Abstract
Objective
To evaluate changes in neuropsychological (NP) performance and in plasma and cell surface markers of peripheral monocyte activation/migration following treatment with cenicriviroc (CVC), a dual C-C chemokine receptor type 2 (CCR2) and type 5 (CCR5) antagonist, in treatment-experienced, HIV-infected individuals.
Setting
Single-arm, 24-week, open-label clinical trial.
Methods
HIV-infected individuals on antiretroviral therapy (ART) ≥1 year with plasma HIV RNA ≤50 copies/ml and below-normal cognitive performance [defined as age, gender and education-adjusted NP performance (NPZ) <−0.5 in a single cognitive domain or in global performance] were enrolled. Changes over 24 weeks were assessed for global and domain-specific NPZ scores, plasma markers of monocyte/macrophage activation [neopterin, soluble (s)CD14 and sCD163] quantified by ELISA, and CCR2 and CCR5 expression on monocytes and T cells measured by flow cytometry.
Results
Seventeen of 20 enrolled participants completed the study. Improvements over 24 weeks were observed in global NPZ [median change (Δ)=0.24; p=0.008], and in cognitive domains of attention (Δ0.23; p=0.011) and working memory (Δ0.44; p=0.017). Plasma levels of sCD163, sCD14 and neopterin decreased significantly (p’s<0.01). CCR2 and CCR5 monocyte expression remained unchanged; however, CCR5 levels on CD4+ and CD8+ T cells and CCR2 expression on CD4+ T cells increased (p’s<0.01).
Conclusions
CVC given over 24 weeks was associated with improved NP test performance and decreased plasma markers of monocyte immune activation in virally-suppressed, HIV-infected participants. These data potentially link changes in monocyte activation to cognitive performance. Further study of CVC for HIV cognitive impairment in a randomized controlled study is warranted.
Keywords: C-C chemokine receptor type 2 and 5 (CCR2 and CCR5), monocytes, HIV, antiretroviral therapy (ART), cognitive impairment, clinical trials
INTRODUCTION
Neurocognitive performance is compromised in approximately 30-50% of chronically HIV-infected individuals despite treatment with virally-suppressive antiretroviral therapy (ART).1,2 Cognitive dysfunction negatively impacts daily function, quality of life, and increases morbidity and mortality.3–5 At present, clinically approved therapies for HIV-associated cognitive impairment do not exist.6
The neuropathogenesis of HIV-associated cognitive impairment has not been completely defined but it is generally hypothesized that transmigration of HIV-infected monocytes into the central nervous system (CNS) provides entry of HIV into the brain and establishes a neuroinflammatory process that disrupts brain integrity and function.7–12 Persistent immune activation, driven in part by activated monocytes, is believed to be a major component of HIV neuropathogenesis.13 Monocyte/macrophage mediators such as soluble (s)CD163, monocyte chemoattractant protein (MCP)-1 and interleukin (IL)-6, have been linked to reduced cognitive performance among individuals on ART.9–11,14–16 Combined, these myeloid features represent a potential target for the treatment of cognitive dysfunction among individuals on ART.
Maraviroc (MVC), a C-C chemokine receptor type 5 (CCR5) antagonist, is FDA-approved as an antiretroviral medication to be used with other antiretroviral agents in CCR5-tropic HIV-infected individuals. MVC has been associated with improved cognitive performance and reduction of plasma markers of monocyte activation.17–19 In a previous single arm, open-label, 24-week study of MVC intensification in ART-treated, chronically infected individuals, we demonstrated improved cognitive performance, reductions in HIV DNA levels in monocytes and in sCD163 levels, a plasma marker of monocyte activation.17 These data provide a platform for targeting chemokine receptors (CKRs) to improve cognitive performance in HIV-infected individuals.
The MCP-1/CCR2 axis has also been associated with cognitive dysfunction. In ART-naïve HIV-infected Thai individuals, lower numbers of circulating activated monocytes expressing CCR2 were linked to worse cognitive performance.20 Reduced numbers of CCR2 expressing monocytes in the periphery suggest preferential trafficking of these cells into the brain towards MCP-1, a potent inducer of monocyte migration21–24, contributing to neuroinflammation and reduced cognitive function.9,21 Given the involvement of CCR2 and CCR5 in HIV-related cognitive dysfunction, pharmacotherapeutic strategies that target both CKRs may be more effective than inhibiting a single CKR.
Cenicriviroc (CVC) is an oral, dual CCR2 and CCR5 antagonist with nanomolar potency and a long plasma half-life25–27 currently in Phase 3 evaluation for treatment of liver fibrosis in adults with nonalcoholic steatohepatitis (NCT03028740). In the Phase 2b CENTAUR study 652-2-203 (NCT0221747528), one year of CVC treatment led to twice as many participants achieving improvement in fibrosis and no worsening of steatohepatitis when compared to placebo.29 CVC has also demonstrated anti-inflammatory and anti-fibrotic activity in animal models of liver disease, which was largely attributed to decreased monocyte/macrophage infiltration into the liver following hepatocyte injury.30–32 In a Phase 2b clinical trial (NCT01338883) in ART-naïve, HIV-infected individuals, CVC decreased viremia and sCD14 levels (marker of monocyte/macrophage activation).33 In an ex vivo study, CVC decreased HIV entry into peripheral blood mononuclear cells (PBMCs).34 Considering the role of monocyte inflammation and migration into the CNS in the neuropathogenesis of HIV, we hypothesized that CCR2 and CCR5 blockade would improve cognitive function by decreasing monocyte activation and migration into the CNS.
METHODS
Study Design
The study was approved by the University of Hawaii Human Subjects Program, received clearance to proceed from the Food and Drug Administration (FDA) [IND 119671], and was registered at ClinicalTrials.gov (NCT02128828). Twenty chronically-infected aviremic (HIV RNA <50 copies/ml) individuals ages 18 to 70 years on uninterrupted ART for >1 year were enrolled into the single-arm, open label, 24 week pilot study. Participants were required to be on the same ART regimen for at least 6 months prior to entry. Below-normal cognitive performance was defined as performance of <−0.5 standard deviation (SD) below published normative standards in a cognitive domain or global cognitive performance (NPZ Global). Exclusion criteria included currently receiving or having used a CCR5 antagonist as part of an ART regimen within 6 months of entry, on-going need for use of medications known to have unacceptable drug-drug interactions with CVC (provided by the manufacturer of CVC), history of plasma HIV RNA >100 copies/ml within 6 months of screening, chronic hepatitis B or C or diagnosis of any other active or chronic liver disease, chronic uncontrolled seizures or significant past history of central nervous system disease or head trauma, depression (Beck Depression Inventory-II total score >29), chronic illnesses or cancers except for stable treated hypogonadism or hypothyroidism, unstable cardiovascular or cerebrovascular disease, or the following abnormal lab values: hemoglobin <8.5 g/dL, absolute neutrophil count <1000/μL, platelet count <100,000/μL, AST and ALT ≥2.5 upper limit of normal (ULN), lipase >2.0 × ULN, estimated creatinine clearance by the Cockcroft-Gault Equation ≤30 mL/min, and bradycardia (<50 beats/min).
