Abstract
Initial assessment of acid-base status is usually based on measurement of total CO2 concentration ([TCO2]) in venous blood, a surrogate for [HCO3−]. Previously, we posited that the reference limits of serum [TCO2] in current use are too wide. Based on studies on the acid-base composition of normal subjects, we suggested that the reference limits of serum [TCO2] at sea level be set at 23-30 mEq/L. To validate this proposal, we queried the UCLA's Integrated Clinical and Research Data Repository (xDR), a database containing information on 4.5 million patients seen at UCLA from 2006 to the present. Criteria for inclusion included adults (18-40 years of age), who were free of disorders that could affect acid-base balance, were not taking medications that could affect acid-base balance, and were seen for a routine medical examination or immunization in the outpatient setting. Twenty-eight thousand four hundred eighty individuals met the inclusion criteria (52% female and 48 % male) with a mean age of 28.9 ± 5.1 years. Mean serum [TCO2] was slightly higher in males than females, 26.6 ± 2.16 mEq/L vs 25.0 ± 2.11 mEq/L (p < 0.05). Ninety-one percent of patient values laid within the proposed 23-30 mEq/L range and 61.7% were within the 24-27 mEq/L range. These findings validate our proposal that the reference range of serum [TCO2] in venous blood at sea level be narrowed to 23-30 mEq/L. Subjects with serum [TCO2] outside this range might require assessment with a venous blood gas to exclude the presence of clinically important acid-base disorders.
Keywords: serum [TCO2], serum [HCO3−], acid-base disorders, acid-base balance
Introduction
Disorders of acid-base balance can adversely affect the clinical outcome and can also point to the presence of an underlying disease1. Therefore, it is important to assess whether the acid-base status of a patient is normal or abnormal, and if the latter, to define the precise nature of the acid-base disorder(s) present. Such assessment requires reliable determination of pH, PCO2, and [HCO3−] in arterial or venous blood. However, in clinical practice, determination of these acid-base parameters is not routinely obtained. Rather, serum total CO2 concentration ([TCO2]) in venous blood, a surrogate for [HCO3−], is measured and used as a screening tool for acid-base abnormalities2. The underlying rationale is that both metabolic and respiratory disorders (the latter by virtue of the secondary responses of [HCO3−] to changes in PCO2) are associated with abnormalities in [HCO3−]2;3. Obviously, optimal use of serum [TCO2] as a screening tool for acid-base disorders rests with a rigorous definition of its reference range.
We have long been concerned about the inordinately wide limits of the reference range for serum [TCO2] reported by clinical laboratories (commonly with a span of 10-13 mEq/L) and the associated risk that values residing within the lower or upper end of this expansive range might be masking the presence of a cardinal acid-base disorder. In a recent publication4, we first derived the expected reference range of serum [TCO2] in venous blood in adults at sea level by analyzing carefully conducted studies on acid-base composition of normal subjects. We then compared this range to that reported by the clinical laboratories of 64 hospitals in the United States and 2 large commercial clinical laboratories, as well as the reference range endorsed by the American Association of Clinical Chemistry and that listed in the Tietz Textbook of Clinical Chemistry and Molecular Diagnostics5, the major clinical chemistry textbook.
The expected reference range of serum [TCO2] in venous blood formulated by us was 23-30 mEq/L (a span of 8 mEq/L) and was closely approximated by that cited by the American Association of Clinical Chemistry6 and the Tietz Textbook of Clinical Chemistry and Molecular Diagnostics5(23-29 mEq/L, a span of 7 mEq/L). In sharp contrast, there was marked variability in the reference range among clinical laboratories, with values at the lower limit varying from 18 mEq/L to 25 mEq/L, and values at the upper limit varying from 26 mEq/L to 35 mEq/L.
We argued that the reference range for serum [TCO2] reported by many clinical laboratories was too wide and encompasses values both at the lower and the upper end that could be consistent with a cardinal acid-base disorder. We therefore suggested that these limits be reconsidered and that the reference range of serum [TCO2] be narrowed to 23-30 mEq/L.
