Abstract
Deficits in social communication are a core feature of autism spectrum disorder (ASD), yet significant social problems have been observed in youth with many neurodevelopmental disorders. In this preliminary investigation, we aimed to explore whether domains of social reciprocity (i.e., social communication, social cognition, social awareness, social motivation, and restricted and repetitive behaviors) represent transdiagnostic traits. These domains were compared across youth ages 7 to 17 with obsessive-compulsive disorder (OCD; N=32), tic disorders (TD; N=20), severe mood dysregulation (N=33) and autism spectrum disorder (N=35). While the ASD group was rated by parents as exhibiting the greatest social reciprocity deficits across domains, a high proportion of youth with severe mood dysregulation also exhibited pronounced deficits in social communication, cognition, and awareness. The ASD and severe mood dysregulation groups demonstrated comparable scores on the social awareness domain. In contrast, social motivation and restricted and repetitive behaviors did not appear to be transdiagnostic domains in severe mood dysregulation, OCD, or TD groups. The present work provides preliminary support that social awareness, and to a lesser extent social communication and cognition, may represent features of social reciprocity that are transdiagnostic across ASD and severe mood dysregulation.
Keywords: social reciprocity, social communication, neurodevelopmental disorders, autism spectrum disorder, child, adolescent, transdiagnostic
1. Introduction
The construct of social reciprocity includes several components: social communication (interaction), understanding how to react in social situations (social awareness), desire to interact with others (social motivation), ability to attribute perspective to others (social cognition), and appropriate management of atypical (restrictive and repetitive) behaviors in social settings (Constantino and Gruber, 2005). Social reciprocity deficits are considered a core feature of autism spectrum disorder (ASD; American Psychiatric Association, 2013). Yet social reciprocity difficulties may not be limited to ASD, as social problems have been demonstrated as a correlate of several neurodevelopmental conditions.
Very few studies have examined social reciprocity in youth with other neurodevelopmental disorders. In regard to obsessive-compulsive disorder (OCD) and tic disorder (TD), studies have only examined the affected group (Griffiths et al., 2017; McGuire et al., 2013; Stewart et al., 2016) or compared the affected sample to healthy controls (Guler et al., 2015). Across investigations, findings support the hypothesis that youth with OCD and TD experience elevations in social impairment relative to measurement norms and case controls. Unfortunately, little work has been done to examine social responsiveness impairments between youth with ASD, a group for which social impairments are a defining feature, and those with OCD and/or TD, who appear to have impairment in comparison to non-affected youth. Additionally, severe mood dysregulation, a condition characterized by excessive irritability, reactivity, and hyperarousal (Leibenluft et al., 2003; Brotman et al., 2006), has also been associated with pronounced impairment in social communication in youth (Pine et al., 2008; Rich et al., 2010). Given these findings that other neurodevelopmental disorders are associated with social impairment, social reciprocity has been proposed as a transdiagnostic construct (Constantino, 2011; Constantino and Frazier, 2013). This hypothesis has clinical significance for two reasons. First, it suggests that social reciprocity might be measured across neurodevelopmental conditions using standardized measurement in order to compare across conditions. Second, it may indicate the degree to which social reciprocity should be assessed and targeted in intervention across neurodevelopmental disorders, and not only in ASD. Unfortunately, little work has been done to examine domains of social functioning across neurodevelopmental conditions.
