Abstract
IN BRIEF Several guidelines and position statements are published to help clinicians manage hypertension in patients with diabetes. Although there is an unequivocal call to treat hypertension in diabetes, professional organizations and experts have differing opinions regarding the most optimal blood pressure targets and treatments to lower vascular risks in the diabetes population. The objective of this article is to summarize the most recent hypertension management guidelines with particular attention to the origins and evidence behind these recommendations.
The importance of diabetes management in the primary care setting cannot be overstated. As of 2015, diabetes affects ∼30.3 million Americans, or about 9.4% of the population (1). Worldwide, the number is estimated to be a staggering 422 million adults, and if the incidence continues to rise at its current pace, the number of people with diabetes is projected to reach 592 million by 2035 (2).
Diabetes is a well-documented risk factor for cardiovascular disease (CVD). According to recent statistics from the American Heart Association (AHA), at least 68% of patients who are ≥65 years of age who have diabetes will die from some form of heart disease, and 16% will die from stroke. Adults with diabetes are two to four times more likely to die from heart disease than those who do not have diabetes. Diabetes can also result in microvascular complications such as retinopathy, neuropathy, and nephropathy, which are the leading causes of blindness, nontraumatic foot amputation, and end-stage renal disease, respectively.
Hypertension is a common co-morbidity in patients with type 2 diabetes. The prevalence of hypertension is higher in patients with diabetes than in the general population. Current estimates are that ∼74% of adult patients with diabetes have a systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg or are on prescription medication for high blood pressure (1). The coexistence of hypertension and diabetes increases the incidences of CVD and mortality and augments the risks of nephro-pathy and retinopathy (3–5).
Given the frequency of the coexistence of diabetes and hypertension in patients and the significant impact both have on cardiovascular risk, management of hypertension is of utmost importance in people with diabetes. For this reason, several professional societies and groups of experts in the field in recent years have published recommendations for the management of hypertension in people with diabetes. In this article, we briefly describe the most current recommendations for blood pressure goals and initial therapy options from key organizations involved in the care of patients with diabetes.
Current Recommendations: Blood Pressure Goals
Many, but not all, guidelines, as described in more detail below, advocate treating hypertension in people with diabetes to a blood pressure goal <130/80 mmHg. These recommendations are mostly based on data from meta-analyses, observational studies, and studies that did not set out to treat diabetic hypertension to a certain blood pressure goal. Although these data have collectively shown better CVD and mortality outcomes with blood pressure controlled to <130/80 mmHg, there have been no randomized, controlled trials (RCTs) testing this goal versus higher blood pressure targets in people with diabetes.
Thus, there is insufficient evidence to determine the blood pressure cut-point at which the benefits offered by antihypertensive therapy outweigh the related risks. There is a need for caution regarding the widespread adoption of the lower blood pressure goals supported by the Action to Control Cardiovascular Risk in Diabetes–Blood Pressure (ACCORD BP) trial. That trial, which compared the effects of SBP-lowering of 120 versus 140 mmHg, found no difference in primary outcomes between groups, whereas those in the group with the lower SBP goal had an increased incidence of adverse events (6). Until more is known about the risk-benefit ratio of achieving blood pressure goals <130/80 mmHg, and considering some limitations to the application of clinical trial data in daily practice (discussed in more detail below), we suggest following recommendations that are based on the outcomes of prospective, interventional treat-to-target RCTs.
The American Diabetes Association (ADA) defines hypertension as SBP ≥140 mmHg and DBP ≥90 mmHg that is confirmed during separate clinic visits (7). Current ADA guidelines recommend a treatment goal of SBP <140 mmHg and DBP <90 mmHg for most patients with diabetes (Table 1). Those at higher cardiovascular risk may require more intensive blood pressure control to <130/80 mmHg. The 2018 ADA recommendations are based on the ACCORD BP trial that compared CVD outcomes in diabetes patients randomized to intensive versus less intensive blood pressure control (6). The ACCORD BP trial showed no benefit to the primary composite end point of nonfatal myocardial infarction, nonfatal stroke, and CVD death in the group treated to the more intensive blood pressure goal of SBP <120 mmHg compared to the standard group for whom SBP was maintained at <140 mmHg, while demonstrating an increased incidence of adverse effects (hypotension and worsening renal function) in the more intensively treated group.
