Highlights
-
•
This was the first study to use PEEK scapula material prepared by 3D printing technology.
-
•
The 3D-printed PEEK scapula prosthesis offers precise reconstruction.
-
•
The 3D-printed PEEK scapula prosthesis is beneficial for early functional recovery.
Keywords: Polyetheretherketone, Implant, Benign fibrous histiocytoma
Abbreviations: bfh, benign fibrous histiocytoma; 3d, 3-dimensional; Peek, polyetheretherketone; Ct, computed tomography; WHO, World Health Organization; MRI, magnetic resonance imaging; CAD, computer aided design
Abstract
Background
Bone benign fibrous histiocytoma (BFH) is an invasive primary bone tumor. When the local excision is not complete, the risk of recurrence is high, and hence, one-piece resection is necessary. The major challenge for clinicians is to reconstruct the bone after resection of the tumor. The present study investigated the efficacy of 3-dimensional (3D) printing technique in the treatment of benign fibrous histiocytoma of the scapula.
Methods
The patient with benign fibrous histiocytoma of scapular bone was treated with PEEK (polyetheretherketone) prosthesis replacement using the 3D printing technique. X-ray and computed tomography (CT) scans evaluated the relationship between the position of the prosthesis and that of the shoulder joint. Also, the constant score of the shoulder joint was calculated.
Results
The anteroposterior radiograph showed that the position of the left scapula prosthesis is satisfactory and that of the shoulder joint is normal. Three months after the operation, the X-ray examination indicated the lack of flexibility and shift, as well as, dislocation and disjunction of PEEK prosthesis. The constant score of the left shoulder function was 68 points. Active shoulder joint activity: 120° on the lift, 90° on abduction, 50° on the external rotation, and 70° on internal rotation.
Conclusions
The application of 3D-printed PEEK scapula prosthesis with total shoulder replacement offers the possibility of accurate reconstruction, improves the operability of surgery, shortens the operation time, and allows early functional recovery of the patients.
1. Introduction
BFH is a rare primary bone tumor that belongs to the category of fibrous histiocytoma in the World Health Organization (WHO) tumor classification [1]. The BFH commonly occurs in soft tissues and is rare in primary bone. It mainly affects 6–66-year-old patients. Previous studies reported that a large number of incidences occurred in 30-year age groups [2]. The backbone and distal metaphyseal of the femur, tibia, and sacrum, as well as that in the pelvis, clavicle, ribs, and phalanges, are common [3]. According to the Enneking surgical stage, the BFH of bone should be classified as S2. It exhibits invasiveness and active biological behavior. The postoperative local tumor recurrence is plausible. Only a few atypical cases may have lung metastasis [4]. The main treatments include extensive local resection or marginal resection and bone grafting.
2. Materials and methods
2.1. History
A 16-year-old male was admitted to the hospital and required surgical treatment. Nine months after the left scapula BFH resection surgery, the pain occured in surgery area and lasted 3 months. The patient was treated with scraping and bone grafting of the left scapula in another hospital 1 year ago. The postoperative pathology showed benign fibrous histiocytoma without the history of trauma.
2.2. Examination
The patient had a clear mind and good physical development. A 6-cm-long surgical scar was visible above the left scapular sac. Any palpable mass was not detected in the original surgical area. The left shoulder joint was limited in external rotation, while the internal rotation was normal. The bilateral biceps tendon reflex was normal.
2.3. Imaging
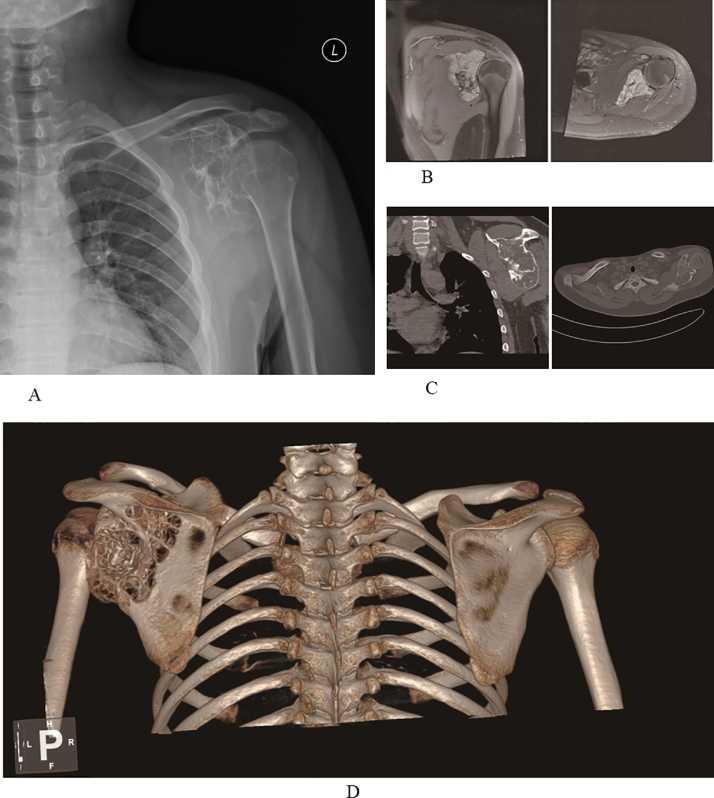
Multi-atrial osteolytic bone destruction was observed in X-ray scan (Fig. 1A). The CT image of the shoulder joint (Fig. 1C, D) displayed that the left shoulder-sacrum lesion was consistent with the recurrence of the tumor. The magnetic resonance imaging (MRI) examination of the shoulder joint (Fig. 1B) showed an abnormal signal in the left shoulder blade. The size of the tumor was approximately 7.9 × 5.7 cm; however, the surrounding soft tissues were not affected.