The present study aims to explore domains of social reciprocity as putative transdiagnostic constructs in four pediatric psychiatric groups: ASD, OCD, TD, and severe mood dysregulation. Social reciprocity subdomains were defined as: social awareness, social communication, social cognition, social motivation, and restricted and repetitive behaviors. In this preliminary investigation, we defined “transdiagnostic” using two criteria: (Aim 1) whether diagnostic groups would demonstrate comparable mean scores and (Aim 2) whether a significant (50%) proportion of each group would endorse clinically significant scores on social reciprocity subdomains. To this end, we utilized the most common dimensional parent-report of youth social behavior as an initial evaluation of this question (Social Responsiveness Scale; Constantino and Gruber, 2005). For Aim 1, we hypothesized that OCD, TD, and ASD groups would demonstrate comparable scores in restricted and repetitive behavior due to the repetitive nature of compulsions and tics, and that severe mood dysregulation and ASD groups would demonstrate comparable scores on social awareness, communication, and cognition, areas in which youth with severe mood dysregulation have previously been found to show impairment (Pine et al., 2008). For Aim 2, we hypothesized that a significant proportion of OCD and TD groups would exhibit elevations in restrictive and repetitive behaviors, while a significant proportion of the severe mood dysregulation group would exhibit elevations in social awareness, communication, and cognition. Prior studies of the SRS in non-ASD psychiatric (e.g., anxiety, mood disorders) samples have found that over 50% of youth endorsed elevated scores on the SRS (e.g., Pine, Guyer, Goldwin, Towbin, & Leibenluft, 2008). Based on this, and the desire to select a proportion cutoff that would reflect a majority, we utilized a 50% cutoff when identifying the proportion of each group with elevated SRS subscale scores.
2. Methods
2.1 Participants
OCD, TD, and severe mood dysregulation.
For the present study, deidentified data were compiled from separate research protocols approved by the UCLA Institutional Review Board. The OCD group was recruited for computerized intervention (R34 MH095885), the TD group for habit reversal training (P50 MH077248 02), and the severe mood dysregulation group for psychopharmacologic (R21 MH093582) studies. Youth age ranged between 7 and 17 years (severe mood dysregulation: 7–17, OCD: 8–17, TD: 9–14) and IQ was ≥ 80 across studies, and none had received a diagnosis of ASD. For this investigation, youth within each psychiatric group who received a secondary diagnosis of interest (e.g., youth with primary OCD who also had TD) were excluded. As all youth in the severe mood dysregulation group also had comorbid ADHD, we elected to exclude youth with comorbid ADHD from the OCD and TD groups. This yielded a final sample of 32 youth with OCD, 20 with TD, and 33 with severe mood dysregulation. Parents completed the Social Responsiveness Scale (Constantino and Gruber, 2005) and Child Behavior Checklist (Achenbach and Rescorla, 2001) during initial evaluation for each intervention trial. All youth met diagnostic criteria for respective diagnoses, determined through semi-structured interviews using the Kiddie-SADS (Kaufman et al., 1997; severe mood dysregulation, TD) or Anxiety Disorders Interview Schedule (Silverman and Albano, 1996; OCD). See Table 1 for demographic characteristics by group and Table 1 in supplementary materials for key inclusion/exclusion criteria for each study.
Table 1.
Sample demographic and clinical information by group
| TD | OCD | Severe Mood Dysregulation |
ASD | |
|---|---|---|---|---|
| (N=20) | (N=32) | (N=33) | (N=35) | |
| Age M(SD)** | 11.02(1.52) | 12.41(3.03)dc | 10.31(2.58)b | 10.14(2.52)b |
| Gender % male* | N=14(70%) | N=15(47%)d | N=20(61%) | N=28(80%) |
| FSIQ M(SD) | 104.55(10.62) | 109.97(13.59) | 103.62(14.33) | 102.29(15.60) |
| CGIS | 4.58(0.77) | 4.72(0.63) | 4.64(0.99) | |
| CBCL Anxious/ Depressed*** |
55.75(5.89)bc | 64.28(9.07)a | 65.25(9.73)ad | 59.37(9.04)c |
significant at p < .05
significant at p < .01
significant at p < .001
= Tic
= OCD
= Severe Mood Dysregulation
= ASD
ASD.
The ASD group (N=35) was randomly sampled from youth with ASD in the Simons Simplex Collection (SSC; Fischbach and Lord, 2010) who were ages 7 to 17, had full scale IQ ≥ 80, and who fell below the CBCL Attention Problems subscale cut-off for clinical significance (t-score=70; N=662). Representativeness of the ASD subsample was evaluated by computing ordinary nonparametric bootstrap means (replications = 1000) and corresponding standard errors for each predictor and outcome of interest, and evaluating differences between bootstrap estimates and subsample using Cohen’s d. All differences between subsample means and bootstrap mean estimates fell below/within a small effect size difference (d=.20-.30, M=.06), excluding FSIQ in girls with ASD (d=.68, Mbootstrap=103.23, SEbootstrap= 2.15, Msample=93.57, SEsample=4.20).
