Abstract
Background
PrEP uptake has lagged among US women. PrEP stigma is a recognized barrier to uptake among MSM but remains largely unexplored among women. This study examined the pervasiveness of PrEP stigma among US women and its implications for uptake.
Setting/Methods
In a 2017 online survey of Planned Parenthood patients drawn from the three cities with the highest numbers of new HIV infections in Connecticut, 597 heterosexually-active, HIV-negative, PrEP-inexperienced women reported background characteristics, two dimensions of anticipated PrEP stigma (PrEP-user stereotypes and PrEP disapproval by others), and three indicators of potential PrEP uptake (interest in learning more about PrEP, intention to use PrEP, and comfort discussing PrEP with a provider).
Results
Participants commonly perceived PrEP-user stereotypes, with many believing that others would regard them as promiscuous (37%), HIV-positive (32%), bad (14%), or gay (11%) if they used PrEP. Thirty percent would feel ashamed to disclose PrEP use. Many participants expected disapproval by family (36%), sex partners (34%), and friends (25%). In adjusted analyses, perception of PrEP-user stereotypes was uniquely associated with lower comfort discussing PrEP with a provider. Expected PrEP disapproval by others was uniquely associated with less PrEP interest, less intention to use PrEP, and less comfort discussing PrEP with a provider. Exploratory moderation analyses suggested intention to use PrEP was greatest when participants anticipated low levels of both PrEP-user stereotypes and PrEP disapproval by others.
Conclusion
Findings highlight the need for positive messaging targeting potential PrEP users and their social networks to increase PrEP acceptance and uptake.
Keywords: HIV infections, pre-exposure prophylaxis, prevention of sexual transmission, social stigma, healthcare, women
INTRODUCTION
HIV pre-exposure prophylaxis (PrEP) uptake has lagged among US women: Although about 200,000 are considered strong candidates for PrEP based on their sexual and/or injection practices [1], retail pharmacy records indicate that fewer than 50,000 have initiated PrEP [2,3]. This gap between PrEP candidacy and PrEP uptake is particularly extreme among women of color: Black and Latina women are respectively 17 and 4 times more likely than White women to become HIV infected in their lifetime [4] but significantly less likely to initiate PrEP [1,5]. Addressing low PrEP uptake among women requires understanding and overcoming the psychosocial barriers to PrEP access that they experience.
PrEP stigma is one such barrier that has received increasing attention among men who have sex with men (MSM) [6–15] but remains understudied among women. PrEP stigma is a social harm involving the association of negative meaning with PrEP and corresponding devaluation of PrEP users [16]. As described by MSM, PrEP users are commonly stereotyped as promiscuous and/or secretly HIV-positive (concealing their HIV medication as PrEP) [6–9,12,15]. PrEP stigma has consistently been linked to reduced PrEP interest and uptake among MSM [7–10, 14].
Less is known about the scope and impact of PrEP stigma among women. In one community sample, nearly half of women endorsed the belief that PrEP users probably engage in “too much sex” or “sex with the wrong kind of people” [17]. Additionally, early qualitative research suggests that women’s concern about other people reacting negatively or making assumptions about their HIV status [18–22] operates as a barrier to PrEP use. Further research is needed to better understand the nature and implications of PrEP stigma among women, including both cultural stereotypes associated with people who use PrEP (e.g., promiscuity) and anticipated reactions to PrEP use (e.g., partner disapproval).
PrEP stigma is a particularly relevant issue for women already engaged in healthcare because, in the absence of challenges surrounding healthcare access, it may operate as one of few significant barriers to PrEP uptake. Women who are already engaged in healthcare can be readily contacted about PrEP services, have experience navigating the medical system (e.g., scheduling appointments, acquiring prescriptions), and may have experience using preventive medications such as contraception—particularly those receiving care in reproductive health settings such as Planned Parenthood. Planned Parenthood is an international nonprofit organization with nearly 650 sexual and reproductive healthcare centers across the US, which annually serve over two million women [23]. Many Planned Parenthood patients are members of sociodemographic groups disproportionately affected by HIV [23, 24]. Women have reported Planned Parenthood to be among the most trusted places to obtain PrEP services [21].
The present cross-sectional survey study explored PrEP stigma and its implications for uptake among HIV-negative, sexually active adult women recently engaged in care at Connecticut Planned Parenthood centers. We approached the study with two aims: First, we sought to describe the pervasiveness of PrEP stigma—including perceived PrEP-user stereotypes and expected disapproval of PrEP use by others. Second, we sought to examine how these dimensions of stigma affected three indicators of potential PrEP uptake: women’s interest in learning more about PrEP, intention to use PrEP, and comfort discussing PrEP with a provider. Theoretical “cascade” models characterizing the stepwise progression from initial PrEP awareness to sustained PrEP use have indicated PrEP interest, intention, and discussion with a provider are key precursors to PrEP use [25, 26]. We hypothesized that participants expressing stronger perceived PrEP-user stereotypes and greater expected PrEP disapproval by others would report less interest in learning about PrEP, less intention to use PrEP, and less comfort discussing PrEP with a provider.
