Abstract
Background
Gonorrhea (GC) and Chlamydia (CT) disproportionately affect men who have sex with men (MSM), and public health implications vary by anatomic site and bacterial agent. Urethral and rectal GC and CT can increase risk of HIV transmission, while pharyngeal GC may be a reservoir for antimicrobial resistance. To define screening priorities in Latin America, we compare differences in the prevalence and correlates of urethral, pharyngeal, and rectal GC and CT among MSM in Peru.
Methods
A cross-sectional sample of 787 MSM from Lima was screened between 2012-2014. We described prevalence of urethral, pharyngeal, and rectal GC and CT infection and conducted bivariate analyses of associations with social, behavioral, and biological characteristics. Poisson regression analyses assessed the correlates of each infection at each anatomic site.
Results
The most commonly symptomatic infection (urethral GC; 42.1%) was the least prevalent (2.4%). The most prevalent infections were rectal CT (15.8%) and pharyngeal GC (9.9%). Rectal CT was the least commonly symptomatic (2.4%) infection, and was associated with younger age (aPR, 95% CI: 0.96, 0.94-0.98), HIV infection (1.46, 1.06-2.02), and pasivo (receptive; 3.59, 1.62-7.95) and moderno (versatile; 2.63, 1.23-5.60) sexual roles.
Conclusions
Results highlight limitations of current syndromic screening strategies for STDs in Peru, wherein urethral CT and rectal GC and CT may be missed due to their frequently asymptomatic presentations. Successful management of GC and CT infections among MSM in low-resource settings requires differentiating between bacterial agent, symptomatic presentation, associated risk factors, and public health implications of untreated infection at different anatomic sites.
Keywords: Gonorrhea, Chlamydia, Screening, Resource-limited, Public health
Introduction
Neisseria gonorrhoeae (GC) and Chlamydia trachomatis (CT) are common, frequently asymptomatic, sexually transmitted diseases (STDs) among men who have sex with men (MSM) (1-5). Routine screening of the urethra, pharynx, and rectum using nucleic acid amplification testing (NAAT) has become the standard of care for MSM in the United States and Europe. In resource-limited settings, however, the cost of these assays is frequently prohibitive and syndromic management is the norm (6). To improve this approach, the WHO has called for screening algorithms guided by detailed understanding of local epidemiologic patterns and correlates of asymptomatic infection (7, 8). In heterogeneous populations like MSM, these factors may vary substantially across different anatomic sites according to social factors like sexual orientation (1). To address these issues, we explored variations in the epidemiology of urethral, pharyngeal, and rectal GC and CT infection and associated social, behavioral, and biological correlates of infection in a sample of MSM in Lima, Peru.
In managing GC and CT infection in MSM, it is important to acknowledge the potential clinical and public health implications of infections at different anatomic sites. Prevalence of urethral GC and CT infection in MSM worldwide has been estimated between 0.4-11.1% and 1.9-8.4%, respectively (4, 5, 9, 10). Urethral infections are more often symptomatic than infection at other sites, with up to 90% of patients with urethral GC and more than half of patients with urethral CT presenting with symptoms (4). Symptomatic disease is more likely to be recognized, diagnosed, and treated (11). Untreated urethral infections in men, however, can lead to epididymitis, reduced fertility, and urethral strictures (11). Coinfection with urethral GC or CT and HIV also triples the risk of HIV transmission during insertive intercourse through inflammation and viral shedding in the genital tract (12).
In contrast, prevalences of oropharyngeal GC and CT infection have been estimated between 0.5-16.5% and 0-3.6%, respectively, with as few as 0-8% of cases presenting with symptoms (3, 13, 14). Previous research suggests undiagnosed pharyngeal gonorrhea may be a source of antimicrobial drug resistance via horizontal gene transfer events with other Neisseria species colonizing the throat (13, 15). Resistant bacterial strains could potentially be transmitted to sexual partners via kissing, oro-genital, or oro-anal sex (16). Accordingly, pharyngeal GC may play an important role in the development, maintenance, and circulation of antimicrobial resistance throughout MSM sexual networks.
Prevalence of rectal GC and CT infection in MSM has been reported between 0.2-24% and 2.1-23%, respectively, with more than three-quarters of GC and CT cases presenting asymptomatically (3, 4, 9, 17). Notably, rectal GC has been associated with a 2- to 17-fold increase, and rectal CT with a 2.9-fold increase, in the risk of HIV acquisition (18). The biological mechanism of this increased vulnerability to HIV is likely due to rectal mucosal inflammation and recruitment of CD4+ T-cells to lymphoid tissue (19). The increased risk for HIV acquisition seen in cases of rectal GC and CT can also be explained by behavioral and network factors that increase risk of exposure to HIV and GC/CT, like condomless receptive anal intercourse (cRAI) and contact with high HIV/STD prevalence sexual networks (20). Accordingly, routine testing for rectal GC and CT is a potential cornerstone intervention for reducing HIV acquisition among MSM (20).
Despite the diversity of risk factors, symptom presentations, and public health implications of different kinds of GC and CT infection, current STD management strategies in Peru are based on syndromic management without use of NAAT screening (21). A detailed understanding of factors associated with GC and CT infection at different anatomic sites is critical for targeting limited testing resources to the areas of greatest need. Our study describes prevalence and explores correlates of GC and CT infection at three anatomic sites in a sample of MSM in Peru. Our approach considers each site as a potential correlate of multi-site infection at another location, highlights variations and similarities in correlates of infection at different anatomic sites, and identifies potential public health implications of diagnosis and treatment of GC and CT infection at each site.
Materials and Methods
Participants and Recruitment
Participants were identified during the screening process of a study of sexual partner management following GC and/or CT infection (22). Research staff recruited participants at STD clinics and venues frequented by MSM in Lima and Callao, Peru between August, 2012 and June, 2014. Enrollment was limited to individuals who: 1) were at least 18 years old, 2) were assigned male sex at birth, and 3) reported oral and/or anal sex with a male or male-to-female transgender partner in the preceding year.