All study visits were conducted at a single site at the University of Hawaii (UH) Clinics at Kaka’ako. Following written informed consent and screening, CVC was administered once-daily with food in dosage adjusted for each participant’s ART regimen and other medications as per the manufacturer’s recommendations. Individuals with ART regimen consisting of a nucleoside reverse transcriptase inhibitor (NRTI) and unboosted/boosted atazanavir or boosted darunavir received 50 mg (1 tablet) of CVC, individuals taking dolutegravir or raltegravir-based ART received 200 mg (4 tablets) of CVC, and individuals receiving efavirenz received 400 mg (8 tablets) daily. Research bloods were drawn at entry and at weeks 4, 8, 12, and 24.
Neuropsychological Evaluation
Neuropsychological (NP) testing was conducted at entry and week 24 by trained psychometrists. Testing was conducted in a quiet room and participants were provided breaks as needed throughout the testing sessions. The test battery (Table 1) was comprised of measures known to be sensitive to HIV-related infection including: attention (A); working memory (WM); psychomotor speed (PM); visuospatial reasoning (VPR); executive function (EF); learning and memory (LM) and gross motor (GM).35,36 Raw scores were converted into standardized z-scores according to demographically-adjusted norms.37,38 Global cognitive function (Global NPZ) was defined by aggregating the domain specific NP Z-scores.
Table 1. Tests comprising each cognitive subdomain.
| Attention | CalCap Choice | |
| CalCap Sequential | ||
| Digit Span Total | ||
|
| ||
| Working Memory | Digit Span Backward | |
| CVLT B | ||
| Letter Number Sequencing | ||
|
| ||
| Psychomotor Speed | Digit Symbol | |
| Trail A | ||
| Grooved Pegboard (GP) Dominant Hand (Dom) | ||
| GP NonDom | ||
|
| ||
| Visuospatial Reasoning | Rey Copy | |
| Block Design | ||
|
| ||
| Executive Function | Verbal Fluency Test (FAS) | |
| Stroop | ||
| Trail B | ||
| Action | ||
|
| ||
| Learning and Memory | California Verbal Learning Test (CVLT) Total | |
| CVLT Long-Delay Free Recal | ||
| Brief Visuospatial Memory Test (BVMT) Total | ||
| BVMT Delay | ||
|
| ||
| Gross Motor | Timed Gait | |
| Finger Tapping – Dom | ||
| Finger Tapping – NonDom | ||
Assessments of Plasma Derived Soluble Biomarkers
Plasma sCD163, sCD14 and neopterin were quantified at entry and weeks 8, 12 and 24 by single analyte ELISA array (Trillium Diagnostics; Bangor, ME; R&D Systems, Minneapolis, MN and Thermo Scientific, Waltham, MA, respectively).
Quantification of Monocyte and T Cell Subset Frequencies and CKR Expression
Monocyte and T cell subpopulations were measured at entry and week 24 after CVC by flow cytometry. Briefly cryopreserved PBMCs were placed in 96 well polypropylene round bottom plates and stained with Live/Dead® Fixable Red Dead Cell Stain (Invitrogen, Carlsbad, CA) for 15 min at room temperature followed by two, 10 min sequential incubations with conjugated monoclonal antibodies (mAbs) against CCR2 (AlexaFluor647, Catalog Number [Cat] 558406) and CCR5 (Phycoerythrin (PE), Cat 555993) at 37 ºC.39 Cells were then stained at room temperature for 30 min with mAbs against CD3 (Brilliant Violet (BV) 711, Cat 317328), CD4 (peridinin chlorophyll protein) PerCP-Cyanine (Cy)5.5, Cat 300530), CD8 (PE-Cy5, Cat 555368), CD14 (AlexaFluor700, Cat 557923), CD16 (BV421; Cat 343113), CD7 (PE-Cy7, Cat 343113), CD19 (PE-Cy7, Cat 557835), CD20 (PE-Cy7, Cat 560735), CD11b (AlexaFluor488, Cat 557701) and human leukocyte antigen-D related (HLA-DR) (Allophycocyanin (APC)-H7, Cat 561358). Cells were fixed with 1% PFA and data were acquired on a custom 4-laser BD LSRFortessa (BD Bioscience, San Jose, CA). Compensation and gating analyses were performed using FlowJo (FlowJo LCC, Ashland, OR). All mAbs were purchased from BD Bioscience (San Jose, CA) except for Live/Dead Stain (Invitrogen, Carlsbad, CA), and CD3-BV711, CD4-PerCP-Cy5.5 and CD16-BV421 (BioLegend, San Diego, CA). The gating strategy for identification of CD4+ and CD8+ T cells, and monocyte subsets, along with CKR expression is shown in Supplemental Figure 1. Median viability for the frozen PBMC samples was 93.8% (interquartile range 25th–75th [IQR]: 89.7-96.1%). Samples were excluded if the viability was below 80%.
Monocyte subset counts were calculated by multiplying monocyte number (Mono/μl) from the white blood cell count obtained from the clinical laboratory values and the percent frequency generated by flow cytometry. CD4+ and CD8+ T cell counts were obtained from the white blood cell count.
Statistical Analyses
Descriptive statistics for all continuous and categorical variables are reported as median (IQR) and n (percent), respectively. Wilcoxon Signed Rank test was used to assess changes from entry to week 24 and Spearman correlation was used to assess the relationship between continuous variables. The magnitude of change from entry to week 24 in NP testing was examined in relation to the standard error of measurement (SEM) estimates where applicable based on prior studies.40 All statistical analyses were performed using SAS version 9.4 (Cary, NC: SAS Institute Inc. 2002-2012). A two-sided p-value <0.05 was regarded as statistically significant for all tests, while p-values between 0.05 and 0.1 were reported as trends.