2.2 Measures
Social Responsiveness Scale (Constantino and Gruber, 2005) is a 65-item measure that dimensionally assesses five domains of social reciprocity: social cognition, social communication, social awareness, restricted and repetitive behaviors, and social motivation. In this study, subscale raw scores were used to maintain maximum variability in responses for general linear models, and t-scores were used for between-group comparison of clinical cut-offs.
Child Behavior Checklist (CBCL; Achenbach and Rescorla, 2001) is a parent-report measure of youth emotional and behavioral problems. In this study, we used the Anxious/Depressed subscale of the CBCL as a covariate in analyses given that each condition under study has been associated with internalizing symptoms and diagnoses, and others have found internalizing youth to experience social difficulties (e.g., Strauss et al., 2010).
FSIQ:
Full scale IQ (FSIQ) was measured using two different instruments across the four study samples. The severe mood dysregulation, TD, and OCD groups were assessed using the Weschler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999). The ASD sample was assessed using the Differential Ability Scales-Second Edition Global Conceptual Ability (DAS; Elliott, 2007).
CGI-S:
The clinical global impression severity scale (CGI-S; Guy, 1976) is presented to reflect disorder-related clinical severity in the severe mood dysregulation, TD, and OCD groups.
Analyses
Prior to conducting analyses, we compared diagnostic groups on relevant demographic (i.e., age, gender) variables and total social reciprocity scores using ANOVAs. For Aim 1, group differences on each of the five SRS subscale raw scores were tested using five separate general linear models in SPSS version 24. In each model, the respective SRS subscale was entered as the dependent variable, and group, age, CBCL Anxious/Depressed t-score, and interactions were tested as predictors. A family-wise Bonferroni correction was used to account for multiple comparisons (α=.05/5=.01) for each main effects analysis. Insignificant interactions were dropped from each analysis, however all main effects (i.e., age, Anxious/Depressed t-score) were retained regardless of significance. Post-hoc Bonferroni-corrected pairwise comparisons were conducted to evaluate differences between diagnostic groups. For Aim 2, likelihood ratio chisquare tests were conducted with SAS version 9.4 to evaluate whether the percentage of youth endorsing clinically significant symptoms in each social reciprocity domain differed by diagnostic group.
3. Results
Overall, youth with ASD were rated as having higher scores across SRS subscales in comparison to youth with OCD, TD, and SMD. There were significant group differences in age, F(1,116)=5.34, p<.01, and therefore age was included as a covariate in general linear models.
For Aim 1 general linear models, the interactions between age and diagnostic group, and CBCL Anxious/Depressed subscale and group, were not significant (p>.05), and these interactions were dropped from subsequent analyses. For each domain, there was a significant effect of diagnostic group and post hoc tests were explored (see Figure 1 for all post-hoc tests).
Figure 1.
