Supplemental Digital Content is Available in the Text.
Key Words: CXL Plus, corneal collagen cross-linking, photorefractive keratectomy, keratoconus
Abstract
Purpose:
To evaluate the effectiveness and safety of combined epithelium-off cross-linking (CXL) with photorefractive keratectomy (CXL Plus) for correction of the myopic and astigmatic components of keratoconus.
Methods:
Seventy-nine eyes of 46 patients who underwent CXL Plus were enrolled in this retrospective, multicenter, noncomparative clinical study. Uncorrected distance visual acuity, corrected distance visual acuity, refraction, keratometry, and pachymetry measurements were recorded preoperatively and at 3, 6, 12, and 18 months during follow-up.
Results:
The mean (±SD) preoperative uncorrected distance visual acuity and corrected distance visual acuity were 1.00 ± 0.22 logarithm of the minimum angle of resolution (logMAR) and 0.62 ± 0.38 logMAR, respectively, and improved to 0.71 ± 0.36 logMAR and 0.32 ± 0.18 logMAR postoperatively. The mean k value, mean corneal thickness at the thinnest location, and mean myopic and astigmatic components decreased from 46.58 ± 0.97 D, 473 ± 29 μm, 3.65 ± 1.72 D, and 1.83 ± 0.69 D preoperatively to 43.79 ± 1.17 D, 431 ± 38 μm, 1.02 ± 0.78 D, and 1.15 ± 0.26 D, respectively, during follow-up. Eleven eyes had delayed epithelial healing, 2 had stromal opacities, 1 had primary herpes simplex keratitis, and 5 showed progression of keratoconus.
Conclusions:
CXL Plus improved the refractive status of keratoconus during 18 months of follow-up, despite its potential early postoperative complications of delayed epithelial healing and corneal haze. CXL Plus reduced the myopic component more than the astigmatic component of keratoconus. However, the safety and stability of the procedure were offset by longer-term postoperative complications and a high rate of postoperative progression of keratoconus.
Keratoconus is a progressive noninflammatory corneal disorder with both myopic and astigmatic components. Many parameters have been used to define the progression of keratoconus, particularly the anterior and posterior k readings, central corneal thickness at the thinnest location, and back surface elevations. Continued progression of at least 2 of the above parameters indicates progression of keratoconus.1–3
It is now widely agreed that corneal collagen cross-linking (CXL) is the only effective treatment for keratoconus because of its ability to halt the pathological progression of the disease. It has also been suggested that standard CXL may have an additional but unpredictable refractive effect.4–6
CXL Plus4 combines 2 surgical procedures to treat keratoconus. The main procedure is CXL, which is combined with another refractive procedure, usually topography-guided photorefractive keratectomy (PRK) or intracorneal ring segments, either in the same session or sequentially. Other refractive procedures that may be combined with CXL, usually sequentially, are phakic intraocular lens implantation and clear lens extraction or refractive lens surgery. CXL Plus includes the mandatory CXL procedure to halt the pathological progression of keratoconus and another refractive procedure to correct the refractive status of the affected eye.5–7 The Athens protocol was designed to treat eyes with progressive keratoconus and a highly irregular anterior corneal surface and combines topography-guided PRK and CXL. Using this protocol, up to 50 μm of the anterior corneal surface is ablated to correct corneal surface abnormalities and is immediately followed by CXL in the same session.8–10 Other protocols have also been developed.
Our aim was to evaluate the safety, effectiveness, and stability of standard non-topography-guided PRK combined with accelerated pulsed epithelium-off CXL for correction of up to 5 D of myopia and/or astigmatism during 18 months of follow-up in patients with keratoconus.
MATERIALS AND METHODS
Patients
This retrospective, multicenter, noncomparative study was performed at 7 sites in Egypt, namely, Sohag University Hospital, Alexandria University Hospital, Minia University Hospital, Suez Canal University Hospital, Tanta University Hospital, Ain Shams University Hospital, and Banha University Hospital. The study protocol was approved by the ethical committee at Sohag University Hospital and adhered to the principles of the Declaration of Helsinki. Written consent was provided by all patients before surgery.
Seventy-nine eyes of 46 patients with grade 1 keratoconus were included in the study. The diagnosis was made using the Amsler–Krumeich classification, which is characterized by mean central k readings <48 D with myopia, induced astigmatism, or both <5.00 D, and corneal thickness >400 μm. All 79 eyes underwent CXL Plus, which included a combination of simultaneous standard non-topography-guided PRK and accelerated epithelium-off CXL (pulsed mode, 7.2 J/cm2 total energy according to the Avedro nomogram; Avedro, Waltham, MA) in the same session. The data were collected from the patients' medical records.
Preoperative Data
The measurement devices used in the study were the Sirius topographer (CSO Italia, Firenze, Italy), VISX STAR S4 IR (Abbott Laboratories, Abbott Park, IL), and the KXL system (Avedro Inc, Waltham, MA).
All eyes included in the study met the following inclusion criteria: treatment provided by one of the authors, grade 1 keratoconus (Amsler–Krumeich classification); non-topography-guided PRK performed to correct up to 5 D of myopia and/or astigmatism only if the corneal thickness allowed; and a postoperative corneal thickness of at least 400 μm; treatment with the VISX STAR S4 IR and KXL system; and follow-up for 18 months.