TABLE 1.
Summary of Blood Pressure Goals and Initial Choice of Antihypertensive Agent for Patients With Diabetes Endorsed by Different Professional Societies or Expert Groups
| Recommendation (Year) | Blood Pressure Goals (mmHg) | First-Line Pharmacological Treatment |
|---|---|---|
| ADA (2018) | <140/90 (<130/80*) | ACEI/ARB†, thiazide-like diuretic, or dihydropyridine CCB |
| ACC/AHA (2017) | <130/80 | No preference |
| JNC 8 (2014) | <140/90 | Non-black: ACEI/ARB, thiazide-like diuretic, or CCB Black: thiazide-like diuretic or CCB |
| VA/DoD (2014) | <150/85 (140/85**) | Thiazide-like diuretic (chlorthalidone or indapamide) |
| CDA (2013) | <130/80 | ACEI/ARB‡, thiazide-like diuretic, or dihydropyridine CCB |
| ESH/ESC (2013) | <140/85 | ACEI/ARB†, thiazide-like diuretic, or CCB |
May be appropriate for individuals at high risk of CVD.
Suggested for patients who can tolerate the antihypertensive medications necessary to reach this goal.
Recommended if hypertension is associated with proteinuria and suggested if hypertension is associated with microalbuminuria as the preferred first-line agent.
Recommended in the presence of known kidney disease, including microalbuminuria, or CVD.
The AHA, American College of Cardiology (ACC), and multiple other professional societies released joint guidelines for the management of hypertension in 2017 (8). These guidelines recommend initiating antihypertensive therapy for patients with diabetes at a blood pressure ≥130/80 mmHg with a goal blood pressure <130/80 mmHg. Although the ACC/AHA guidelines also use data from the ACCORD BP trial to support this recommendation, the lower blood pressure goal of <130/80 mmHg for all patients with diabetes is based on the assumption that patients with diabetes have a high cardiovascular risk and on the results of two meta-analyses that showed better cardiovascular and microvascular risk reduction if SBP is maintained at <130 mmHg (9,10).
The eighth Joint National Committee (JNC 8) recommendations have been a major guide to patient management in the primary care setting since they were released in 2014 (11). They recommend initiating treatment for hypertension in patients with diabetes whose blood pressure is >140/90 mmHg with a treatment goal of SBP <140 mmHg and DBP <90 mmHg. The SBP goal is based on the ACCORD BP trial similar to other current guidelines, as well as other trials that included patients with diabetes such as the Systolic Hypertension in the Elderly Program (SHEP) and Systolic Hypertension in Europe (Syst-Eur) trials (12,13). The choice of a DBP target <90 mmHg was based on four RCTs conducted between 1970 and 2008 that demonstrated a reduction in cerebrovascular morbidity and mortality and a decrease in heart failure incidence in patients who achieved a DBP <90 mmHg.
The U.S. Department of Veterans Affairs (VA) and Department of Defense (DoD) also released hypertension guidelines for primary care providers in 2014 (14). Based on these recommendations, the therapeutic goal for patients with diabetes of all ages is <150/85 mmHg. This guideline also suggests that some patients with diabetes who can tolerate more intensive antihypertensive therapy should be treated to a goal blood pressure of <140/85 mmHg. The standard SBP goal for patients with diabetes of <150 mmHg from the VA/DoD guidelines is based on data from the SHEP, Syst-Eur trial, and UK Prospective Diabetes Study (UKPDS) (12,13,15). The tighter SBP goal of <140 mmHg was labeled a weak recommendation compared to the strong recommendation of <150 mmHg because there have been no prospective, interventional trials in patients with diabetes testing the efficacy of targeting an SBP of <140 mmHg compared to <150 mmHg. The DBP goal of <85 mmHg is based on the outcomes of the Hypertension Optimal Treatment (HOT) trial (16) and UKPDS (15).
