Abstract
Purpose
To explore 10-year longitudinal predictors (personal, psychological, behavioral and socio-environmental) of exiting obesity from adolescence to young adulthood.
Methods
Data were collected from a population-based cohort of adolescents (n=2,287) attending middle/high schools in Minneapolis-St. Paul in 1998–1999 (mean age=14.9) and again in 2008–2009 (mean age=25.3) participating in Project EAT. Self-reported height and weight were used to calculate weight status change between adolescence and young adulthood, among participants with obesity at baseline (n=175). Questionnaires assessed personal, psychological, behavioral and socio-environmental factors hypothesized to play a role in obesity. Modified Poisson regressions estimated adjusted relative risks (RR) for exiting obesity as a function of each baseline and 10-year change in predictor, controlling for relevant covariates.
Results
Thirty-two percent of adolescents exited obesity in young adulthood. Reductions in fast food intake (RR=0.73, 95% CI=0.61–0.87) and screen time (RR=0.98, 95% CI=0.96–0.99), and increases in fruit/vegetable intake (RR=1.06, 95% CI 1.01–1.12), moderate-to-vigorous physical activity (RR=1.06, 95% CI=1.00–1.12), home fruit/vegetable availability (RR=1.58, 95% CI=1.19–2.09), family meals (RR=1.12, 95% CI=1.03–1.22), and serving vegetables at dinner (RR=1.45, 95% CI=1.10–1.92) were associated with exiting obesity. Not dieting as an adolescent, and improvements in body satisfaction, depressive symptoms, self-esteem, and weight teasing were also associated with exiting obesity.
Conclusions
Promoting healthy eating and activity, and improving the healthfulness of home food environments may be promising intervention targets for promoting healthier weights in adolescents and young adults with obesity. Addressing dieting behavior and the psycho-social health of adolescents with obesity may also be needed throughout the transition to young adulthood.
Keywords: adolescent obesity, young adulthood, weight-loss
Current estimates suggest that 20% of US adolescents have obesity,[1] a weight status that increases their risk of experiencing negative psychosocial and health consequences.[2] Unfortunately, intervention programs that target weight-related behaviors (e.g. diet, activity) have had limited success in reducing adolescent obesity with no strong evidence of long-term effectiveness.[3] Furthermore, weight control practices commonly employed by adolescents (e.g., overly restricting food intake through dieting) are counterproductive and lead to increased weight gain over time.[4] Some behavioral strategies that might be effective in promoting successful weight loss come from adult participants of the National Weight Control Registry and include fat restriction, dietary restraint, regular self-weighing, and high levels of physical activity.[5] In non-adult populations, past weight loss reported by adolescents has been positively associated with behavioral strategies such as increasing physical activity, drinking less soda, and watching less television.[6] Socio-environmental factors, such as parent and peer support, modeling behaviors, and parents making positive changes to the home environment have also been identified as important for adolescent weight loss in weight management programs.[7–9]
In addition to what we have learned from studies examining individuals who are trying to lose weight, there is an opportunity to examine those who exit obesity in population-based samples may be more useful for informing population-based strategies to reduce adolescent obesity. In younger US school children, exit from obesity between fifth and tenth grade was associated with higher parent education, but not other behavioral/psychological baseline factors such as fast-food and soda consumption, exercise, TV watching, and body image.[10] In adolescent girls from ages 12–19 years, African American and Latina girls were more likely to exit overweight or obesity than European American girls when examined on one-year intervals.[11] Another study using National Health and Nutritional Examination Survey data identified greater physical activity, less sedentary time, and endorsement of efforts at trying to lose weight as correlates of past year weight loss among 16–18 year old adolescents with overweight or obesity.[12]
These previous studies did not examine weight loss that was maintained into young adulthood and did not examine the many psychological or socio-environmental factors that might be important for successful weight loss in a population-based sample. For example, there may be more favorable social (e.g., peer and parent influences) and environmental (e.g., home food environment) contexts in adolescence that support the behaviors and psychological state that lead to weight change. Other factors such as gender, ethnicity, socio-economic status (SES), dieting and body dissatisfaction have been implicated in adolescent weight gain[13,14] and may also play a role in weight loss from adolescence to young adulthood.
To address these gaps, this study utilized data from Project EAT (Eating and Activity Among Teens and Young Adults), an ongoing population-based longitudinal study that includes the collection of weight-related behavior and outcome data from a group of adolescents as they transition to young adulthood. Project EAT provides a unique opportunity to examine a comprehensive set of factors that may influence weight outcomes over a 10-year period. Predictors of incident overweight or obesity have been examined in this data to inform obesity prevention efforts,[14,15] but very little is known about how to successfully manage adolescents who already have obesity.[16] Therefore, the aim of this study was to examine the personal, psychological, behavioral and socio-environmental contexts of adolescence with obesity and to identify factors associated with exiting obesity. Exiting obesity was examined because it represents a clinically meaningful change in weight-related health risk.[17] The selection of predictor variables examined in this study was informed by social cognitive theory and socio-ecological models of health behavior,[18] and reflects variables that our team have found to be important for adolescent weight-related health through our work over the past decade on Project EAT.[15,18] It was hypothesized that a range of factors including healthy eating, physical activity, home availability of healthy foods, and a positive body image would predict a favorable weight status change. The identification of key factors that are amenable to change or that can be used to identify individuals at increased risk of maintaining a high body weight will guide intervention strategies during the transition from adolescence to adulthood.