The preoperative data collected for these 46 eyes included uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), subjective refraction, spherical equivalent (SE), pachymetry, and keratometry measurements for both anterior and posterior corneal surfaces on preoperative examination by corneal topography. The preoperative attempted SE refraction varied from one patient to another according to the available corneal thickness to be ablated to completely correct most or all the refractive error. However, our main aim was to achieve a postoperative refraction within ±1 D spherical equivalent.
CXL Plus
CXL Plus included PRK followed by accelerated epithelium-off CXL in the same session. PRK was used as a refractive treatment to correct the myopic and/or astigmatic components of keratoconus, and epithelium-off CXL was used to halt the progression of keratoconus.
The first step was to perform standard non-topography-guided PRK using the conventional nomogram (VISX S4; Maloney Vision Institute, Los Angeles, CA). Non-topography-guided PRK was performed to completely correct the refractive error. This is because topography-guided or custom PRK using iDesign (Abbott) can be adjusted to correct only 2.5 D of sphere of the associated refractive error according to the manufacturer profile, whereas our study aimed to correct up to 5 D of sphere and/or cylinder using non-topography-guided PRK.
Topical anesthetic eye drops (Benox, benoxinate hydrochloride 0.4% sterile ophthalmic solution; Egyptian International Pharmaceutical Industries Co, 10th of Ramadan, Egypt) were instilled into the patient's eye 10 minutes before surgery. The patient was instructed to fixate on the excimer laser beam, thereby allowing centration of the reticle over the entrance pupil onto the cornea. The epithelium was removed within a 6-mm ablation zone. PRK was performed by stromal ablation aiming to correct up to 5 D of myopia and/or astigmatism and to preserve a corneal thickness of at least 400 μm at the thinnest location postoperatively. A sponge soaked in 0.02% mitomycin C solution was placed onto the deepithelialized corneal surface for 20 seconds to decrease postoperative corneal haze. The anterior corneal surface was then carefully washed in balanced salt solution to remove any remaining mitomycin C solution from the corneal surface.
The second step of the CXL Plus procedure was an accelerated epithelium-off CXL procedure using the Avedro nomogram with the Avedro KXL CXL system. First, a blunt hockey knife was used to widen the 6-mm ablated epithelial zone to an 8-mm deepithelialized corneal zone. Riboflavin (VibeX Rapid; Avedro Inc) was applied to the cornea at 2-minute intervals for a total soaking time of 10 minutes. The aim of accelerated epithelium-off CXL was to deliver a total energy of 7.2 J/cm2 with a power of 30 mW/cm2. The pulsed ultraviolet mode (1 second on and 1 second off) was used to achieve a total treatment time of 8 minutes; allowing 10 minutes of soaking time, the procedure took 18 minutes to complete. At the end of surgery, antibiotic eye drops (Zymar, gatifloxacin 0.3%; Allergan, Inc, Jersey City, NJ) were instilled into the eye, followed by application of a bandage contact lens (CooperVision, The Cooper Companies, Inc, Pleasanton, CA) to the cornea.
Postoperative Care and Follow-up
All patients were prescribed antibiotic eye drops (gatifloxacin 0.3%), steroid eye drops (Pred Forte, prednisolone acetate 1%; Allergan, Inc), and lubricant eye drops (carboxymethylcellulose; Alcon Laboratories, College Station, TX) to be used postoperatively for 4 weeks. All patients were instructed to instill the eye drops every 2 hours on the first postoperative day, 5 times daily in the first postoperative week, 4 times daily in the second postoperative week, 3 times daily in the third postoperative week, and twice daily in the fourth postoperative week.
All eyes were examined twice during the first postoperative week, with close observation and slit-lamp examination of the cornea until complete healing of the epithelium was achieved, after which the bandage contact lens was removed from the patient's eye. The follow-up visits were weekly in the first postoperative month, and at 3, 6, 12, and 18 months thereafter.
During follow-up, the postoperative UDVA, CDVA, subjective refraction, spherical equivalent, pachymetry, and keratometry data were collected by topographic examination of the anterior and posterior corneal surfaces. Postoperative corneal haze was graded from 0 to +5 using the scoring system on slit-lamp microscopy after photoablation (0, clear cornea; +1, mild haze not affecting refraction; +2, moderate haze with difficult refraction; +3, marked haze preventing refraction; +4, unclear iris details; and +5, inability to view the anterior chamber details).11
Statistical Analysis
Statistical analysis was performed using IBM SPSS for Windows version 22 software (IBM Corp, Armonk, NY). Quantitative data are shown as the median and range or mean ± standard deviation. Qualitative data are presented as the number and percentage. The Wilcoxon test was used to analyze nonnormally distributed data, and the paired-samples t test was used for normally distributed data. Postoperative results were considered significant at the 5% level.
RESULTS
The study included 79 eyes of 46 patients [27 males (58.7%) and 19 females (41.3%); mean age 20.7 ± 6.8 (range 13–30) years].