The Canadian Diabetes Association (CDA) released guidelines for the management of hypertension in patients with diabetes in 2013 (17). These guidelines recommend an SBP goal of <130 mmHg and a DBP goal of <80 mmHg. The major determinate for the SBP goal cited by the guidelines is the ACCORD BP trial, although the CDA also relied on data from the HOT trial and several meta-analyses.
The European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) also released a joint statement on the management of hypertension in patients with diabetes (18). They recommend achieving a blood pressure goal of <140/85 mmHg in patients with diabetes. The SBP goal is based mainly on results of the ACCORD BP trial.
Initial Hypertension Therapy in Patients With Diabetes
Although lifestyle changes, including dietary modifications, weight reduction, increased physical activity, reduction in salt intake, tobacco cessation, and appropriate sleep hygiene, are known to improve metabolic health and reduce blood pressure, pharmacological interventions are frequently required to achieve optimal blood pressure goals in patients with diabetes. According to the ADA recommendations, first-line therapy should include a drug class with demonstrated cardiovascular benefits such as a renin-angiotensin system (RAS) inhibitor (angiotensin-converting enzyme inhibitor [ACEI] or angiotensin receptor blocker [ARB]), thiazide-like diuretic, or dihydropyridine calcium channel blocker (CCB) (6,19) (Table 1). There is no compelling evidence in favor of one drug class over another except for data supporting early use of RAS inhibitors in patients with overt proteinuria (urine albumin-to-creatinine ratio >300 mg/g). The ACC/AHA experts emphasize that blood pressure reduction is the main approach to reducing cardiovascular risk in hypertensive patients without stating a preference regarding which antihypertensive agent should be first initiated (8). Based on the recommendations of the panel members appointed to the JNC 8, non-black patients with diabetes should experience equal therapeutic benefits regardless of whether an ACEI/ARB, CCB, or thiazide-like diuretic is initiated for hypertension treatment, whereas, for black patients with diabetes, initial antihypertensive treatment should be a thiazide-like diuretic or a CCB (11).
Thiazide-like diuretics are recommended as a first-line therapy of hypertension in the general hypertensive population, including patients with diabetes, by the VA/DoD hypertension clinical practice guideline for primary care providers (14). The authors of this guideline suggest choosing chlorthalidone or indapamide over hydrochlorothiazide.
The CDA guidelines suggest that an ACEI or an ARB should be recommended as initial therapy for people with CVD or kidney disease, including those with microalbuminuria, and for those with cardiovascular risk factors (17). For individuals with diabetes and hypertension not included in the above recommendation, ACEIs/ARBs, dihydropyridine CCBs, or thiazide/thiazide-like di-uretics are deemed equally effective in blood pressure management.
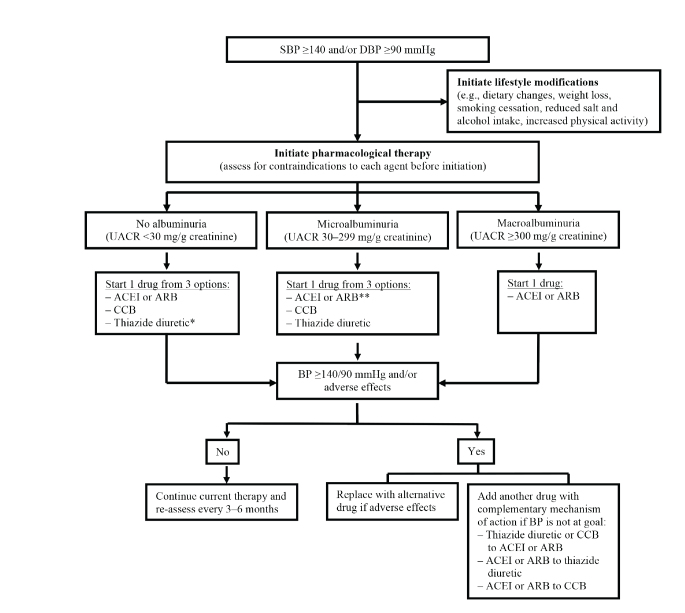
Finally, the ESH/ESC recommendations emphasize that all classes of antihypertensive agents are recommended and can be used in patients with diabetes with the caveat that RAS blockers may be preferred in the presence of proteinuria or microalbuminuria (18). Figure 1 summarizes recommendations by professional societies on initiation of an optimal antihypertensive regimen in patients with diabetes.