Study Procedures
All participants completed a computer-assisted self-interview (CASI) behavioral survey. The survey assessed sexual orientation (heterosexual, bisexual, homosexual) and role (activo [insertive], pasivo [receptive], moderno [versatile]), partner-specific sexual acts (anal, vaginal, oral intercourse) with the three most recent sexual partners, position during intercourse (insertive, receptive, both), and condom use.
Physicians performed a medical history and physical exam for signs of STDs, and collected urine samples and rectal and pharyngeal swabs. Only participants with NAAT results from all three anatomic sites were included in this analysis. All specimens were tested for GC and CT infection using the Gen-Probe Aptima II assay (Hologic, San Diego, CA, USA) at the U.S. Naval Medical Research Unit-6 Bacteriology Laboratory in Callao. HIV testing was offered to participants, but not required as a condition of enrollment (22). Participants were compensated 15 Nuevos soles (approximately US$5.00) and provided with five condoms and sachets of lubricant at each visit.
Participants with clinically symptomatic urethritis or proctitis were treated with Ceftriaxone 250 mg IM once and Azithromycin 1g PO once at initial evaluation, according to CDC Guidelines (23). All participants were provided with results of NAAT testing within two weeks and treated with Ceftriaxone and Azithromycin for asymptomatic GC or Azithromycin alone for asymptomatic CT infection.
Consent/Permissions
The IRBs of University of California, Los Angeles, Asociación Civil Impacta Salud y Educación, and NAMRU-6 reviewed and approved all study procedures. Written informed consent was obtained from all participants prior to participation.
Data Analysis
Bivariate analyses with chi-squared and Fisher's exact tests, when appropriate, were used to estimate the association of participant characteristics with GC or CT at the three anatomic sites. Wilcoxon's Rank Sum test was used to measure differences in the distribution of non-parametric numeric variables between participants with and without infection at each site.
Variables were selected for inclusion in multivariate regression models based on conceptual reasoning. To measure associations between independent variables and outcomes, we computed prevalence ratios with Poisson regression using robust estimation of standard errors (24-26). All analyses were conducted using Stata 12.0 (StataCorp, College Town, TX). Pairwise deletion was performed for variables with missing data; less than 5% of data were missing for any single variable.
Results
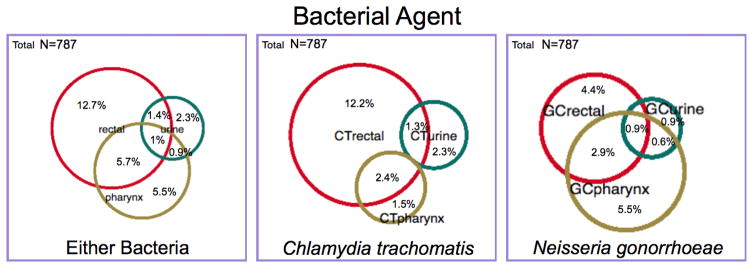
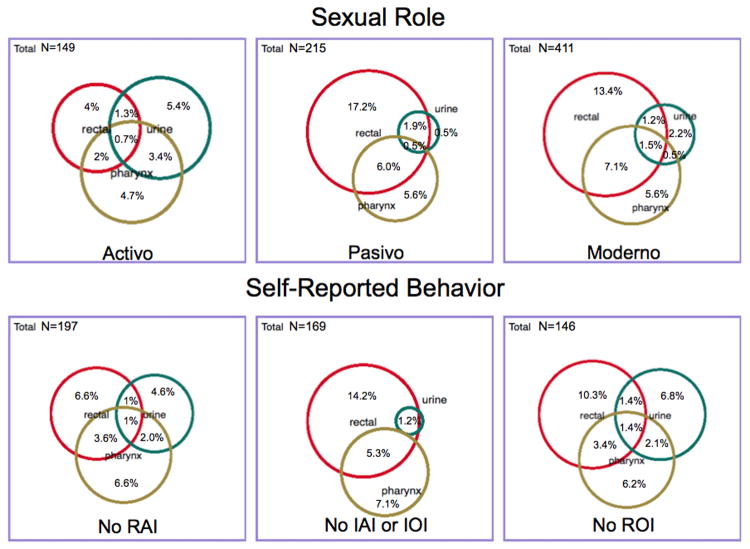
The age range of participants was 18 to 65 years. GC and/or CT infection at any anatomic site was identified in 29.5% of the sample. Prevalence of gonoccocal infection (15.3%) was lower than chlamydial infection (19.7%). Single-site infection with GC and/or CT was diagnosed in 20.5% of participants, while multi-focal infection was identified in 9.0%, most frequently as simultaneous infection in the rectum and oropharynx (63.4%; 45/71). Only 2.4% of all participants manifested clinical signs of urethritis or proctitis. Figures 1 and 2 show patterns of infection based on bacterial agent and sexual role and behavior with the last three partners.
Figure 1. Prevalence of urethral, pharyngeal, and rectal infections by bacterial agent.
Figure 2. Prevalence of urethral, pharyngeal, and rectal infections by sexual role, and self-reported sexual behavior.
LEGEND (for Figures 1 and 2): The square figure for each Venn diagram represents the sub-population presented therein (denominator for the percentages presented). The relative size of the circles in relation to each other represents the proportion of that population that tested positive for infection at the specified site (numerator for the percentages presented). The percentages presented in the figures are discreet and define only the site(s) of infection they represent. For example, for the “Either Bacteria” sub-population in Figure 1, the “Rectal” percentage equals 12.7%, indicating that 12.7% of participants had infection at the rectal site only, not including those participants with infection of the rectum and another anatomic site. IAI, insertive anal intercourse; IOI, insertive oral intercourse; RAI, receptive anal intercourse; ROI, receptive oral intercourse.
There were fifteen new HIV diagnoses (4.0%) among 378 participants who requested HIV testing and reported no prior HIV diagnosis. Two of these participants (13.3%) were diagnosed with only pharyngeal GC, and one (6.7%) was diagnosed with pharyngeal GC and rectal CT. Overall, 53.9% of participants were HIV-infected (previous or newly diagnosed infection). Prevalences of GC and CT at any site in this subgroup were 16.4% and 21.8%, respectively, compared to 14.0% and 17.5% in participants who were HIV-uninfected or reported an unknown HIV status (Table 1).