METHODS
Procedures
In February of 2017, participants were recruited for an anonymous online survey. The survey was distributed via email to patients 18 and older who were recently engaged in care at Planned Parenthood centers in the three cities reporting the highest annual number of HIV infections in Connecticut: Bridgeport, New Haven, and Hartford [27]. Recently engaged in care was defined as having one or more visits in the past 10 months documented in their medical record. The survey was restricted to patients who had agreed to receiving email communication from Planned Parenthood (77%). Participants were compensated with $10 gift cards. All procedures were approved by the Yale University institutional review board.
Measures
Participants were asked to complete online self-report measures assessing PrEP stigma, potential PrEP uptake, and background characteristics as part of a larger needs assessment survey, which also included questions pertaining to health, behavior, relationships, and service delivery preferences. Before viewing the PrEP stigma and uptake measures, participants were presented with a brief introduction to PrEP, including basic facts concerning dosing, effectiveness, and side effects. The introductory information about PrEP and all PrEP stigma and uptake measures are included in full as supplemental digital content (see Text and Figure, Appendix 1).
PrEP stigma
In early 2016, the PrEP Anticipated Stigma Scale was developed based on existing measures of HIV stigma [e.g., 28] and review of PrEP stigma literature to date [e.g., 6, 7]. Items were designed to measure anticipated social stigma surrounding PrEP, including the stereotypical assumptions and (dis)approval by others that participants expected to encounter if they used PrEP. All items were pilot-tested with HIV-negative, PrEP-inexperienced, heterosexually active women (n = 163) who were patients engaged in care at different Planned Parenthood centers than those in the current study. An exploratory factor analysis identified two factors, from which two subscales were formed: PrEP-User Stereotypes (5 items) and PrEP Disapproval by Others (3 items). In the current study, we performed a confirmatory factor analysis with the present analytic sample (n = 597) to further validate these subscales, confirming the 2-factor solution [X2 (19) = 45.00, RMSEA = .05, CFI = .99]. Further details of scale development and item-by-item correlations are available as supplemental digital content (see Text and Tables, Appendix 2).
The PrEP-User Stereotypes subscale represents perceived cultural associations with PrEP [29], e.g., “People would assume I slept around if they knew I took PrEP.” Response options ranged from (1) Strongly Disagree to (4) Strongly Agree. Mean scores were calculated, with higher subscale scores indicating stronger perceived PrEP-user stereotypes (Cronbach’s α = .87).
The PrEP Disapproval by Others subscale represents expected judgment by close others for using PrEP, e.g., “My sexual partner(s) would approve of me taking PrEP.” Response options ranged from (1) Strongly Disagree to (4) Strongly Agree. After reverse-scoring the items, mean scores were calculated, with higher subscale scores indicating greater expected PrEP disapproval by others (α = .91).
PrEP uptake indicators
Three key precursors to PrEP uptake were assessed: PrEP interest, PrEP intention, and comfort discussing PrEP with a provider. PrEP interest was assessed with the item, “How interested are you in learning more about PrEP (daily HIV prevention pill)?” [(1) Not At All Interested to (5) Extremely Interested]. PrEP intention was assessed with the item, “How likely would you be to take PrEP (daily HIV prevention pill) if it were available for free?” [(1) Definitely Would Not Take PrEP to (5) Definitely Would Take PrEP] [30]. Comfort discussing PrEP with a provider was assessed with the item, “How comfortable would you be talking with a healthcare provider about PrEP (daily HIV prevention pill)?” [(1) Not At All Comfortable to (5) Extremely Comfortable].
Background characteristics
Participants reported their sociodemographic characteristics, including age, ethnicity, race, sexual orientation, education, employment status, annual household income, and geographic location (location of most recent Planned Parenthood visit). They also indicated their HIV status, number of vaginal and anal male sex partners over the past six months, condom use consistency over the past six months (recoded as 0% vs. 100% vs. inconsistent), partnership status (recoded as currently in a monogamous relationship with a recently-tested HIV-negative partner vs. not or don’t know), perceived HIV risk (recoded as any vs. none), familiarity with PrEP (recoded as ever vs. never heard of PrEP), and prior PrEP use.
Analysis
The analytic sample was restricted to Planned Parenthood patients recently engaged in care (past 10 months) who met the following criteria based on self-report: identified as a woman, age 18 or older, HIV-negative, heterosexually active (i.e., participated in anal or vaginal sex with one or more men in the past six months), and never used PrEP. Means, standard deviations, and frequencies were calculated to describe the sample and measures of interest. Bivariate analyses (correlation, independent samples t-test, and one-way analysis of variance with post-hoc pairwise comparisons using Scheffé’s method) were performed to examine associations between background characteristics and PrEP stigma subscale scores and uptake indicators. Linear regressions were performed to test partial, conditional, and interaction effects of PrEP-user stereotypes and PrEP disapproval by others on the three PrEP uptake indicators. Uptake indicators were considered as independent outcomes in regression models. For each outcome, Model 1 included only background characteristics. Model 2 (partial effects model) retained all previous independent variables and added PrEP stigma (i.e., PrEP-user stereotypes and PrEP disapproval by others). Percentage of total variance explained by PrEP stigma was determined from adjusted R-squared values. Model 3 (conditional and interaction effects model) retained all previous independent variables and added the PrEP-user stereotypes × PrEP disapproval by others interaction term. PrEP-user stereotypes and PrEP disapproval by others were mean-centered for interpretation of conditional effects. We probed any significant interaction effects (p < .05) using the Johnson-Neyman technique to determine regions of significance [31].
