Highlights
-
•
Adenosquamous carcinoma is a rare colorectal tumor with both glandular and squamous histologic component.
-
•
To the best of our knowledge only few cases have been reported in the literature till date.
-
•
Adenosquamous carcinoma is a rare colorectal neoplasm with non-specific complaints.
-
•
Its clinicopathologic behavior is not understood.
-
•
Preoperative diagnosis is often difficult. Surgical resection remains the mainstay of treatment.
Abbreviation: ASC, Adenosquamous carcinoma
Keywords: Case report, Adenosquamous carcinoma, Right hemicolectomy
Abstract
Introduction
Adenosquamous carcinoma is a rare colorectal tumor with both an adenocarcinoma and a squamous cell carcinoma component. To the best of our knowledge, only few cases have been reported in the literature.
Case presentation
We report a case of a 46-year-old woman, hospitalized for large bowel obstruction syndrome. Computed tomography scan showed an irregular mass of the right colic angle, responsible for an occlusive syndrome with distension of the right colon, the appendix and the terminal ileum. The patient underwent right hemicolectomy with D2 lymphadenectomy. Histopathological examination revealed mixed adenocarcinoma and squamous carcinoma. Adjuvant chemotherapy was prescribed for the patient.
Discussion
Adenosquamous carcinoma is a rare colorectal neoplasm revealed by non-specific complaints. Its clinicopathology is not yet understood. Preoperative diagnosis is often difficult. Surgical resection remains the mainstay of treatment.
Conclusion
Adenosquamous carcinoma is a malignant tumor with poorer prognosis than adenocacinomas.
1. Introduction
The incidence of colorectal cancers is increasing throughout the world, the majority of them being adenocarcinoma. Adenosquamous carcinoma (ASC) is very rare [1]. The incidence is around 0.06% of all colorectal malignant tumors [2]. This rare entity is characterized by the presence of both adenocarcinoma and squamous cell carcinoma components, and is characterized by greater potential of metastasis than adenocacinoma [3].Thus, early detection and treatment of ASC is important.
The aim of this study is to describe a rare case of ASC in a 46-year-old female, who presented with large bowel obstruction syndrome treated by surgical resection and adjuvant chemotherapy. This case has been reported in line with the SCARE criteria [4].
2. Case description
A 46-year-old female presented with a two-day history of abdominal distention, nausea, vomiting, and crampy abdominal pain. The level of hemoglobin was 9 g/dl. There were no other abnormal laboratory findings.
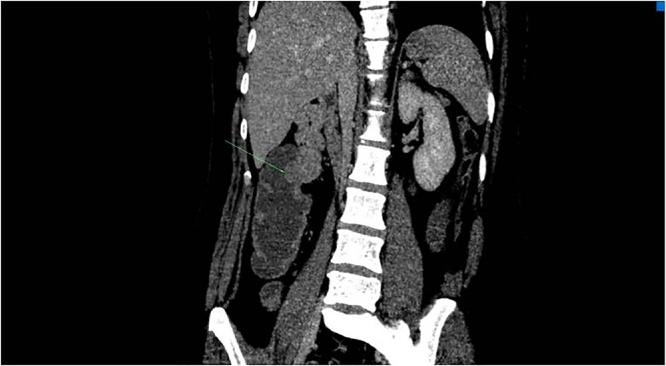
A computed tomography (CT) scan of the abdomen showed an obstructive, irregular mass of the right colic flexure, responsible for distension of the right colon, the appendix and the terminal ileum. (Fig. 1).
Fig. 1.
Irregular process tissue of the right colic angle, responsible for an occlusive syndrome with distension of the right colon, the appendix and the terminal ileum.