Table 1. Characteristics and bivariate associations of Neisseria gonorrhoeae (GC) and Chlamydia trachomatis (CT) in urethral, pharyngeal, and rectal infection among MSM in Lima (N=787).
| Urethra | Pharynx | Rectum | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neisseria gonorrhea | Chlamydia trachomatis | Neisseria gonorrhea | Chlamydia trachomatis | Neisseria gonorrhea | Chlamydia trachomatis | ||||||||
| Characteristic | Total | + | - | + | - | + | - | + | - | + | - | + | - |
| Age | 787 (100) | 23 (21, 21) | 27 (23, 33) | 26 (22.5, 31.5) | 27 (23, 33) | 26 (21, 21) | 28 (23, 33) | 25 (23, 32) | 27 (23, 33) | 24 (21, 21) | 28 (23, 33) | 25 (22, 22) | 28 (23, 34) |
| HIV Status | |||||||||||||
| Positive | 424 (53.9) | 12 (2.8) | 412 (97.2) | 10 (2.4) | 414 (97.6) | 42 (9.9) | 382 (90.1) | 18 (4.3) | 406 (95.7) | 42 (9.9) | 382 (90.1) | 79 (18.6) | 345 (81.4) |
| Negative | 363 (46.1) | 7 (1.9) | 356 (98.1) | 18 (5) | 345 (95) | 36 (9.9) | 327 (90.1) | 13 (3.6) | 350 (96.4) | 23 (6.3) | 340 (93.7) | 46 (12.7) | 317 (87.3) |
| Sexual orientation | |||||||||||||
| Heterosexual | 24 (3.05) | 3 (12.5) | 21 (87.5) | 0 (0) | 24 (100) | 2 (8.3) | 22 (91.7) | 0 (0) | 24 (100) | 1 (4.2) | 23 (95.8) | 2 (8.3) | 22 (91.7) |
| Bisexual | 207 (26.3) | 5 (2.4) | 202 (97.6) | 14 (6.8) | 193 (93.2) | 22 (10.6) | 185 (89.4) | 8 (3.9) | 199 (96.1) | 13 (6.3) | 194 (93.7) | 31 (15) | 176 (85) |
| Homosexual | 532 (67.6) | 11 (2.1) | 521 (97.9) | 13 (2.4) | 519 (97.6) | 52 (9.8) | 480 (90.2) | 23 (4.3) | 509 (95.7) | 49 (9.2) | 483 (90.8) | 88 (16.5) | 444 (83.5) |
| Other/Unsure | 24 (3.05) | 0 (0) | 24 (100) | 1 (4.2) | 23 (95.8) | 2 (8.3) | 22 (91.7) | 0 (0) | 24 (100) | 2 (8.3) | 22 (91.7) | 4 (16.7) | 20 (83.3) |
| Sexual role | |||||||||||||
| Activo | 149 (18.9) | 6 (4) | 143 (96) | 12 (8.1) | 137 (91.9) | 14 (9.4) | 135 (90.6) | 2 (1.3) | 147 (98.7) | 5 (3.4) | 144 (96.6) | 9 (6) | 140 (94) |
| Pasivo | 215 (27.3) | 2 (0.9) | 213 (99.1) | 4 (1.9) | 211 (98.1) | 15 (7) | 200 (93) | 12 (5.6) | 203 (94.4) | 22 (10.2) | 193 (89.8) | 47 (21.9) | 168 (78.1) |
| Moderno | 411 (52.2) | 11 (2.7) | 400 (97.3) | 12 (2.9) | 399 (97.1) | 48 (11.7) | 363 (88.3) | 16 (3.9) | 395 (96.1) | 38 (9.3) | 373 (90.7) | 67 (16.3) | 344 (83.7) |
| Other/Unsure | 12 (1.5) | 0 (0) | 12 (100) | 0 (0) | 12 (100) | 1 (8.3) | 11 (91.7) | 1 (8.3) | 11 (91.7) | 0 (0) | 12 (100) | 2 (16.7) | 10 (83.3) |
| Female partners | |||||||||||||
| Any | 57 (7.2) | 0 (0) | 57 (100) | 2 (3.5) | 55 (96.5) | 2 (3.5) | 55 (96.5) | 2 (3.5) | 55 (96.5) | 3 (5.3) | 54 (94.7) | 1 (1.8) | 56 (98.2) |
| None | 730 (92.8) | 19 (2.6) | 711 (97.4) | 26 (3.6) | 704 (96.4) | 76 (10.4) | 654 (89.6) | 29 (4) | 701 (96) | 62 (8.5) | 668 (91.5) | 124 (17) | 606 (83) |
| Sexual behaviors with last 3 partners | |||||||||||||
| ROI | 641 (81.5) | 11 (1.7) | 630 (98.3) | 18 (2.8) | 623 (97.2) | 63 (9.8) | 578 (90.2) | 26 (4.1) | 615 (95.9) | 52 (8.1) | 589 (91.9) | 108 (16.9) | 533 (83.1) |
| No ROI | 146 (18.5) | 8 (5.5) | 138 (94.5) | 10 (6.9) | 136 (93.1) | 15 (10.3) | 131 (89.7) | 5 (3.4) | 141 (96.6) | 13 (8.9) | 133 (91.1) | 17 (11.6) | 129 (88.4) |
| IAI | 534 (67.9) | 18 (3.4) | 516 (96.6) | 24 (4.5) | 510 (95.5) | 55 (10.3) | 479 (89.7) | 15 (2.8) | 519 (97.2) | 37 (6.9) | 497 (93.1) | 74 (13.9) | 460 (86.1) |
| No IAI | 253 (32.1) | 1 (0.4) | 252 (99.6) | 4 (1.6) | 249 (98.4) | 23 (9.1) | 230 (90.9) | 16 (6.3) | 237 (93.7) | 28 (11.1) | 225 (88.9) | 51 (20.2) | 202 (79.8) |
| RAI | 590 (75) | 11 (1.9) | 579 (98.1) | 17 (2.9) | 573 (97.1) | 57 (9.7) | 533 (90.3) | 25 (4.2) | 565 (95.8) | 52 (8.8) | 538 (91.2) | 109 (18.5) | 481 (81.5) |
| No RAI | 197 (25) | 8 (4.1) | 189 (95.9) | 11 (5.6) | 186 (94.4) | 21 (10.7) | 176 (89.3) | 6 (3.1) | 191 (96.9) | 13 (6.6) | 184 (93.4) | 16 (8.1) | 181 (91.9) |
| Any urethral infection | |||||||||||||
| Positive | 44 (5.6) | 15 (34.1) | 29 (65.9) | 1 (2.3) | 43 (97.7) | 9 (20.5) | 35 (79.5) | 13 (29.6) | 31 (70.4) | ||||
| Negative | 743 (94.4) | 63 (8.5) | 680 (91.5) | 30 (4) | 713 (96) | 56 (7.5) | 687 (92.5) | 112 (15.1) | 631 (84.9) | ||||
| Any pharyngeal infection | |||||||||||||
| Positive | 103 (13.1) | 12 (11.7) | 91 (88.3) | 4 (3.9) | 99 (96.1) | 35 (34) | 68 (66) | 31 (30.1) | 72 (69.9) | ||||
| Negative | 684 (86.9) | 7 (1) | 677 (99) | 24 (3.5) | 660 (96.5) | 30 (4.4) | 654 (95.6) | 94 (13.7) | 590 (86.3) | ||||
