dermoscopy experts about teledermoscopy involving primary care physicians and dermatologists. J Eur Acad Dermatol Venereol. 2017;31(10):e470–e471. doi: 10.1111/jdv.14259. [DOI] [PubMed] [Google Scholar]
- 94.McKoy K, Antoniotti NM, Armstrong A, et al. practice guidelines for teledermatology. Telemed J E Health. 2016;22(12):981–990. doi: 10.1089/tmj.2016.0137. [DOI] [PubMed] [Google Scholar]
- 95.Rosen AR, Littman-Quinn R, Kovarik CL, Lipoff JB. Landscape of business models in teledermatology. Cutis. 2016;97(4):302–304. [PubMed] [Google Scholar]
- 96.Stevenson P, Finnane AR, Soyer HP. Teledermatology and clinical photography: safeguarding patient privacy and mitigating medico-legal risk. Med J Aust. 2016;204(5):198–200. doi: 10.5694/mja15.00996. [DOI] [PubMed] [Google Scholar]
- 97.Health informatics — Telehealth services — Quality planning guidelines. International Organization for Standardization; 2014. p. 32. [Google Scholar]
- 98.Information technology — Security techniques — Information security management systems — Requirements. Vol ISO/IEC 27001:2013. 2nd ed. International Organization for Standardization; 2013. p. 23. [Google Scholar]
- 99.Finnane A, Curiel-Lewandrowski C, Wimberley G, et al. International Society of Digital Imaging of the Skin (ISDIS) for the International Skin Imaging Collaboration (ISIC) Proposed technical guidelines for the acquisition of clinical images of skin-related conditions. JAMA Dermatol. 2017;153(5):453–457. doi: 10.1001/jamadermatol.2016.6214. [DOI] [PubMed] [Google Scholar]
- 100.Landow SM, Oh DH, Weinstock MA. Teledermatology within the Veterans Health Administration, 2002–2014. Telemed J E Health. 2015;21(10):769–773. doi: 10.1089/tmj.2014.0225. [DOI] [PubMed] [Google Scholar]
- 101.Bobbs M, Bayer M, Frazer T, et al. Building a global teledermatology collaboration. Int J Dermatol. 2016;55(4):446–449. doi: 10.1111/ijd.13223. [DOI] [PubMed] [Google Scholar]
- 102.Abbott LM, Magnusson RS, Gibbs E, Smith SD. Smartphone use in dermatology for clinical photography and consultation: current practice and the law. Australas J Dermatol. 2018;59(2):101–107. doi: 10.1111/ajd.12583. [DOI] [PubMed] [Google Scholar]
- 103.Byamba K, Syed-Abdul S, García-Romero M, et al. Mobile teledermatology for a prompter and more efficient dermatological care in rural Mongolia. Br J Dermatol. 2015;173(1):265–267. doi: 10.1111/bjd.13607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Peart JM, Kovarik C. Direct-to-patient teledermatology practices. J Am Acad Dermatol. 2015;72(5):907–909. doi: 10.1016/j.jaad.2015.01.019. [DOI] [PubMed] [Google Scholar]
- 105.Resneck JS, Jr, Abrouk M, Steuer M, et al. Choice, transparency, coordination, and quality among direct-to-consumer telemedicine websites and apps treating skin disease. JAMA Dermatol. 2016;152(7):768–775. doi: 10.1001/jamadermatol.2016.1774. [DOI] [PubMed] [Google Scholar]
- 106.Fogel AL, Teng J, Sarin KY. Direct-to-consumer teledermatology services for pediatric patients: room for improvement. J Am Acad Dermatol. 2016;75(5):887–888. doi: 10.1016/j.jaad.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 107.Kochmann M, Locatis C. Direct to consumer mobile teledermatology apps: an exploratory study. Telemed J E Health. 2016;22(8):689–693. doi: 10.1089/tmj.2015.0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Spinks J, Janda M, Soyer HP, Whitty JA. Consumer preferences for teledermoscopy screening to detect melanoma early. J Telemed Telecare. 2016;22(1):39–46. doi: 10.1177/1357633X15586701. [DOI] [PubMed] [Google Scholar]
- 109.Stratton D, Loescher LJ. The acceptance of mobile teledermoscopy by primary care nurse practitioners in the state of Arizona. J Am Assoc Nurse Pract. 2016;28(6):287–293. doi: 10.1002/2327-6924.12313. [DOI] [PubMed] [Google Scholar]
- 110.Ngoo A, Finnane A, McMeniman E, Tan JM, Janda M, Soyer HP. Efficacy of smartphone applications in high-risk pigmented lesions. Australas J Dermatol. 2017 doi: 10.1111/ajd.12599. [DOI] [PubMed] [Google Scholar]