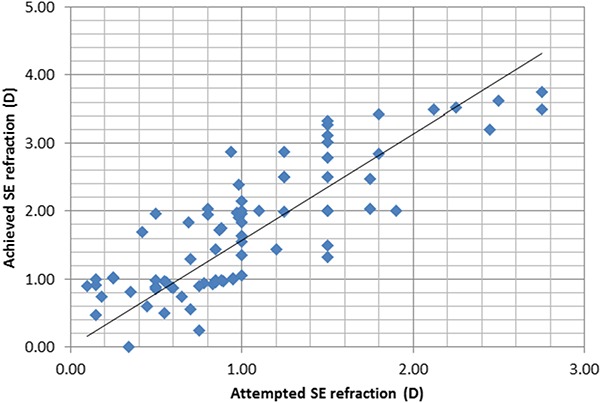
Corneal Topographic Outcomes
After CXL Plus, there was a decrease in mean k (k1, k2, and k average) readings. There was a significant decrease in the mean k average reading from 46.58 ± 0.97 D to 43.79 ± 1.17 D postoperatively (P < 0.001). There was a significant postoperative reduction in mean k1 and k2 readings of up to 3 D from 44.75 ± 1.18 D and 48.28 ± 0.66 D to 42.14 ± 1.38 D and 45.91 ± 1.05 D, respectively (both P < 0.05). The preoperative and postoperative data at the end of 18 months of follow-up are summarized in Table 1.
TABLE 1.
Summary of the Corneal Topographic Parameters of the Study Eyes After 18 Months of Follow-up
Visual and Refractive Outcomes
Mean UDVA and CDVA values improved markedly postoperatively from 1.00 ± 0.22 logarithm of the minimum angle of resolution (logMAR) and 0.62 ± 0.38 logMAR to 0.71 ± 0.36 logMAR and 0.32 ± 0.18 logMAR, respectively (both P < 0.05). The mean myopic component was markedly decreased from 3.65 ± 1.72 D to 1.02 ± 0.78 D postoperatively (P < 0.001) and the mean astigmatic component from 1.83 ± 0.69 D to 1.15 ± 0.26 D postoperatively (P < 0.05). The mean spherical equivalent was also greatly reduced from −4.47 ± 1.98 D to −1.72 ± 0.93 D postoperatively (P < 0.001). By 