Fig. 1.
The preoperative imaging examination of the patient. (A) Anteroposterior view of the left shoulder joint in the X-ray film. Multi-atrial osteolytic bone destruction of the left scapula is shown as expansive growth. The boundary of the scapular lesion is clear, and no pathological fracture is detected. (B) Inhomogeneous high signal in MRI T2 phase of the left shoulder joint. MRI results suggest that the original tumor relapses after surgery. (C) CT of the left shoulder. Calcification in the lesion is observed, while osteophyte and separation are formed. The size of the lesion is approximately 8 cm × 5.5 cm. The left axillary lymph nodes are swollen and enlarged. The soft tissue around the scapula is undamaged. (D) 3D CT reconstruction of bilateral shoulder joints. Osteolytic destruction on the left scapula is observed.
2.4. Laboratory examination
The abnormal results for the evaluation of the biochemical parameters were as follows: aspartate aminotransferase 148 IU/L, total protein 56.8 g/L, indirect bilirubin 3.7 μmol/L, and alkaline phosphatase 190 IU/L. The results of blood routine, blood clotting, liver and kidney function, and serum ion did not show any obvious abnormalities after tests.
2.5. Diagnosis
Recurrence of benign fibrous histiocytoma of the left scapula.
2.6. Treatment plan
Since the tumor is highly invasive, it putatively occurs locally after partial resection. If total scapula resection is performed, postoperative function would be poor and exact reconstruction difficult. Thus, the 3D printing technology was used to perform total scapular prosthetic shoulder replacement.
2.7. Preoperative preparation
Scapular X-ray film (Fig. 1A) and thin-slice spiral CT (0.625 mm layer thickness, resolution 512 × 512) were used to obtain the CT scan of the contralateral scapula and 3D reconstruction images (Fig. 1C and D). A computer image processing system was used to construct a 3D computer aided design (CAD) model, and the porous structure designed. 3D printing technology was performed to generate a 1:1 PEEK prosthesis (Fig. 2A).
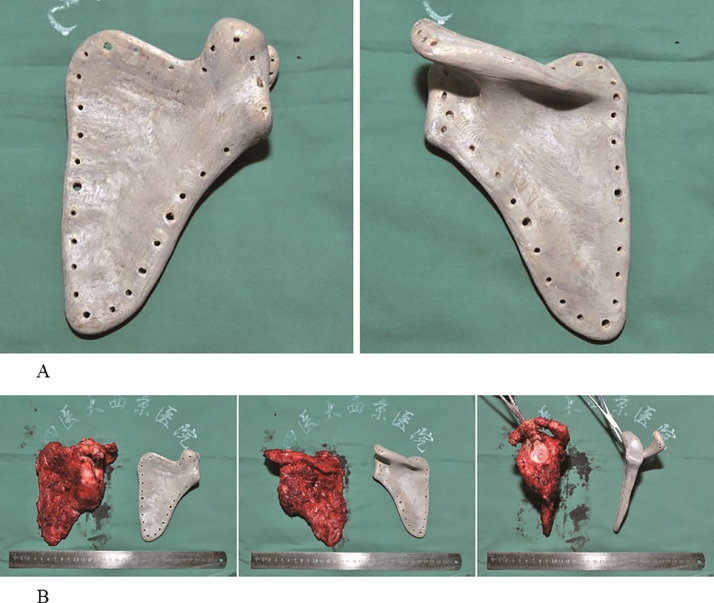
Fig. 2.
Comparison of scapular tumor and prosthesis. (A) The 3D-printed PEEK prosthesis of shoulder scapular. The front and back views of the prosthesis are shown, and the void structure of the scapula is regular and obvious. (B) The tumor is completely removed.