RESULTS
Study Participant Clinical and Demographic Characteristics
Seventeen of the 20 enrolled participants completed the study. One participant withdrew from the study due to grade 1 nausea, and 2 participants left the study for non-medical personal issues. Baseline participant characteristics of the 17 participants who completed the study are found in Table 2. The participants were generally older, male except for one participant, with a long history of living with HIV and being on ART. Of the 17 participants, 6 were on dual NRTIs (all on tenofovir/emtricitabine) and protease inhibitor (PI) regimens utilizing boosted atazanavir or boosted darunavir; 7 were on dual NRTIs (either tenofovir/emtricitabine or abacavir/lamivudine) and Integrase Inhibitor (INSTI) therapy with either dolutegravir or raltegravir; and one was on a dual NRTI (tenofovir/emtricitabine) and a non-nucleoside reverse transcriptase inhibitor (NNRTI, efavirenz). The other 3 patients were on less common regimens consisting of a triple NRTI regimen (zidovudine, lamivudine and abacavir); triple NRTI (tenofovir, emtricitabine, abacavir) plus an NNRTI (efavirenz); and dual NRTI (tenofovir, emtricitabine) plus a PI (darunavir) and an INSTI (raltegravir).
Table 2.
Participant characteristics at entry
| Baseline Characteristics (n=17) | |
|---|---|
| Gender, male | 16 (94%) |
| Caucasian | 7 (41%) |
| Asian/Pacific Islander | 6 (35%) |
| Other Ethnicity | 4 (24%) |
| Age, years | 55 (47, 58) |
| Education, years | 15 (14, 16) |
| CD4 Nadir*, cells/mm3 | 200 (90, 280) |
| CD4 Count, cells/mm3 | 545 (404, 731) |
| CD4/CD8 Ratio | 0.85 (0.55, 0.97) |
| Time on ART*Ɨ | 15.5 (6.7, 19.5) |
| Years Infected* | 21 (14, 25) |
| NRTI Use | 17 (100%) |
| NNRTI Use | 2 (12%) |
| PI Use | 7 (41%) |
| INSTI Use | 8 (47%) |
Median (IQR) presented for continuous variables, N (%) presented for categorical variables.
Self-Reported.
N = 13.
CVC Tolerance by Study Participants
A total of 58 clinical adverse events were observed in 14 participants (n=49, grade 1 and n=9, grade 2). Grade 2 clinical adverse events included: loose stools (n=2; 10%), nausea (n=1; 5%), abdominal cramps (n=1; 5%), and fatigue (n=1; 5%). Additionally, 17 laboratory adverse events were reported in 6 participants while on study drug (n=13 grade 1; n=2 grade 2 and n=2 grade 3). The grade 2 adverse events included elevated lipase and creatinine. The grade 3 adverse events included asymptomatic elevated lipase at weeks 24 and 28, both of unclear relationship to CVC. Average/overall compliance was 95%. The lowest compliance recorded in a patient was 65% between weeks 4 and 8. At all other time points recorded, compliance was at least 80%.
Changes in Neuropsychological Performance after CVC Treatment
After 24 weeks, significant improvements were noted in Global NPZ, attention and working memory (Table 3; Figure 1). Trends towards improved psychomotor speed and visuospatial performance were also observed (Table 3; Figure 1). No significant changes were seen in executive function, learning and memory, or gross motor (Table 3; Figure 1).
Table 3.
Clinical and experimental data before and after cenicriviroc
| Entry | Week 24 | p Value | |
|---|---|---|---|
| Cognitive Domain (NPZ Score) | |||
|
| |||
| Global | −0.14 [−0.52, 0.08] | −0.03 [−0.19, 0.29] | 0.008 |
| Attention | −0.93 [−1.42, −0.21] | −0.74 [−1.02, 0.08] | 0.011 |
| Working Memory | −0.50 [−0.72, −0.22] | −0.22 [−0.56, 0.28] | 0.017 |
| Psychomotor Speed | 0.09 [−0.26, 0.55] | 0.41 [−0.03, 0.73] | 0.080 |
| Visuospatial Reasoning | −0.17 [−0.75, 0.41] | 0.33 [−0.41, 0.66] | 0.084 |
| Executive Function | 0.40 [−0.23, 0.96] | 0.48 [−0.29, 1.07] | 0.207 |
| Learning and Memory | 0.03 [−0.98, 0.40] | 0.23 [−0.35, 0.50] | 0.431 |
| Gross Motor | −0.61 [−1.08, 0.26] | −0.48 [−1.21, 0.06] | 0.712 |
|
| |||
| Soluble Monocyte Activation Markers (ng/ml) | |||
|
| |||
| sCD163 | 2.91 [2.00, 4.04] | 1.78 [1.38, 2.34] | 0.001 |
| sCD14 | 8.28 [7.76, 9.34] | 7.28 [6.90, 8.24] | 0.003 |
| Neopterin | 3.69 [3.13, 5.00] | 2.43 [1.98, 3.62] | <0.001 |
|
| |||
| Leukocyte Counts (Cells/ul) | |||
|
| |||
| Total Monocyte Count | 42 [34, 61] | 36 [27, 46] | 0.001 |
| Classical Monocyte Count | 36 [29, 51] | 34 [25, 44] | 0.016 |
| Intermediate Monocyte Count | 0.36 [0.14, 1.0] | 0.47 [0.26, 0.65] | >0.999 |
| Non-Classical Monocyte Count | 1.0 [0.55, 2.1] | 1.2 [0.90, 1.5] | 0.470 |
| CD4+ T Cell Count | 545 [404, 731] | 732 [397, 900] | 0.030 |
| CD8+ T Cell Count | 856 [476, 1192] | 1028 [739, 1229] | 0.035 |
| CD4+/CD8+ T Cell Ratio | 0.85 [0.55, 0.97] | 0.74 [0.48, 0.95] | 0.110 |
|
| |||
| Chemokine Receptor Expression (Geometric Mean Fluorescence) | |||
|
| |||
| CCR2 Levels on Classical Monocytes | 157 [139, 188] | 197 [152, 230] | 0.096 |
| CCR2 Levels on Intermediate Monocytes | 46 [38, 68] | 48 [21, 82] | 0.970 |
| CCR2 Levels on Non-Classical Monocytes | 30 [9, 41] | 27 [15, 39] | 0.791 |
| CCR5 Levels on Classical Monocytes | 796 [627, 1093] | 1032 [902, 1406] | 0.204 |
| CCR5 Levels on Intermediate Monocytes | 781 [451, 1220] | 1148 [801, 1580] | 0.206 |
| CCR5 Levels on Non-Classical Monocytes | 296 [216, 345] | 367 [293, 441] | 0.233 |
| CCR2 Levels on CD4+ T Cells | 11.9 [9.3, 15.2] | 14.9 [13.4, 15.9] | 0.007 |
| CCR2 Levels on CD8+ T Cells | ND | ND | ND |
| CCR5 Levels on CD4+ T Cells | 30.9 [8.0, 50.9] | 67.25 [38.8, 91.4] | 0.002 |
| CCR5 Levels on CD8+ T Cells | 209 [106, 290] | 712 [453, 816] | <0.001 |
ND = Not detected by flow cytometry method
Figure 1. Neuropsychological testing.