Emergency laparotomy revealed the presence of tumor in the ascending colon without liver or peritoneal metastases. The first step consisted of an approach of the superior mesenteric vessels. The patient had a right hemicolectomy with lymph node dissection, without intestinal anastomosis. Ovariectomy was not performed, as the ovaries were free from secondary lesions or locoregional invasion. Finally, the mass was diagnosed as a colic ASC of stage IIIB (T3 N2a M0) according to the seventh edition of the colon and rectum cancer staging system published by the American Joint Committee on Cancer (Fig. 2, Fig. 3, Fig. 4, Fig. 5).
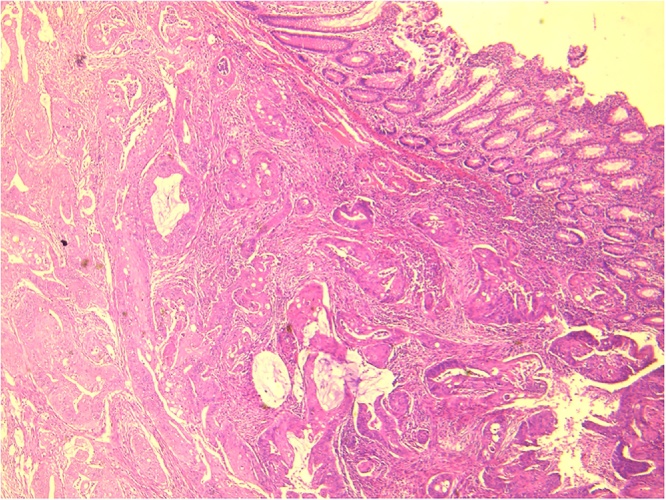
Fig. 2.
Infiltrating carcinomatous proliferation of the colonic wall (HEx40).
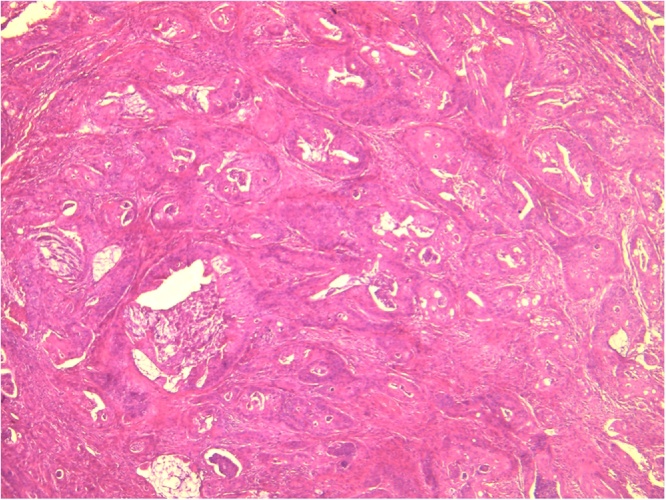
Fig. 3.
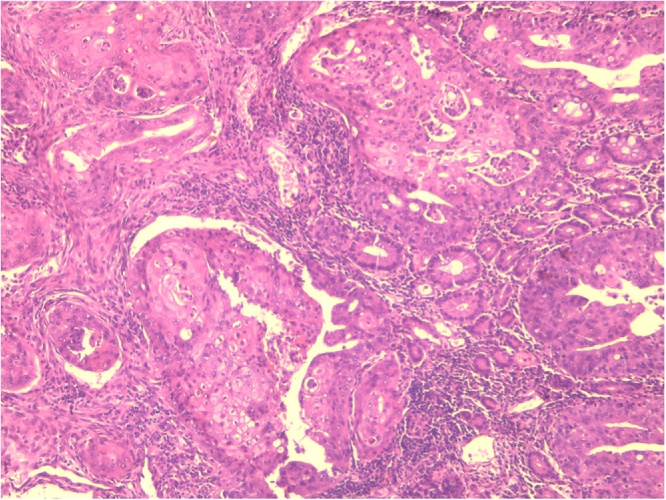
The proliferation is formed by two entangled components (HEx40).