METHODS
Study Design and Population
Baseline data were collected from 4,746 Project EAT participants: middle/high school students attending 31 public schools in the Minneapolis/St. Paul metropolitan area of Minnesota who completed in-class surveys in 1998–1999. Among those who could be contacted at 10-year follow-up (2008–2009), 2,287 young adults (66.4% response rate) completed online surveys investigating changes in previously assessed health behaviors. Previous studies have found little impact of mode (paper-and-pencil vs. online surveys) in adolescent reporting of health behavior.[19] At both time points, the majority of surveys were completed during the late fall and winter months (October-March). Informed consent was obtained from all study participants and protocols were approved by the University of Minnesota’s Institutional Review Board.
Measures
Survey measures were tested in pilot studies (focus groups and test-retest examined over a two week period) with adolescents at baseline and young adults at 10-year follow-up. Details are described elsewhere.[18]
Height and Weight
Self-reported height and weight were used to calculate body mass index (BMI) (kg/m2), and age and sex adjusted BMI percentile based on CDC growth charts for children and adolescents.[20] At baseline and follow-up, self-reports were highly correlated with measured height and weight in validation studies carried out in a subsample of adolescents (r=0.88 males; r=0.85 females) and young adults (r=0.95 males; r=0.98 females). At baseline, adolescents were classified as having obesity (BMI ≥ 95th percentile). At follow-up, young adults were classified based on CDC cut-points for adults: non-overweight=BMI < 25kg/m2; overweight=BMI ≥ 25kg/m2 and <30 kg/m2; and obesity=BMI ≥ 30 kg/m2.[17]
Psychological
Body dissatisfaction was assessed using items from the Body Shape Satisfaction Scale.[21] Participants described level of dissatisfaction related to 10 different body parts. Responses ranged from 'very satisfied' to 'very dissatisfied' on a 5-point scale for each body feature. All items were summed for an overall score, with higher scores indicating higher overall body dissatisfaction (range: 10–50, Cronbach’s α = .92).
Weight concern was assessed from two items: "I think a lot about being thinner" and "I am worried about gaining weight" using a 4-point Likert scale from ‘strongly disagree’ to ‘strongly agree’ (range: 2–8, Cronbach's α = .86).
Depressive symptoms were assessed using Kandel and Davies’ six-item scale[22] for adolescents by asking participants how often they had been bothered or troubled by six different symptoms of depression over the past 12 months (e.g., hopelessness, worry), with responses being not at all, somewhat and very much (range: 6–18, Cronbach's α=.84).
Self-esteem was assessed via six items from the Rosenberg Self-Esteem Scale (e.g., “on the whole, I am satisfied with myself”, “I feel that I have a number of good qualities”) with responses ranging ‘strongly disagree to ‘strongly agree’ on a 4-point Likert scale (range: 6–24, Cronbach's α=.71).
Behavioral
Daily servings of fruits and vegetables, snack food and soda were obtained from the 2007 Willett semi-quantitative food frequency questionnaire at follow-up and the youth version of this questionnaire at baseline. The validity and reliability of these measures were assessed in previous studies.[23,24] In addition, comparability of these estimates were examined in 91 male and 103 female participants who completed both versions of the questionnaire approximately 3 weeks apart; Pearson correlations in mean intake of these food groups were found to be moderate (0.5–0.6).[25] Frequency of fast food intake and eating breakfast (range: 0–7 times per week) were self-reported for the past week.
Moderate-to-vigorous physical activity (MVPA) was measured with the Leisure Time Exercise Questionnaire.[26] Two survey items individually assessed hours per week spent in strenuous intensity (e.g., biking fast, aerobics, jogging) and moderate intensity exercise (e.g., walking quickly, easy bicycling, volleyball, skiing). This tool was validated against accelerometer-derived MVPA in a sub-study of follow-up participants, with associations between the two methods considered good (r=0.40).[27] Screen time was assessed using items adapted from Planet Health[28] that asked participants to report the number of hours per weekday and weekend day they spend watching TV & videos.
Dieting was assessed with the question, “How often have you gone on a diet during the last year? By ‘diet’ we mean changing the way you eat so you can lose weight.” Responses ranged from 0=never to 5=I am always dieting. A list of nine weight control behaviors was used to assess past year use (yes/no) of any unhealthy weight control behavior (e.g., fasting, very little food, food substitute, meal skipping, and smoking; range 0–9) or extreme weight control behavior (e.g., diet pills, vomiting, laxatives, and diuretics; range 0–4).
Socio-environmental Characteristics
Home food availabiliy was assessed by asking about the availability of fruits and vegetables (1-item) and low-nutrient, high-caloric snack foods (3-items); the frequency of involvement in meal preparation (range: 0–7 times per week); and the frequency of having vegetables served at dinner (responses ranged from 1=never to 4=always). The frequency of family meals was also assessed (range: 0–7 times per week). In young adulthood an additional response option was “I live alone” and these respondents were counted as never eating family meals.
Mother and peer eating and physical activity attitudes were assesed by asking separately about how much their mother and most of their friends cared about staying fit and active and how much their mother and most of their friends cared about eating healthy food. Mother/peer dieting was assessed by asking seperately if mother/friends dieted to lose weight or keep from gaining weight. Responses to these items ranged from 1=not at all to 4=very much. Weight-teasing was assessed with the item, “How often were you teased about your weight?”; responses ranged from 1=never to 5=at least once a week. Mother’s weight status was assessed by the adolescent’s description of very underweight, underweight, just about right, overweight, or very overweight. Responses were categorized as overweight (overweight or very overweight) and non-overweight.