To provide external validation of the proposed more limited reference range of serum [TCO2] in venous blood, in the present study we queried a large data repository for serum [TCO2] values of apparently healthy younger adults.
Materials and Methods
Patient Selection and Data Sources
We examined values for serum [TCO2] of patients selected from the Integrated Clinical and Research Data Repository (xDR) of the University of California at Los Angeles (UCLA). This database contains records of approximately 4.5 million patients cared for at the UCLA’s hospitals and clinics between 2006 and the present. Information available includes patient demographics, diagnosis and procedure codes (ICD-9 or ICD-10 codes, and CPT codes), laboratory tests, and medications. The sources of information are de-identified datasets that are extracted from the clinical data warehouse, transformed into a common data representation, and stored in a separate, dedicated data repository. De-identification of the patient information is accomplished using recognized best practices. Serum [TCO2] is measured with the enzymatic method adapted for the autoanalyzer. The reference range of serum [TCO2] in the measuring clinical laboratories is 20-30 mEq/L (a span of 11 mEq/L).
Inclusion criteria were as follows: 1. Adults 18-40 years of age seen as outpatients, whose encounter information indicated they were seen for a general adult medical examination without abnormal findings, a routine general medical examination at a healthcare facility, or for routine immunization. 2. Absence of kidney disease (chronic kidney disease, acute kidney injury, or renal tubular acidosis), pulmonary disease, heart failure, liver disease, cancer (other than localized disease), diabetes mellitus, gastrointestinal disease, vomiting, diarrhea, or pregnancy, each on the basis of absence of the corresponding ICD-9 or ICD-10 codes. 3. Patients should not be taking medications that could affect acid-base balance, such as diuretics, base-containing substances (including salts of bicarbonate, citrate, acetate, or carbonate), converting enzyme inhibitors or angiotensin receptor blockers, carbonic anhydrase inhibitors, or steroids. Only the initial value for serum [TCO2] was included for each eligible patient. This investigation was approved by the UCLA Committee on Human Research.
Statistics
Continuous variables are presented as mean ± SD and categorical variables as frequency count (percentage). Differences between groups were determined using Student’s t-test, chi-square analysis, and quantile regression. P values < 0.05 were considered significant.
Results
Twenty-eight thousand four hundred eighty individuals met the inclusion criteria (0.63% of the total individuals in the database). Of these, 12,570 patients were seen for a general adult medical examination without abnormal findings, 15,592 were seen for a routine general medical examination at a healthcare facility, and 318 were seen for routine immunization.
The general characteristics of the analyzed patients are summarized in Table 1. Fifty-two percent of the patients (14,766) were female and 48 % (13,714) were male. The mean age of the combined cohort was 28.9 ± 5.1 years, whereas the mean age of males was 29.1 ± 5.1 years and that of females was 28.7 ± 5.0 years (p <0.05). The distribution of race is shown in Table 1; in 13,554 patients (48%), race was not reported.
Table 1.
General Patient Characteristics
| Parameter | |
|---|---|
| Gender, N (%) | |
| Males | 13,714 (48.153%) |
| Females | 14,766 (51.847%) |
| Age, years, mean ± SD | Males 29.1 ± 5.1 |
| Females 28.7 ± 5.0 | |
| Combined cohort 28.9 ± 5.1 | |
| Race, N (%) | |
| Caucasian | 9,269 (32.546%) |
| Black | 774 (2.718%) |
| Asian | 2,608 (9.157%) |
| Hispanic | 2,275 (7.988%) |
| Not Reported | 13,554 (47.591%) |
The mean serum [TCO2] of the combined cohort was 25.8 ± 2.28 mEq/L (Fig. 1) and the median value was 26 mEq/L; ninety-one percent of patient values laid within the proposed 23-30 mEq/L range (span of 8 mEq/L) and 61.7% were within the 24-27 mEq/L range (span of 4 mEq/L) (Table 2 and Fig. 2).
Figure 1.