RESULTS
Descriptive Characteristics
The survey recruitment email was distributed to 11,238 Planned Parenthood patients. The survey was closed to new participants when 973 had enrolled and initiated the survey. The survey was closed prior to reaching our enrollment maximum of 1,000 participants to avoid exceeding this maximum. (Additional patients had initiated the preliminary screening portion of the survey and we were uncertain whether they would proceed to enrollment). All data were collected within 100 hours of distributing the recruitment email. A total of 597 patients met criteria for the present analyses.
Sociodemographic characteristics of the sample are reported in Table 1.Twenty-nine percent of participants, all of whom were sexually active, reported sex with multiple male partners in the past 6 months. Ninety percent reported “never” or “sometimes” (vs. “always”) using condoms. Over half (59%) reported being in a monogamous relationship with a recently-tested HIV-negative partner, and 21% perceived themselves to be at any level of risk for acquiring HIV in their lifetime. Less than a quarter (23%) had heard of PrEP before the survey.
Table 1.
Sociodemographic Characteristics (n = 597)
| Characteristic | n (%) |
|---|---|
| Age | |
| 18–25 years | 257 (43.0) |
| 26–45 years | 326 (54.6) |
| 46–65 years | 14 (2.3) |
| Ethnicity | |
| Non-Latina/Hispanic | 453 (75.9) |
| Latina/Hispanic | 144 (24.1) |
| Racea | |
| White | 250 (41.9) |
| Black/African American | 235 (39.4) |
| Asian | 13 (2.2) |
| Other | 98 (16.4) |
| Sexual Orientation | |
| Heterosexual | 460 (77.1) |
| Bisexual | 88 (14.7) |
| Gay/Lesbian | 8 (1.3) |
| Other | 41 (6.9) |
| Education | |
| <Bachelor’s degree | 434 (72.7) |
| ≥Bachelor’s degree | 163 (27.3) |
| Employment Status | |
| Employed (full-time or part-time) | 409 (68.5) |
| Unemployed | 65 (10.9) |
| Other | 123 (20.6) |
| Annual Household Income | |
| ≤10,000 | 146 (24.5) |
| 11,000–30,000 | 202 (33.8) |
| 31,000–50,000 | 134 (22.4) |
| 51,000–70,000 | 59 (9.9) |
| >70,000 | 56 (9.4) |
| Geographic Locationb | |
| Bridgeport | 236 (39.5) |
| New Haven | 207 (34.7) |
| Hartford | 101 (16.9) |
| Other | 53 (8.9) |
n = 596 for this variable only
Represents location of Planned Parenthood center visited most recently
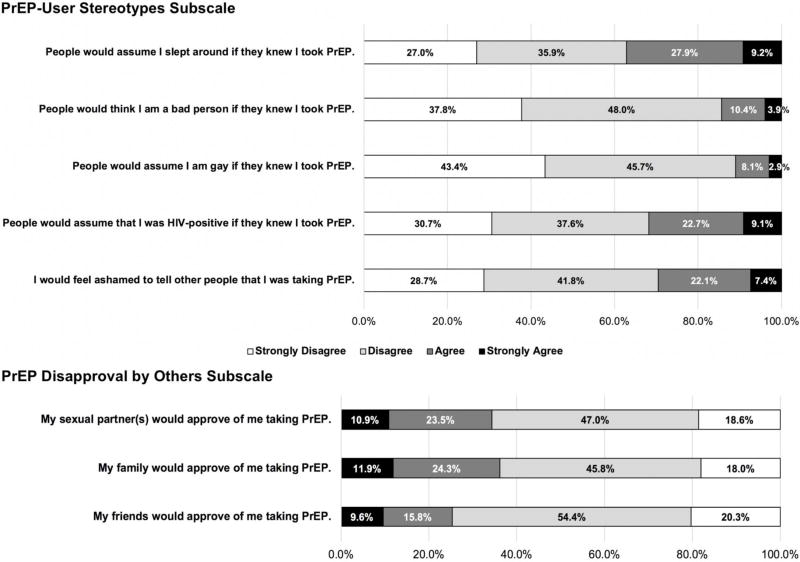
Figure 1 displays frequency distributions of PrEP stigma items. Stereotypes about PrEP users were perceived by a substantial minority of participants, with the most commonly endorsed belief being that people would assume they slept around (37% “agreed” or “strongly agreed”). Many participants expected disapproval by their family (36% “disagreed” or “strongly disagreed” that their family would approve), as well as from their sexual partner(s) (34%) and friends (25%).