| Any rectal infection | |||||||||||||
| Positive | 164 (20.8) | 9 (5.5) | 155 (94.5) | 10 (6.1) | 154 (93.9) | 37 (22.6) | 127 (77.4) | 20 (12.2) | 144 (87.8) | ||||
| Negative | 623 (79.2) | 10 (1.6) | 613 (98.4) | 18 (2.9) | 605 (97.1) | 41 (6.6) | 582 (93.4) | 11 (1.8) | 612 (98.2) | ||||
Bold text = p-value <0.05.
IAI, insertive anal intercourse; IOI, insertive oral intercourse; RAI, receptive anal intercourse; ROI, receptive oral intercourse
Urethral Infection
Of the 2.4% of participants with urethral GC, 42.1% (8/19) had clinical signs of urethritis. While 26.3% (5/19) had urethral infection only, the pharynx was the most frequent location (63.2%) of multi-site infection. Urethral GC was more common among participants who identified as heterosexual (12.5%) compared to bi- or homosexual (2.4% and 2.1%, respectively; p=0.011). These results corresponded with differences in reported frequency of insertive anal intercourse (IAI), as 61.7% of homosexual participants reported IAI with one or more recent sexual partners compared to 95.8% of heterosexual MSM (p<0.001).
Of the 3.6% of participants with urethral CT, 14.3% (4/28) had clinical signs of urethritis. While 53.6% (15/28) had urethral infection only, the rectum was the most frequent location (35.7%) of multi-site infection. No heterosexual participants had urethral CT. Activo MSM had a higher prevalence of chlamydial urethritis compared to moderno or pasivo participants (8.1% vs. 2.9% vs. 1.9%; p=0.017). These results corresponded with differences in reported frequency of IAI: 25.1% of pasivo participants reported IAI with one or more recent sexual partners compared to 95.3% of activo MSM (p<0.001).
Pharyngeal Infection
Prevalence of pharyngeal GC was 9.9%. While GC was limited to the oropharynx in 43.6% (34/78) of participants, the rectum was the most frequent location (47.4%) of multi-site infection. The prevalence of pharyngeal GC was similar across all sexual orientations (8.3% heterosexual; 10.6% bisexual; 9.8% homosexual) and roles (9.4% activo; 7.0% pasivo; 11.7% moderno). Out of the 146 MSM reporting no receptive oral intercourse (ROI) in their last three sexual encounters, 10.3% had pharyngeal GC, similar to the 9.8% prevalence of in those who did endorse ROI.
Prevalence of pharyngeal CT was 3.9%, and was limited to the oropharynx in 32.3% (10/31) of participants. The rectum was the most frequent location (64.5%) of multi-site infection. Zero heterosexual participants and only 1.3% (2/149) of activo men had pharyngeal CT. Out of the 146 MSM reporting no ROI in their last three sexual encounters, 3.4% had pharyngeal CT, similar to the 4.1% prevalence in those who did endorse ROI.
Rectal Infection
The rectum was the most common site of infection (20.8%) and the most common site for GC and CT co-infection in our sample. Clinical signs of rectal GC were uncommon (4.6%; 3/65), and infection was isolated to the rectum in 43.1% (28/65) of cases. Prevalence of rectal GC in participants who did not endorse RAI with any of their last three partners (6.6%) was similar to that of those endorsing RAI (8.8%).
Clinical signs of rectal CT were also uncommon (2.4%; 3/125), and infection was isolated to the rectum in 66.4% (83/125) of cases. HIV infection was associated with rectal chlamydia (18.6% vs. 12.7% of HIV-uninfected; p=0.023). MSM who identified as pasivo or moderno had a higher prevalence of rectal CT than activo men (21.9% vs. 16.3% vs. 6.0%; p=0.001). Notably, only 23.5% of activo men reported one or more episodes of RAI during their last three partnerships, compared with 84.9% of moderno and 93.5% of pasivo men (p<0.001). Prevalence of rectal CT was 8.1% in participants who did not endorse RAI with any of their last three partners compared to 18.5% of those endorsing RAI (p=0.001).
Poisson Regression of Social, Behavioral, and Biological Factors
After adjusting for age, HIV serostatus, sexual role and behavior, and other sites of GC infection, men who identified as bisexual had a lower prevalence of urethral GC (aPR, 95% CI: 0.18, 0.06-0.58) compared to men who identified as heterosexual (Table 2). Rectal GC was associated with younger age (0.95, 0.92-0.99) and a pasivo sexual role (3.23, 1.19-8.79). GC infection of the oropharynx, the most common site of GC in our sample, was associated with urethral (3.57, 2.20-5.79) and rectal GC (5.75, 3.71-8.92).