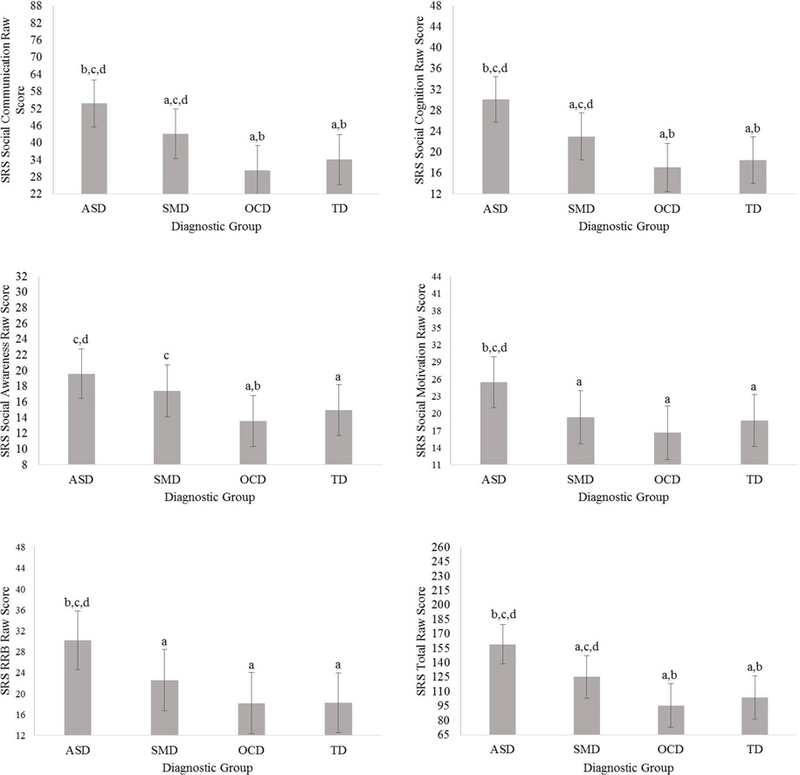
Comparison of social reciprocity domain scores across diagnostic groups. Letters (a, b, c, d) are indicative of a significant difference between the diagnostic group, and the diagnostic group with the corresponding letter; “a” = ASD, “b” = severe mood dysregulation (SMD), “c” = OCD, “d” = TD. Error bars reflect standard deviation.
For social cognition and social communication, post-hoc comparisons indicated that the severe mood dysregulation group exhibited significantly greater impairment than OCD and TD groups. OCD and TD groups did not significantly differ on social cognition or communication. The ASD group was significantly more impaired on social cognition and cognition than all other groups.
For social awareness, post-hoc comparisons indicated that the severe mood dysregulation group scored significantly higher than the OCD, but not the TD, group. OCD and TD groups did not significantly differ on social awareness. The ASD group was significantly more impaired on social awareness than OCD and TD groups, but not the severe mood dysregulation group.
For restricted and repetitive behaviors and social motivation, post-hoc tests revealed that the severe mood dysregulation, OCD, and TD groups did not significantly differ from one another. The ASD group was significantly more impaired on restricted and repetitive behaviors and social motivation than all other groups.
For Aim 2, there were significant between-group differences in the proportion of youth scoring above clinical significance (>60 t-score) in each of the five subscales (Table 3). More than 50% of the ASD group endorsed clinically significant scores on each of the five subscales. More than 50% of the severe mood dysregulation group endorsed clinically significant scores on all subscales with the exception of social motivation. For OCD and TD groups, comparably lower proportions of the samples exceeded clinical-cutoffs. As such a low proportion of OCD and TD groups demonstrated elevated subscale and total scores, we then examined whether the severe mood dysregulation and ASD groups differed. For social cognition, social communication, restricted and repetitive behaviors, and social motivation, significantly more individuals with ASD endorsed clinical levels of behavior. In contrast, for social awareness, ASD and severe mood dysregulation groups did not differ in the proportion of youth exhibiting clinically significant impairment.
Table 3.
Proportion of youth in each group meeting elevated symptom cutoffs across social reciprocity domains
| ASD (%) |
Severe Mood Dysregulation (%) |
OCD (%) |
TD (%) |
LR-χ2 | ||
|---|---|---|---|---|---|---|
| Social awareness |
> 60 | 65.71 | 54.84 | 18.75 | 10.53 | 27.05, p<.001 |
| Social cognition |
> 60 | 94.29 | 54.55 | 12.90 | 10.53 | 71.97, p<.001 |
| Social communication |
> 60 | 88.57 | 59.38 | 6.45 | 5.56 | 69.28, <.001 |
| Social motivation |
> 60 | 54.29 | 27.27 | 19.35 | 10.00 | 15.49, p<.01 |
| Restricted and Repetitive Behavior |
> 60 | 88.57 | 50.00 | 22.58 | 15.00 | 44.18, p<.001 |
| Total | > 60 | 94.29 | 56.67 | 14.29 | 5.88 | 65.53, p<.001 |
4. Discussion
In this preliminary study, we tested the hypothesis that subdomains of social reciprocity may be transdiagnostic constructs across several pediatric neurodevelopmental disorders. Specifically, we compared youth with OCD, TD, and severe mood dysregulation to those with ASD, and examined the proportion of each group demonstrating elevations in: social awareness, social communication, social cognition, social motivation, and restricted and repetitive behavior. We found that the ASD group was rated by parents as exhibiting the greatest elevations, and a larger proportion of the ASD sample exceeded clinical cutoffs, compared to the other diagnostic groups in most subdomains. These findings are not surprising, as the SRS – our measure of social reciprocity – was developed for use with ASD (Constantino and Gruber, 2005).