Demographics
Age, sex, race/ethnicity, and SES were based on self-report at baseline. Five levels of SES were based on the highest educational attainment by either parent. Where this information was missing, eligibility for public assistance, eligibility for free/reduced cost school meals, and parental employment status were used to infer SES. Information was also collected on the highest level of education achieved at follow-up.
Analysis
Of the 2,287 young adults who completed follow-up surveys, analyses were restricted to 175 adolescents who were classified as obese at baseline (based on self-reported height and weight). Adolescents who exited obesity (i.e., moved to overweight or non-overweight) were compared to those whose obesity persisted at follow-up.
Paired t-tests were used to test for mean changes in psychological, behavioral and socio-environmental characteristics from baseline to follow-up. Modified Poisson regression (Poisson regression with robust standard errors)[29] was used to model relative risk ratios (RR) for exiting obesity as a function of baseline and 10-year changes in each psychological, behavioral and socio-environmental factor, controlling for adolescent age, gender, race/ethnicity and SES. Additionally, models examining 10-year changes in each independent variable were adjusted for the baseline value so that comparisons represented individuals who were identical on the factor as adolescents. It was of interest to examine both baseline and 10-year changes in each predictor to determine if: 1) factors in adolescence conferred a weight-loss benefit in young adulthood; and 2) if more favorable changes to these factors were associated with a corresponding change in weight status. Because adolescents who completed both baseline and follow-up surveys represent 48.2% of the original school based sample (n=4,746), regression models were adjusted for non-response rates between baseline and follow-up using the response propensity method, described in detail elsewhere,[30] to produce estimates generalizable to the diverse young people of the Minneapolis/St. Paul metropolitan area. All analyses were conducted in STATA version 13 (Statacorp LP, College Station, TX, USA) and a p-value <0.05 was considered statistically significant.
RESULTS
Of the 175 adolescents with a BMI≥95th percentile, their mean age was 14.9 (SD=4.1) at baseline and 25.3 (SD=1.7) at follow-up; 38.3% were female. Over half (57%) of adolescents identified as white, 17% identified as Asian American, 14% identified as black, 8% as mixed/other, and 6% as Hispanic. This sample of adolescents also represented a range of SES (16% low, 23% low-middle, 27% middle, 25% middle-high, and 9% high).
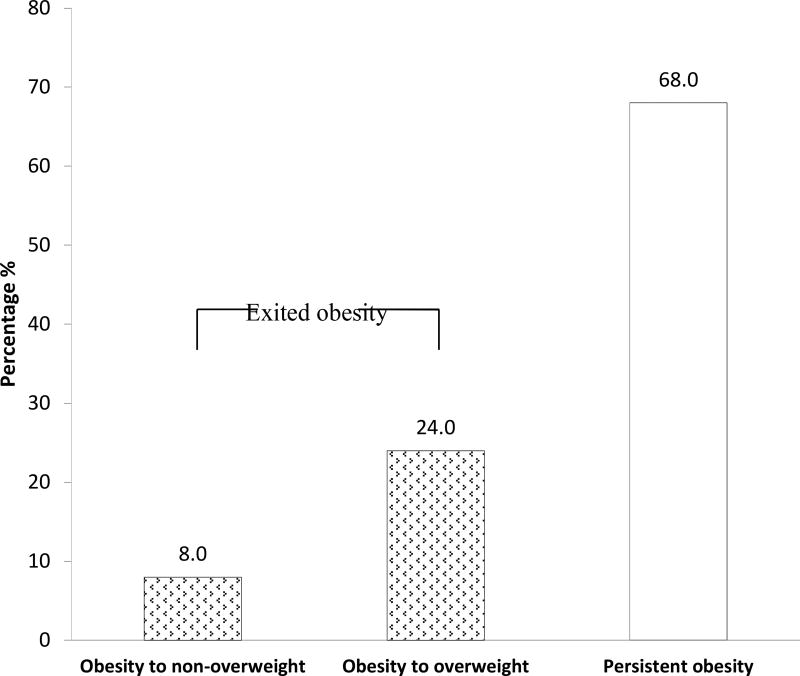
The majority of adolescents with obesity at baseline (68%) demonstrated persistent obesity in young adulthood; however, 32% exited obesity. Of these adolescents, approximately 24% transitioned from obesity to overweight, while 8% transitioned from obesity to non-overweight (Figure 1).
Figure 1.
Ten-year patterns of weight status change from adolescence to young adulthood among adolescents with a body mass index (BMI) ≥ 95th percentile at baseline (n=175).
1Weight categories are mutually exclusive and based on CDC cut-points for adolescents and adults:
Non-overweight=BMI <25 kg/m2 in adulthood;
Overweight ≥25 kg/m2 and <30 kg/m2 in adulthood;
Obesity=BMI≥95th percentile in adolescence and ≥30 kg/m2 in adulthood.
Baseline predictors of exiting obesity
Table 1 presents the demographic, psychological, behavioral and socio-environmental characteristics of adolescents with obesity at baseline. In models adjusting for demographics, only dieting was associated with exiting obesity: adolescents who reported dieting were less likely to exit obesity by young adulthood (RR=0.56, 95% CI=0.35–0.88) (Table 2). No other baseline characteristics predicted moving to a more favorable weight status in young adulthood. Educational attainment at follow-up was also unrelated to exiting obesity (data not shown).