Table 2. Crude and adjusted Poisson regression models for gonoccocal infection of the urethra, pharynx, and rectum.
| Characteristic or behavior | URETHRA (N=19) | PHARYNX (N=78) | RECTUM (N=65) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PR | (95% CI) | aPR* | (95% CI) | PR | (95% CI) | aPR* | (95% CI) | PR | (95% CI) | aPR* | (95% CI) | |||
| Age | 0.92 | (0.84, 1.00) | 0.95 | (0.88, 1.03) | 0.96 | (0.93, 0.99) | 0.98 | (0.95, 1.00) | 0.95 | (0.91, 0.98) | 0.95 | (0.92, 0.99) | ||
| HIV infection | ||||||||||||||
| Negative | Ref | Ref | Ref | Ref | Ref | |||||||||
| Positive | 1.47 | (0.58, 3.69) | 2.13 | (0.78, 5.81) | 1.00 | (0.65, 1.52) | 0.86 | (0.58, 1.27) | 1.56 | (0.96, 2.55) | 1.50 | (0.94, 2.41) | ||
| Sexual orientation | ||||||||||||||
| Heterosexual | Ref | Ref | Ref | Ref | Ref | |||||||||
| Bisexual | 0.19 | (0.05, 0.76) | 0.18 | (0.06-0.58) | 1.28 | (0.32, 5.10) | 2.04 | (0.82, 5.10) | 1.51 | (0.21, 11.04) | 1.29 | (0.32, 5.21) | ||
| Homosexual | 0.17 | (0.05, 0.55) | 0.26 | (0.07, 1.02) | 1.17 | (0.30, 4.54) | 2.16 | (0.89, 5.27) | 2.21 | (0.32, 15.36) | 1.60 | (0.40, 6.48) | ||
| Other/Unknown | - | - | - | - | 1.00 | (0.15, 6.54) | 1.84 | (0.34, 9.86) | 2.00 | (0.19, 20.64) | 1.74 | (0.27, 11.34) | ||
| Sexual role | ||||||||||||||
| Activo | Ref | Ref | Ref | Ref | Ref | |||||||||
| Pasivo | 0.23 | (0.05, 1.13) | 0.52 | (0.06, 4.42) | 0.74 | (0.37, 1.49) | 0.50 | (0.25, 1.02) | 3.05 | (1.18, 7.86) | 3.23 | (1.19, 8.79) | ||
| Moderno | 0.66 | (0.25, 1.77) | 0.62 | (0.19, 2.03) | 1.24 | (0.71, 2.19) | 0.84 | (0.47, 1.51) | 2.75 | (1.10, 6.86) | 2.32 | (0.89, 6.04) | ||
| Other/unknown | - | - | 0.89 | (0.13, 6.19) | 1.22 | (0.15, 9.96) | - | - | - | - | ||||
| Sexual behavior in the last three encounters | ||||||||||||||
| No IOI | Ref | Ref | No ROI | Ref | Ref | No cRAI | Ref | Ref | ||||||
| IOI | 3.30 | (0.77, 14.17) | 1.93 | (0.29, 12.65) | ROI | 0.96 | (0.56, 1.63) | 1.13 | (0.68, 1.90) | cRAI | 1.14 | (0.71, 1.81) | 0.83 | (0.53, 1.30) |
| No cIAI | Ref | Ref | ||||||||||||
| cIAI | 3.20 | (1.23, 8.32) | 2.03 | (0.59, 6.98) | ||||||||||
| Other sites of infection | ||||||||||||||
| Urethral | - | - | - | - | 7.35 | (4.86, 11.12) | 3.57 | (2.20, 5.79) | 4.88 | (2.57, 9.24) | 1.76 | (1.02, 3.01) | ||
| Pharyngeal | 15.58 | (6.32, 38.44) | 10.32 | (3.98, 26.75) | - | - | - | - | 7.79 | (5.08, 11.96) | 6.75 | (4.29, 10.64) | ||
| Rectal | 6.48 | (2.64, 15.90) | 1.89 | (0.77, 4.60) | 6.94 | (4.75, 10.14) | 5.75 | (3.71, 8.92) | - | - | - | - | ||
Bold text = p-value <0.05.
Adjusted for: age, HIV infection, sexual orientation, sexual role, sexual behavior in the last three encounters, and other sites of infection.
cIAI, condomless insertive anal intercourse; cRAI, condomless receptive anal intercourse; IOI, insertive oral intercourse; ROI, receptive oral intercourse
After adjusting for the same characteristics described above, men who identified as moderno had a lower prevalence of urethral CT (0.35, 0.15-0.82) compared to activo men (Table 3). Rectal CT infection, the most common site of CT in our sample, was associated with younger age (0.96, 0.94-0.98), a pasivo (3.59, 1.62-7.95) or moderno (2.63, 1.23-5.60) sexual role, prevalent HIV infection (1.46, 1.06-2.02), and urethral (3.53, 2.10-5.93) and pharyngeal CT (3.91, 2.77-5.52).