FIGURE 1.
Pathway to initial antihypertensive therapy in patients with diabetes. *Use of chlorthalidone or indapamide is preferred. **Can be suggested as first-line therapy in patients with microalbuminuria. BP, blood pressure; UACR, urine albumin-to-creatinine ratio.
Little is known regarding whether there are any additional benefits from the initial use of more intensive antihypertensive protocols in patients with diabetes. An ADA position statement recommends beginning monotherapy if a patient’s initial blood pressure is between 140/90 and 159/99 mmHg (19). For patients with a blood pressure ≥160/100 mmHg, these experts advocate an initial pharmacological regimen containing two antihypertensive medications (19). These recommendations are based on the results of two randomized studies of 3–6 months’ duration demonstrating that a greater proportion of participants with a baseline SBP >160 mmHg were able to achieve target blood pressure control when initially treated with two blood pressure–lowering medications (20,21). The long-term implications of these short-term studies are unknown. Hypertension is a chronic disease, and it is unclear whether rapid blood pressure reduction is of immediate benefit in patients with diabetes and particularly in those who are elderly, have multiple comorbidities including kidney disease, have polypharmacy, or are at risk for orthostatic hypotension. We suggest that providers use clinical judgment before selecting the intensity of initial antihypertensive therapy in the diabetes population.
Discussion
Current professional guidelines and recommendations for the management of hypertension in patients with diabetes are based on data available from only a few RCTs in patients with type 2 diabetes. Historically, the clinical benefits of DBP control were the first tested in the diabetes population.
In this regard, the strongest evidence was provided by the UKPDS (22). Patients with a mean blood pressure of 160/94 mmHg at baseline were randomized to tight versus less tight blood pressure control (target blood pressure <150/85 vs. <180/105 mmHg). Tight control was associated with reduced risks of important outcomes, including death due to diabetes or stroke. Although this was not a direct comparison of a target DBP of ≥85 mmHg versus a lower goal, the achieved blood pressure was 144/82 mmHg in the tight control group versus an achieved blood pressure of 154/87 mmHg in the group with less tight control.
In the HOT trial, patients with a DBP between 100 and 115 mmHg were randomized to a target DBP of ≤90, ≤85, or ≤80 mmHg (16).Achieved DBPs were 85.2, 83.2, and 81.1 mmHg, respectively. Among patients with diabetes, intensive treatment was associated with significant declines in major cardiovascular events. The relatively small diabetes sub-sample and the fact that the analysis of patients with diabetes was not pre-specified limit the strength of this evidence.
Whereas these large studies recruited patients with type 2 diabetes, it is unclear how these data can be generalized to the population with type 1 diabetes. Additionally, contemporary interpretations of the clinical effects of the lower DBP goals can be somewhat limited because the UKPDS and HOT trial enrolled patients with diabetes based on fasting blood glucose levels >140 mg/dL, making application of the results less certain for patients with milder forms of diabetes using modern diagnostic criteria.