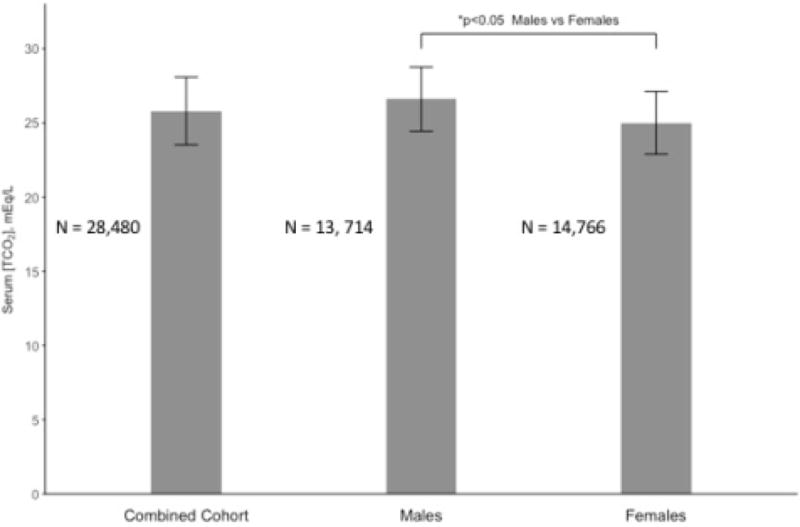
Mean serum total CO2 concentration ([TCO2]) in venous blood in a cohort of 28,480 apparently healthy younger adults seen at UCLA outpatient clinics from 2006 to the present. Bars for the combined cohort, males, and females are shown separately. Mean serum [TCO2] was slightly but significantly higher in males than females. Error bars represent standard deviation.
Table 2.
Frequency of Values of Serum [TCO2]
| Serum [TCO2] mEq/L | Combined Cohort N = 28,480 |
Males N = 13,714 |
Females N = 14,714 |
|||
|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | |
| 15 | 1 | 0.004 | 0 | 1 | 0.007 | |
| 16 | 2 | 0.007 | 1 | 0.007 | 1 | 0.007 |
| 17 | 4 | 0.01 | 1 | 0.007 | 3 | 0.020 |
| 18 | 20 | 0.07 | 1 | 0.007 | 19 | 0.13 |
| 19 | 63 | 0.22 | 15 | 0.11 | 48 | 0.33 |
| 20 | 197 | 0.69 | 23 | 0.17 | 174 | 1.18 |
| 21 | 540 | 1.89 | 92 | 0.67 | 448 | 3.04 |
| 22 | 1264 | 4.43 | 283 | 2.06 | 981 | 6.67 |
| 23 | 2320 | 8.15 | 629 | 4.59 | 169 | 11.49 |
| 24 | 3711 | 13.03 | 1135 | 8.28 | 2576 | 17.51 |
| 25 | 4620 | 16.22 | 1843 | 13.44 | 2777 | 18.87 |
| 26 | 4931 | 17.31 | 2401 | 17.51 | 2530 | 17.19 |
| 27 | 4297 | 15.10 | 2491 | 18.16 | 1806 | 12.27 |
| 28 | 3205 | 11.25 | 2165 | 15.79 | 1040 | 7.07 |
| 29 | 1913 | 6.72 | 1468 | 10.70 | 445 | 3.02 |
| 30 | 930 | 3.26 | 763 | 5.56 | 168 | 1.14 |
| 31 | 336 | 1.18 | 294 | 2.14 | 42 | 0.29 |
| 32 | 90 | 0.32 | 79 | 0.58 | 11 | 0.07 |
| 33 | 28 | 0.98 | 25 | 0.18 | 3 | 0.02 |
| 34 | 6 | 0.02 | 5 | 0.03 | 1 | 0.007 |
| 35 | 1 | 0.004 | 1 | 0.007 | 0 | |
| 36 | 1 | 0.004 | 0 | 1 | 0.007 | |
Figure 2.