Figure 1. PrEP stigma.
Response frequency distributions among HIV-negative, PrEP-inexperienced, sexually active adult women recently engaged in care at Planned Parenthood. For both subscales, anticipated stigma is indicated by dark gray and black shading.
Most participants (66%) expressed some level of interest in learning more about PrEP, 32% “probably” or “definitely” would take PrEP if freely available, and 57% were “very” or “extremely” comfortable talking to a provider about PrEP.
Associations Between Background Characteristics and PrEP Measures
Only a single background characteristic—condom use consistency—was associated with either PrEP stigma subscale score. Specifically, stronger perceived PrEP-user stereotypes were reported among participants who used condoms 0% vs. 100% of the time (p = .028).
Multiple bivariate associations between background characteristics and PrEP uptake indicators were identified. Greater interest in learning about PrEP was associated with having less than a bachelor’s degree, having multiple sexual partners, not being in a monogamous relationship with a recently-tested HIV-negative partner, perceiving HIV risk, being Black or another race (vs. White), and having an annual household income less than $10,000 (vs. over $70,000). Greater intention to use PrEP was associated with younger age, having less than a bachelor’s degree, having multiple sexual partners, not being in a monogamous relationship with a recently-tested HIV-negative partner, perceiving HIV risk, being another race (vs. White), and having an annual household income less than $50,000 (vs. over $70,000). Greater comfort discussing PrEP with a provider was associated with being non-Latina and being non-heterosexual (p < .050).
Associations Between PrEP Stigma and PrEP Uptake Indicators
As shown in Table 2, stronger perception of PrEP-user stereotypes was correlated with less PrEP interest and less comfort discussing PrEP with a provider (p < .050) and marginally correlated with less intention to use PrEP (p = .052). Greater expected PrEP disapproval by others was correlated with less PrEP interest, less PrEP intention, and less comfort discussing PrEP with a provider (p < .050).
Table 2.
PrEP Stigma Subscale Means, Standard Deviations, and Bivariate Correlations with PrEP Uptake Indicators
| Pearson Correlation Coefficient (r)
|
|||||||
|---|---|---|---|---|---|---|---|
| Measurea | n | Mean (SD) | 1 | 2 | 3 | 4 | 5 |
| 1 PrEP-User Stereotypes | 596 | 1.98 (.70) | – | ||||
| 2 PrEP Disapproval by Others | 596 | 2.24 (.81) | .20** | – | |||
| 3 PrEP Interest | 596 | 2.28 (1.20) | −.10* | −.20** | – | ||
| 4 Intention to Use PrEP | 597 | 2.89 (1.36) | −.08† | −.21** | .46** | – | |
| 5 Comfort Discussing PrEP with a Provider | 597 | 3.51 (1.22) | −.25** | −.23** | .25** | .20** | – |
PrEP-User Stereotypes and PrEP Disapproval by Others represent subscale scores with theoretical and empirical ranges of 1 to 4. PrEP Interest, Intention to Use PrEP, and Comfort Discussing PrEP with a Provider represent single-item scores with theoretical and empirical ranges of 1 to 5.
p < .10
p < .05
p < .01
Table 3 presents partial, conditional, and interaction effects of PrEP-user stereotypes and PrEP disapproval by others on the three outcomes. With respect to our first outcome, interest in learning more about PrEP, the two PrEP stigma subscales added in Model 2 accounted for an additional 3% of the variance beyond the 10% captured by background characteristics in Model 1. Greater expected PrEP disapproval by others was uniquely associated with less PrEP interest. In Model 3, no interaction effect was detected.
Table 3.
Linear Regression Models of Partial, Conditional, and Interaction Effects of Two Dimensions of PrEP Stigma
| PrEP Interest
|
Intention to Use PrEP
|
Comfort Discussing PrEP with a Provider
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variablea | b | SE | p | b | SE | p | b | SE | p |
| Partial Effects Modelb | |||||||||
| PrEP-User Stereotypes | −.13 | .07 | .066 | −.11 | .08 | .158 | −.37 | .07 | <.001 |
| PrEP Disapproval by Others | −.24 | .06 | <.001 | −.28 | .07 | <.001 | −.34 | .06 | <.001 |
|
| |||||||||
| Conditional and Interaction Effects Modelb | |||||||||
| PrEP-User Stereotypes | −.13 | .07 | .065 | −.12 | .08 | .142 | −.36 | .07 | <.001 |
| PrEP Disapproval by Others | −.24 | .06 | <.001 | −.25 | .07 | <.001 | −.35 | .06 | <.001 |
| PrEP-User Stereotypes × PrEP Disapproval by Others | .02 | .07 | .733 | .18 | .08 | .029 | −.11 | .07 | .107 |
PrEP-User Stereotypes and PrEP Disapproval by Others were mean-centered for interpretation of conditional effects
Models were adjusted for background characteristics (age, ethnicity, race, sexual orientation, education, employment status, annual household income, geographic location, number of sex partners, condom use consistency, partnership status, perceived HIV risk, and familiarity with PrEP).
