Abstract
Background:
With passage of the HIV Organ Policy Equity (HOPE) Act, people living with HIV (PLWH) can donate organs to PLWH awaiting transplant. Understanding knowledge and attitudes regarding organ donation among PLWH in the US is critical to implementing the HOPE Act.
Methods:
PLWH were surveyed regarding their knowledge, attitudes, and beliefs about organ donation and transplantation at an urban academic HIV clinic in Baltimore, MD between 08/2016–10/2016. Responses were compared using Fisher’s exact and chi-squared tests.
Results:
Among 114 survey respondents, median age was 55 years, 47.8% were female, and 91.2% were African American. Most were willing to be deceased donors (79.8%) or living donors (62.3%). Most (80.7%) were aware of the US organ shortage; however, only 24.6% knew about the HOPE Act and only 21.1% were registered donors. Respondents who trusted the medical system or thought their organs would function adequately in recipients were more likely to be willing to be deceased donors (p<0.001). Respondents who were concerned about surgery, worse health post-donation, or need for changes in HIV treatment due to donation were less likely to be willing to be living donors (p<0.05 for all). Most believed that PLWH should be permitted to donate (90.4%) and that using HIV+ donor organs for transplant would reduce discrimination against PLWH (72.8%).
Conclusions:
Many of the PLWH surveyed expressed willingness to be organ donors. However, knowledge about the HOPE Act and donor registration was low, highlighting a need to increase outreach.
Keywords: organ transplantation, organ donation, HIV/AIDS, survey, HOPE Act
INTRODUCTION
Under the HIV Organ Policy Equity (HOPE) Act, it is now permissible to transplant organs from HIV-infected donors (HIV D+) into recipients who are also HIV-infected (HIV R+) under research protocols1,2. National registry studies estimate there are 350–600 potential HIV+ organ donors per year in the US3,4. Such an expansion of the donor pool would help ameliorate the organ shortage crisis, not only for people living with HIV (PLWH), but also for others awaiting transplant. The potential success of HIV D+/R+ transplantation depends greatly on the attitudes and beliefs of PLWH towards organ donation.
Many barriers to organ donation have been identified previously, including religious and cultural beliefs, family influences, concerns about body integrity, medical mistrust, questions about the validity of brain death, fear of premature organ recovery, and lack of knowledge or reservations about the donation process.5 PLWH may share the same concerns, or have other concerns regarding organ donation impacting their willingness to donate and the feasibility of implementing HIV D+/R+ transplants. Alternatively, there may be perceived benefits unique to PLWH, such as feeling empowered by being able to donate, which could increase willingness to donate. There may also be unique administrative barriers since Organ Procurement Organizations have varied policies on HIV disclosure to legal next of kin during the donation process.
The objective of this study was to learn more from PLWH regarding knowledge, attitudes, and beliefs regarding HIV D+/R+ transplants, focusing primarily on their willingness to donate organs.
METHODS
Survey design
The initial survey instrument was developed by the study team, including members with expertise in transplant surgery, infectious diseases, bioethics, and statistics, and research staff; the study team subsequently evaluated the relevance and appropriateness of the survey items. A revised instrument of 53 items was initially tested with ten individuals receiving care at the Johns Hopkins HIV Clinic, Baltimore, MD. Initial testing was conducted along with cognitive interviews to assess clarity and comprehension of each survey item and response options6. The survey was further revised, yielding a final instrument consisting of 58 items (See Supplement 1). This study was reviewed and approved by the Johns Hopkins Medicine Institutional Review Board.
Closed-ended response options (“yes,” “no,” “not sure”) were used to assess knowledge and willingness to donate organs. Knowledge items included awareness of: a) the current organ shortage in the United States; b) the prior ban on the use of HIV+ donor organs in transplantation; and c) the HOPE Act. Attitudes and beliefs about HIV D+/R+ transplants were assessed using a Likert scale (“definitely not,” “probably not,” “not sure,” “probably yes,” “definitely yes”). An open-ended question was included to allow respondents to describe any other influences on their willingness to donate organs.