Table 1.
Baseline and 10-year changes in psychological, behavioral and socio-environmental characteristics of adolescents with a BMI ≥95th percentile (n=175).
| Baseline | 10-year Change | |||
|---|---|---|---|---|
|
| ||||
| Characteristic | n | Mean ± SD or % |
n | Change in mean or % (95% CI) |
| Psychological | ||||
| Body dissatisfaction | 170 | 28.9± 8.9 | 170 | 1.79 (0.4, 3.2) |
| Depressive symptoms | 168 | 10.4± 2.8 | 168 | 0.9 (0.4, 1.5) |
| Self-esteem | 167 | 17.5± 3.4 | 167 | 0.04 (−0.6, 0.7) |
| Weight concern | 175 | 8.1± 2.3 | 171 | 2.4 (2.0, 2.8) |
| Behavioral | ||||
| Fruit and vegetables, servings/day | 153 | 3.9±2.8 | 129 | 0.4 (−0.2, 1.1) |
| Snack foods, servings/day | 149 | 2.3±2.1 | 125 | −0.5 (−0.9, −0.1) |
| Sugar-sweetened beverages, servings/day | 175 | 1.7±1.2 | 145 | −0.9 (−1.2, −0.7) |
| Fast food, times/wk | 175 | 1.6±1.4 | 174 | 0.1 (−0.2, 0.4) |
| Breakfast eating, days/wk | 175 | 3.6±2.6 | 175 | −0.2 (−0.7, 0.3) |
| MVPA, hours/wk | 168 | 5.6±4.5 | 168 | −1.7 (−2.5, −1.0) |
| Screen time, hours/wk | 166 | 29.2±15.3 | 166 | 3.6 (0.6, 6.7) |
| Dieting, % yes | 174 | 62.9% | 175 | 3.4 (−5.8, 12.6) |
| Unhealthy WCB, % yes | 175 | 60.0% | 175 | 2.3 (−6.8, 11.3) |
| Extreme WCB, % yes | 175 | 6.9% | 175 | 14.9 (8.5, 21.3) |
| Socio-Environmental | ||||
| Home food availability | ||||
| Fruits and vegetables | 175 | 3.4±0.7 | 174 | −0.4 (−0.5, −0.2) |
| Sweets/snacks | 175 | 2.7±0.6 | 175 | −0.3 (−0.4, −0.2) |
| Vegetables served at dinner, times/wk | 174 | 3.1±0.9 | 175 | −0.2 (−0.3, −0.003) |
| Involved in meal preparation, times/wk1 | 174 | 2.0±1.8 | - | |
| Family meals, times/wk | 174 | 3.7±2.4 | 174 | −0.3 (−0.8, 0.2) |
| Mother physical activity attitudes1 | 170 | 2.9±1.0 | - | |
| Mother healthy eating attitudes1 | 171 | 3.1±0.8 | ||
| Parent dieting1, % yes | 172 | 76.7% | - | |
| Perceived mother’s weight1, % overweight | 161 | 49.7% | - | |
| Peer physical activity attitudes | 168 | 2.6±1.0 | 168 | 0.2 (0.04, 0.4) |
| Peer healthy eating attitudes | 169 | 2.3±0.9 | 169 | 0.4 (0.2, 0.6) |
| Peer dieting, % yes | 169 | 65.1% | 169 | 15.4 (6.8, 24.0) |
| Weight-related teasing, % yes | 167 | 65.3% | 167 | −5.4 (−14.0, 3.2) |
BMI=body mass index; SD=standard deviation; CI=confidence interval; MVPA=moderate-to-vigorous physical activity; WCB=weight control behaviors
Bolded values are statistically significant at p<0.05
Variable only collected at baseline so changes could not be examined
Table 2.