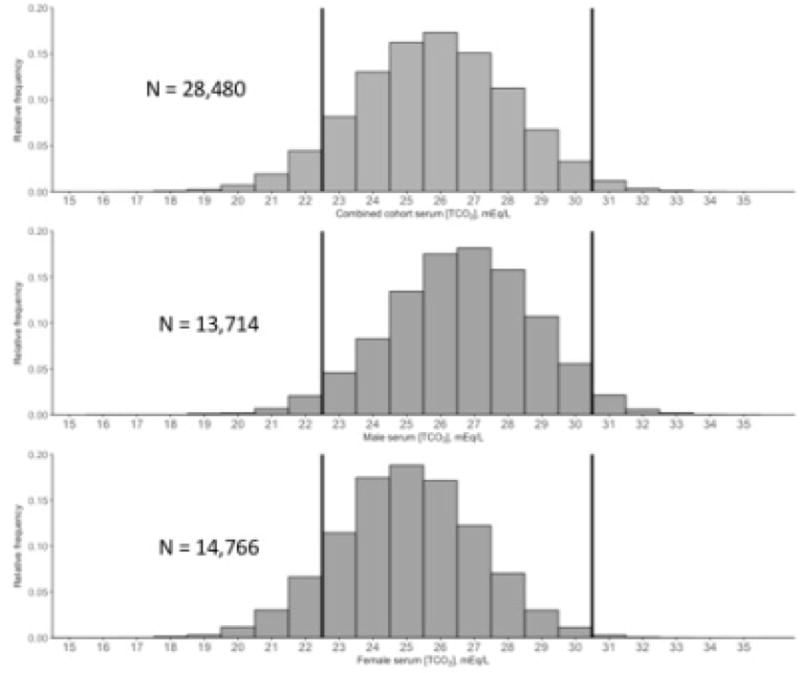
Relative frequency of values for serum total CO2 concentration ([TCO2]) in venous blood observed in a cohort of 28,480 apparently healthy younger adults seen at UCLA outpatient clinics from 2006 to the present. Relative frequency of serum ([TCO2] values for the combined cohort, males, and females and shown separately.
The mean serum [TCO2] was slightly higher in males than females, 26.6 ± 2.16 mEq/L vs 25.0 ± 2.11 mEq/L (p < 0.05) (Fig. 1), with 94% of male values and 88.3% of female values laying within the 23-30 mEq/L range (p < 0.05) (Table 2 and Fig. 2). The median serum [TCO2] was also higher in males than females, 27 mEq/L vs 25 mEq/L (p < 0.05). Ninety-seven percent of males and 88.7% of females had a venous [TCO2] ≥23 mEq/L (p < 0.05). Ninety-seven percent of males and 99.6 % of females had a venous [TCO2] ≤30 mEq/L (p < 0.18, ns). Fifty-seven percent of males compared to 65.6% of females had a venous [TCO2] within the 24-27 mEq/L range (p < 0.05).
Discussion
On the basis of an analysis of carefully conducted studies on acid-base composition of normal subjects, we recently proposed that the reference range of serum [TCO2] in venous blood at sea level be narrowed to 23-30 mEq/L4. The results of the present study provide strong validation of the proposed range, in that 91% of the serum [TCO2] of apparently healthy younger adults residing at sea level laid within the 23-30 mEq/L limits (Table 2 and Fig. 2). This finding is all the more remarkable, considering that serum [TCO2] was measured utilizing routine procedures in different clinical laboratories in the UCLA system. In individuals residing above sea level (particularly at altitudes greater 1500 m or 4196 feet), the prevailing chronic hypocapnia is expected to shift the reference range of serum [TCO2] to the left. Reference ranges for these individuals should be established separately.