2.8. Operative intervention
The surgery was performed in strict accordance with preoperative planning. The skin incision began at the shoulder peak, inward along the scapular ganglion to the scapular spine margin, and then, towards the inferior corner of the scapula. After full exposure, the left scapula was removed together with a layer of muscle cuff. The proximal humerus was cut according to the preoperative osteotomy plane. After the medullary cavity of the humerus was processed, the cemented prosthesis was implanted. The major muscle ligaments of the shoulder joint were sutured to the pre-drilled sieve holes on the scapular prosthesis. After the implant was satisfactorily fixed, the acromioclavicular ligament and the shoulder joint capsule were reconstructed. The short muscle head and small pectoralis muscles were sewn to the condyle in situ, and the severed coracoclavicular ligament was repaired. Consequently, a satisfactory joint motion was observed, and dislocation did not occur while moving the shoulder joint. Intraoperative X-ray examination results established a satisfactory correlation between the artificial scapula and shoulder joints. The bleeding ceased, the surgical field was rinsed one time and negative pressure drainage placed. Finally, the surgical incisions were sutured layer-by-layer. The duration of the operation was 215 min, and the intraoperative blood loss was 1000 mL.
2.9. Postoperative course
Pre-braking, infection prevention, swelling reduction, and other routine treatments were performed. The patient was required to wear the shoulder adduction brace for 8 weeks, following which, he removed the brace, and the joint activities strengthened gradually.
2.10. Main observations
X-ray of the patient's left shoulder, CT scan of the left scapular prosthesis, and a constant score of the shoulder were observed.
3. Results
3.1. X-ray of the left shoulder joint
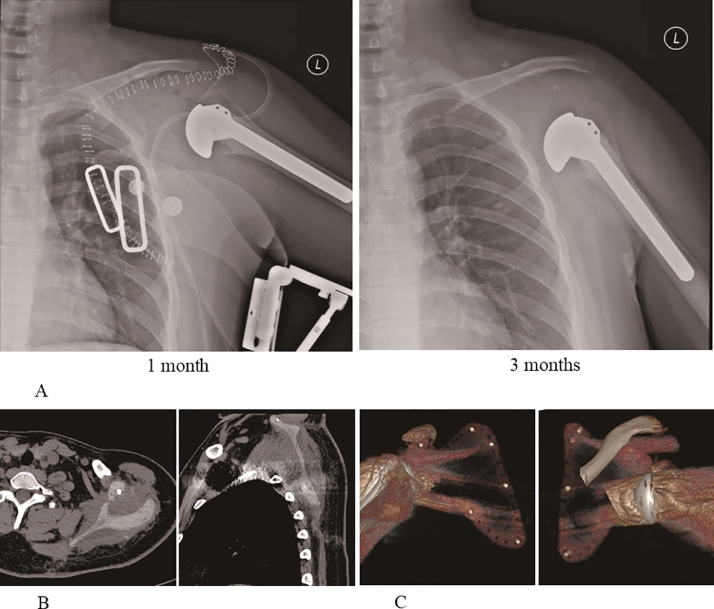
The X-ray of the left shoulder a satisfactory position of the left scapula prosthesis and normal position of the shoulder joint (Fig. 3A).
Fig. 3.
The imaging examination after surgery. (A) X-ray of the left shoulder after surgery. Shoulder joint position is normal, and the humeral head does not sink. (B) Thin-slice CT results of the left shoulder after surgery. High-density marker is visible in the scapular prosthesis. (C) 3D CT reconstruction of the left shoulder after surgery. However, since the CT value of PEEK material is indistinguishable from the soft tissue, the subtraction effect is not good.
3.2. CT of the left shoulder
The postoperative CT images showed a lack of autogenous scapula. A slightly high-density shadow was seen in the scapular region (Fig. 3B and C).
3.3. Constant score of the shoulder
The Constant score of left shoulder joint is 68 points. The shoulder joint activity: 120° on the lift, 90° adduction, 50° on the external rotation, and 70° on internal rotation (Fig. 4). The patient was satisfied with the results of the surgery.
Fig. 4.
The joint movement degree of the left shoulder 3 months after surgery.
3.4. Complications
Any complications, such as incision infection, effusion, joint dislocation, prosthesis rejection, prosthetic looseness, and prosthesis fracture, did not occur after the operation.
4. Discussion
A large number of patients present bone defects due to trauma, congenital malformation, and tumor resection every year. The repair of bone defects is yet a major challenge for orthopedic surgeons [5]. Autologous and allogeneic bones have limited application due to scarce sources, the possible transmission of diseases, and rejection. Therefore, the artificial bone substitute materials have are becoming favorable for bone defect repair. Recently, the clinical research is primarily focused on the medical titanium alloy material. However, some inherent properties of titanium alloy, such as the significant difference in the modulus of elasticity between titanium alloy and bone and the release of toxic metal ions, restrict its large-scale application [6]. Owing to the biocompatibility and elastic modulus, PEEK materials have more advantages than titanium alloy prostheses. Reportedly, PEEK materials can significantly reduce the occurrence of stress shielding [7].