We also found preliminary evidence that a high proportion of youth with severe mood dysregulation also exhibit pronounced deficits in social communication, cognition, and awareness. However, based on our two definitions of transdiagnostic traits, it should be noted that ASD and severe mood dysregulation groups demonstrated comparable scores only for the social awareness domain. It may be possible that ASD and severe mood dysregulation groups appeared phenomenologically similar in social awareness because youth in both groups may demonstrate a lack of awareness about their environment and situational social norms. However, we were not able to test whether the underlying processes are similar (e.g., both groups experience hyperarousal, which may interfere with social awareness) or distinct (e.g., youth with severe mood dysregulation may experience distractibility and flight of ideas [Leibenluft et al., 2003], while youth ASD may lack an understanding of, or interest in, social situations [Chevallier et al., 2012]). Future work in this area may help to explicate whether similar mechanisms underlie social awareness deficits in ASD and severe mood dysregulation, and test the sequencing of deficits in social reciprocity in relation to symptom/diagnostic presentation. Social awareness skills, however, do not occur in isolation, and given our findings that a significant proportion of the severe mood dysregulation group also were rated as elevated in social communication and cognition deficits, interactions between social reciprocity domains should also be considered. In addition, the current study lends support to findings that have described the negative impact of mood symptoms on social responsiveness (Grzadzinski et al., 2011). Prior research has found that, in fact, the presence of oppositional behavior and mood symptoms, both characteristic of severe mood dysregulation, discriminates individuals with ADHD with impaired social responsiveness and those without (Grzadzinski et al., 2011). While the all youth with severe mood dysregulation in the current study also endorsed diagnoses of ADHD, it appears that the presence of mood symptoms may be particularly impairing in regard to social responsiveness.
Of note, social motivation and restricted and repetitive behaviors did not appear to be transdiagnostic domains in severe mood dysregulation, OCD, or TD groups. Social motivation falls squarely within the core diagnostic criteria for ASD (e.g., deficits in social-emotional reciprocity) and theoretical work has proposed that social motivation underlies the social impairments that characterize ASD (e.g., Chevallier et al., 2012). Similarly, absence of marked elevation in restricted and repetitive behaviors in OCD and TD groups suggest that the SRS items assessing these behaviors may in fact be specific to ASD (e.g., unusual sensory interests, unusually narrow range of interests) and do not capture the repetitive nature of compulsions or tics. This finding may suggest that, at least on the SRS, endorsement of social motivation and restrictive and repetitive behavior problems for youth with severe mood dysregulation, OCD, and TD are unrelated to these disorders and instead reflect features associated with ASD. Future studies might test parent- or clinician-rated, or behavioral, assessments of these social reciprocity domains to determine whether this finding is specific to the SRS.
Although prior studies have found that youth with OCD and TD exhibit deficits in social reciprocity (Griffiths et al., 2017; Guler et al., 2015; McGuire et al., 2013; Stewart et al., 2016), our data suggest that these groups exhibit less impairment in social reciprocity domains when compared to neurodevelopmental groups for which social deficits are a hallmark feature (i.e., ASD). Mean group comparisons in our sample suggested that OCD and TD group demonstrated significantly less impairment than ASD and SMD groups in social cognition and social communication, as well as less impairment than the ASD group in social awareness. Moreover, less than 22% of the OCD group and less than 15% of the TD group exhibited clinical elevations across social reciprocity subscales. Therefore, while youth with OCD and TD may exhibit relatively greater mean impairments than normed samples or non-affected youth (Griffiths et al., 2017; Guler et al., 2015; McGuire et al., 2013; Stewart et al., 2016; Storch et al., 2007), the vast majority of youth in OCD and TD groups may not show social deficits that rise to clinical levels. This is not surprising, as diagnostic criteria for these conditions do not necessitate social impairments and do not necessarily impact social abilities. Instead, the global social functioning deficits associated with these conditions (Piacentini et al., 2003) may be due to the impact of the psychopathology itself on opportunities to engage with peers.