18 months postoperatively, there was a highly statistically significant reduction in mean myopic correction of 2.93 ± 0.65 D (P < 0.001); however, mean postoperative astigmatic correction at this time was only 0.86 ± 0.34 D, albeit being statistically significant (P < 0.05). The visual and refractive outcomes in the study eyes after 18 months of follow-up are shown in Table 2.
TABLE 2.
Visual and Refractive Outcomes in the Study Eyes After 18 Months of Follow-up
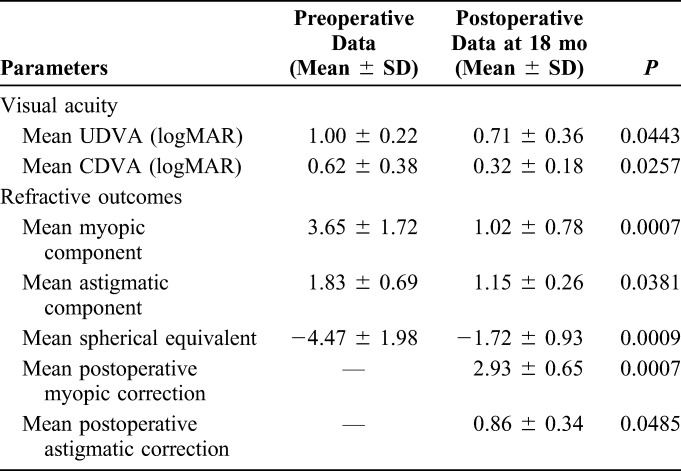
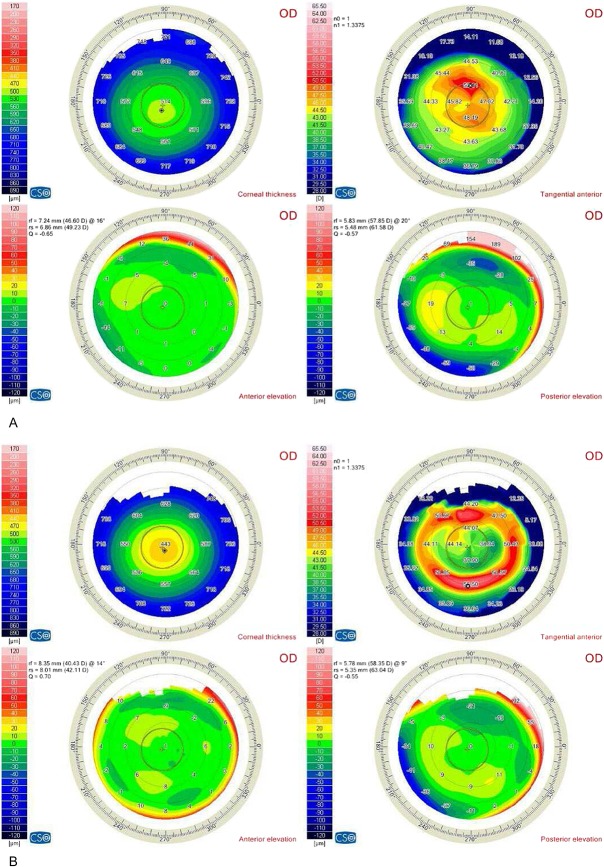
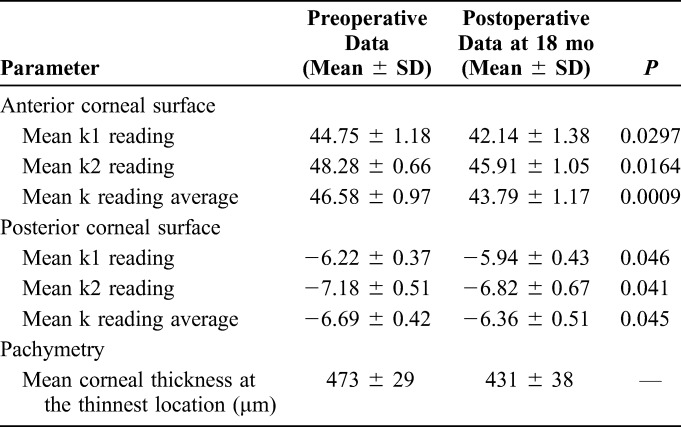
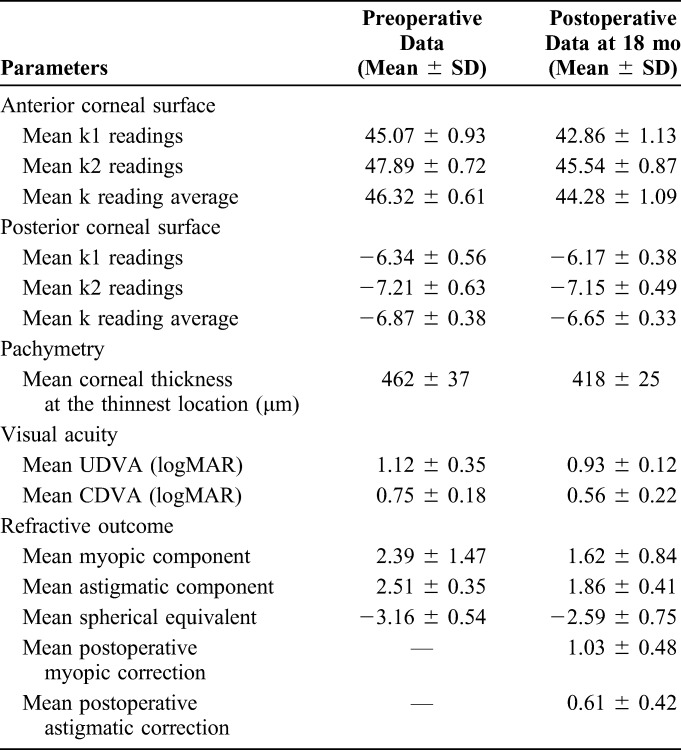
Table 3 shows a representative example of the postoperative results of the right eye of a 24-year-old woman with grade 1 keratoconus (Amsler–Krumeich classification) who underwent CXL Plus. Figures 1A, 1B show the preoperative and postoperative corneal topography details of this patient. Figure 2 shows a scatterplot of attempted versus achieved SE refraction. Thirty-two eyes (40.5%) had postoperative refraction of ±1 D SE, thus achieving the preoperative attempted SE refraction.
TABLE 3.
Preoperative and 18-Month Postoperative Data of the Right Eye of One Female Patient Who Underwent CXL Plus
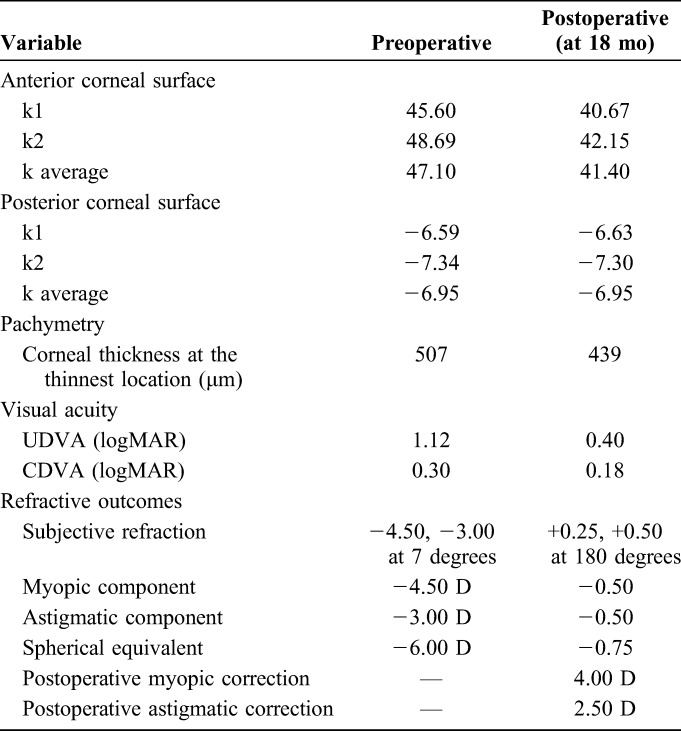
FIGURE 1.