Survey administration
Participants were recruited from the Johns Hopkins HIV Clinic between August and October 2016 during clinic hours. Research staff members either approached patients entering the clinic, or interested patients directly approached research staff members stationed adjacent to the clinic waiting room. Surveys were administered orally one-on-one in a private setting and took approximately 30 minutes. All respondents provided written informed consent. Upon survey completion, respondents received a $25 gift card to a major department store.
Study population
The study population was a non-random convenience sample of 114 individuals attending the Johns Hopkins HIV Clinic. PLWH who were able to speak English, and were ≥ 18 years of age were eligible to participate. While a precise response rate was not obtained, approximately >90% of those approached agreed to participate.
Demographic and health characteristics
Respondents were asked their age, education, employment, number of co-habitants, income, insurance, gender identity and biological sex, sexual orientation, race, ethnicity, and marital status. History of chronic kidney disease (CKD), chronic liver disease, dialysis, and hepatitis C virus (HCV) were ascertained by self-report. Respondents were also asked to report whether they had disclosed their HIV status to family members or friends.
Statistical analysis
Responses were categorized as “willing to donate organs of any type” if they answered “yes” to being willing to be deceased donors or living donors. For closed-ended items with response options of “yes,” “no,” “not sure,” we dichotomized responses, considering a “not sure” response to indicate “no.” Responses to items using a Likert scale was used were also dichotomized into “yes” (for “probably yes” or “definitely yes”) or “no” (for “not sure,” “probably not,” or “definitely not”). We examined associations between a) respondent characteristics and b) knowledge, attitudes and beliefs, and willingness to donate organs using Fisher’s exact and chi-squared tests for categorical variables and Wilcoxon-Mann-Whitney tests for continuous variables. Responses to open-ended questions were analyzed for themes defined by two independent coders.
All analyses were performed using Stata 14.2/SE for Linux (College Station, Texas).
RESULTS
Demographic and health characteristics
Among the 114 study participants, the median age was 55 years (IQR:49–58), the median time living with HIV was 20 years (IQR:12–25), 47.8% were female, 91.2% were African American, and 15.8% were married or co-habitating (Table 1). Regarding educational status, 27.2% of respondents had less than a high school degree, 63.2% had completed high school or its equivalent, and 9.6% had at least some college education. While 22.8% of respondents were unemployed or retired and 70.2% were disabled, 7.0% were employed (either part time or full time); 97.4% had public insurance. Based on self-reported medical history, 8.8% had chronic liver disease, 3.5% were on dialysis, and 52.6% were co-infected with HCV.
Table 1.
Demographic characteristics of survey respondents.
| Characteristic | All (N=114) |
Willing to be deceased donors (N=91) | Willing to be living donors (N=71) |
|---|---|---|---|
| Age in years, median (IQR) | 55 (49–58) | 55 (49–58) | 55 (50–58) |
| Years living with HIV, median (IQR) | 20 (12–25) | 20 (12–25) | 19 (11–25) |
| Female, n (%) | 54 (47.7) | 44 (48.9) | 34 (47.9) |
| African American Race, n (%) | 104 (91.2) | 82 (90.1) | 63 (88.7) |
| Education status, n (%) | |||
| Less than high school | 31 (27.2) | 26 (28.6) | 21 (29.6) |
| High school or equivalent | 72 (63.2) | 58 (63.7) | 43 (60.6) |
| At least some college | 11 (9.6) | 7 (7.7) | 6 (8.5) |
| Employment status, n (%) | |||
| Unemployed or retired | 25 (21.9) | 19 (20.9) | 11 (15.5) |
| Disabled | 80 (70.2) | 64 (70.3) | 52 (73.2) |
| Employed (full time or part time) | 8 (7.0) | 7 (7.7) | 7 (9.9) |
| Marital status, n (%) | |||
| Single | 96 (84.2) | 76 (83.5) | 56 (78.9) |
| Married/co-habitating | 18 (15.8) | 15 (16.5) | 15 (21.1) |
| Public insurance (Medicare or Medicaid), n (%) | 111 (97.4) | 88 (96.7) | 69 (97.2) |
| Self-reported medical history, n (%) | |||
| Chronic liver disease | 10 (8.8) | 10 (11.0) | 5 (7.0) |
| Dialysis | 4 (3.5) | 3 (3.3) | 2 (2.8) |
| Hepatitis C | 60 (52.6) | 51 (56.0) | 42 (59.2) |
Knowledge and attitudes regarding HIV D+/R+ organ transplants
Most respondents (92; 80.7%) were aware of the organ shortage in the U.S. Thirty-nine respondents (34.2%) were aware of the prior ban on the use of HIV+ donor organs for transplants, and 28 (24.6%) had heard of the HOPE Act. The majority (103; 90.4%) agreed that PLWH should have the choice to donate organs to other PLWH, and 107 respondents (93.8%) agreed that HIV D+/R+ transplantation should be studied. The majority (83; 72.8%) agreed that using HIV+ donor organs for transplants would reduce discrimination against PLWH (Figure 1).