Baseline and 10-year changes in personal, psychological, behavioral and socio-environmental factors predicting the likelihood of exiting obesity in young adulthood1
| Exiting Obesity2 | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Characteristic | Baseline predictor | 10-year change in predictor3 |
||||
|
|
|
|||||
| RR | 95%CI | p | RR | 95%CI | p | |
|
|
|
|||||
| Age | 0.90 | 0.76, 1.07 | 0.24 | - | ||
| Gender, female | 1.09 | 0.61, 1.95 | 0.78 | - | ||
| Ethnicity | ||||||
| White | Ref | - | ||||
| Black | 1.22 | 0.67, 2.24 | ||||
| Hispanic | 1.91 | 0.83, 4.37 | ||||
| Asian | 0.82 | 0.38, 1.74 | ||||
| Other/Mixed | 0.90 | 0.31, 2.60 | ||||
| Socio-economic background | ||||||
| Low | Ref | - | ||||
| Low-middle | 0.89 | 0.38, 2.10 | 0.52 | |||
| Middle | 0.79 | 0.34, 1.83 | 0.13 | |||
| Middle-high | 1.24 | 0.55, 2.80 | 0.60 | |||
| High | 1.36 | 0.62, 2.98 | 0.84 | |||
| BMI | 0.93 | 0.86, 1.01 | 0.10 | - | ||
| Psychological | ||||||
| Body dissatisfaction | 1.03 | 1.00, 1.06 | 0.08 | 0.94 | 0.92, 0.97 | <.001 |
| Depressive symptoms | 1.02 | 0.94, 1.11 | 0.64 | 0.91 | 0.84, 0.98 | 0.02 |
| Self-esteem | 1.04 | 0.95, 1.12 | 0.41 | 1.08 | 1.01, 1.16 | 0.04 |
| Weight concern | 0.95 | 0.86, 1.05 | 0.34 | 0.90 | 0.81, 1.00 | 0.06 |
| Behavioral | ||||||
| Fruit and vegetables, servings/d | 1.04 | 0.95, 1.15 | 0.36 | 1.06 | 1.01, 1.12 | 0.02 |
| Snack foods, servings/d | 1.05 | 0.96, 1.15 | 0.27 | 0.91 | 0.74, 1.11 | 0.35 |
| Sugar-sweetened beverages, servings/d | 1.04 | 0.82, 1.31 | 0.77 | 0.76 | 0.56, 1.03 | 0.08 |
| Fast food, times/wk | 1.07 | 0.91, 1.27 | 0.40 | 0.73 | 0.61, 0.87 | 0.001 |
| Breakfast eating, days/wk | 1.00 | 0.91, 1.10 | 0.97 | 1.03 | 0.92, 1.14 | 0.64 |
| MVPA, hours/wk | 0.96 | 0.91, 1.02 | 0.19 | 1.06 | 1.00, 1.12 | 0.03 |
| Screen time, hours/wk | 0.99 | 0.97, 1.01 | 0.23 | 0.98 | 0.96, 0.99 | 0.01 |
| Any dieting, yes/no | 0.56 | 0.35, 0.88 | 0.01 | 0.76 | 0.48, 1.19 | 0.23 |
| Any unhealthy WCB, yes/no | 0.75 | 0.46, 1.22 | 0.24 | 0.96 | 0.56, 1.63 | 0.88 |
| Extreme WCB, yes/no | 0.82 | 0.30, 2.23 | 0.70 | 0.92 | 0.50, 1.70 | 0.78 |
| Socio-Environmental | ||||||
| Home food availability | ||||||
| Fruits and vegetables | 0.89 | 0.64, 1.23 | 0.64 | 1.58 | 1.19, 2.09 | 0.001 |
| Sweets/snacks | 1.32 | 0.91, 1.92 | 0.14 | 0.77 | 0.55, 1.09 | 0.14 |
| Vegetables served at dinner, times/wk | 1.14 | 0.87, 1.48 | 0.33 | 1.45 | 1.10, 1.92 | 0.01 |
| Involved in meal preparation, times/wk4 | 1.04 | 0.90, 1.21 | 0.56 | - | ||
| Family meals, times/wk | 1.02 | 0.91, 1.14 | 0.78 | 1.12 | 1.03, 1.22 | 0.01 |
| Mother physical activity attitudes4 | 0.97 | 0.74, 1.28 | 0.85 | - | ||
| Mother healthy eating attitudes4 | 1.08 | 0.78, 1.49 | 0.65 | - | ||
| Parent dieting behaviors, yes/no4 | 1.42 | 0.72, 2.79 | 0.31 | - | ||
| Mother overweight, yes/no4 | 0.73 | 0.45, 1.19 | 0.20 | - | ||
| Peer physical activity attitudes | 0.92 | 0.69, 1.21 | 0.55 | 1.36 | 0.92, 2.00 | 0.13 |
| Peer healthy eating attitudes | 0.94 | 0.78, 1.13 | 0.54 | 0.90 | 0.70, 1.17 | 0.44 |
| Peer dieting behaviors, yes/no | 0.93 | 0.53, 1.64 | 0.81 | 1.27 | 0.57, 2.85 | 0.56 |
| Weight-related teasing, yes/no | 0.65 | 0.39, 1.09 | 0.10 | 0.37 | 0.22, 0.61 | <.001 |
CI=confidence interval; MVPA=moderate-to-vigorous physical activity; WCB=weight control behaviors
Bolded values are statistically significant at p<0.05
A risk ratio greater than 1.0 indicates a positive outcome, i.e., an increased likelihood of exiting overweight or obesity to a lower weight status in young adulthood
Analyses weighted to account for non-response and adjusted for age, gender, race/ethnicity and SES
Additionally adjusted for baseline value
Variables only collected at baseline; Demographics and BMI only examined as baseline predictors
Ten-year changes in psychological, behavioral and socio-environmental factors
Table 1 highlights the psychological, behavioral and socio-environmental factors that were significantly different between baseline (adolescence) and 10-year follow-up (young adulthood) among adolescents with obesity at baseline. Overall, patterns tended to worsen over time. Body dissatisfaction, depressive symptoms, weight concerns, screen time, extreme weight control behaviors, and peer dieting behaviors increased, while MVPA, home availability of fruit and vegetables, and the frequency of having meals served with vegetables decreased. Positive changes over this time period included an increase in fruit and vegetable intake, and peer interest in healthy eating and physical activity, and a decrease in home availability of snacks/sweets, sugar-sweetened beverage intake, and snack food consumption.