In subsequent years, clinical interest shifted toward the testing of SBP targets in patients with diabetes. So far, the ACCORD BP trial is the only prospective RCT comparing clinical outcomes of different SBP targets in a population with type 2 diabetes (7). Although it is accepted from the results of this trial that a more intensive SBP goal of <120 mmHg compared to a standard approach targeting SBP <140 mmHg did not prove beneficial with regard to the primary composite end point of nonfatal MI, nonfatal stroke, or death from cardiovascular causes, in secondary end-point analyses, the rate of cerebrovascular outcomes was significantly lower in the intensive group. On the other hand, the more intensive group was also limited by an increased rate of adverse events such as hypotension and worsening renal function. Although this study provided assurance that an SBP goal of <140 mmHg is as effective as a goal of <120 mmHg, it may have resulted in controversy about what the ideal SBP goal should be, which has been reflected in the variation in SBP goal recommendations from different professional societies. One possible reason for this is that, although the target for the less intensive arm was <140 mmHg, the average SBP actually achieved in that group was 133 mmHg. Additionally, the trial was initially intended to assess the difference between SBP goals of <120 and <130 mmHg based on the seventh JNC guidelines, but there was concern that there would not be enough of a difference between the two values to result in statistical significance, so the less intensive goal was changed to <140 mmHg. Most guidelines have accepted that an SBP of <120 mmHg would not be beneficial, but it remains unclear whether there will be any differences between an SBP goal of <130 mmHg and one of <140 mmHg. In our opinion, patients with diabetic kidney disease may benefit the most from the lower blood pressure goals if these goals can be achieved without side effects (23), whereas for the majority of patients with diabetes, a blood pressure goal of <140/90 mmHg appears to be reasonable and based on solid evidence.
The elderly comprise a growing population of patients with multiple comorbidities, including diabetes. Previous interventional studies tended to exclude older patients with diabetes, limiting generalization of their results to this group of the patients. Not surprisingly, the majority of professional recommendations do not discuss blood pressure management in the elderly. High prevalence rates of polypharmacy, renal dysfunction, cognitive impairment, and diabetes complications including neuropathy, atherosclerotic vessel disease, and other comorbid conditions in the elderly suggest that, in the absence of outcomes research, we must use caution when providing care to these patients and to do so on an individual basis. With the uncertainty surrounding blood pressure treatment goals for elderly patients with diabetes and hypertension, the VA/DoD position statement can be viewed as a compromise to address the current evidence of benefits of certain SBP and DBP targets, the lack of prospective trials targeting an SBP of <150 mmHg in the diabetes population, and the paucity of data on clinical outcomes of blood pressure regulation in the elderly (14).
Finally, with the accumulating body of evidence demonstrating the clinical benefits of hypertension control in diabetes, more questions have arisen with regard to the applicability of these research findings to routine clinical care. The ideal scenario of blood pressure measurement undertaken in the research setting consists of an average of two out of three office blood pressure measurements taken with a proper cuff size 1 minute apart after 5 minutes of rest in a quiet area with an automated or semi-automated manometer. Subjects are seated, with back supported, and bare arm placed at the level of the right atrium. No conversation occurs during blood pressure measurements. However, this ideal scenario is impossible to achieve in the busy and often-crowded clinical setting.
Recent research clearly shows that blood pressure measurements taken without the benefit of these ideal conditions are likely to overestimate the actual blood pressure. It has been suggested by several authors that clinical practice blood pressure readings will be higher by anywhere from 10/5 to 12/12 mmHg compared with blood pressure measurements in research settings (24–26). Therefore, non-research clinical blood pressure measurements will likely lead to overtreatment and overdiagnosis, particularly if lower blood pressure targets are accepted for therapeutic considerations, as proposed by the ACC/AHA or the CDA. Taking into account the paucity of clear research data showing additional benefits of blood pressure control to <130/80 mmHg in the general diabetes population, differences in blood pressure determinations in research settings versus clinical practice, and the growing number of patients who are old and have comorbidities, it is appealing for us to accept the ADA or VA/DoD recommendations to guide providers’ decisions regarding long-term hypertension management in the diabetes population.
Conclusion
Clearly, hypertension management mitigates vascular risks in diabetes. The question, however, is how low we should go with blood pressure reduction to achieve the best therapeutic benefits without significant side effects from antihypertensive therapy. Although we are witnessing a proliferation of guidelines and recommendations suggesting optimal blood pressure targets in the diabetes population, there is little scientific evidence to support aiming at lower targets such as <130/80 mmHg. Knowing the methodological differences between blood pressure measurement in the research and clinical settings that current guidelines do not take into consideration, clinicians should approach each patient individually and attempt to offer the best of available treatment options without compromising patient safety.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Disclaimer
A.R.G. is an employee of the U.S. Department of Veterans Affairs; opinions expressed in this article are the authors’ alone and do not necessarily represent the opinion of the Department of Veterans Affairs.