Figure 1.
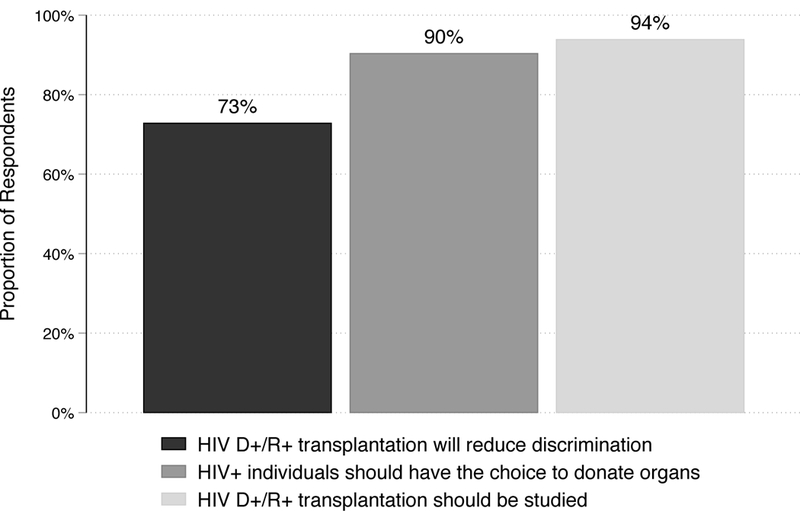
Respondents’ beliefs about HIV D+/R+ transplants (N=114)
Information sources
Respondents who were aware of the HOPE Act (n=28) were asked to indicate the source of information; multiple sources could be selected if applicable. News (newspapers, TV) was the most common source identified (n=17); additional sources included academic journals (n=9), word of mouth (n=8), community groups (n=7), doctors or other healthcare providers (n=6), social media (n=5), and other (n=3).
Willingness to donate organs and donor registration rate
Ninety-one respondents (79.8%) were willing to be deceased donors and 71 respondents (62.3%) were willing to be living donors (Figure 2). Sixty-three respondents (55.3%) were willing to be both deceased and living donors. Organ donor registration overall was 21.1% (n=24) (Figure 3). Eighteen respondents (17.8%) reported having discussed organ donation with their family, while 106 respondents (93.0%) reported having discussed their HIV status with their family.
Figure 2.
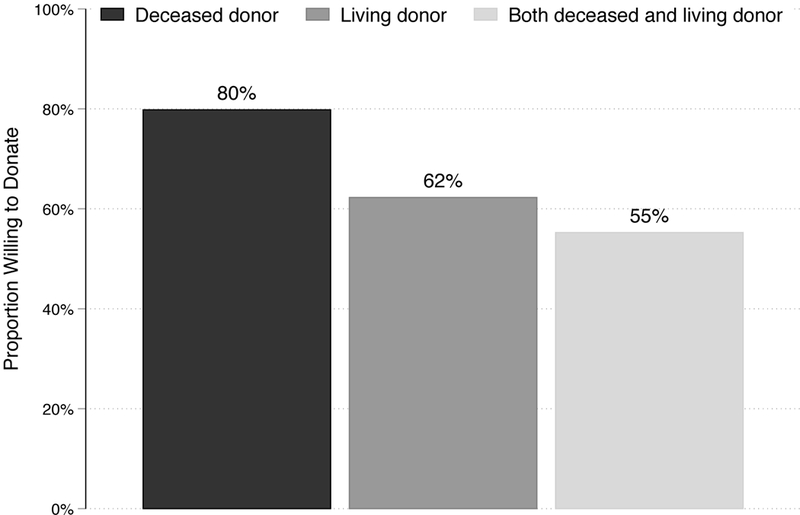
Proportion of respondents willing to donate organs (N=114).