With respect to our second outcome, intention to use PrEP, the two PrEP stigma subscales added in Model 2 accounted for an additional 3% of the variance beyond the 7% captured by background characteristics in Model 1. Greater expected PrEP disapproval by others was uniquely associated with less intention to use PrEP. In Model 3, a significant interaction was detected (p = .029; see Figure 2). Probing the interaction, we found that perception of PrEP-user stereotypes was not associated with intention to use PrEP among participants who expected moderate or higher levels of PrEP disapproval by others (≥1.97 mean score on 1-4 response scale; reported by 79% of the sample); however, among participants who reported lower levels of perceived PrEP disapproval by others (i.e., reported perceiving higher levels of PrEP approval by others), stronger perception of PrEP-user stereotypes was associated with less intention to use PrEP. Intention to use PrEP was greatest when participants anticipated low levels of both PrEP-user stereotypes and PrEP disapproval by others.
Figure 2. Interaction Effect.
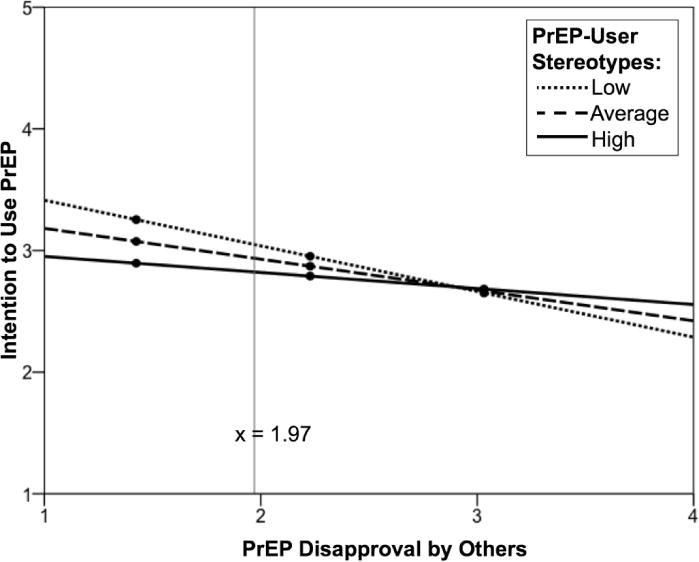
Effect of PrEP disapproval by others on intention to use PrEP as moderated by PrEP-user stereotypes. The model was adjusted for relevant background characteristics (age, ethnicity, race, sexual orientation, education, employment status, annual household income, geographic location, number of sex partners, condom use consistency, partnership status, perceived HIV risk, and familiarity with PrEP). High and low values of PrEP-user stereotypes represent one standard deviation above and below the mean level, respectively. Graphed x-values span the original 1-4 response range (i.e., values were not mean-centered). The gray vertical line indicates the threshold below which intention to use PrEP significantly differs by level of stereotype endorsement. The figure shows that intention to use PrEP was greatest when perceived PrEP-user stereotypes and PrEP disapproval by others were both low.
With respect to our third outcome, comfort discussing PrEP with a provider, the two PrEP stigma subscales added in Model 2 accounted for an additional 11% of the variance beyond the 2% captured by background characteristics in Model 1. Stronger perception of PrEP-user stereotypes and greater expected PrEP disapproval by others were both uniquely associated with less comfort discussing PrEP with a provider. In Model 3, no interaction effect was detected.
DISCUSSION
Our results demonstrate that perceived PrEP-user stereotypes and expected PrEP disapproval by others could deter women’s PrEP uptake. When considered concurrently, the two dimensions of PrEP stigma were additively associated with less comfort discussing PrEP with a provider. PrEP disapproval by others was also uniquely associated with less PrEP interest and less intention to use PrEP. Exploratory analyses indicated that the two stigma dimensions may interactively affect intention to use PrEP, underscoring the value of addressing both.
Beyond stigma, our study also revealed widespread unawareness about PrEP: Only 23% of participants reported having heard of PrEP prior to the survey. This low level of PrEP familiarity is notable because our data were collected in 2017, five years after US federal approval of PrEP, and our sample consisted of women who recently visited Planned Parenthood. Furthermore, the health centers from which participants were recruited were located in Connecticut cities in which the state health department had previously launched PrEP public awareness campaigns, including advertisements targeting women [32]. Thus, even fewer women may be aware of PrEP in neighboring regions.
PrEP Messaging Considerations
Collectively, our findings suggest a need to broaden the reach of PrEP messaging to women and include message content that counters PrEP stigma. Some participants who were newly introduced to PrEP during the survey anticipated PrEP stigma even though they were provided with only basic factual information about PrEP prior to viewing the stigma items, perhaps due to heightened suggestibility in the absence of pre-existing knowledge. However, unlike previous research with MSM associating greater PrEP awareness with lower PrEP stigma [11], both dimensions of PrEP stigma were just as high among women with prior awareness of PrEP. Message-framing strategies that effectively address PrEP stigma among women with varying levels of PrEP knowledge are needed.