The results of this preliminary investigation should be considered in the context of methodological limitations. The severe mood dysregulation, OCD, and TD diagnostic groups were comprised of treatment-seeking families, which may represent youth with greater clinical severity than the ASD group. Additionally, variability in study inclusion/exclusion criteria (e.g., age, excluded co-occurring medical conditions, prior treatment) may have contributed to observed differences between groups. In addition, for each diagnostic group, we excluded youth with the other diagnoses under study, in order to understand the unique contribution of each disorder; thus, findings may not necessarily be generalizable to youth with more complex symptom presentations. The sample size of each group was relatively small, which may limit our ability to draw conclusions about the broader heterogeneous populations under study. Finally, the study focused on one parent-report measure of social reciprocity and future work might take a multimodal assessment approach. Despite these limitations, the present work provides preliminary support that social awareness, and to a lesser extent social communication and cognition, may represent features of social reciprocity that are transdiagnostic across ASD and severe mood dysregulation. Additional work in this area may provide clarification and a more nuanced understanding of whether and how the mechanisms underlying social reciprocity may span across neurodevelopmental conditions, as well as the environmental conditions and stimuli that may drive social behavior.
Supplementary Material
Table 2.
| SRS Subscale | Parameter | F | Significance | ƞ2 |
|---|---|---|---|---|
| Social Cognition | ||||
| Model | 38.64 | p < 0.001 | 0.63 | |
| Group | 54.68 | p <.001 | 0.59 | |
| CBCL Anx/Dep | 28.02 | p <.001 | 0.20 | |
| Age | 1.71 | p = 0.19 | 0.02 | |
| Social Communication | ||||
| Model | 30.50 | p < 0.001 | 0.58 | |
| Group | 46.30 | p < 0.001 | 0.56 | |
| CBCL Anx/Dep | 16.72 | p < 0.001 | 0.13 | |
| Age | 6.88 | p = 0.01 | 0.06 | |
| Social Awareness | ||||
| Model | 13.34 | p < 0.001 | 0.38 | |
| Group | 21.20 | p < 0.001 | 0.37 | |
| CBCL Anx/Dep | 4.38 | p = 0.04 | 0.04 | |
| Age | 4.58 | p = 0.03 | 0.04 | |
| RRB | ||||
| Model | 20.70 | p < 0.001 | 0.48 | |
| Group | 30.27 | p < 0.001 | 0.45 | |
| CBCL Anx/Dep | 13.78 | p < 0.001 | 0.11 | |
| Age | 2.17 | p = 0.14 | 0.02 | |
| Social Motivation | ||||
| Model | 19.18 | p < 0.001 | 0.46 | |
| Group | 22.59 | p < 0.001 | 0.38 | |
| CBCL Anx/Dep | 35.73 | p < 0.001 | 0.24 | |
| Age | 4.06 | p = 0.046 | 0.04 |
Note. “CBCL Anx/Dep” = CBCL Anxious/Depressed Subscale T score
Highlights.
Social reciprocity was tested as a transdiagnostic construct in psychiatric youth.
Overall, youth with autism demonstrated deficits across social domains.
Social awareness deficits were found in autism and severe mood dysregulation (SMD).
Significant social deficits were not observed in OCD or tic disorders.
Social awareness may represent a common feature across pediatric autism and SMD.