Preoperative (A) and postoperative (B) corneal topographic images of a 24-year-old woman with grade 1 keratoconus.
FIGURE 2.
Scatter plot of attempted versus achieved SE refraction at 18 months of follow-up.
Early and Late Complications
The postoperative complications in this study were classified as early or late. Early postoperative complications included those that appeared within the first postoperative week and are summarized in Supplemental Digital Content 1 (see Supplemental Table, http://links.lww.com/ICO/A682). Fifty-seven eyes (72.2%) had early postoperative pain, photophobia, lacrimation, and/or foreign body sensation. Most of these complications were related to removal of the epithelium. Benoxinate eye drops 3 times daily on the first postoperative day were prescribed to alleviate these complaints. Systemic analgesics were also prescribed, and patients were advised to wear sunglasses. Complete healing of the corneal epithelium occurred within 2 to 3 days postoperatively in all cases.
Epithelial healing was delayed in 11 eyes (13.9%). Corticosteroid eye drops were replaced by nepafenac 0.1% eye drops (Alcon Laboratories) 3 times daily in these patients. Epithelial healing was noted in 9 of the 11 eyes at the end of the first postoperative week; however, they developed corneal haze. The remaining 2 eyes developed further late complications, that is, primary herpes simplex keratitis (n = 1) and persistent epithelial defect (n = 1).
Corneal haze was recorded in 19 eyes (24.1%), including the 9 eyes with delayed epithelial healing in which corneal haze developed from the second postoperative week onwards. Frequent instillation of steroid eye drops with sodium chloride 5% was prescribed. Lubricant eye drops (Refresh Plus) were also added. Seventeen eyes (score +1 or +2) recovered completely within 2 weeks after surgery, whereas 2 eyes (score +3) developed central corneal opacity.
Late postoperative complications were defined as those that appeared or progressed after the first postoperative week. Supplemental Digital Content 2 (see Supplemental, Table, http://links.lww.com/ICO/A683) summarizes the late postoperative complications. Primary herpes simplex keratitis was recorded in one eye (1.3%). There was no known history of herpes simplex keratitis in this patient. Furthermore, there were no recorded postoperative symptoms of common cold, influenza, or an upper respiratory tract disorder. However, the instillation of steroid eye drops was stopped and eye ointment (Zovirax, acyclovir 3%; GlaxoSmithKline, Brentford, United Kingdom) was used 5 times daily. This eye showed complete healing without sequelae at the end of the first postoperative month.
A persistent epithelial defect was recorded in one eye (1.3%). Both steroid and nonsteroidal antiinflammatory eye drops were stopped. Supportive care was initiated with frequent artificial tears and lubricants. Sodium hyaluronate 0.15% eye drops (Hyabak, Théa Laboratories, Clermont-Ferrand, France) and Refresh Plus lubricant eye drops were prescribed. Despite this supportive care, complete epithelial healing was not achieved at 6 weeks postoperatively; the patient still had a hazy cornea with central corneal scarring at that time, which affected the postoperative visual outcome.
Central corneal stromal opacities were recorded in 2 eyes (2.5%). Both eyes were in the delayed epithelialization group in the first postoperative week and thereafter developed corneal haze, which unfortunately resulted in permanent central corneal stromal opacity. Frequent instillation of steroid and sodium chloride 5% eye drops was prescribed. Carboxymethylcellulose sodium solution 0.5% lubricant eye drops were also prescribed. Both eyes had persistent central opacities that had a marked effect on visual acuity. The CDVA was much lower postoperatively than preoperatively, decreasing from 0.30 to 1.00 logMAR in one eye and from 0.60 to 1.22 logMAR in the other eye. The visual outcomes in the study eyes with late postoperative complications are summarized in Supplemental Digital Content 3 (see Supplemental, Table, http://links.lww.com/ICO/A684).
Progression of keratoconus was documented in 5 eyes (6.3%), all of which underwent a conventional 30-minute epithelium-off CXL procedure using the Opto XLink CXL system (Opto Global Pty Ltd, Adelaide, Australia). The standard Dresden protocol was used to irradiate the cornea with ultraviolet A light. An 8-mm zone marker was used to mark the area of the cornea to be deepithelialized. A blunt hockey knife was used to remove the epithelium. Riboflavin 0.1% eye drops (Ricrolin Sooft SpA, Montegiorgio, Italy) were applied at 3-minute intervals for 30 minutes. The aim of retreatment was to deliver a 5.37-J/cm2 dose for 30 minutes (intensity 2.98 mW/cm2 and power 1.50 mW). Postoperative treatment included topical eye drops (gatifloxacin 0.3%, prednisolone acetate 1%, and sodium hyaluronate 0.15%) 5 times daily in the first postoperative week, which were tapered gradually to twice daily in the fourth postoperative week. The 5 retreated eyes showed good stability during 18 months of follow-up. Table 4 shows the topographic, visual, and refractive outcomes in these 5 eyes.
TABLE 4.
Topographic, Visual, and Refractive Outcomes for Five Eyes Retreated With CXL
The postoperative visual outcome in 3 eyes (3.8%) was worse than their preoperative state. Two eyes (2.5%) were complicated by delayed postoperative epithelial healing that led to postoperative central corneal opacities, and the third eye was complicated by a persistent epithelial defect that also led to central corneal opacity.