PrEP messaging should target not only potential PrEP users, but their social networks as well. Both PrEP stigma subscales in this study measured anticipated PrEP stigma, assessing perceived stereotype endorsement and expected disapproval by others. Therefore, results suggest that other people’s beliefs about PrEP can play a key role in an individual’s personal decision to pursue PrEP. Promoting community visibility and public discourse may help to foster norms of acceptance and decrease the likelihood of PrEP candidates anticipating negative reactions from others.
PrEP Messaging and Education in Healthcare Settings
Both PrEP stigma subscales were uniquely associated with comfort discussing PrEP with a provider and accounted for the most variance in this PrEP uptake indicator of all three, suggesting that PrEP messaging could be particularly influential in healthcare settings. Such messaging includes information explicitly communicated by providers as well as indirect messages conveyed, for example, through educational pamphlets and closed-circuit videos presented in waiting areas.
PrEP messaging by providers can be cultivated through direct medical training. Such training should encourage providers to conceptualize PrEP as a tool that empowers patients to take control of their sexual health [33]. Framing it as an intervention for patients “at very high risk” stigmatizes PrEP and potential PrEP users [33]. Training should instruct providers to ask open-ended questions about patients’ sexual health concerns and goals rather than relying on traditional risk assessment tools, which can alienate patients and fail to identify prospective PrEP candidates [33,34].
The regularity with which PrEP is discussed and offered to patients in healthcare settings can also convey meaning and affect stigma. Integrating conversations about PrEP into routine preventive healthcare would help to raise awareness among patients and their social networks and normalize PrEP discussion and use [34]. Most survey participants expressed some interest in learning about PrEP, and about a third intended to use PrEP if it were made freely available—supporting a broad-based approach to PrEP education.
Patient education about PrEP should be embedded in more comprehensive conversations about HIV prevention and sexual health. The majority (90%) of study participants reported using condoms inconsistently if at all. Federal clinical guidance [35] lists “history of inconsistent or no condom use” among the indicators of substantial sexual risk for HIV acquisition (p. 13), suggesting at least 90% of our sample could be considered as candidates for PrEP, and likely more given other risk indicators (e.g., high number of sex partners). However, considerably fewer (21%) perceived any risk of acquiring HIV in their lifetime, indicating potential underestimation of HIV risk. Incongruence between risk behavior and risk perception has been reported among female reproductive healthcare patients elsewhere and underscores the need for further sexual health education with this population [36].
Limitations and Other Considerations
Our sample included women who accessed medical services at Connecticut Planned Parenthood centers, where PrEP is available to patients. It is not representative of all US women, and findings should not be assumed to generalize to women who are not engaged in care or who receive care in settings where PrEP availability is constrained.
Our use of a quantitative design—though advantageous in capturing the attitudes of a large sample and allowing for broader inference—limited the range of PrEP-user stereotypes we explored to a pre-defined list with close-ended response options. Because these items were developed from PrEP stigma literature primarily involving men, anticipated stereotypes of particular salience to women may not have been captured. For example, women have reported anticipating their male partners would associate their PrEP use with infidelity and mistrust [22]. Qualitative research could help to uncover additional nuances in women’s impressions of PrEP users and concerns surrounding the impressions of others. Qualitative methods may be more sensitive to unique manifestations of stigma among subgroups of women who are disproportionately affected by HIV, such as women of color. Whereas our measure did not detect racial or ethnic differences in anticipated PrEP stigma, several studies have reported race-based differences in PrEP stigma among MSM [6,11], inviting a more in-depth analysis with women.
We also limited our study of PrEP stigma to anticipated PrEP stigma (i.e., expected stereotyping and disapproval by others) and identified two dimensions. We acknowledge, however, that there are other dimensions of PrEP stigma that could play a systematic role in PrEP uptake [16,37]. Personal endorsement of PrEP-user stereotypes, for example, was not captured, but it could be assessed in the future with other PrEP stigma instruments (e.g., PrEP Stigma and Positive Attitudes scale [11]). We encourage exploration of multiple stigma dimensions and their combined effects on PrEP attitudinal and behavioral outcomes in future research.
Conclusion
PrEP is a promising prevention tool that offers immense benefit to women and others at risk for HIV. However, it is only as promising as it is accessible. Addressing PrEP stigma and other psychosocial hurdles is essential to enabling such access in the years to come.
Supplementary Material
Acknowledgments
The authors wish to thank the Planned Parenthood patients who generously contributed their time and effort by participating in this study. We are grateful to Ms. Susan Lane for her help with data collection and other facets of the study. We appreciate the funding and resources provided by the Center for Interdisciplinary Research on AIDS (CIRA) Pilot Projects in HIV Program at Yale University. CIRA is funded by the National Institute of Mental Health (NIMH) via Award Number P30-MH062294. Effort was supported by the NIMH via Award Numbers K01-MH103080 (SKC), T32-MH02003 (TT), and F31-MH113508 (TCW). Additional support for TT was provided by the National Institute on Drug Abuse (NIDA) via the HIV/AIDS, Substance Abuse, and Trauma Training Program at the University of California, Los Angeles (R25-DA035692). Additional support for TCW was provided by the Brown Initiative in HIV and AIDS Clinical Research for Minority Communities (R25-MH083620). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH, NIDA, National Institutes of Health (NIH), or Planned Parenthood Federation of America, Inc.