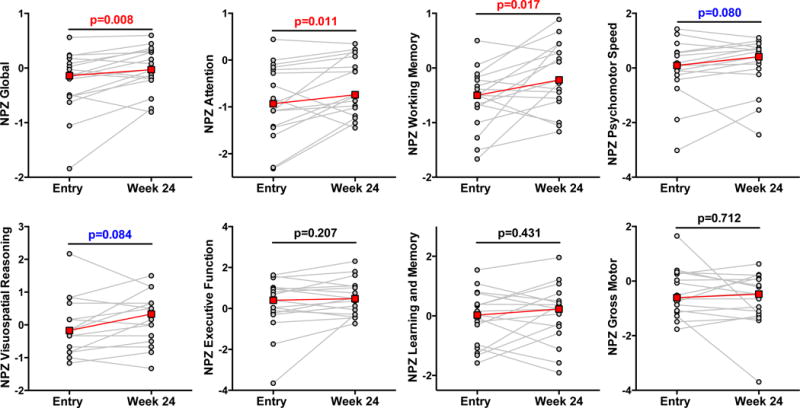
Global NPZ and subdomain NPZs of attention; working memory; psychomotor speed; visuospatial reasoning; executive function; learning and memory and gross motor were measured at entry and after 24 weeks of cenicriviroc.
In the attention domain, trends towards improvements in performance were observed on the CalCap Choice test (median increase=0.57 [−0.45, 1.18], p=0.071) and Digit Span Total (median increase=0.33 [0, 0.66], p=0.094; Supplemental Table 1). Within the working memory domain, the greatest change was evident on the Letter Number Sequencing test (median increase=0.33 [0, 1.00]; p = 0.030), with a less robust effect seen on Digit Span (median increase=0.33 [0, 1.33]; p = 0.065)) and no significant change on CVLT-II trial B were noted (Supplemental Table 1). Comparisons of change in performance relative to the SEM of each neuropsychological measure revealed that initiation of CVC was associated with improvements in performance that exceeded the SEM on the Letter Number Sequencing test.40
Changes in Monocyte/Macrophage Activation
After 24 weeks of CVC, significant declines in plasma sCD163, sCD14, and neopterin were observed (Table 3). The trajectories of individual and overall trends are shown in Figure 2.
Figure 2. Plasma soluble biomarkers.
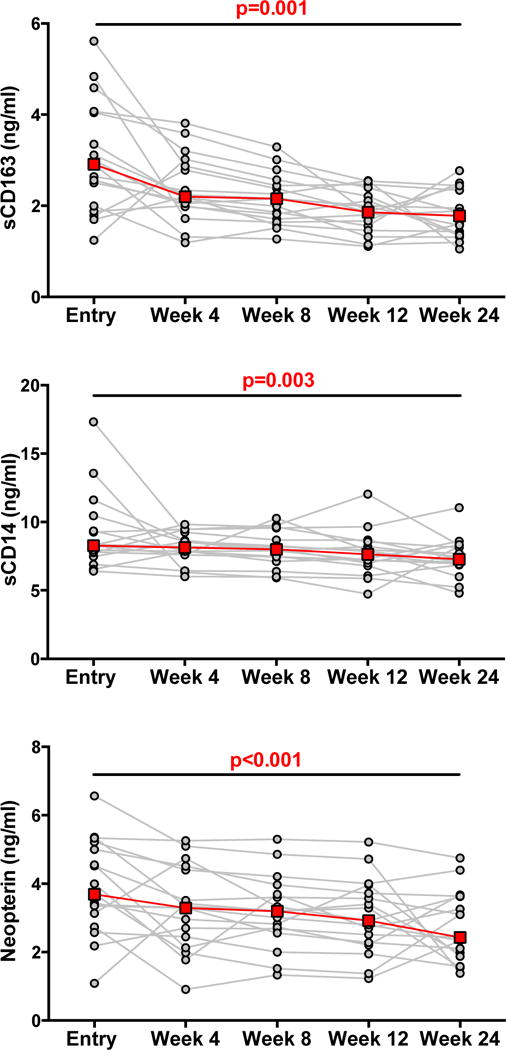
Plasma sCD163, sCD14 and neopterin were measured at entry and after 4; 8; 12 and 24 weeks of cenicriviroc.
Changes in Leukocyte Counts
After 24 weeks, significant declines in total monocyte and classical monocyte counts along with significant increases in CD4+ T cell and CD8+ T cell counts were observed (Table 3). No significant changes were noted with CD4+/CD8+ ratios or the intermediate and non-classical monocyte subset counts (Table 3).
Changes in CCR2 and CCR5 Expression on Monocyte and T Cell Populations
Monocytes are composed of three distinct phenotypic subsets based on CD14 and CD16 expression into classical, intermediate and non-classical monocytes.41 Functionally these are defined by having scavenging/phagocytic, inflammatory and patrolling properties, respectively.42,43 After 24 weeks, we observed a trend towards increased CCR2 expression on classical monocytes (Table 3). No significant changes were observed in CCR2 expression on intermediate and non-classical monocytes or in CCR5 expression on any of the monocyte subsets (Table 3). A significant increase in CCR2 levels on CD4+ T cells and significant increases in CCR5 expression on CD4+ and CD8+ T cells were noted (Table 3).