Figure 3.
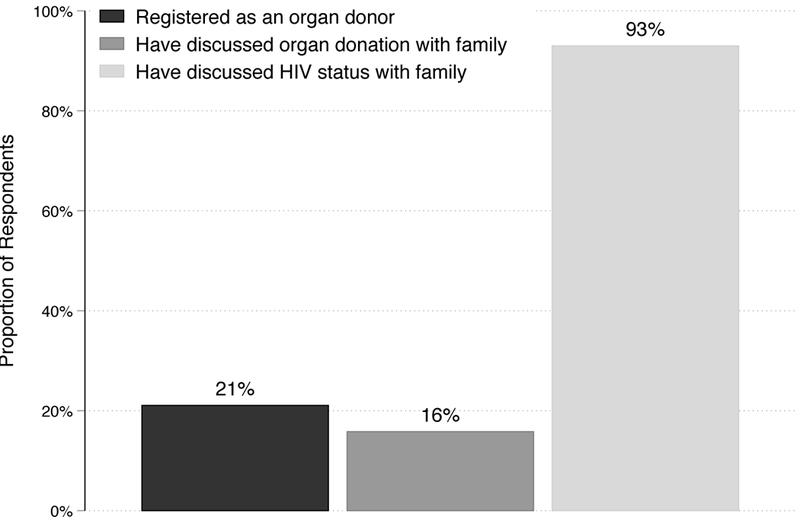
Organ registration rate and discussion with family (N=114)
Of the 91.2% of total respondents who are African American (n=104), 78.5% (82 of 104) were willing to be deceased donors, 60.6% (63 of 104) were willing to be living donors, and 52.9% (55 of 104) were willing to be both deceased and living donors.
Concerns and beliefs about deceased organ donor donation
A minority of respondents cited concerns and beliefs regarding deceased donation: 5.2% thought donating organs would add financial burden to themselves and/or their family; 12.3% thought their body would be disfigured before their funeral, and 23.7% thought their organs would be recovered before they were dead. Seventy-one percent thought their organs would function well in a recipient and 84.2% trusted the medical system to handle the donation process (Table 2). Respondents who thought their organs would function as well in the recipient despite the potential donors’ medical illnesses were more likely to be willing to be deceased donors (88.9% vs. 57.6%, p<0.001); those who trusted the medical system to handle the donation process were also more likely to be willing to be deceased donors than those who did not (87.5% vs. 38.9%, p<0.001).
Table 2.
Concerns and beliefs about donation
| Concern/Belief | % Expressing concern/belief | % Willing to donate with concern/belief | % Willing to donate without concern/belief | P-value | |
|---|---|---|---|---|---|
| Factors relating to deceased organ donation | |||||
| Financial burden | 5.2 | 66.7 | 80.6 | 0.6 | |
| Body disfigured before funeral | 12.3 | 64.3 | 82.0 | 0.1 | |
| Organs taken before death | 23.7 | 85.1 | 78.1 | 0.6 | |
| Adequate organ function in recipient | 71.1 | 88.9 | 57.6 | <0.001 | |
| Trust the medical system | 84.2 | 87.5 | 38.9 | <0.001 | |
| Factors relating to living organ donation | |||||
| HIV treatment would be changed | 27.2 | 41.9 | 69.9 | <0.01 | |
| Undergoing surgery | 32.4 | 45.9 | 70.1 | 0.01 | |
| Poor health post-donation because of HIV | 34.2 | 38.5 | 74.7 | <0.001 | |
Concerns and beliefs about living organ donor donation
When asked about reasons they were not willing to be living donors, 27.2% of respondents thought their HIV treatment would need to be changed, 32.4% had concerns about going through surgery, and 34.2% thought they would be at higher risk for poor health after donation because of their HIV status (Table 2). Respondents were less likely to be willing to be living donors if they thought their HIV treatment would need to be changed (41.9% vs. 69.9%, p=0.006), they had concerns about going through surgery (45.9% vs. 70.1%, p=0.01), and they thought they would be at higher risk for poor health because of their HIV status (38.5% vs. 74.7%, p<0.001).