Table 3. Crude and adjusted Poisson regression models for chlamydial infection of the urethra, pharynx, and rectum.
| Characteristic or behavior | URETHRA (N=28) | PHARYNX (N=31) | RECTUM (N=125) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PR | (95% CI) | aPR* | (95% CI) | PR | (95% CI) | aPR* | (95% CI) | PR | (95% CI) | aPR* | (95% CI) | |||
| Age | 0.99 | (0.95, 1.04) | 1.00 | (0.96, 1.05) | 0.98 | (0.94, 1.02) | 1.00 | (0.96, 1.04) | 0.96 | (0.93, 0.98) | 0.96 | (0.94, 0.98) | ||
| HIV infection | ||||||||||||||
| Negative | Ref | Ref | Ref | Ref | Ref | |||||||||
| Positive | 0.48 | (0.22, 1.02) | 0.51 | (0.24, 1.10) | 1.19 | (0.59, 2.39) | 0.96 | (0.49, 1.90) | 1.47 | (1.05, 2.06) | 1.46 | (1.06, 2.02) | ||
| Sexual orientation | ||||||||||||||
| Heterosexual | - | - | - | - | - | - | - | - | Ref | Ref | ||||
| Bisexual | Ref | Ref | Ref | 1.80 | (0.46, 7.05) | 0.81 | (0.20, 3.18) | |||||||
| Homosexual | 0.36 | (0.17, 0.76) | 0.58 | (0.25, 1.33) | 1.12 | (0.51, 2.46) | 0.97 | (0.48, 1.96) | 1.98 | (0.52, 7.59) | 0.73 | (0.18, 2.98) | ||
| Other/Unknown | 0.62 | (0.08, 4.49) | 1.04 | (0.16, 6.83) | - | - | - | - | 2.00 | (0.40, 9.92) | 1.11 | (0.24, 5.13) | ||
| Sexual role | ||||||||||||||
| Activo | Ref | Ref | Ref | Ref | Ref | |||||||||
| Pasivo | 0.23 | (0.08, 0.70) | 0.26 | (0.06, 1.10) | 4.16 | (0.94, 18.33) | 2.28 | (0.53, 9.76) | 3.62 | (1.83, 7.16) | 3.59 | (1.62, 7.95) | ||
| Moderno | 0.36 | (0.17, 0.79) | 0.35 | (0.15, 0.82) | 2.90 | (0.67, 12.47) | 1.92 | (0.48, 7.67) | 2.70 | (1.38, 5.28) | 2.63 | (1.23, 5.60) | ||
| Other/unknown | - | - | - | - | 6.21 | (0.60, 63.73) | 20.12 | (2.21, 183.59) | 2.76 | (0.67, 11.37) | 2.39 | (0.67, 8.55) | ||
| Sexual behavior in the last three encounters | ||||||||||||||
| No IOI | Ref | Ref | No ROI | Ref | Ref | No cRAI | Ref | Ref | ||||||
| IOI | 3.23 | (0.99, 10.61) | 2.12 | (0.56, 8.09) | ROI | 1.18 | (0.46, 3.03) | 0.81 | (0.31, 2.12) | cRAI | 1.49 | (1.08, 2.07) | 1.18 | (0.86, 1.63) |
| No cIAI | Ref | Ref | ||||||||||||
| cIAI | 1.47 | (0.71, 3.05) | 0.81 | (0.38, 1.71) | ||||||||||
| Other sites of infection | ||||||||||||||
| Urethral | - | - | - | - | - | - | - | - | 2.36 | (1.39, 3.98) | 3.53 | (2.10, 5.93) | ||
| Pharyngeal | - | - | - | - | - | - | - | - | 4.37 | (3.14, 6.09) | 3.91 | (2.77, 5.52) | ||
| Rectal | 2.94 | (1.39, 6.23) | 4.43 | (2.07, 9.50) | 8.39 | (4.17, 16.84) | 8.32 | (3.88, 17.85) | - | - | - | - | ||
Bold text = p-value <0.05.
Adjusted for: age, HIV infection, sexual orientation, sexual role, sexual behavior in the last three encounters, and other sites of infection.
cIAI, condomless insertive anal intercourse; cRAI, condomless receptive anal intercourse; IOI, insertive oral intercourse; ROI, receptive oral intercourse
Discussion
To our knowledge, our study is the first to both report prevalence and differentiate between epidemiologic patterns of urethral, pharyngeal, and rectal GC and CT infection among MSM in Latin America. Previous studies have established a dichotomy between urethral infection (which is more likely to be symptomatic, diagnosed, and treated), and pharyngeal or rectal infections (which are frequently asymptomatic, occult, and consolidated under the rubric of “extra-genital infection”) (5, 10, 13). Few studies have examined correlations between infection at a specific anatomic site and risk factors for STD acquisition and onward transmission (14, 17). Our study is unique in that it synthesizes these approaches, describing prevalence at each site and exploring how correlates of infection differ by site, rather than considering pharyngeal and rectal infections as interchangeable diseases. This approach allows us to consider each site as a potential correlate of multi-site infection at another location, to highlight differences in sociobehavioral correlates of infection by anatomic site, and to identify the potential public health impact of diagnosis and treatment of occult infections at each site.
Consistent with previous studies, our results show that urethral GC and CT are more often symptomatic than rectal infections (13), and urethral GC is more often symptomatic than urethral CT (27). We also found urethral CT was associated with an activo role, which has been described previously as a heterosexual consolidation of masculinity in Peru and associated with MSM reporting a heterosexual orientation (28). Combined with the fact that urethral CT was frequently asymptomatic in our sample, this finding suggests timely diagnosis and prevention of transmission to male and female partners of affected men relies on clinician assessments of sensitive subjects like sexual role and behavior. This finding also has implications for women because cervical CT is often asymptomatic, but can lead to pelvic inflammatory disease (PID), pregnancy complications, and infertility (3, 29). Targeting this subgroup of MSM for urethral NAAT testing for CT rather than screening all MSM could limit spending while limiting the spread of chlamydia through MSM populations and associated heterosexual networks.
Consistent with several previous studies of MSM in the US, the oropharynx was the most common site of GC infection in our study (5, 13, 27). While pharyngeal GC poses minimal health risk to its carriers (7, 8), the oropharynx has been shown to act as a transmission reservoir for urethral infection via oral sex (30). Others suggest pharyngeal infection may be spread to the rectum by anilingus or “rimming” and to the oropharynx of others by kissing (16). Moreover, because pharyngeal infection is often asymptomatic, emerging antibiotic resistant strains may go undetected and serve as a reservoir for the spread of resistance throughout the population (3). The most effective public health approach to this common, asymptomatic reservoir for antimicrobial resistance would be to screen all sexually active MSM for pharyngeal GC.