DISCUSSION
Kanellopoulos and colleagues8–10 designed the Athens protocol to correct approximately 2.5 to 3 D and to abolish the anterior corneal surface irregularities by ablating up to 50 μm from the anterior corneal surface in advanced keratoconus. In contrast, our study focused on grade 1 keratoconus and attempted to correct up to 5 D of myopia and/or astigmatism provided that a minimum corneal thickness of 400 μm at the thinnest location would remain postoperatively. The aim was to reduce the optical zone in an attempt to correct the refractive error completely.
The Athens protocol uses topography-guided PRK (Allegretto Wave Eye-Q, 400 Hz, Alcon Laboratories, Fort Worth, TX), whereas our study used standard non-topography-guided PRK (VISX STAR S4 IR). The Athens protocol restricts laser ablation to a maximum of 50 μm of corneal stroma, treating up to 1 D of the myopic component and up to 2.5 D of the astigmatic component of keratoconus.8–10 In contrast, our study allowed ablation of all possible corneal stromal tissue provided that at least 400 μm of the corneal thickness would remain postoperatively. The Athens protocol was designed for eyes with advanced keratoconus, whereas our study evaluated a protocol for only grade 1 keratoconus and allowed for ablation of more than 50 μm of the corneal stroma. Furthermore, our study was able to treat up to 5 D of myopic and astigmatic components. Up to 4.5 D of myopia and up to 1.5 D of astigmatism were corrected in our study eyes.
Kanellopoulos and colleagues8–10 reported almost no complications using the Athens protocol, whereas we encountered many complications using a simultaneous combination of standard non-topography-guided PRK and CXL. In our study, 11 eyes had delayed epithelial healing, 2 had stromal opacities, 1 had primary herpes simplex keratitis, and 5 showed progression of keratoconus.
In a prospective comparative study of 62 eyes with keratoconus, Abou Samra et al12 reported good results using combined wavefront-guided PRK and CXL both in the same session and in separate sessions. They performed combined wavefront-guided PRK and CXL in the same session in 30 eyes and wavefront-guided PRK first and then CXL 6 months later in 32 eyes. They concluded that wavefront-guided PRK combined with accelerated CXL safely and effectively improved visual outcomes and reported similarities between both groups. In our noncomparative study, only one type of procedure was evaluated, and the follow-up duration was 18 months.
Bor'i13 compared 34 eyes with early keratoconus that underwent topography-guided PRK with CXL on the same day (n = 17) or topography-guided PRK first and CXL 6 months later (n = 17). They concluded that there was no significant postoperative difference in the mean spherical equivalent between both groups (−1.25 ± 0.35 D vs. −1.5 ± 0.21 D). However, we found a significant improvement in the postoperative mean spherical equivalent from −4.47 ± 1.98 D to −1.72 ± 0.93 D (P < 0.001) in eyes that underwent CXL Plus.
Shaheen et al14 performed wavefront-guided PRK using the VISX STAR S4 IR excimer laser with the iDesign system in 34 eyes with grade I or II keratoconus (Amsler–Krumeich classification) 1 year after CXL. They reported excellent postoperative safety and efficacy results during 12 months of follow-up. They reported significant postoperative improvements in UDVA and CDVA of 1.58 ± 1.11 and 1.96 ± 1.52 logMAR, respectively (P < 0.001); in contrast, we found postoperative improvements of 0.71 ± 0.36 logMAR and 0.32 ± 0.18 logMAR, respectively. Correction of the myopic component of keratoconus was excellent in our study and reached 2.93 ± 0.65 (P < 0.001), which is consistent with the significant reduction in the manifest sphere (P < 0.001) reported by Shaheen et al.
Müller and Lange15 reported reasonable postoperative results for CXL combined with topography-guided PRK in 9 eyes with keratoconus or post-LASIK ectasia. There was marked improvement in uncorrected and best-corrected visual acuity (P < 0.05) postoperatively. However, our study did not include any eyes with post-LASIK ectasia.
Fadlallah et al16 performed a retrospective study that included 140 eyes with grade 1 or 2 keratoconus, all of which underwent combined non-topography-guided PRK and CXL in the same session and were followed up for 2 years. They reported significant improvements, with the mean spherical equivalent reaching −0.42 ± 0.60 D (P < 0.001).
Sakla et al,17 Altroudi et al,18 and Kontadakis et al19 reported similar results, in which they found combined CXL and topography-guided PRK to be a safe and effective procedure for treating and correcting refractive errors of keratoconus. Dirani et al20 used non-topography-guided PRK to correct refractive errors in eyes with keratoconic corneas that had previously undergone CXL and implantation of intracorneal ring segments and concluded that PRK was a safe and effective procedure. Knezović et al21 reported similar results.17–21
Koller et al22 reported a 7.6% failure rate, and 6.3% of cases in our study showed postoperative progression of keratoconus after CXL. Furthermore, Koller et al reported that 2.8% of their cases were complicated by scars in the central stroma; similarly, we found a postoperative central corneal stromal opacity rate of 2.5%. Sterile infiltrates were found in 7.6% of cases in their study but not in any of the patients in our study.