Ten-year changes associated with exiting obesity
In covariate-adjusted models, many psychological, behavioral and socio-environmental factors that changed from adolescence to young adulthood were significantly associated with exiting obesity after adjusting for baseline values (Table 2). An increase in fruit and vegetable intake (RR=1.06, 95% CI 1.01–1.12), availability of fruits and vegetables at home (RR=1.58, 95% CI=1.19–2.09), the frequency of having vegetables served with dinner (RR=1.45, 95% CI=1.10–1.92), and the frequency of family meals (RR=1.12, 95% CI=1.03–1.22), and a were decrease in fast food consumption (RR=0.73, 95% CI=0.61–0.87) and screen time (RR=0.98, 95% CI=0.96–0.99) were associated with exiting obesity by young adulthood. Reductions in body dissatisfaction (RR=0.94, 95% CI=0.92–0.97), depressive symptoms (RR=0.91, 95% CI=0.84–0.98) and weight-teasing (RR=0.37, 95% CI=0.22–0.61), and increases in self-esteem (RR=1.08, 95% CI=1.01–1.16) were associated with exiting obesity.
DISCUSSION
Much attention has been placed on the weight gain that often occurs from adolescence to adulthood. Indeed, we found that most adolescents have persistent obesity (68%). However, the results of this study highlight that a modest number of adolescents (32%) transition to a more favorable weight status in young adulthood (exit obesity). Importantly, we found a number of weight-related behaviors that were associated with moving to a lower weight status, namely reducing fast food intake and screen time, and increasing fruit and vegetable intake, home availability of fruits and vegetables, the number of times vegetables are served at dinner, and family meals. A decrease in body dissatisfaction, depressive symptoms, and weight-teasing, and an increase in self-esteem also occurred more frequently for adolescents who exited obesity in young adulthood. These factors may be promising targets for intervention and should be further examined in other samples and tested in intervention studies to determine their importance for promoting the transition to a healthier weight in adolescents and young adults who struggle with obesity.
We examined adolescents who exited obesity because of the health risks associated with obesity and the need for intervention strategies that target this group.[2,3] Examining this group of adolescents precluded identification of factors that might be associated with smaller amounts of weight loss (but not enough to shift someone out of obesity) or adolescents who were overweight and became a normal weight in young adulthood. However, the risks associated with overweight are less clear than those for obesity, and small changes in BMI could be the result of normal adolescent development and maturation (i.e. increased musculature and height)[31] or small fluctuations in weight. None the less, examination of these individuals may have revealed other factors important for intervention.
Overall, psychological, behavioral and socio-environmental changes from adolescence to young adulthood were in an unfavorable direction. Several of the observed changes have been documented in healthy weight samples (e.g. young adulthood is a time period associated with declining physical activity [32]) and some psychological changes were small and may have limited clinical relevance. However, these downward trends remain a concern and may explain why obesity persists in a large number of young adults. Of particular concern was that the percent engaging in extreme weight control behaviors more than doubled, from 7% to 22% and that increased dieting was associated with the persistence of obesity. These findings provide further support for the discouragement of these behaviors for effective weight management.
Potentially modifiable behaviors associated with exiting obesity included decreasing fast food intake and screen time, and increasing fruit and vegetable intake and MVPA, behaviors that have previously been identified as important targets for intervention.[33–35] Of particular interest were the findings that positive changes to the home food environment predicted exiting obesity, namely increasing the availability of fruits and vegetables, the frequency of serving vegetables with dinner, and more frequent family meals. These environmental changes may have helped to reduce overall energy intake by displacing the consumption of less healthful foods, perhaps through the observed increase fruit and vegetable consumption. Whether these changes were initiated by young adults themselves or by moving into a new environment influenced by someone else (e.g. roommate, partner, family member) is worthy of further exploration.
Several psychosocial factors were associated with exiting obesity, including a decrease in body dissatisfaction, depressive symptoms and weight-teasing, and an increase in self-esteem. It is possible that these changes (e.g., greater body satisfaction) occurred subsequent to weight loss.[36] On the other hand, previous work with adolescent girls has demonstrated that higher body satisfaction results in less weight gain over time, suggesting that body satisfaction may precede weight gain or loss.[37] Further benefits of positive self-esteem and body image for adolescent and young adult psychosocial health are well established.[38,39] Unexpectedly, baseline levels of body dissatisfaction, depressive symptoms, self-esteem, weight concern or teasing were not associated with exiting obesity by young adulthood in the present study; however, changes may have preceded the observed weight status change. Giving attention to these psychosocial factors in weight management and obesity interventions early on may help young adults achieve a healthier weight status.
Previous studies have demonstrated that early experiences predict weight status later on in life.[40] Only dieting in adolescence was found to be associated with persistent obesity in adulthood, but is an important finding that adds to the growing body of literature that suggests dieting has negative health consequences and is not a successful weight-loss strategy.[14] Overall, the results of this study suggest that 10-year changes in risk factors seemed to be more important for achieving a healthier weight status in young adulthood than the baseline context in adolescence. However, adolescents in this sample may have already established behaviors that were conducive to weight gain over time.
A limitation of this study is that 10-year changes in predictors may have occurred before or after weight loss; therefore, reverse causation is possible. In addition, attrition and self-reported measures may have biased the study findings. Compared to the original sample, adolescents who completed both the baseline and follow-up survey were more likely to be female, white and in the upper SES categories. However, sampling weights were used to correct for this bias. In addition, several validation studies were conducted that increase our confidence around the validity of the measures used for BMI, diet, and physical activity.[25,27] Finally, this study examined a comprehensive set of weight-related risk factors, but may have missed some important predictors of weight loss, including genetics. Unmeasured factors, such as living circumstances, associated with both changes in weight and changes in psychology, behavior, or environment may provide alternate explanations for why some adolescents exit obesity. The large number of predictors examined in this study may also result in spurious associations; therefore, findings should be replicated in other samples.