Our validation cohort, although large (28,480 individuals), was a fraction of the approximately 4.5 million patients contained in the UCLA xDR database (0.63%), as a result of the strict inclusion criteria used. As noted, we selected younger adults (18-40 years of age), who were free of diseases and conditions that could perturb acid-base status, were not taking medications that could affect acid-base balance and were seen for a routine medical examination or immunization in the outpatient setting. Indeed, the mean age of the combined cohort was 28.9 years. This relative youthfulness made it less likely that the selected individuals would have underlying diseases at a covert stage. Similarly, their age range excluded age-related decreases in GFR that might not have been captured by ICD-9 or ICD-10 codes for chronic kidney disease. Thus, it seems reasonable to posit that the cohort examined was representative of apparently healthy younger adults residing at sea level and expected to have normal acid-base status.
The reference range of serum [TCO2] recently proposed by us (23-30 mEq/L) incorporates the fact that serum [HCO3−] in premenopausal women is approximately 1 mEq/L lower than that in men7. This small difference has been attributed to the PaCO2 of premenopausal women being lower by 2-4 mm Hg than that of normal men reflecting the centrally-mediated effect of progesterone to stimulate alveolar ventilation. Serum [HCO3−] rises with the appearance of menopause and such rise is reversed by hormone replacement therapy that includes progesterone8. Expectedly, females (premenopausal) in our study had a slightly lower mean serum [TCO2] than males (by 1.6 mEq/L) (Fig. 1) and the distribution of their serum [TCO2] values was shifted toward lower values (Table 2 and Fig. 2).
Only a small fraction of our combined cohort (9%) had serum [TCO2] values residing outside the proposed 23-30 mEq/L range (Fig. 2). Examining this issue in more detail, 3% of males but 11.3% of females had serum [TCO2] <23 mEq/L (p < 0.05). More specifically, 2.1% of males and 6.6% of females had serum [TCO2] of 22 mEq/L (p < 0.05); 0.67% of males and 3% of females had serum [TCO2] of 21 mEq/L (p < 0.13, ns); 0.17% of males and 1.18% of females had serum [TCO2] of 20 mEq/L(p < 0.30, ns); and tiny fractions of individuals had serum [TCO2] values as low as 15 mEq/L (Table 2). Note that individuals with serum [TCO2] values in venous blood of 20-22 mEq/L are expected to have [HCO3−] values in arterial blood of approximately 18-20 mEq/L. The lower end of the normal range of [HCO3−] in arterial blood in adults (males and females) at sea level extends to 21 mEq/L7. Thus, some of the individuals just outside the lower end of the reference range of serum [TCO2] are normal outliers, more females than males, because of the normal distribution of the serum [TCO2] in females toward lower values. However, the bulk of the individuals with serum [TCO2] values <23 mEq/L must harbor a cardinal acid-base disorder, namely metabolic acidosis or respiratory alkalosis. Increased consumption of animal protein and grains and decreased intake of fruits and vegetables might be contributing to the serum [TCO2] residing outside the lower end of the reference range9.
Undiagnosed bowel disorders, diet-induced ketosis, mild diabetic ketoacidosis, renal tubular acidosis, and hyperventilation triggered by a number of causes (e.g., anxiety, the hyperventilation syndrome) are among the many potential etiologies of the low serum [TCO2] values in our cohort. Because our data originate from an administrative database, we were unable to search for potential etiologies.
On the other hand, only 2.9% of males and 0.39% of females had serum [TCO2] values >30 mEq/L (p < 0.09, ns), the upper end of the proposed normal range. More specifically, 2.1% of males and 0.28% of females had serum [TCO2] of 31 mEq/L (p < 0.23, ns); 0.58% of males and 0.07% of females had serum [TCO2] of 32 mEq/L (p<0.66, ns); and tiny fractions of individuals had serum [TCO2] values as high as 36 mEq/L (Table 2). Again, a limited number of individuals with values just outside the upper limit of the reference range are normal outliers, but many must harbor a cardinal acid-base disorder, namely metabolic alkalosis or respiratory acidosis. Subjects ingesting primarily a vegetarian diet might also have values outside the upper end of the reference range. Undiagnosed disorders, such as surreptitious vomiting or diuretic use, Gitelman syndrome, and rare cases of hypoventilation (e.g., the obesity-hypoventilation syndrome) are among the potential etiologies of high serum [TCO2] values in our cohort.