Correlations at Entry Between Leukocyte Measurements, Soluble Markers of Monocyte/Macrophage Activation and Neuropsychological Testing
At entry, higher CCR2 levels on non-classical monocytes correlated with better performance on tests of attention (rho=0.637; p=0.026). Higher CCR5 expression on classical monocytes correlated with greater classical monocyte counts (rho=0.587; p=0.045). Additionally, sCD14 positively correlated with non-classical monocyte counts (rho=0.755; p=0.005). Trends noted at entry included a positive correlation between CCR5 levels on non-classical monocytes and non-classical monocyte counts (rho=0.559; p=0.059) and negative correlations between CCR5 on CD4+ T cells and visuospatial performance (rho= −0.574; p=0.065), and between sCD14 and psychomotor speed (rho= −0.458; p=0.064). No correlations were noted between sCD163 and neopterin, and monocyte counts, CKR expression or performances on neuropsychological measures.
DISCUSSION
Our study demonstrated improved neuropsychological testing performance and reduced monocyte activation following 24 weeks of CVC in 17 virally suppressed HIV-infected individuals on stable ART. These data potentially link changes in monocyte/macrophage activation induced by CVC to improved cognitive performance in HIV-infected participants on virally suppressive ART.
Although the effects of CVC on cognitive performance were relatively subtle, the improvements approximated 0.5 SD, which is commonly referenced as a clinically meaningful degree of change.44 Working memory, one of the subdomains which improved with CVC, is a specific component of executive function that is sensitive to HIV.45 The working memory cognitive domain encompasses short-term storage and manipulation of a limited amount of information in real time46,47 and is essential for effective implementation of daily activities such as driving, problem solving, and complex decision-making.48
As a single-arm study design, the potential influence of practice effects on the cognitive outcomes merits consideration. Practice effects are common and are typically pronounced between the first and second exposures.49 The cohort recruited in the present study had undergone cognitive testing through prior longitudinal studies and therefore the impact of practice from baseline to 24 weeks in the present study is less clear. The magnitude of change in the working memory domain, particularly on the Letter Number Sequencing test, exceeded the SEM, suggesting that the magnitude of change in performance observed in the present study is unlikely to be due to practice effects.49 However, larger studies with a demographically matched control group are needed to address the important issue of practice effects more completely.
Potential therapeutic interventions for HIV-associated cognitive difficulties are limited. Our study suggests that modulation of monocyte/macrophage activation should be considered as a potential therapeutic intervention option to improve cognitive performance. Both sCD163 and sCD14, which are shed after monocyte/macrophage activation50–52, have been previously shown to be biomarkers of cognitive performance in HIV. In ART-treated individuals, plasma sCD163 levels are elevated among individuals with more severe cognitive deficits.14 Plasma sCD14 levels have also been shown to be higher in HIV-infected individuals with worse performance in attention and learning.53 Similarly, in the Women’s Interagency HIV Study (WIHS), higher plasma sCD163 levels associated with worse global cognitive performance and lower scores on tests of verbal learning, verbal memory, executive function, psychomotor speed.15 Higher sCD14 levels were associated with worse verbal learning, verbal memory, executive function, and psychomotor speed.15 Neopterin, which is produced by monocytes after stimulation with pro-inflammatory cytokines such as interferon-γ (IFN-γ)54, remains elevated in treated HIV.55–58 Although we did not observe significant correlations between sCD163, sCD14 or neopterin with cognition at baseline, the concomitant decrease in soluble markers of monocyte/macrophage activation with improved cognitive performance is suggestive of a direct link. Further studies are needed to explore the causal pathways that cannot be established in this preliminary study.
Decreases in monocyte counts in the periphery may be a result of diminished rates of egress of classical monocytes out of the bone marrow, as murine studies have demonstrated that CCR2 is required for monocyte trafficking out of the bone marrow into the circulation.42,59 Increases in CKRs observed in our study are in concert with a double-blind, placebo controlled randomized trial of MVC where CCR5+ CD4+ and CD8+ T cell frequencies were significantly increased in the MVC group compared to placebo.60 Although chemokine receptor levels on the monocyte subsets from the periphery were not significantly altered by CVC, we did note a limited number of correlations between CKR expression and cognitive performances, suggesting modulation of chemokine receptors have beneficial effects. In fact, murine models have shown that decreased function of CCR5 lead to enhanced hippocampal-dependent learning and memory, while neuronal CCR5 overexpression caused memory deficits.61 Moreover, treatment of mice with HIV peptide decreases long-term potentiation deficits that can be prevented by CCR5 knockout or knockdown.61
Four out of the 17 participants had worse global cognition after 24 weeks of CVC. There were no evident factors that contributed to the decline in cognitive performance in 3 out of the 4 participants. One participant tested positive for methamphetamines, marijuana and amphetamines at week 24 but not at entry, which could have affected cognitive performance at the follow-up visit. Removal of this case did not affect the pattern of results. When comparing the participants who exhibited worse cognition after 24 weeks of CVC to the remainder of the sample revealed no significant differences in clinical or laboratory parameters, including monocyte activation, leukocyte counts, age, or years infected (data not shown).
This study was planned as a small exploratory study. The conclusions of this study are limited by the small sample size of only 17 evaluable participants. In addition, the design was that of a single arm study without a placebo control arm which limits our ability to conclusively define a causal link between CVC and changes in cognition and monocyte/macrophage immune activation. Finally it should be noted that participants enrolled in the present study were chronically-infected with a long history of ART and we cannot make any conclusions on the potential effect of CVC on individuals who are ART-naïve, or were treated early or in acute HIV infection. It is possible that CVC therapy may not have as great a response in early HIV when monocyte/macrophage inflammation is likely less than in those with delayed therapy, but it is equally possible that early intervention with CVC soon after diagnosis in conjunction with potent ART may prevent or diminish the occurrence of even mild forms of cognitive impairment.
The results of this small single-arm study are however intriguing. Given the lack of pharmacological interventions to improve cognition in HIV-infected individuals, further study of CVC in a randomized controlled study with a placebo arm and a longer follow-up period would be important to both confirm our findings and also to determine the magnitude and relevance of outcomes to patient care. Additional points of interest include characterizing monocyte/macrophages from tissues. The observed increases in CD4+ counts may indicate a restoration of the immune system and further study of the effect of CVC on T cells should be pursued. Lastly, the unexpected increase in CD8+ counts also merits further investigation.
Supplementary Material
Supplemental Figure 1: Representative gating strategy for monocytes and T cells using flow cytometry. To identify monocytes and lymphocytes from the peripheral blood mononuclear cell population, doublet and dead cells were first excluded. Lymphocytes, positive for CD3, were subset into CD4+ and CD8+ T cells. Monocytes, positive for CD11b and HLA-DR, and negative for natural killer and B cell markers (CD7, CD19 or CD20), were subset by CD14 and CD16 expression: Classical monocytes (CD14++CD16−), intermediate monocytes (CD14++CD16+), non-classical monocytes (CD14+CD16+). CCR2 and CCR5 expression were assessed on the CD4+ and CD8+ T cells, and monocyte subsets.