The rectum was the most common site of CT infection in our study. Participants with rectal infection were less likely than those with urethral infection to have symptomatic disease. Moreover, rectal CT was associated with HIV infection in our sample, and has been epidemiologically linked with HIV acquisition in other settings (18). Accordingly, screening for rectal CT could be a cost-effective strategy to identify and target the highest-risk MSM for delivery of social and biomedical HIV and STD prevention interventions. Whether the increased risk for HIV acquisition following rectal CT infection is due to biological or behavioral factors, or a combination of the two, targeting prevention services and STD treatment to MSM with occult rectal CT may be an effective strategy for limiting HIV acquisition and transmission throughout their sexual network.
Strategies to reduce cost in developed country settings recommend MSM be screened at sites of sexual contact based on self-reported risk behaviors (23). However, in our sample, pharyngeal and rectal GC and CT infection were frequently diagnosed in men reporting no relevant risk behaviors with their three most recent partners. This understudied phenomenon has been reported in other studies as well (3). Our results suggest clinicians could use sexual role as a proxy for sexual risk behavior in assessing anatomic site-specific STD risk, but only in addition to a detailed exploration of recent sexual practices as the consistent presence of multi-site GC and CT infections in our sample suggests sexual role segregation among MSM does not preclude cross-transmission of bacterial STDs across multiple anatomic sites.
Our findings should be considered in the context of several limitations. First, our results may not be generalizable to all MSM in Lima because we collected a convenience sample of men who volunteered to be screened for a trial of partner notification at one clinical site. As the recruitment site is a center for HIV and STD research, our sample is likely to be higher risk, and have a higher prevalence of HIV infection, than the general MSM population. Second, because we collected data only on the three most recent sexual partners, the time frame of our analysis was limited, and lacks comprehensive data on all recent sexual practices. For example, while our sample included men with rectal GC and CT infection who did not endorse RAI, our results may have been different had we asked about RAI with any recent partners. Third, due to the cross-sectional nature of this sample, we were not able to assess the temporal association of rectal STDs with HIV incidence. However, we did identify a baseline association between HIV and rectal CT, suggesting an important area for future study.
Conclusions
Our results highlight limitations of the current syndromic management approach to STDs in Peru, wherein urethral CT and rectal GC and CT may be missed due to their frequently asymptomatic presentations. Successful management of GC and CT infections among MSM in low-resource settings requires differentiating between bacterial agent, symptomatology, associated risk factors, and public health implications of infection at different anatomic sites.
Acknowledgments
We would like to thank the study participants and staff who devoted their time and efforts to make this project possible. Funding for this work was provided by the US National Institute of Health grants NIH R25 MH087222 to JLC, R21 MH 092322, and K23 AI110532 to JEL.
Sources of Support: Funding for this work was provided by the US National Institute of Health grants NIH R25 MH087222 to JLC, R21 MH 092322, and K23 AI110532 to JEL
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government.
Footnotes
We have no conflicts of interest to disclose.
Copyright Statement: SM is an employee of the U.S. Government. This work was prepared as part of her official duties. Title 17 U.S.C. § 105 provides that ‘Copyright protection under this title is not available for any work of the Unites States Government.’ Title 17 U.S.C. § 101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person's official duties.
References
- 1.Allan-Blitz LT, Leon SR, Bristow CC, Konda KA, Vargas SK, Flores JA, et al. High prevalence of extra-genital chlamydial or gonococcal infections among men who have sex with men and transgender women in Lima, Peru. International Journal of STD and AIDS. 2017;28(2):138–44. doi: 10.1177/0956462416630909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leon SR, Segura ER, Konda KA, Flores JA, Silva-Santisteban A, Galea JT, et al. High prevalence of Chlamydia trachomatis and Neisseria gonorrhoeae infections in anal and pharyngeal sites among a community-based sample of men who have sex with men and transgender women in Lima, Peru. BMJ Open. 2016;6(1):e008245. doi: 10.1136/bmjopen-2015-008245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan PA, Robinette A, Montgomery M, Almonte A, Cu-Uvin S, Lonks JR, et al. Extragenital Infections Caused by Chlamydia trachomatis and Neisseria gonorrhoeae: A Review of the Literature. Infectious Diseases in Obstetrics and Gynecology. 2016;2016:5758387. doi: 10.1155/2016/5758387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kent CK, Chaw JK, Wong W, Liska S, Gibson S, Hubbard G, et al. Prevalence of Rectal, Urethral, and Pharyngeal Chlamydia and Gonorrhea Detected in 2 Clinical Settings among Men Who Have Sex with Men: San Francisco, California, 2003. Clinical Infectious Diseases. 2005;41(1):67–74. doi: 10.1086/430704. [DOI] [PubMed] [Google Scholar]
- 5.Marcus JL, Bernstein KT, Kohn RP, Liska S, Philip SS. Infections Missed by Urethral-Only Screening for Chlamydia or Gonorrhea Detection Among Men Who Have Sex With Men. Sexually Transmitted Diseases. 2011;38(10):922–4. doi: 10.1097/OLQ.0b013e31822a2b2e. [DOI] [PubMed] [Google Scholar]