Güell et al23 reported on a patient who presented with late-onset corneal scarring after combined PRK and CXL. Prakash et al24 reported a similar case of persistent stromal scarring after simultaneous PRK and CXL. The postoperative central corneal stromal opacities found in both these cases were similar to those in 2 of our patients. Unfortunately, these opacities greatly reduced the postoperative visual acuity to values much lower than the preoperative CDVA.
There are reports of eyes complicated with infectious keratitis after combined PRK and CXL. Yuksel et al25 and Kymionis et al26 reported cases in which only one eye was complicated with herpes simplex keratitis. The postoperative BCVA was 20/25 in both reports. Their findings are very similar to ours, in that only one eye (1.3%) in our study was complicated with herpes simplex keratitis and healed completely without any sequelae; the postoperative CDVA in this case was 0.22 logMAR. Other studies have reported postoperative infectious keratitis caused by Acanthamoeba, Pseudomonas aeruginosa, Staphylococci, and Streptococci spp.27–29
The amount of tissue ablated during CXL Plus varies from report to report. Kanellopoulos and colleagues8–10 recommended ablation of 50 μm of corneal thickness in their Athens protocol. Other authors, such as Shaheen et al,14 ablated up to 15% of the total corneal thickness at the thinnest location when PRK was performed 1 year after CXL. In our study, we ablated up to 70 μm (13.2%) of tissue to correct up to 5 D of myopia and/or astigmatism.
Another important difference between these 2 studies was that Shaheen et al14 performed customized PRK 1 year after conventional epithelium-off CXL. This raises an important issue, given that standard CXL may have an additional refractive effect. In theory, conventional epithelium-off CXL would flatten the cornea and reduce the corneal thickness over a 1-year period. Therefore, in the study by Shaheen et al,14 the eyes that had undergone conventional epithelium-off CXL 1 year before customized PRK would be expected to have a flatter corneal surface, a reduction in the original myopic component of keratoconus, and decreased corneal thickness, meaning that less corneal tissue would need to be ablated by customized PRK. However, Shaheen et al14 did not provide details regarding the original visual, refractive, or topographic parameters of their study eyes before conventional 30-minute epithelium-off CXL.
Our study recorded 5 (6.3%) cases of progression of postoperative keratoconus. This very high rate can be attributed to 2 main factors. First, accelerated CXL is less effective than standard CXL in halting the progression of keratoconus; second, PRK decreases the corneal thickness, weakening the cornea. Thus, the high rate of postoperative progression of keratoconus could be explained by the fact that accelerated CXL did not maintain the stability of the thinned cornea.
In conclusion, despite the small risk of early postoperative complications, CXL Plus was an effective way of improving refractive status in eyes with keratoconus during 18 months of follow-up. However, CXL Plus was more effective in correcting the myopic component of keratoconus than the astigmatic component. Most complications occurring after CXL Plus could be attributed to removal of the epithelium. Unfortunately, CXL Plus cannot be regarded as a completely safe procedure. Moreover, there was a high rate of progression of keratoconus postoperatively. Further prospective studies using standard CXL instead of accelerated CXL are needed to evaluate the stability, efficacy, and safety of CXL Plus.
Supplementary Material
ACKNOWLEDGMENTS
The authors are grateful for the help and support of Dr Islam Awny, Tamer Badawy, Ahmed Saber, Mr. El Khominy Omar, Mr. Ammar Omar, Mrs. Sarah Saleem, and Miss Asmaa Hashem.
Footnotes
The authors have no funding or conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.corneajrnl.com).
REFERENCES
- 1.Brown S, Simmasalam R, Antonova N, et al. Progression in keratoconus and the effect of corneal cross-linking on progression. Eye Contact Lens. 2014;40:331–338. [DOI] [PubMed] [Google Scholar]
- 2.Vinciguerra P, Piscopo R, Camesasca F, et al. Progression in keratoconus. Int J Keratoconus Ectatic Corneal Dis. 2016;5:21–31. [Google Scholar]
- 3.Joshua K, Michael W, Borgstrom M. Assessing progression of keratoconus: novel tomographic determinants. Eye Vis (Lond). 2016;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kymionis GD, Grentzelos MA, Portaliou DM, et al. Corneal collagen cross-linking (CXL) combined with refractive procedures for the treatment of corneal ectatic disorders: CXL Plus. J Refract Surg. 2014;30:566–576. [DOI] [PubMed] [Google Scholar]
- 5.Saleem MIH, Elzembely HAI, AboZaid MA, et al. Three-year outcomes of cross-linking PLUS (combined cross-linking with femtosecond laser intracorneal ring segments implantation) for management of keratoconus. J Ophthalmol. 2018;2018:6907573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spoerl E, Hafezi F, Bradley J. Corneal Collagen Cross-linking. Vol 20 Thorofare, NJ: SLACK Incorporated; 2013:139–142. [Google Scholar]