Conclusions
Addressing weight-related behaviors and outcomes during the transition from adolescence to young adulthood is critical given the majority of adolescents experience persistent obesity as young adults. This study identified a relatively large group, about one third of the population-based sample, who exited obesity and transitioned to a weight status in young adulthood that confers a lower health risk. Baseline weight status and demographic factors were unrelated to exiting obesity in this study, which suggests there may be limited opportunities to identify adolescents with obesity for whom interventions should be targeted. The present study did identify several psychological, behavioral and socio-environmental factors associated with exiting obesity that may be important targets for intervention, such as reducing fast food intake and screen time in addition to increasing MVPA, fruit and vegetable intake, home availability of fruits and vegetables, the number of times vegetables are served at dinner, and family meals. Interventions that aim to increase body satisfaction and self-esteem, and decrease dieting attempts, weight concern, and weight-teasing may also be beneficial and deserve great attention. The development and evaluation of interventions that focus on these factors during the transition from adolescence to adulthood may hold promise for adolescent obesity management.
IMPLICATIONS AND CONTRIBUTION.
This study identified several intervention targets for adolescents with obesity that may help promote healthier weight status in young adulthood. These include: reducing fast food intake, screen time, dieting, body dissatisfaction, depressive symptoms, low self-esteem, and weight-teasing; and increasing fruit and vegetable intake, moderate-to-vigorous physical activity, home availability of fruits and vegetables, serving vegetables with dinner, and family meals.
Acknowledgments
This study was supported by Grant Number R01HL084064 from the National Heart, Lung, and Blood Institute (PI: Dianne Neumark-Sztainer). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. AWW was supported by a fellowship from the Canadian Institutes of Health Research. All parties who contributed to this week are included as authors.
Abbreviations
- OW/OB
Overweight or obesity
- SES
Socio-economic Status
- BMI
Body Mass Index
- MVPA
moderate-to-vigorous physical activity
- RR
Relative Risk Ratio
- CI
Confidence Interval
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None
Parts of these results were presented at the Annual Meeting of the International Society for Behavioral Nutrition and Physical Activity in Edinburgh, Scotland.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reilly J, Kelly J. Long term impact of overweight and obesity. Int J Obes. 2011;35:891–8. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 3.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;3:1–57. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Macpherson-Sánchez AE. Integrating fundamental concepts of obesity and eating disorders: implications for the obesity epidemic. Am J Public Health. 2015;105:e71–85. doi: 10.2105/AJPH.2014.302507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas JG, Bond DS, Phelan S, et al. Weight-loss maintenance for 10 years in the national weight control registry. Am J Prev Med. 2014;46:17–23. doi: 10.1016/j.amepre.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 6.Boutelle KN, Libbey H, Neumark-Sztainer D, et al. Weight control strategies of overweight adolescents who successfully lost weight. J Am Diet Assoc. 2009;109:2029–35. doi: 10.1016/j.jada.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Jensen CD, Duraccio KM, Hunsaker SL, et al. A qualitative study of successful adolescent and young adult weight losers: Implications for weight control intervention. Child Obes. 2014;10:482–90. doi: 10.1089/chi.2014.0062. [DOI] [PubMed] [Google Scholar]
- 8.Gierut KJ, Pecora KM, Kirschenbaum DS. Highly successful weight control by formerly obese adolescents: A qualitative test of the healthy obsession model. Child Obes. 2012;8:455–65. doi: 10.1089/chi.2012.0101. [DOI] [PubMed] [Google Scholar]
- 9.Golan M. Parents as agents of change in childhood obesity - from research to practice. Int J Pediatr Obes. 2006;1:66–76. doi: 10.1080/17477160600644272. [DOI] [PubMed] [Google Scholar]
- 10.Schuster MA, Elliott MN, Bogart LM, et al. Changes in obesity between fifth and tenth grades: A longitudinal study in three metropolitan areas. Pediatrics. 2014:2014–195. doi: 10.1542/peds.2014-2195. [DOI] [PubMed] [Google Scholar]
- 11.Huh D, Stice E, Shaw H, et al. Female overweight and obesity in adolescence: Developmental trends and ethnic differences in prevalence, incidence, and remission. J Youth Adolesc. 2011;41:76–85. doi: 10.1007/s10964-011-9664-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boutelle KN, Hannan PJ, Neumark-Sztainer D, et al. Identification and correlates of weight loss in adolescents in a national sample. Obesity. 2007;15:473–82. doi: 10.1038/oby.2007.501. [DOI] [PubMed] [Google Scholar]
- 13.Sherwood NE, Wall M, Neumark-Sztainer D, et al. Effect of socioeconomic status on weight change patterns in adolescents. Prev Chronic Dis. 2008;6:A19. [PMC free article] [PubMed] [Google Scholar]