Sources of Support: Funding for this research was provided by the Yale University Center for Interdisciplinary Research on AIDS and the National Institute of Mental Health (NIMH) via Award Number P30-MH062294. SKC was supported by the NIMH via Award Number K01-MH103080. TT was supported by the NIMH and the National Institute on Drug Abuse (NIDA) via Award Numbers T32-MH020031 and R25-DA035692, respectively. TCW was supported by the NIMH via Award Numbers F31-MH113508 and R25-MH083620. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH, NIDA, National Institutes of Health (NIH), or Planned Parenthood Federation of America, Inc.
Footnotes
Prior Presentation of Data: Some of the results presented in this manuscript were presented at the 12th International Conference on HIV Treatment and Prevention Adherence (Miami, FL; 6/04/17) and the CFAR Social and Behavioral Sciences Network 2017 Annual Meeting (San Francisco, CA; 10/24/17).
References
- 1.Smith DK, Van Handel M, Grey JA. Presented at: Conference on Retroviruses and Opportunistic Infections (CROI 2018) Boston, USA: 2018. By race/ethnicity, Blacks have highest number needing PrEP in the United States [Abstract 86] [Google Scholar]
- 2.Mera Giler R, Magnuson D, Trevor H, et al. Presented at: 9th International AIDS Society Conference on HIV Science (IAS 2017) Paris, France: 2017. Changes in Truvada (TVD) for HIV pre-exposure prophylaxis (PrEP) utilization in the United States: (2012-2016) [Abstract 1614] [Google Scholar]
- 3.Mera R, McCallister S, Palmer B, et al. Presented at: International AIDS Conference (AIDS 2016) Durban, South Africa: 2016. Truvada (TVD) for HIV pre-exposure prophylaxis (PrEP) utilization in the United States (2013-2015) [Abstract TUAX0105LB] [Google Scholar]
- 4.Hess KL, Hu X, Lansky A, Mermin J, Hall HI. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27:238–243. doi: 10.1016/j.annepidem.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bush S, Magnuson D, Rawlings MK, Hawkins T, McCallister S, Mera Giler R. Presented at: ASM Microbe. Boston, USA: 2016. Racial characteristics of FTC/TDF for preexposure prophylaxis (PrEP) users in the US [Abstract 2651] [Google Scholar]
- 6.Golub SA, Gamarel KE, Surace A. Demographic differences in PrEP-related stereotypes: Implications for implementation. AIDS Behav. 2017;21:1229–1235. doi: 10.1007/s10461-015-1129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mutchler MG, McDavitt B, Ghani MA, et al. Getting PrEPared for HIV prevention navigation: Young Black gay men talk about HIV prevention in the biomedical era. AIDS Patient Care STDS. 2015;29:490–502. doi: 10.1089/apc.2015.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Underhill K, Guthrie K, Operario D, et al. Presented at: 2016 International AIDS Conference (AIDS 2016) Durban, South Africa: 2017. A qualitative study of PrEP stigma, pride and predicted community benefits among MSM and male sex workers [Abstract THPED417] [Google Scholar]
- 9.Eaton LA, Kalichman SC, Price D, et al. Stigma and conspiracy beliefs related to pre-exposure prophylaxis (PrEP) and interest in using PrEP among Black and White men and transgender women who have sex with men. AIDS Behav. 2017;21:1236–1246. doi: 10.1007/s10461-017-1690-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnold T, Brinkley-Rubinstein L, Chan PA, et al. Social, structural, behavioral, and clinical factors influencing retention in pre-exposure prophylaxis (PrEP) care in Mississippi. PLoS ONE. 2017;12:e0172354. doi: 10.1371/journal.pone.0172354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mustanski B, Ryan DT, Hayford C, Phillips G, II, Newcomb ME, Smith JD. Geographic and individual associations with PrEP stigma: Results from the RADAR cohort of diverse young men who have sex with men and transgender women [published online ahead of print May 22, 2018] AIDS and Behavior. doi: 10.1007/s10461-018-2159-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Storholm E, Volk JE, Marcus JL, et al. Risk perceptions, sexual behaviors, and PrEP adherence among substance-using men who have sex with men: A qualitative study. Prev Sci. 2017;18:737–747. doi: 10.1007/s11121-017-0799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lelutiu-Weinberger C, Golub SA. Enhancing PrEP access for Black and Latino men who have sex with men. J Acquir Immune Defic Syndr. 2016;73:547–555. doi: 10.1097/QAI.0000000000001140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu A, Cohen S, Follansbee S, et al. Early experiences implementing pre-exposure prophylaxis (PrEP) for HIV prevention in San Francisco. PLoS Med. 2014;11:e1001613. doi: 10.1371/journal.pmed.1001613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia J, Parker C, Parker RG, et al. Psychosocial implications of homophobia and HIV stigma in social support networks: Insights for high-impact HIV prevention among Black men who have sex with men. Health Educ Behav. 2016;43:217–225. doi: 10.1177/1090198115599398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haire BG. Preexposure prophylaxis-related stigma: Strategies to improve uptake and adherence – a narrative review. HIV AIDS. 2015;7:241–249. doi: 10.2147/HIV.S72419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farhat D, Greene E, Paige MQ, et al. Knowledge, stereotyped beliefs and attitudes around HIV chemoprophylaxis in two high HIV prevalence neighborhoods in New York City. AIDS Behav. 2017;21:1247–1255. doi: 10.1007/s10461-016-1426-6. [DOI] [PubMed] [Google Scholar]