Author Contributions
P.P. wrote the manuscript and researched data. T.A.K. and F.V.V. contributed to discussion and reviewed/edited the manuscript. A.R.G. researched data, contributed to discussion, and reviewed/edited the manuscript. A.R.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Centers for Disease Control and Prevention National diabetes statistics report—2017. Available from www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 23 December 17
- 2.NCD Risk Factor Collaboration Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000;321:412–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gosmanov AR, Lu JL, Sumida K, et al. Synergistic association of combined glycemic and blood pressure level with risk of complications in US veterans with diabetes. J Hypertens 2016;34:907–913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care 1993;16:434–444 [DOI] [PubMed] [Google Scholar]
- 6.ACCORD Study Group; Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Diabetes Association Cardiovascular disease and risk management. Sec. 9 in Standards of Medical Care in Diabetes—2018. Diabetes Care 2018;41(Suppl. 1):S86–S104 [DOI] [PubMed] [Google Scholar]
- 8.Whelton PK, Carey RM, Aronow WS, et al. 2017ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017;pii:S0735-1097(19)41519-1 [DOI] [PubMed] [Google Scholar]
- 9.Lv J, Ehteshami P, Sarnak MJ, et al. Effects of intensive blood pressure lowering on the progression of chronic kidney disease: a systematic review and meta-analysis. CMAJ 2013;185:949–957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet 2016;387:435–443 [DOI] [PubMed] [Google Scholar]
- 11.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–520 [DOI] [PubMed] [Google Scholar]
- 12.SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA 1991;265:3255–3264 [PubMed] [Google Scholar]
- 13.Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension: the Systolic Hypertension in Europe (Syst-Eur) trial investigators. Lancet 1997;350:757–764 [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Veterans Affairs , U.S. Department of Defense. VA/DoD clinical practice guideline for the diagnosis and management of hypertension in the primary care setting. October 2014. Available from www.healthquality.va.gov/guidelines/cd/htn. Accessed 20 December 2017
- 15.U.K. Prospective Diabetes Study Group Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ 1998;317:713–720 [PMC free article] [PubMed] [Google Scholar]
- 16.Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet 1998;351:1755–1762 [DOI] [PubMed] [Google Scholar]
- 17.Canadian Diabetes Association Clinical Practice Guidelines Expert Committee; Cheng AY. Canadian Diabetes Association 2013 clinical practice guidelines for the prevention and management of diabetes in Canada: introduction. Can J Diabetes 2013;37(Suppl. 1):S1–S3 [DOI] [PubMed] [Google Scholar]
- 18.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34:2159–2219 [DOI] [PubMed] [Google Scholar]
- 19.de Boer IH, Bangalore S, Benetos A, et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care 2017;40:1273–1284 [DOI] [PubMed] [Google Scholar]
- 20.Bakris GL, Weir MR, Study of Hypertension and the Efficacy of Lotrel in Diabetes (SHIELD) Investigators. Achieving goal blood pressure in patients with type 2 diabetes: conventional versus fixed-dose combination approaches. J Clin Hypertens (Greenwich) 2003;5:202–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feldman RD, Zou GY, Vandervoort MK, et al. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension 2009;53:646–653 [DOI] [PubMed] [Google Scholar]
- 22.U.K. Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703–713 [PMC free article] [PubMed] [Google Scholar]
- 23.Gosmanov AR, Wall BM, Gosmanova EO. Diagnosis and treatment of diabetic kidney disease. Am J Med Sci 2014;347:406–413 [DOI] [PubMed] [Google Scholar]
- 24.Agarwal R. Implications of blood pressure measurement technique for implementation of Systolic Blood Pressure Intervention Trial (SPRINT). J Am Heart Assoc 2017;6:pii:e004536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drawz PE, Ix JH. BP measurement in clinical practice: time to SPRINT to guideline-recommended protocols. J Am Soc Nephrol 2018;29:383–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Myers MG, Godwin M, Dawes M, et al. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension 2010;55:195–200 [DOI] [PubMed] [Google Scholar]