- 14.Neumark-Sztainer D, Wall M, Story M, et al. Dieting and unhealthy weight control behaviors during adolescence: Associations with 10-year changes in body mass index. J Adolesc Health. 2012;50:80–6. doi: 10.1016/j.jadohealth.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quick V, Wall M, Larson N, et al. Personal, behavioral and socio-environmental predictors of overweight incidence in young adults: 10-yr longitudinal findings. Int J Behav Nutr Phys Act. 2013;10:37. doi: 10.1186/1479-5868-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reinehr T, Kleber M, Lass N, et al. Body mass index patterns over 5 y in obese children motivated to participate in a 1-y lifestyle intervention: age as a predictor of long-term success. Am J Clin Nutr. 2010;91:1165–71. doi: 10.3945/ajcn.2009.28705. [DOI] [PubMed] [Google Scholar]
- 17.NHLBI Obesity Education Initiative Expert Panel on the Identification. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda, MD: National Heart, Lung, and Blood Institute; 1998. Evaluation, and Treatment of Overweight and Obesity in Adults. [Google Scholar]
- 18.Larson N, Neumark-Sztainer D, Story M, et al. Identifying correlates of young adults’ weight behavior: survey development. Am J Health Behav. 2011;35:712–25. [PMC free article] [PubMed] [Google Scholar]
- 19.van de Looij-Jansen PM, de Wilde EJ. Comparison of web-based versus paper-and-pencil self-administered questionnaire: effects on health indicators in Dutch adolescents. Health Serv Res. 2008;43:1708–21. doi: 10.1111/j.1475-6773.2008.00860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barlow SE, the Expert Committee Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120:S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 21.Pingitore R, Spring B, Garfield D. Gender differences in body satisfaction. Obes Res. 1997;5:402–9. doi: 10.1002/j.1550-8528.1997.tb00662.x. [DOI] [PubMed] [Google Scholar]
- 22.Kandel DB, Davies M. Epidemiology of depressive mood in adolescents: an empirical study. Arch Gen Psychiatry. 1982;39:1205–12. doi: 10.1001/archpsyc.1982.04290100065011. [DOI] [PubMed] [Google Scholar]
- 23.Feskanich D, Rimm EB, Giovannucci EL, et al. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc. 1993;93:790–6. doi: 10.1016/0002-8223(93)91754-e. [DOI] [PubMed] [Google Scholar]
- 24.Rockett HR, Wolf AM, Colditz GA. Development and reproducibility of a food frequency questionnaire to assess diets of older children and adolescents. J Am Diet Assoc. 1995;95:336–40. doi: 10.1016/S0002-8223(95)00086-0. [DOI] [PubMed] [Google Scholar]
- 25.Larson N, Harnack L, Neumark-Sztainer D. Assessing dietary intake during the transition to adulthood: a comparison of age-appropriate FFQ for youth/adolescents and adults. Public Health Nutr. 2012;15:627–34. doi: 10.1017/S136898001100228X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10:141–6. [PubMed] [Google Scholar]
- 27.Sirard JR, Hannan PJ, Cutler GJ, et al. Evaluation of two self-report measures of physical activity with accelerometry in young adults. J Phys Act Health. 2013;10:85–96. doi: 10.1123/jpah.10.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153:409–18. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 29.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 30.Neumark-Sztainer D, Wall M, Eisenberg ME, et al. Overweight status and weight control behaviors in adolescents: longitudinal and secular trends from 1999 to 2004. Prev Med. 2006;43:52–9. doi: 10.1016/j.ypmed.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 31.Nevill AM, Winter EM, Ingham S, et al. Adjusting athletes’ body mass index to better reflect adiposity in epidemiological research. J Sports Sci. 2010;28:1009–16. doi: 10.1080/02640414.2010.487071. [DOI] [PubMed] [Google Scholar]
- 32.Caspersen CJ, Pereira MA, Curran KM. Changes in physical activity patterns in the United States, by sex and cross-sectional age. Med Sci Sports Exerc. 2000;32:1601–9. doi: 10.1097/00005768-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 33.Epstein LH, Gordy CC, Raynor HA, et al. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obes Res. 2001;9:171–8. doi: 10.1038/oby.2001.18. [DOI] [PubMed] [Google Scholar]
- 34.Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study: 15-year prospective analysis. Lancet. 2005;365:36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 35.Mitchell JA, Rodriguez D, Schmitz KH, et al. Greater screen time is associated with adolescent obesity: a longitudinal study of the BMI distribution from ages 14 to 18. Obesity. 2013;21:572–5. doi: 10.1002/oby.20157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hrabosky JI, Masheb RM, White MA, et al. A prospective study of body dissatisfaction and concerns in extremely obese gastric bypass patients: 6- and 12-month postoperative outcomes. Obes Surg. 2006;16:1615–21. doi: 10.1381/096089206779319527. [DOI] [PubMed] [Google Scholar]
- 37.van den Berg P, Neumark-Sztainer D. Fat ’n happy 5 years later: is it bad for overweight girls to like their bodies? J Adolesc Health. 2007;41:415–7. doi: 10.1016/j.jadohealth.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 38.Kevin J, Heinberg LJ, Altabe M, et al. Exacting beauty: Theory, assessment, and treatment of body image disturbance. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- 39.van den Berg PA, Mond J, Eisenberg M, et al. The link between body dissatisfaction and self-esteem in adolescents: Similarities across gender, age, weight status, race/ethnicity, and socioeconomic status. J Adolesc Health. 2010;47:290–6. doi: 10.1016/j.jadohealth.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brisbois TD, Farmer AP, McCargar LJ. Early markers of adult obesity: a review. Obes Rev. 2012;13:347–67. doi: 10.1111/j.1467-789X.2011.00965.x. [DOI] [PMC free article] [PubMed] [Google Scholar]