Open-ended Responses
At the end of the survey, respondents were given an opportunity to provide other factors influencing their opinion on HIV D+/R+ organ transplants as well as reasons influencing their willingness to be a deceased or living donor. Altruism was identified as a motivating factor with responses such as: “If it’s going to save a life,” “[It] might help save lives” and “It could give someone a better chance of surviving, a new outlook on life.” A few respondents raised concerns that more information was needed, with responses such as “We need to study more because there is still a lot we don’t know about,” “There’s not enough info to decide,” and, “We need more information generally.”
DISCUSSION
In this survey of the knowledge, attitudes, and beliefs of 114 PLWH at an urban HIV clinic, 91.2% of respondents were African American, and willingness to donate was high (79.8% willing to be deceased donors; 62.3% willing to be living donors). Most respondents (80.7%) were aware of the organ shortage in the US; however, only 24.6% were aware of the HOPE Act, which now allows the use of HIV+ donor organs for transplants. Although nearly all respondents (93.0%) had discussed their HIV-status with their next-of-kin, few had discussed their willingness to donate with them (17.8%) or were registered organ donors (21.1%).
Historically, organ donor registration rates have been lower for African Americans than for whites7, and an association between mistrust in the medical community and reduced organ donor registration among African Americans has been identified previously8,9. However, we found that 78.9% of African American respondents were willing to be deceased donors. This is markedly higher than studies among HIV-uninfected African Americans, which demonstrated that approximately 60% were willing to donate10. Future studies should determine whether this higher relative willingness to donate among African Americans living with HIV is found in other populations of PLWH. Potential benefits of organ donor registration specific to PLWH include reduced stigma, support of community through helping PLWH awaiting transplant, and belief that the HOPE Act creates a more equitable opportunity for transplantation for PLWH. These perceptions were common in our study: 72.8% of respondents agreed that HIV D+/R+ could reduce discrimination against PLWH and 90.4% agreed PLWH should be permitted to donate organs.
To our knowledge, this is the first study of organ donation among PLWH in the United States. However, there have been two cross-sectional surveys of willingness to donate among PLWH in other countries. In a 2012 survey of PLWH in the United Kingdom (n=206), 62% of respondents were willing to be organ donors11. Respondents in that survey were primarily black Africans (70%), about half of whom were female (54%) and mean age was 42 years. In a 2016 survey of PLWH in Taiwan (n=1010), 71.9% were willing to donate when the Taiwanese government was considering lifting the ban on using organs from HIV+ patients for transplants 12. Respondents in that study were 93.7% male, 100% Asian and mean age was 37.3 years.
We found that trust in the medical system and believing that organs from PLWH would function well in recipients were associated with increased willingness to be deceased donors whereas concerns about changes to HIV treatment, surgery, and worsened health post-donation were associated with decreased willingness to be living donors. Concern about whether one’s organs would be “usable” for transplant and willingness to be registered as an organ donor among African Americans have been documented13. Studies investigating long-term outcomes of HIV D+/R+ transplants may address concerns about long-term organ function in recipients (NCT02602262). Additionally, information on outcomes among living donors with HIV should be forthcoming based on the results of current research (NCT03408106).
Despite the high proportion of respondents who were willing to donate, only 21.1% were registered organ donors, compared to 55% of the US adult population14. This reflects a significant gap between positive attitudes towards organ donation and low registration rates. A current low registration rate among PLWH is not necessarily surprising, given that it has only been legally permissible for a few years. Accordingly, providing general education about organ donation and its value, addressing concerns about the registration process, and providing HOPE-specific education could be valuable to increase the registration rates among PLWH. This is important since a lack of registration and declined authorization for donation by next-of-kin are both recognized barriers to organ donation in the general population15. An additional concern specific to donation among PLWH is unintentional disclosures of HIV status during these next-of-kin discussions about donation after death. It is encouraging that knowledge of HIV status by next-of kin was very common in our study population, and suggests an opportunity for targeted educational interventions for similar discussions about organ donation with the next-of-kin of PLWH. For Organ Procurement Organizations, these preliminary data are also potentially important: if there are concerns related to disclosure of HIV status to legal next of kin during donation discussion, a high rate of disclosure about HIV status among potential donors could mitigate such concerns.