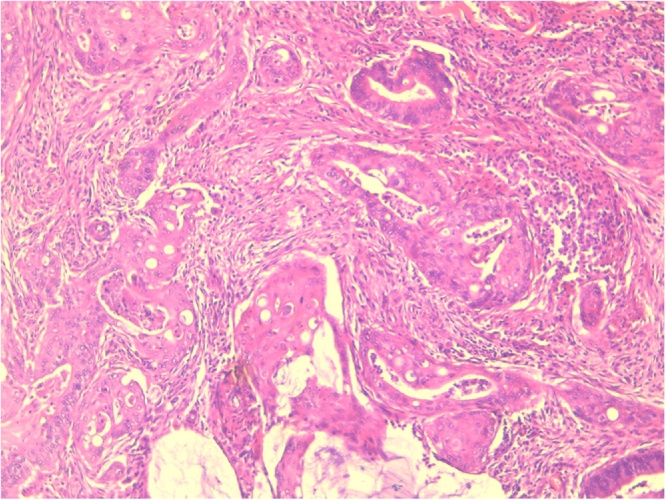
Fig. 4.
Glands covered with basophilic columnar cells.
Fig. 5.
Squamous differentiation (HEx100).
The patient received adjuvant chemotherapy that consisted of 12 injections of FOLFOX4 (oxaliplatin, leucovorin, and fluoro uracil) regimen. This chemotherapy was well tolerated by the patient.
After completion of the adjuvant chemotherapy, the patient had regular visits every 3–4 months. At each visit, she had a physical examination and was checked for abnormal functional symptoms. CT scans were performed annually; chest X-ray and abdominal ultrasound were performed every 6 months.
There has been no evidence of tumor recurrence during the 18 months follow up after the completion of adjuvant chemotherapy.
3. Discussion
ASC of the colon accounts for 0.02%–0.06% of all colorectal malignant tumors [2,5]. The first case was reported by Herxheimer in 1907 [3]. In 1999, Cagir et al. [2] reported 145 cases of ASC. To our knowledge, this is the first case reported in Tunisia. The pathogenesis of ASC is unclear. Several hypotheses have been advanced for its histogenesis in the gastrointestinal tract. Four hypotheses have been suggested:
-
1)
Ectopic squamous cells in the colonic mucosa may be directly transformed into squamous malignant cells.
-
2)
Undifferentiated or reserve cells in the colonic epithelium may be transformed directly into squamous cell carcinoma.
-
3)
Normal glandular cells may be transformed into a malignant squamous neoplasm.
-
4)
Adenocarcinomas in situ can directly be transformed into malignant squamous cells [[5], [6], [7]].
In the review of Cagir et al., the mean age of patients was 67 years [2], with male predominance (57%) [3] and the sex-ratio was 1.34. These findings contrast with those of our case, our patient being an old female in her fifth decade of life.
In the review of Cagir et al. [2] 53% of the carcinomas were located in the sigmoid colon, rectum, and anus, 28% in the right colon (cecum and ascending colon), and 19% in the middle segment (transverse colon and descending colon). In our case the tumor was located in the right colon.
The clinical signs and symptoms are those of a typical colonic adenocarcinoma. The squamous cell component has been reported to have greater metastatic potential than the glandular cell component. Thus, patients may experience more aggressive clinical symptoms. Indeed, in our observation, bowel obstruction was the first sign.
ASC of the colon, though rare, has been associated with a worse prognosis than colorectal adenocarcinoma.
The treatment of ASC is a colectomy with regional mesenteric lymph nodes dissection. Because of the rarity of this entity, the role of adjuvant chemotherapy is unknown [8,5]. The most commonly used adjuvant chemotherapeutic agents are semustine, 5-fluorouracil, carmustine, and methotrexate. However, the precise impact of these drugs on the outcome is not yet known due to the rarity of this tumor and the lack of clinical trial data. Another patient with ASC had been treated with combination of chemotherapy and radiotherapy. In fact, patients who had ASC with lymph node involvement, had poorer prognosis, and the treatment with chemoradiotherapy may lead to more favorable results [8]. The patient in our case had ASC with lymph node involvement, that’s why she underwent adjuvant chemotherapy. She showed no evidence of recurrence in the 18 months of follow up post resection.