Acknowledgments
We thank the Hawaii Center for AIDS (HICFA) study participants and the HICFA clinical team.
Sources of funding: This work was funded by the National Institute on Minority Health and Health Disparities of the National Institutes of Health (NIH) under award number U54MD007584 (CMS) and the National Institute of General Medical Sciences of the NIH under award number 4U54GM104944-04 (MLD). CVC was supplied by Tobira Therapeutics (now Allergan).
Footnotes
Part of this work was presented at Conference on Retroviruses and Opportunistic Infections (CROI), February 13 to February 16, 2017, in Seattle, Washington, Abstract #381.
Conflicts of interest
The authors have no conflicts to declare.
References
- 1.Tozzi V, Balestra P, Salvatori MF, et al. Changes in cognition during antiretroviral therapy: comparison of 2 different ranking systems to measure antiretroviral drug efficacy on HIV-associated neurocognitive disorders. J Acquir Immune Defic Syndr. 2009;52(1):56–63. doi: 10.1097/qai.0b013e3181af83d6. [DOI] [PubMed] [Google Scholar]
- 2.Heaton RK, Franklin DR, Ellis RJ, et al. HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. J Neurovirol. 2011;17(1):3–16. doi: 10.1007/s13365-010-0006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heaton RK, Marcotte TD, Mindt MR, et al. The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychol Soc. 2004;10(3):317–331. doi: 10.1017/S1355617704102130. [DOI] [PubMed] [Google Scholar]
- 4.Ellis RJ, Deutsch R, Heaton RK, et al. Neurocognitive impairment is an independent risk factor for death in HIV infection. San Diego HIV Neurobehavioral Research Center Group. Archives of neurology. 1997;54(4):416–424. doi: 10.1001/archneur.1997.00550160054016. [DOI] [PubMed] [Google Scholar]
- 5.Ickovics JR, Hamburger ME, Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. Jama. 2001;285(11):1466–1474. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]
- 6.Shapshak P, Kangueane P, Fujimura RK, et al. Editorial neuroAIDS review. Aids. 2011;25(2):123–141. doi: 10.1097/QAD.0b013e328340fd42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kusao I, Shiramizu B, Liang CY, et al. Cognitive performance related to HIV-1-infected monocytes. J Neuropsychiatry Clin Neurosci. 2012;24(1):71–80. doi: 10.1176/appi.neuropsych.11050109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonzalez-Scarano F, Martin-Garcia J. The neuropathogenesis of AIDS. Nat Rev Immunol. 2005;5(1):69–81. doi: 10.1038/nri1527. [DOI] [PubMed] [Google Scholar]
- 9.Sevigny JJ, Albert SM, McDermott MP, et al. Evaluation of HIV RNA and markers of immune activation as predictors of HIV-associated dementia. Neurology. 2004;63(11):2084–2090. doi: 10.1212/01.wnl.0000145763.68284.15. [DOI] [PubMed] [Google Scholar]
- 10.Cassol E, Misra V, Morgello S, Gabuzda D. Applications and limitations of inflammatory biomarkers for studies on neurocognitive impairment in HIV infection. J Neuroimmune Pharmacol. 2013;8(5):1087–1097. doi: 10.1007/s11481-013-9512-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thames AD, Briones MS, Magpantay LI, et al. The role of chemokine C-C motif ligand 2 genotype and cerebrospinal fluid chemokine C-C motif ligand 2 in neurocognition among HIV-infected patients. AIDS. 2015;29(12):1483–1491. doi: 10.1097/QAD.0000000000000706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gisslen M, Price RW, Andreasson U, et al. Plasma Concentration of the Neurofilament Light Protein (NFL) is a Biomarker of CNS Injury in HIV Infection: A Cross-Sectional Study. EBioMedicine. 2016;3:135–140. doi: 10.1016/j.ebiom.2015.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gannon P, Khan MZ, Kolson DL. Current understanding of HIV-associated neurocognitive disorders pathogenesis. Curr Opin Neurol. 2011;24(3):275–283. doi: 10.1097/WCO.0b013e32834695fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burdo TH, Weiffenbach A, Woods SP, Letendre S, Ellis RJ, Williams KC. Elevated sCD163 in plasma but not cerebrospinal fluid is a marker of neurocognitive impairment in HIV infection. AIDS. 2013;27(9):1387–1395. doi: 10.1097/QAD.0b013e32836010bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Imp BM, Rubin LH, Tien PC, et al. Monocyte Activation Is Associated With Worse Cognitive Performance in HIV-Infected Women With Virologic Suppression. J Infect Dis. 2017;215(1):114–121. doi: 10.1093/infdis/jiw506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agsalda-Garcia MA, Sithinamsuwan P, Valcour VG, et al. Brief Report: CD14+ Enriched Peripheral Cells Secrete Cytokines Unique to HIV-Associated Neurocognitive Disorders. J Acquir Immune Defic Syndr. 2017;74(4):454–458. doi: 10.1097/QAI.0000000000001259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ndhlovu LC, Umaki T, Chew GM, et al. Treatment intensification with maraviroc (CCR5 antagonist) leads to declines in CD16-expressing monocytes in cART-suppressed chronic HIV-infected subjects and is associated with improvements in neurocognitive test performance: implications for HIV-associated neurocognitive disease (HAND) J Neurovirol. 2014 doi: 10.1007/s13365-014-0279-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gates TM, Cysique LA, Siefried KJ, Chaganti J, Moffat KJ, Brew BJ. Maraviroc-intensified combined antiretroviral therapy improves cognition in virally suppressed HIV-associated neurocognitive disorder. AIDS. 2016;30(4):591–600. doi: 10.1097/QAD.0000000000000951. [DOI] [PubMed] [Google Scholar]