- 7.De Bernardo M, Capasso L, Lanza M, et al. Long-term results of corneal collagen crosslinking for progressive keratoconus. J Optom. 2015;8:180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanellopoulos J, Asimellis G. Keratoconus management: long-term stability of topography-guided normalization combined with high-fluence CXL stabilization (the Athens Protocol). J Refract Surg. 2014;30:88–93. [DOI] [PubMed] [Google Scholar]
- 9.Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26:891–895. [DOI] [PubMed] [Google Scholar]
- 10.Kanellopoulos J. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25:S812–S818. [DOI] [PubMed] [Google Scholar]
- 11.Andrade HA, McDonald MB, Liu JC, et al. Evaluation of an opacity lensometer for determining corneal clarity following excimer laser photoablation. Refract Corneal Surg. 1990;6:346–351. [PubMed] [Google Scholar]
- 12.Abou Samra WA, El Emam DS, Farag RK, et al. Simultaneous versus sequential accelerated corneal collagen cross-linking and wave front guided PRK for treatment of keratoconus: objective and subjective evaluation. J Ophthalmol. 2016;2016:2927546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bor'i A. Simultaneous versus sequential photorefractive keratectomy and cross-linking for the management of early keratoconus. Delta J Ophthalmol. 2016;17:123–127. [Google Scholar]
- 14.Shaheen MS, Shalaby Bardan A, Piñero DP. Wave front-guided photorefractive keratectomy using a high-resolution aberrometer after corneal collagen cross-linking in keratoconus. Cornea. 2016;35:946–953. [DOI] [PubMed] [Google Scholar]
- 15.Müller T, Lange A. Topography-guided PRK and crosslinking in eyes with keratoconus and post-LASIK ectasia. Klin Monbl Augenheilkd. 2017;234:451–454. [DOI] [PubMed] [Google Scholar]
- 16.Fadlallah A, Dirani A, Chelala E, et al. Non-topography-guided PRK combined with CXL for the correction of refractive errors in patients with early stage keratoconus. J Refract Surg. 2014;30:688–693. [DOI] [PubMed] [Google Scholar]
- 17.Sakla H, Altroudi W, Munoz G, et al. Simultaneous topography-guided photorefractive keratectomy and accelerated corneal collagen cross-linking for keratoconus. Cornea. 2016;35:941–945. [DOI] [PubMed] [Google Scholar]
- 18.Sakla H, Altroudi W, Muñoz G, et al. Simultaneous topography-guided partial photorefractive keratectomy and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg. 2014;40:1430–1438. [DOI] [PubMed] [Google Scholar]
- 19.Kontadakis G, Kankariya V, Tsoulnaras K, et al. Long-term comparison of simultaneous topography-guided photorefractive keratectomy followed by corneal cross-linking versus corneal cross-linking alone. Ophthalmology. 2016;123:974–983. [DOI] [PubMed] [Google Scholar]
- 20.Dirani A, Fadlallah A, Syed Z, et al. Non-topography-guided photorefractive keratectomy for the correction of residual mild refractive errors after ICRS implantation and CXL in keratoconus. J Refract Surg. 2014;30:266–271. [DOI] [PubMed] [Google Scholar]
- 21.Knezović I, Višnjić M, Raguž H. Partial topography-guided photorefractive keratectomy followed by corneal cross linking in the management of progressive keratoconus: our initial ten-month results. Acta Clin Croat. 2015;54:193–200. [PubMed] [Google Scholar]
- 22.Koller T, Mrochen M, Seiler T. Complication and failure rates after corneal crosslinking. J Cataract Refract Surg. 2009;35:1358–1362. [DOI] [PubMed] [Google Scholar]
- 23.Güell JL, Verdaguer P, Elies D, et al. Late onset of a persistent, deep stromal scarring after PRK and corneal cross-linking in a patient with forme fruste keratoconus. J Refract Surg. 2014;30:286–288. [DOI] [PubMed] [Google Scholar]
- 24.Prakash G, Jain M, Shakunthala A, et al. Persistent stromal scar after PRK and CXL: different preoperative findings, similar complication. J Refract Surg. 2015;31:211–212. [DOI] [PubMed] [Google Scholar]
- 25.Yuksel N, Bilgihan K, Hondur A, et al. Herpetic keratitis after corneal collagen cross-linking with riboflavin and ultraviolet-A for progressive keratoconus. Int Ophthalmol. 2011;31:513–515. [DOI] [PubMed] [Google Scholar]
- 26.Kymionis G, Portaliou D, Bouzoukis D, et al. Herpetic keratitis with iritis after corneal crosslinking with riboflavin and ultraviolet A for keratoconus. J Cataract Refract Surg. 2007;33:1982–1984. [DOI] [PubMed] [Google Scholar]
- 27.Pollhammer M, Cursiefen C. Bacterial keratitis early after corneal crosslinking with riboflavin and ultraviolet-A. J Cataract Refract Surg. 2009;35:588–589. [DOI] [PubMed] [Google Scholar]
- 28.Juan J, Alberto A, Aliój, et al. Microbial keratitis after corneal collagen crosslinking. J Cataract Refract Surg. 2009;36:1138–1140. [DOI] [PubMed] [Google Scholar]
- 29.Rama P, Di Matteo F, Matuska S, et al. Acanthamoeba keratitis with perforation after corneal crosslinking and bandage contact lens use. J Cataract Refract Surg. 2009;35:788–791. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.