Frizelle et al. [1] reported a 5-year survival rate of 86% for patients with Stage II disease and only 24% for patients with Stage III disease.
4. Conclusion
ASC of the colon is rare and associated with a worse prognosis than adenocarcinoma. Since the efficacy of adjuvant chemotherapy and radiation therapy for ASC of the colon has not been yet elucidated, surgical resection remains the best therapeutic option.
Conflicts of interest
The authors declare that they have no conflict of interest.
Sources of funding
This study has not received any funding.
Ethical approval
The study was approved by Ethics Committee of Hospital fattouma bourguiba monastir.
Consent
Written informed consent was obtained from the patient.
Author’s contribution
Study concept or design – OT, HA, AB
Data collection – MN, BH, AD,
Data interpretation – FN, HA, RG
Literature review – SB, KZ, SZ,
Drafting of the paper – AD, RG, SZ
Editing of the paper – FN, SB,MN,
Registration of research studies
As this was a case report and not a clinical trial, this study does not require registration.
Guarantor
Omar Toumi.
Contributor Information
Omar Toumi, Email: toumi.amor@rns.tn.
Badii Hamida, Email: badii@hotmail.com.
Manel Njima, Email: manelji@hotmail.com.
Amal Bouchrika, Email: bouchrika@hotmail.com.
Houssem Ammar, Email: hosshoss24@hotmail.fr.
Amira Daldoul, Email: amiradld@hotmail.com.
Sonia Zaied, Email: soniazay@hotmail.com.
Sadok Ben Jabra, Email: sadokben@hotmail.com.
Rahul Gupta, Email: rahul.g.85@gmail.com.
Faouzi Noomen, Email: faouzinoomen@yahoo.fr.
Khadija Zouari, Email: khadija.zouari@rns.tn.
References
- 1.Frizelle F.A., Hobday K.S., Batts K.P., Nelson H. Adenosquamous and squamous carcinoma of the colon and upper rectum: a clinical and histopathologic study. Dis. Colon Rectum. 2001;44:341–346. doi: 10.1007/BF02234730. [DOI] [PubMed] [Google Scholar]
- 2.Cagir B., Nagy M.W., Topham A., Rakinic J., Fry R.D. Adenosqua-mous carcinoma of the colon, rectum, and anus: epidemiology,distribution,and survival characteristics. Dis. Colon Rectum. 1999;42:258–263. doi: 10.1007/BF02237138. [DOI] [PubMed] [Google Scholar]
- 3.Choi J.W., Park H.U. Adenosquamous carcinoma of the ascending colon: a case report and review of the literature. Ann. Coloproctol. 2013;29:83–86. doi: 10.3393/ac.2013.29.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Petrelli N.J., Valle A.A., Weber T.K., Rodriguez-Bigas M. Adenosquamous carcinoma of the colon and rectum. Dis. Colon Rectum. 1996;39:1265–1268. doi: 10.1007/BF02055120. [DOI] [PubMed] [Google Scholar]
- 6.Kang D.B., Oh J.T., Jo H.J., Park W.C. Primary adenosquamous carcinoma of the colon. J. Korean Surg. Soc. 2011;80:31–35. doi: 10.4174/jkss.2011.80.Suppl1.S31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duncan V.E., Harada S., Stevens T.M. Primary colon adenosquamous carcinoma in a patient with lynch syndrome: a new histologic subtype associated with microsatellite instability? Int. J. Surg. Pathol. 2016;24:653–655. doi: 10.1177/1066896916659539. [DOI] [PubMed] [Google Scholar]
- 8.Shafaghi A., Askari K., Ashoobi M.T., Mansour-Ghanaei F. Adenosquamous carcinoma of the sigmoid colon: a case report and review of literature. Int. J. Clin. Exp. Med. 2013;6:390–392. [PMC free article] [PubMed] [Google Scholar]