- 19.Gutierrez C, Diaz L, Vallejo A, et al. Intensification of antiretroviral therapy with a CCR5 antagonist in patients with chronic HIV-1 infection: effect on T cells latently infected. PLoS One. 2011;6(12):e27864. doi: 10.1371/journal.pone.0027864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ndhlovu LC, D’Antoni ML, Ananworanich J, et al. Loss of CCR2 expressing non-classical monocytes are associated with cognitive impairment in antiretroviral therapy-naive HIV-infected Thais. J Neuroimmunol. 2015;288:25–33. doi: 10.1016/j.jneuroim.2015.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eugenin EA, Osiecki K, Lopez L, Goldstein H, Calderon TM, Berman JW. CCL2/monocyte chemoattractant protein-1 mediates enhanced transmigration of human immunodeficiency virus (HIV)-infected leukocytes across the blood-brain barrier: a potential mechanism of HIV-CNS invasion and NeuroAIDS. J Neurosci. 2006;26(4):1098–1106. doi: 10.1523/JNEUROSCI.3863-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams DW, Calderon TM, Lopez L, et al. Mechanisms of HIV entry into the CNS: increased sensitivity of HIV infected CD14+CD16+ monocytes to CCL2 and key roles of CCR2, JAM-A, and ALCAM in diapedesis. PLoS One. 2013;8(7):e69270. doi: 10.1371/journal.pone.0069270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Williams DW, Veenstra M, Gaskill PJ, Morgello S, Calderon TM, Berman JW. Monocytes mediate HIV neuropathogenesis: mechanisms that contribute to HIV associated neurocognitive disorders. Curr HIV Res. 2014;12(2):85–96. doi: 10.2174/1570162x12666140526114526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weiss JM, Nath A, Major EO, Berman JW. HIV-1 Tat induces monocyte chemoattractant protein-1-mediated monocyte transmigration across a model of the human blood-brain barrier and up-regulates CCR5 expression on human monocytes. J Immunol. 1999;163(5):2953–2959. [PubMed] [Google Scholar]
- 25.Lalezari J, Gathe J, Brinson C, et al. Safety, efficacy, and pharmacokinetics of TBR-652, a CCR5/CCR2 antagonist, in HIV-1-infected, treatment-experienced, CCR5 antagonist-naive subjects. J Acquir Immune Defic Syndr. 2011;57(2):118–125. doi: 10.1097/QAI.0b013e318213c2c0. [DOI] [PubMed] [Google Scholar]
- 26.Marier JF, Trinh M, Pheng LH, Palleja SM, Martin DE. Pharmacokinetics and pharmacodynamics of TBR-652, a novel CCR5 antagonist, in HIV-1-infected, antiretroviral treatment-experienced, CCR5 antagonist-naive patients. Antimicrob Agents Chemother. 2011;55(6):2768–2774. doi: 10.1128/AAC.00713-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baba M, Takashima K, Miyake H, et al. TAK-652 inhibits CCR5-mediated human immunodeficiency virus type 1 infection in vitro and has favorable pharmacokinetics in humans. Antimicrob Agents Chemother. 2005;49(11):4584–4591. doi: 10.1128/AAC.49.11.4584-4591.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Friedman S, Sanyal A, Goodman Z, et al. Efficacy and safety study of cenicriviroc for the treatment of non-alcoholic steatohepatitis in adult subjects with liver fibrosis: CENTAUR Phase 2b study design. Contemp Clin Trials. 2016;47:356–365. doi: 10.1016/j.cct.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 29.Friedman SL, Ratziu V, Harrison SA, et al. A Randomized, Placebo-Controlled Trial of Cenicriviroc for Treatment of Nonalcoholic Steatohepatitis with Fibrosis. Hepatology. 2017 doi: 10.1002/hep.29477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lefebvre E, Moyle G, Reshef R, et al. Antifibrotic Effects of the Dual CCR2/CCR5 Antagonist Cenicriviroc in Animal Models of Liver and Kidney Fibrosis. PLoS One. 2016;11(6):e0158156. doi: 10.1371/journal.pone.0158156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mossanen JC, Krenkel O, Ergen C, et al. Chemokine (C-C motif) receptor 2-positive monocytes aggravate the early phase of acetaminophen-induced acute liver injury. Hepatology. 2016;64(5):1667–1682. doi: 10.1002/hep.28682. [DOI] [PubMed] [Google Scholar]
- 32.Puengel T, Krenkel O, Kohlhepp M, et al. Differential impact of the dual CCR2/CCR5 inhibitor cenicriviroc on migration of monocyte and lymphocyte subsets in acute liver injury. PLoS One. 2017;12(9):e0184694. doi: 10.1371/journal.pone.0184694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thompson M, Saag M, DeJesus E, et al. A 48-week randomized phase 2b study evaluating cenicriviroc versus efavirenz in treatment-naive HIV-infected adults with C-C chemokine receptor type 5-tropic virus. AIDS. 2016;30(6):869–878. doi: 10.1097/QAD.0000000000000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kramer V, Hassounah S, Colby-Germinario S, Mesplede T, Lefebvre E, Wainberg M. Cenicriviroc blocks HIV entry but does not lead to redistribution of HIV into extracellular space like maraviroc. J Int AIDS Soc. 2014;17(4 Suppl 3):19531. doi: 10.7448/IAS.17.4.19531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Antinori A, Arendt G, Becker JT, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69(18):1789–1799. doi: 10.1212/01.WNL.0000287431.88658.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wechsler D. Wechsler adult intelligence scale. Fourth. Vol. 22. San Antonio, TX: NCS Pearson; 2008. [Google Scholar]
- 37.Fastenau PS, Denburg NL, Hufford BJ. Adult norms for the Rey-Osterrieth Complex Figure Test and for supplemental recognition and matching trials from the Extended Complex Figure Test. Clin Neuropsychol. 1999;13(1):30–47. doi: 10.1076/clin.13.1.30.1976. [DOI] [PubMed] [Google Scholar]
- 38.Robert K, Heaton IG, Matthews Charles G. Comprehensive norms for an expanded Halstead-Reitan battery : demographic corrections, research findings, and clinical applications. Psychological Assessment Resources. 1991 [Google Scholar]
- 39.Jalbert E, Shikuma CM, Ndhlovu LC, Barbour JD. Sequential staining improves detection of CCR2 and CX3CR1 on monocytes when simultaneously evaluating CCR5 by multicolor flow cytometry. Cytometry A. 2013;83(3):280–286. doi: 10.1002/cyto.a.22257. [DOI] [PubMed] [Google Scholar]