- 6.Clark JL, Lescano AG, Konda KA, Leon SR, Jones FR, Klausner JD, et al. Syndromic management and STI control in urban Peru. PLoS One. 2009;4(9):e7201. doi: 10.1371/journal.pone.0007201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. WHO Guidelines for the Treatment of Neisseria gonorrhoeae. Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- 8.World Health Organization. WHO Guidelines for the Treatment of Chlamydia trachomatis. Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- 9.Soni S, White JA. Self-Screening for Neisseria gonorrhoeae and Chlamydia trachomatis in the Human Immunodeficiency Virus Clinic- High Yields and High Acceptability. Sexually Transmitted Diseases. 2011;38(12):1107–9. doi: 10.1097/OLQ.0b013e31822e6136. [DOI] [PubMed] [Google Scholar]
- 10.Patton ME, Kidd S, Llata E, Stenger M, Braxton J, Asbel L, et al. Extragenital Gonorrhea and Chlamydia Testing and Infection Among Men Who Have Sex With Men - STD Surveillance Network, United States, 2010-2012. Clinical Infectious Diseases. 2014;58(11):1564–70. doi: 10.1093/cid/ciu184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alirol E, Wi TE, Bala M, Bazzo ML, Chen XS, Deal C, et al. Multidrug-resistant gonorrhea: A research and development roadmap to discover new medicines. PLoS medicine. 2017;14(7):e1002366. doi: 10.1371/journal.pmed.1002366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sadiq ST, Taylor S, Copas AJ, Bennett J, Kaye S, Drake SM, et al. The effects of urethritis on seminal plasma HIV-1 RNA loads in homosexual men not receiving antiretroviral therapy. Sexually Transmitted Infections. 2005;81:120–3. doi: 10.1136/sti.2004.010249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiddou R, Alcaide M, Rosa-Cunha I, Castro J. Pharyngeal Gonorrhea and Chlamydial Infections in Men who have Sex with Men, a Hidden Threat to the HIV Epidemic. Journal of Therapy and Management in HIV Infection. 2013;1:19–23. [Google Scholar]
- 14.Morris SR, Klausner JD, Buchbinder SP, Wheeler SL, Koblin B, Coates TJ, et al. Prevalence and Incidence of Pharyngeal Gonorrhea in a Longitudinal Sample of Men Who Have Sex with Men: The EXPLORE Study. Clinical Infectious Diseases. 2006;43(10):1284–9. doi: 10.1086/508460. [DOI] [PubMed] [Google Scholar]
- 15.Ameyama S, Onodera S, Takahata M, Minami S, Maki N, Endo K, et al. Mosaic-like structure of penicillin-binding protein 2 Gene (penA) in clinical isolates of Neisseria gonorrhoeae with reduced susceptibility to cefixime. Antimicrobial agents and chemotherapy. 2002;46(12):3744–9. doi: 10.1128/AAC.46.12.3744-3749.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fairley CK, Hocking JS, Zhang L, Chow EP. Frequent Transmissions of Gonorrhea in Men Who Have Sex with Men. Emerging Infectious Diseases. 2017;23(1):102–4. doi: 10.3201/eid2301.161205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turner AN, Reese PC, Ervin M, Davis JA, Fields KS, Bazan JA. HIV, rectal chlamydia and rectal gonorrhea in men who have sex with men attending an STD clinic in a midwestern US city. Sexually Transmitted Diseases. 2013;40(6) doi: 10.1097/OLQ.0b013e31828fd163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barbee LA, Khosropour CM, Dombrowski JC, Golden MR. New Human Immunodeficiency Virus Diagnosis Independently Associated with Rectal Gonorrhea and Chlamydia in Men Who Have Sex With Men. Sexually Transmitted Diseases. 2017;44(7):385–9. doi: 10.1097/OLQ.0000000000000614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Henning T, Butler K, Mitchell J, Ellis S, Deyounks F, Farshy C, et al. Development of a rectal sexually transmitted infection--HIV coinfection model utilizing Chlamydia trachomatis and SHIVSF162p3. Journal of medical primatology. 2014;43(3):135–43. doi: 10.1111/jmp.12103. [DOI] [PubMed] [Google Scholar]
- 20.Katz DA, Dombrowski JC, Bell TR, Kerani RP, Golden MR. HIV Incidence Among Men Who Have Sex With Men After Diagnosis With Sexually Transmitted Infections. Sexually Transmitted Diseases. 2016;43(4):249–54. doi: 10.1097/OLQ.0000000000000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ministerio de Salud de la Republica del Peru. Guias Nacionales de Atencion Integral de la Salud Sexual y Reproductiva. Lima, Peru: Ministerio de Salud; 2004. [Google Scholar]
- 22.Clark JL, Segura ER, Oldenburg CE, Rios J, Montano SM, Perez-Brumer A, et al. Expedited Partner Therapy (EPT) increases the frequency of partner notification among MSM in Lima, Peru: a pilot randomized controlled trial. BMC medicine. 2017;15(1):94. doi: 10.1186/s12916-017-0858-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Workowski KA, Bolan GA. Sexually Transmitted Diseases Treatment Guidelines, 2015. MMWR Recomm Rep. 2015;64(3):1–138. Update: https://www.cdc.gov/std/tg2015/default.htm. [PMC free article] [PubMed] [Google Scholar]
- 24.Coutinho LM, Scazufca M, Menezes PR. Methods for estimating prevalence ratios in cross-sectional studies. Revista de saude publica. 2008;42(6):992–8. [PubMed] [Google Scholar]
- 25.Behrens T, Taeger D, Wellmann J, Keil U. Different methods to calculate effect estimates in cross-sectional studies. A comparison between prevalence odds ratio and prevalence ratio. Methods of information in medicine. 2004;43(5):505–9. [PubMed] [Google Scholar]
- 26.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC medical research methodology. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Danby C, Cosentino LA, Rabe LK, Priest CL, Damare KC, Macio IS, et al. Patterns of Extragenital Chlamydia and Gonorrhea in Women and Men Who Have Sex With Men Reporting a History of Receptive Anal Intercourse. Sexually Transmitted Diseases. 2016;43(2):105–9. doi: 10.1097/OLQ.0000000000000384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clark J, Salvatierra J, Segura E, Salazar X, Konda K, Perez-Brumer A, et al. Moderno love: sexual role-based identities and HIV/STI prevention among men who have sex with men in Lima, Peru. AIDS Behav. 2013;17(4):1313–28. doi: 10.1007/s10461-012-0210-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mitchell C, Prabhu M. Pelvic inflammatory disease: current concepts in pathogenesis, diagnosis and treatment. Infectious disease clinics of North America. 2013;27(4):793–809. doi: 10.1016/j.idc.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lafferty WE, Hughes JP, Handsfield HH. Sexually transmitted diseases in men who have sex with men. Acquisition of gonorrhea and nongonococcal urethritis by fellatio and implications for STD/HIV prevention. Sex Transm Dis. 1997;24(5):272–8. doi: 10.1097/00007435-199705000-00007. [DOI] [PubMed] [Google Scholar]