Though most respondents were aware of the organ shortage in the U.S., only a minority were aware of the prior ban on the use of organs from HIV+ donors or had heard of the HOPE Act, indicating a knowledge gap among the respondents. Education on HIV D+/R+ transplantation for PLWH is needed and should include information regarding: 1) HIV D+/R+ transplants are legally permissible; 2) the process of organ donor registration for PLWH is the same as for HIV-uninfected people; and 3) the importance of sharing donation decisions with family members. Awareness efforts should be multi-fold, targeting both the PLWH (potential donors and recipients) as well as the medical community who are in direct communication with both patients and their families. Our study found that most of our respondents learned about the HOPE Act via the news, but some simultaneously identified other sources of media that could potentially be used as effective educational tools. Social media can be a powerful source to not only distribute information but also increase donor registration rates. A recent study by Cameron et al16 used a Facebook platform to link with state registries and found a 21.1-fold increase in organ donor registration within their first day of the initiative, demonstrating that social media as a potentially powerful tool to raise public awareness and increase organ registration rates across the country. Similar strategies may prove effective to increase registrations rates in PLWH.
There are several limitations of this study that merit consideration. First, using a convenience sample may have resulted in selection bias. In our HIV clinic, research studies routinely recruit participants in the clinic waiting room; thus, patients were not only recruited by our team but also approached researchers directly to complete the survey. As a result, there might be a response bias among participants who approached the researchers. We estimate that less than 10% of potential participants who were approached by the research team declined participation. Second, the use of one-on-one surveys might be associated with social desirability bias. However, our findings are similar to an anonymous survey of the general population at the Mayo Clinic, which found that 84% said they would be living donors close friends and family members, and 49% were willing to donate to strangers17. This might alleviate concerns about social desirability bias in our findings. Third, we assessed mistrust in the medical system among survey respondents who were currently receiving care at the clinic. Their responses could imply a higher baseline level of trust than PLWH not in care. Finally, our study was done at an urban center with a predominantly African American population and cannot necessarily be generalized to different settings and groups.
In conclusion, in our pilot study among the 114 predominately African American respondents, willingness to donate was high. As most of our respondents identified with potential benefits of organ donation, including reduction of discrimination against PLWH and supporting the right to donate organs, further investigation is warranted to explore how these benefits can transform into increased community solidarity and decrease concerns about social justice within the transplant system. The results from our study could be further explored in a multi-center study with a larger more diverse participant pool which would increase the generalizability of the findings. In particular, it would be important to target other ethnic and racial groups as this pilot survey’s respondents were primarily African American. Medical mistrust and questions about post-donation outcomes for donors and recipients were associated with decreased willingness to donate. As HIV D+/R+ transplantation is implemented under the HOPE Act, future efforts should also be aimed at increasing awareness of the possibility of organ donation, next-of kin discussions, and registration among PLWH and at understanding barriers to donation for PLWH more broadly across the US.
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported in part by the JHU Center for AIDS Research (1P30AI094189), the NIH (R34-AI123023, K23-CA177321, R01-AI120938, F30-DK116658), and the Greenwall Foundation (Addressing the Ethical Issues in HIV+ to HIV+ Organ Transplants). The authors would also like to thank the Epidemiology Research Group in Organ Transplantation for making this research possible and providing important feedback regarding it.