- 40.Brouillette MJ, Yuen T, Fellows LK, Cysique LA, Heaton RK, Mayo NE. Identifying Neurocognitive Decline at 36 Months among HIV-Positive Participants in the CHARTER Cohort Using Group-Based Trajectory Analysis. PLoS One. 2016;11(5):e0155766. doi: 10.1371/journal.pone.0155766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ziegler-Heitbrock L, Ancuta P, Crowe S, et al. Nomenclature of monocytes and dendritic cells in blood. Blood. 2010;116(16):e74–80. doi: 10.1182/blood-2010-02-258558. [DOI] [PubMed] [Google Scholar]
- 42.Shi C, Pamer EG. Monocyte recruitment during infection and inflammation. Nat Rev Immunol. 2011;11(11):762–774. doi: 10.1038/nri3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang J, Zhang L, Yu C, Yang XF, Wang H. Monocyte and macrophage differentiation: circulation inflammatory monocyte as biomarker for inflammatory diseases. Biomark Res. 2014;2(1):1. doi: 10.1186/2050-7771-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Howard R, Phillips P, Johnson T, et al. Determining the minimum clinically important differences for outcomes in the DOMINO trial. Int J Geriatr Psychiatry. 2011;26(8):812–817. doi: 10.1002/gps.2607. [DOI] [PubMed] [Google Scholar]
- 45.Walker KA, Brown GG. HIV-associated executive dysfunction in the era of modern antiretroviral therapy: A systematic review and meta-analysis. J Clin Exp Neuropsychol. 2017:1–20. doi: 10.1080/13803395.2017.1349879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ericsson KA, Kintsch W. Long-term working memory. Psychol Rev. 1995;102(2):211–245. doi: 10.1037/0033-295x.102.2.211. [DOI] [PubMed] [Google Scholar]
- 47.Hitch ADBG. Working Memory. Psychology of Learning and Motivation. 1974;8:47–89. [Google Scholar]
- 48.Hinson JM, Jameson TL, Whitney P. Impulsive decision making and working memory. J Exp Psychol Learn Mem Cogn. 2003;29(2):298–306. doi: 10.1037/0278-7393.29.2.298. [DOI] [PubMed] [Google Scholar]
- 49.Beglinger LJ, Gaydos B, Tangphao-Daniels O, et al. Practice effects and the use of alternate forms in serial neuropsychological testing. Arch Clin Neuropsychol. 2005;20(4):517–529. doi: 10.1016/j.acn.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 50.Weaver LK, Hintz-Goldstein KA, Pioli PA, et al. Pivotal advance: activation of cell surface Toll-like receptors causes shedding of the hemoglobin scavenger receptor CD163. J Leukoc Biol. 2006;80(1):26–35. doi: 10.1189/jlb.1205756. [DOI] [PubMed] [Google Scholar]
- 51.Etzerodt A, Maniecki MB, Moller K, Moller HJ, Moestrup SK. Tumor necrosis factor alpha-converting enzyme (TACE/ADAM17) mediates ectodomain shedding of the scavenger receptor CD163. J Leukoc Biol. 2010;88(6):1201–1205. doi: 10.1189/jlb.0410235. [DOI] [PubMed] [Google Scholar]
- 52.Triantafilou M, Triantafilou K. Lipopolysaccharide recognition: CD14, TLRs and the LPS-activation cluster. Trends Immunol. 2002;23(6):301–304. doi: 10.1016/s1471-4906(02)02233-0. [DOI] [PubMed] [Google Scholar]
- 53.Lyons JL, Uno H, Ancuta P, et al. Plasma sCD14 is a biomarker associated with impaired neurocognitive test performance in attention and learning domains in HIV infection. J Acquir Immune Defic Syndr. 2011;57(5):371–379. doi: 10.1097/QAI.0b013e3182237e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Werner-Felmayer G, Werner ER, Fuchs D, Hausen A, Reibnegger G, Wachter H. Tumour necrosis factor-alpha and lipopolysaccharide enhance interferon-induced tryptophan degradation and pteridine synthesis in human cells. Biol Chem Hoppe Seyler. 1989;370(9):1063–1069. doi: 10.1515/bchm3.1989.370.2.1063. [DOI] [PubMed] [Google Scholar]
- 55.Abdulle S, Hagberg L, Svennerholm B, Fuchs D, Gisslen M. Continuing intrathecal immunoactivation despite two years of effective antiretroviral therapy against HIV-1 infection. AIDS. 2002;16(16):2145–2149. doi: 10.1097/00002030-200211080-00006. [DOI] [PubMed] [Google Scholar]
- 56.Eden A, Price RW, Spudich S, Fuchs D, Hagberg L, Gisslen M. Immune activation of the central nervous system is still present after >4 years of effective highly active antiretroviral therapy. J Infect Dis. 2007;196(12):1779–1783. doi: 10.1086/523648. [DOI] [PubMed] [Google Scholar]
- 57.Valcour VG, Ananworanich J, Agsalda M, et al. HIV DNA reservoir increases risk for cognitive disorders in cART-naive patients. PLoS One. 2013;8(7):e70164. doi: 10.1371/journal.pone.0070164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hagberg L, Cinque P, Gisslen M, et al. Cerebrospinal fluid neopterin: an informative biomarker of central nervous system immune activation in HIV-1 infection. AIDS Res Ther. 2010;7:15. doi: 10.1186/1742-6405-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Serbina NV, Pamer EG. Monocyte emigration from bone marrow during bacterial infection requires signals mediated by chemokine receptor CCR2. Nat Immunol. 2006;7(3):311–317. doi: 10.1038/ni1309. [DOI] [PubMed] [Google Scholar]
- 60.van Lelyveld SF, Drylewicz J, Krikke M, et al. Maraviroc Intensification of cART in Patients with Suboptimal Immunological Recovery: A 48-Week, Placebo-Controlled Randomized Trial. PLoS One. 2015;10(7):e0132430. doi: 10.1371/journal.pone.0132430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhou M, Greenhill S, Huang S, et al. CCR5 is a suppressor for cortical plasticity and hippocampal learning and memory. Elife. 2016;5 doi: 10.7554/eLife.20985. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Representative gating strategy for monocytes and T cells using flow cytometry. To identify monocytes and lymphocytes from the peripheral blood mononuclear cell population, doublet and dead cells were first excluded. Lymphocytes, positive for CD3, were subset into CD4+ and CD8+ T cells. Monocytes, positive for CD11b and HLA-DR, and negative for natural killer and B cell markers (CD7, CD19 or CD20), were subset by CD14 and CD16 expression: Classical monocytes (CD14++CD16−), intermediate monocytes (CD14++CD16+), non-classical monocytes (CD14+CD16+). CCR2 and CCR5 expression were assessed on the CD4+ and CD8+ T cells, and monocyte subsets.