The strength of this study is the inclusion of more than 28,000 individuals carefully selected from the approximately 4.5 million patients listed in the UCLA xDR database to ensure that only younger adults seen as outpatients and devoid of any conditions that could affect acid-base balance were eligible. However, absence of these undesirable conditions was only based on the absence of the corresponding ICD-9 and ICD-10 codes assigned to the outpatient visit; obviously, the veracity of such assessment rests with the completeness of the patient’s diagnoses described by the health professional. Strengthening the position that we actually analyzed apparently healthy younger adults is that the patients were seen for a general adult medical examination without abnormal findings, a routine general medical examination at a healthcare facility, or for routine immunization. Yet, we acknowledge that they differ from an unselected normal population in that they subjected themselves to an outpatient evaluation by a physician. An additional weakness of our study is that medications listed in the database might not have captured all medications taken by the patient as well as over-the-counter medications. Be that as it may, additional analyses of large cohorts of individuals, in which relevant conditions are rigorously controlled, are needed to confirm these findings.
In summary, the present study provides strong external validation of our recent proposal that the reference range of serum [TCO2] in venous blood at sea level be narrowed to 23-30 mEq/L. As before, we recommend that subjects with verified serum [TCO2] outside this range be considered for assessment with a venous blood gas to exclude the presence of clinically important acid-base disorders.
Acknowledgments
This research was supported by NIH National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881 and by unrestricted funds from UCLA Educational and Research Fund (JAK)
References
- 1.Kraut JA, Madias NE. Approach to patients with acid-base disorders. Respir Care. 2001;(46):392–403. [PubMed] [Google Scholar]
- 2.Adrogue HJ, Gennari FJ, Galla JH, Madias NE. Assessing acid-base disorders. Kidney Int. 2009;76(12):1239–1247. doi: 10.1038/ki.2009.359. [DOI] [PubMed] [Google Scholar]
- 3.Adrogue HJ, Madias NE. Tools for clinical assessment. In: Gennari FJ, Adrogue HJ, Galla JH, Madias NE, editors. Acid-Base Disorders and Their Treatment. 1st. Boca Raton, Fl: Taylor Francis; 2005. pp. 801–816. [Google Scholar]
- 4.Kraut JA, Madias NE. Re-Evaluation of the Normal Range of Serum Total CO2 Concentration. Clin J Am Soc Nephrol. 2018;13(2):343–347. doi: 10.2215/CJN.11941017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schindler E, Brown S, Scott M. Electrolytes and Blood Gases. In: Rifai N, Horvath AR, Wittwer CT, editors. Tietz Textbook of Clinical Chemistry and Molecular Diagnositics. sixth. St Louis: Elsevier; 2017. pp. 604–625. [Google Scholar]
- 6.American Association of Clinical Chemistry. Total CO2 reference range. 2017 10-5-2017. Available at: https://labtestsonline.org/understanding/analytes/CO2/tab/test. Accessed February 10, 2018.
- 7.Adrogue HJ, Madias NE. Normal acid-base values. In: Gennari FJ, Adrogue HJ, Galla JH, Madias NE, editors. Acid-Base Disorders and Their Treatment. 1st. Boca Raton: Taylor and Francis; 2005. pp. 789–799. [Google Scholar]
- 8.Orr-Walker BJ, Horne AM, Evans MC, et al. Hormone replacement therapy causes a respiratory alkalosis in normal postmenopausal women. J Clin Endocrinol Metab. 1999;84(6):1997–2001. doi: 10.1210/jcem.84.6.5797. [DOI] [PubMed] [Google Scholar]
- 9.Goraya N, Simoni J, Hee-Jo C, Wesson DE. A comparison of treating metabolic acidosis in CKD Stage 4 hypertensive kidney disease with fruits and vegetables or sodium bicarbonate. Clin J Am Soc Nephrol. 2013;(8):3–11. doi: 10.2215/CJN.02430312. [DOI] [PMC free article] [PubMed] [Google Scholar]