Acknowledgments:
This work was partially supported by R34 MH095885 [Chang], P50 MH077248 02 [McCracken, Piacentini], Psyadon Pharmaceuticals research support [McCracken], R21 MH093582, NeuroSigma Inc grant support [McGough] and UCLA CTSI UL1TR000124 [Rozenman].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Rescorla LA, 2001. Manual for the ASEBA School-Age Forms and Profiles Burlington, VT: University of Vermont Research Center for Children, Youth and Families. [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders 5th ed. Washington, D. C. [Google Scholar]
- Brotman MA, Schmajuk M, Rich BA, Dickstein DP, Guyer AE, Costello EJ, Egger HL, Angold A, Pine DS, Leibenluft E, 2006. Prevalence, Clinical Correlates, and Longitudinal Course of Severe Mood Dysregulation in Children. Biol. Psychiatry 60, 991–997. [DOI] [PubMed] [Google Scholar]
- Chevallier C, Kohls G, Troiani V, Brodkin ES, Schultz RT, 2012. The social motivation theory of autism. Trends Cogn Sci 16, 231–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, 2011. The quantitative nature of autistic social impairment. Pediatr Res 69, 55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, Frazier TW, 2013. Commentary: The observed association between autistic severity measured by the Social Responsiveness Scale (SRS) and general psychopathology a response to Hus et al. (2013). J Child Psychol Psychiatry 54, 695– 697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP, 2005. Social Responsiveness Scale (SRS) Manual Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Elliott CD, 2007. Differential Ability Scales-Second Edition (DAS-II) San Antonio, TX: Harcourt. [Google Scholar]
- Fischbach GD, Lord C, 2010. The Simons Simplex Collection: A resource for identification of autism genetic risk factors. Neuron 68, 192–195. [DOI] [PubMed] [Google Scholar]
- Griffiths DL, Farrell LJ, Waters AM, White SW, 2017. ASD traits among youth with obsessive-compulsive disorder. Child Psychiatry Hum Dev 48, 911–921. [DOI] [PubMed] [Google Scholar]
- Grzadzinski R, Di Martino A, Brady E, Mairena MA, O’Neale M, Petkova E, Lord C & Castellanos FX, 2011. Examining autistic traits in children with ADHD: does the autism spectrum extend to ADHD?. J Autism Dev Disord, 41, 1178–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Güler AS, Berkem M, Yazgan Y, Kalaça S, 2015. Cognitive flexibility and social responsiveness in children and adolescents with Tourette Syndrome. Child Psychiatry Hum Dev 46, 940–950. [DOI] [PubMed] [Google Scholar]
- Guy W, 1976. ECDEU Assessment Manual for Psychopharmacology Rockville, MD: US Department of Health, Education, and Welfare Public Health Service Alcohol, Drug Abuse, and Mental Health Administration. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N, 1997. Schedule for Affective Disorders and Schizophrenia for School-Age ChildrenPresent and Lifetime Version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS, 2003. Defining Clinical Phenotypes of Juvenile Mania. Am J Psychiatry 160, 430–437. [DOI] [PubMed] [Google Scholar]
- McGuire JF, Hanks C, Lewin AB, Storch EA, Murphy TK, 2013. Social deficits in children with chronic tic disorders: phenomenology, clinical correlates and quality of life. Compr Psychiatry 54, 1023–1031. [DOI] [PubMed] [Google Scholar]
- Piacentini J, Bergman RL, Keller M, McCracken J, 2003. Functional impairment in children and adolescents with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol 13, 61–69. [DOI] [PubMed] [Google Scholar]
- Pine DS, Guyer AE, Goldwin M, Towbin KA, Leibenluft E, 2008. Autism spectrum disorder scale scores in pediatric mood and anxiety disorders. J Am Acad Child Adolesc Psychiatry 47, 652–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich BA, Brotman MA, Dickstein DP, Mitchell DGV, Blair RJR, Leibenluft E, 2010. Deficits in Attention to Emotional Stimuli Distinguish Youth with Severe Mood Dysregulation from Youth with Bipolar Disorder. J Abnorm Child Psychol 38, 695–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman W, Albano A, 1996. The anxiety disorders interview schedule for children-IV child and parent versions San Antonio, TX: Psychological Corporation. [Google Scholar]
- Stewart E, Cancilliere MK, Freeman J, Wellen B, Garcia A, Saptya J, Franklin M, 2016. Elevated autism spectrum disorder traits in young children with OCD. Child Psychiatry Hum Dev 47, 993–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D, 1999. Wechsler Abbreviated Scale of Intelligence Psychological Corporation. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