- 18.Collier KL, Colarossi LG, Sanders K. Raising awareness of pre-exposure prophylaxis (PrEP) among women in New York City: Community and provider perspectives. J Health Commun. 2017;22:183–189. doi: 10.1080/10810730.2016.1261969. [DOI] [PubMed] [Google Scholar]
- 19.Patel RC, Stanford-Moore G, Odoyo J, et al. “Since both of us are using antiretrovirals, we have been supportive to each other”: Facilitators and barriers of pre-exposure prophylaxis use in heterosexual HIV serodiscordant couples in Kisumu, Kenya. J Int AIDS Soc. 2016;19:21134. doi: 10.7448/IAS.19.1.21134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van der Straten A, Stadler J, Luecke E, et al. Perspectives on use of oral and vaginal antiretrovirals for HIV prevention: The VOICE-C qualitative study in Johannesburg, South Africa. J Int AIDS Soc. 2014;17:19146. doi: 10.7448/IAS.17.3.19146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Auerbach JD, Kinsky S, Brown G, et al. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS. 2015;29:102–110. doi: 10.1089/apc.2014.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goparaju L, Praschan NC, Warren-Jeanpiere L, et al. Stigma, partners, providers and costs: Potential barriers to PrEP uptake among US women. J AIDS Clin Res. 2017:8. doi: 10.4172/2155-6113.1000730. [epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Planned Parenthood Federation of America. 2016-2017 Annual Report. Retrieved 25 January 2018 from https://www.plannedparenthood.org/uploads/filer_public/d4/50/d450c016-a6a9-4455-bf7f-711067db5ff7/20171229_ar16-17_p01_lowres.pdf.
- 24.Fowler CI, Gable J, Wang J, et al. Title X Family Planning Annual Report: 2016 National Summary. Retrieved 25 January 2018 from https://www.hhs.gov/opa/sites/default/files/title-x-fpar-2016-national.pdf.
- 25.Parsons JT, Rendina HJ, Lassiter JM, et al. Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States: The Motivational PrEP Cascade. J Acquir Immune Defic Syndr. 2017;74:285–292. doi: 10.1097/QAI.0000000000001251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelley CF, Kahle E, Siegler A, et al. Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2015;61:1590–1597. doi: 10.1093/cid/civ664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Connecticut Department of Public Health. HIV Statistics. Retrieved 8 January 2018 from http://portal.ct.gov/DPH/AIDS–Chronic-Diseases/Surveillance/QuickStats.
- 28.Sayles JN, Wong MD, Kinsler JJ, et al. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24:1101–1108. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brigham JC. Ethnic stereotypes. Psychological Bulletin. 1971;76:15–38. [Google Scholar]
- 30.Gamarel KE, Golub SA. Intimacy motivations and pre-exposure prophylaxis (PrEP) adoption intentions among HIV-negative men who have sex with men (MSM) in romantic relationships. Ann Behav Med. 2015;49:177–186. doi: 10.1007/s12160-014-9646-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis. New York: Guilford Press; 2013. [Google Scholar]
- 32.Connecticut Department of Public Health. Personal communication. 2018 Jan 16; [Google Scholar]
- 33.Golub SA. PrEP stigma: Implicit and explicit drivers of disparity. Curr HIV/AIDS Rep. 2018;15:190–197. doi: 10.1007/s11904-018-0385-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Calabrese SK, Krakower DS, Mayer KH. Integrating HIV pre-exposure prophylaxis (PrEP) into routine preventive healthcare to avoid exacerbating disparities. Am J Public Health. 2017;107:1883–1889. doi: 10.2105/AJPH.2017.304061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: A clinical practice guideline. Retrieved 02 May 2018 from https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf.
- 36.Garfinkel DB, Alexander KA, McDonald-Mosley R, et al. Predictors of HIV-related risk perception and PrEP acceptability among young adult female family planning patients. AIDS Care. 2017;29:751–758. doi: 10.1080/09540121.2016.1234679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Major B, Dovidio JF, Link BG, et al. Stigma and its implications for health: Introduction and overview. In: Major B, Dovidio JF, Link B, editors. The Oxford handbook of stigma, discrimination and health. New York, NY: Oxford University Press; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.