As an emerging technology, 3D printing exhibits several advantages, such as high intensity, short preparation period, and manufacturing process without opening the mold. The 3D printing technology can fulfill the requirements of a highly individualized design, thereby displaying unique advantages [8] in the manufacture of artificial bone substitute material. The 3D-printed PEEK material overcomes the limitation that PEEK materials can only be prepared by injection molding and laser sintering; it is rather conducive to satisfying the need for customized clinical applications.
5. Conclusions
PEEK scapula material prepared by 3D printing technology has not yet been reported clinically. In this case, benign fibrous histiocytoma of the scapula recurred postoperatively, and hence, should be resected and reconstructed extensively. 3D-printed PEEK scapula is a quick preparation, light-weight, and cost-efficient with excellent biocompatibility. A stringent preoperative preparation allows precise intraoperative tumor resection and accurate reconstruction that is highly beneficial to the patient.
Declarations
Ethics approval
The study was approved by the Ethics Committee of Xijing Hospital, Air Force Medical University.
Consent for publication
Written informed consent was obtained from the patient for publication of his clinical details and/or clinical images. A copy of the consent form is available for review.
Availability of data and materials
All data generated or analyzed in this study are included in the article.
Competing interests
The authors declare that they have no competing interests.
Funding
This study was supported by The NationalKey Research and Development Program of China (grant number 2017YFC1104901), the National Natural Science Foundation of China (grant number 51,771,227), the National Natural Science Foundation of Youth Fund (grant number 51,501,223), and the Shaanxi Science and Technology Research and Development Program (grant number 2016GY198).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Authors’ contributions
ZG conceived and designed the study. ZG, DL, JF, HF, and XX performed the study. LW, DL, and ED contributed towards the preparation of the PEEK prosthesis. ZG and DL drafted the manuscript. ZG, LW, JF, HF, DL, ED, and XX reviewed and edited the manuscript. All authors provided intellectual input to the study and approved the final version of the manuscript.
Acknowledgments
Not applicable.
Contributor Information
Ling Wang, Email: menlwang@mail.xjtu.edu.cn.
Zheng Guo, Email: guozheng@fmmu.edu.cn.
References
- 1.Matsuno T. Benign fibrous histiocytoma involving the ends of long bone. Skelet. Radiol. 1990;19:561–566. doi: 10.1007/BF00241277. [DOI] [PubMed] [Google Scholar]
- 2.Grohs J.G., Nicolakis M., Kainberger F., Lang S., Kotz R. Benign fibrous histiocytoma of bone: a report of ten cases and review of literature. Wiener klinische Wochenschrift. 2002;114:56–63. [PubMed] [Google Scholar]
- 3.Basarir K., Saglik Y., Yildiz Y. Benign fibrous histiocytoma of the hand: a case report and literature review. Hand Surg.: Int. J. Devoted Hand Upper Limb Surg. Rel. Res.: J. Asia-Pacific Fed. Soc. Surg. Hand. 2008;13:99–102. doi: 10.1142/S0218810408003876. [DOI] [PubMed] [Google Scholar]
- 4.Pimentel J., Fernandes A., Tavora L., Miguens J., Lobo Antunes J. Benign isolated fibrohistiocytic tumor arising from the central nervous system. Considerations about two cases. Clin. Neuropathol. 2002;21:93–98. [PubMed] [Google Scholar]
- 5.Kutikov A.B., Skelly J.D., Ayers D.C., Song J. Templated repair of long bone defects in rats with bioactive spiral-wrapped electrospun amphiphilic polymer/hydroxyapatite scaffolds. ACS Appl. Mater. Interfaces. 2015;7:4890–4901. doi: 10.1021/am508984y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sagomonyants K.B., Jarman-Smith M.L., Devine J.N., Aronow M.S., Gronowicz G.A. The in vitro response of human osteoblasts to polyetheretherketone (PEEK) substrates compared to commercially pure titanium. Biomaterials. 2008;29:1563–1572. doi: 10.1016/j.biomaterials.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Lee W.T., Koak J.Y., Lim Y.J., Kim S.K., Kwon H.B., Kim M.J. Stress shielding and fatigue limits of poly-ether-ether-ketone dental implants, Journal of biomedical materials research. Part B. Appl. Biomater. 2012;100:1044–1052. doi: 10.1002/jbm.b.32669. [DOI] [PubMed] [Google Scholar]
- 8.Inzana J.A., Olvera D., Fuller S.M., Kelly J.P., Graeve O.A., Schwarz E.M., Kates S.L., Awad H.A. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials. 2014;35:4026–4034. doi: 10.1016/j.biomaterials.2014.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed in this study are included in the article.