ABBREVIATIONS
- CKD
chronic kidney disease
- HCV
hepatitis C virus
- HIV
human immunodeficiency virus
- HIV D+
HIV+ organ donor
- HIV R+
HIV+ transplant recipient
- HIV D+/R+
HIV+ donor and HIV+ recipient
- HOPE Act
HIV Organ Policy Equity Act
- PLWH
people living with HIV
Footnotes
Presented at:
American Society of Transplant Surgeons (ASTS) 17th Annual State of the Art Winter Symposium, 26 – 29 January 2017, Miami, Florida (poster presentation)
American Transplant Congress (ATC) 2017 Meeting, 29 April – 3 May, Chicago, Illinois (poster presentation)
9th International AIDS Society Conference on HIV Science, 23-26 July 2017, Paris, France (poster presentation)
REFERENCES
- 1.Boyarsky BJ, Segev DL. From bench to bill: How a transplant nuance became 1 of only 57 laws passed in 2013. Ann Surg. 2016;263(3):430–433. [DOI] [PubMed] [Google Scholar]
- 2.Health Resources and Services Administration (HRSA), Department of Health and Human Services (HHS). Organ procurement and transplantation: Implementation of the HIV organ policy equity act. final rule. Fed Regist. 2015;80(89):26464–26467. [PubMed] [Google Scholar]
- 3.Boyarsky BJ, Hall EC, Singer AL, Montgomery RA, Gebo KA, Segev DL. Estimating the potential pool of HIV-infected deceased organ donors in the united states. Am J Transplant. 2011;11(6):1209–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richterman A, Sawinski D, Reese PP, et al. An assessment of HIV-infected patients dying in care for deceased organ donation in a united states urban center. Am J Transplant. 2015;15(8):2105–2116. [DOI] [PubMed] [Google Scholar]
- 5.Irving M,J, Tong Allison, Jan Stephen, et al. Factors that influence the decision to be an organ donor: A systematic review of the qualitative literature. Nephrology Dialysis Transplantation. 2011;27(6):2526–2533. [DOI] [PubMed] [Google Scholar]
- 6.Sugarman J, Seils DM, Watson-Ormond JK, Weinfurt KP. Using cognitive interviews to enhance measurement in empirical bioethics: Developing a measure of the preventive misconception in biomedical HIV prevention trials. AJOB Empir Bioeth. 2016;7(1):17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quick BL, LaVoie NR, Reynolds-Tylus T, Bosch D, Morgan SE. Does donor status, race, and biological sex predict organ donor registration barriers? J Natl Med Assoc. 2016;108(3):140–146. [DOI] [PubMed] [Google Scholar]
- 8.Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. J Gen Intern Med. 2006;21(9):995–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morgan SE. Many facets of reluctance: African americans and the decision (not) to donate organs. J Natl Med Assoc. 2006;98(5):695–703. [PMC free article] [PubMed] [Google Scholar]
- 10.Minniefield WJ, Yang J, Muti P. Differences in attitudes toward organ donation among african americans and whites in the united states. J Natl Med Assoc. 2001;93(10):372–379. [PMC free article] [PubMed] [Google Scholar]
- 11.Taha H, Newby K, Das A, Das S. Attitude of patients with HIV infection towards organ transplant between HIV patients. A cross-sectional questionnaire survey. Int J STD AIDS. 2016;27(1):13–18. [DOI] [PubMed] [Google Scholar]
- 12.Lee YC, Hung CC, Cheng A, et al. Willingness of human immunodeficiency virus-positive patients to donate their organs for transplantation in taiwan: A cross-sectional questionnaire survey. Transpl Infect Dis. 2016;18(6):856–861. [DOI] [PubMed] [Google Scholar]
- 13.DuBay DA, Ivankova N, Herby I, et al. African american organ donor registration: A mixed methods design using the theory of planned behavior. Prog Transplant. 2014;24(3):273–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Donate life america. 2017 annual report. https://www.donatelife.net/wp-content/uploads/2016/06/2017_AnnualUpdate_singlepages_small.pdfSeptember 30, 2017.
- 15.Siminoff LA, Gordon N, Hewlett J, Arnold RM. Factors influencing families’ consent for donation of solid organs for transplantation. JAMA. 2001;286(1):71–77. [DOI] [PubMed] [Google Scholar]
- 16.Cameron AM, Massie AB, Alexander CE, et al. Social media and organ donor registration: The facebook effect. Am J Transplant. 2013;13(8):2059–2065. [DOI] [PubMed] [Google Scholar]
- 17.Mayo clinic. half of americans would consider donating a kidney to a stranger. . Science Daily April 13, 2013. Available from: www.sciencedaily.com/releases/2013/04/130418094518.htm. Accessed January 11, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


