Abstract
Background.
One of the most important principles in modern cervical cancer surgery is the concept of tailoring surgical radicality. In practice, this means abandoning the “one-fits-all” concept in favor of tailored operations. The term “radical hysterectomy” is used to describe many different procedures, each with a different degree of radicality. Anatomic structures are subjected to artificial dissection artifacts, as well as different interpretations and nomenclatures. This study aimed to refine and standardize the principles and descriptions of the different classes of radical hysterectomy as defined in the Querleu–Morrow classification and to propose its universal applicability.
Methods.
All three authors independently examined the current literature and undertook a critical assessment of the original classification. Images and pathologic slides demonstrating different types of radical hysterectomy were examined to document a consensual vision of the anatomy. The Cibula 3-D concept also was included in this update.
Results.
The Querleu–Morrow classification is based on the lateral extent of resection. Four types of radical hysterectomy are described, including a limited number of subtypes when necessary. Two major objectives remain constant: excision of central tumor with clear margins and removal of any potential sites of nodal metastasis.
Conclusion.
Studies evaluating radicality in the surgical management of cervical cancer should be based on precise, universally accepted descriptions. The authors’ updated classification presents standardized, universally applicable descriptions of different types of hysterectomies performed worldwide, categorized according to degree of radicality, independently of theoretical considerations.
One of the most important principles in modern cancer surgery is the concept of tailoring surgical radicality. In practice, this means abandoning the “one-fits-all” concept in favor of tailored operations. Wide surgical excision has been validated for a number of tumors including melanomas and sarcomas as well as head and neck, breast, and vulvar cancers. In surgery for cervical cancer, adaptation of radicality according to preoperative estimation of tumor location, surgical margin, and risk of occult lymphatic spread, which may be high for bulky tumors1 or negligible in the setting of low-volume disease,2 has led to the development of ultra-radical cervical cancer surgeries on the one hand and more limited surgeries on the other.
However, the term “radical” or “extended” hysterectomy currently is used to describe a variety of different procedures, each entailing a different degree of radicality. A variety of terms are currently applied to the same anatomic structures. Anatomic structures currently are defined according to different interpretations of the anatomy. Furthermore, original descriptions change over time. Finally, the addition of minor surgical variants—not all of them original—add to the confusion.
A classification of radical hysterectomies published in 20083 was adopted by the National Comprehensive Cancer Network (NCCN) and appears in the NCCN clinical practice guidelines.4 In 2011, a three-dimensional (3D) anatomic template for radical lateral parametrectomy was proposed.5 We aimed to reconcile the two latter studies, further standardize the anatomic nomenclature, and refine the technical descriptions of the different procedures.
METHODS
Anatomic Nomenclature
The international anatomic nomenclature can be found in Terminologia Anatomica (TA)6,7 and should be used wherever it clearly applies. The widely used terms “anterior/posterior,” “deep/superficial,” and “internal/external” are confusing. These should be replaced respectively by ventral/dorsal, caudal/cranial, and medial/lateral.
The dorsolateral attachment of the cervix is known as the paracervix. This term should replace numerous other terms, including “cardinal ligament” or “Mackenrodt’s ligament” (it is not a ligament). However, the term “mesometrium,” including the anatomic parametrium and paracervix, is an accurate correlation with the term “mesorectum” (used in rectal cancer surgery) because it refers to the area at risk for discontinuous spread of cervical carcinoma. It has been associated with a functional view of cancer spread based on embryologic development, a concept that deserves consideration but remains hypothetical.8
Strict use of TA nomenclature is not necessarily applicable in surgical practice, in which different structures are created by surgical dissection and separated by artificially created spaces. We describe these as follows:
The “ventral parametrium” is defined after surgical opening and development of two surgical spaces: the vesicouterine and vesicovaginal septum medially and the medial paravesical space laterally. The medial paravesical space is developed medial to the lateral ligament of the bladder, which contains the umbilical and superior vesical arteries (Fig. S1). The medial vesical space differs from the lateral (Latzko) paravesical space, which is developed between the umbilical ligament and the external iliac vessels. The ventral parametrium can be surgically divided into two portions: one in the plane medial to the terminal ureter (vesicouterine ligament cranial to the ureter and vesicovaginal ligament caudal to the ureter) and the other lateral to the plane of the ureter. The bladder nerves run caudally and parallel to the ureter. Some Japanese authors refer to the vesicovaginal ligament as the “posterior leaf of the vesicouterine ligament.”9
The “dorsal parametrium” is a complex structure composed of the rectouterine and rectovaginal ligaments (rectal pillar) and the dorsal part of the pelvic autonomic nerves. A medial pararectal space (otherwise described as the sacrouterine space or Okabayashi space10) can be artificially created lateral to the rectal pillar and the mesorectum, medial to the autonomic nerves (Fig. S2), with the goal of preserving bladder innervation. The medial pararectal space differs from the Latzko pararectal space, which is developed between the rectum medially, the sacrum dorsally, and the internal iliac vessels laterally.
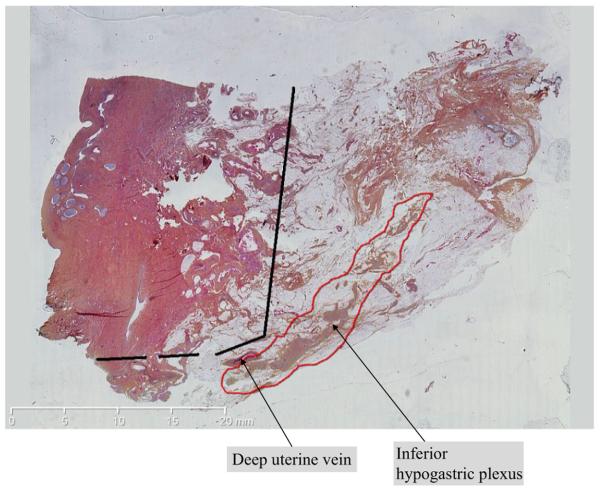
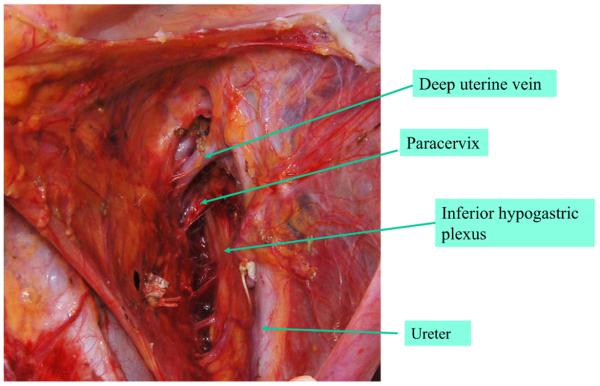
The term “lateral parametrium” refers to the paracervix. Therefore, we use both terms in this report. Notably, the structure empirically called paracolpos or paracolpium is included in the paracervix in the TA nomenclature because no border exists between lateral attachments of the cervix or the vagina. The paracervix is a complex structure with a heterogeneous anatomy that has an impact on surgical management (Figs. 1, S3). The paracervix contains the main blood and lymphatic vessels of the uterine cervix and comprises two parts: the medial part, which is more condensed and fibrous, and the lateral part, which is composed of soft lymph node-bearing fatty tissue surrounding vessels and nerves. The most stable anatomic landmark delineating the boundary between the two parts is the distal ureter (Fig. S1). The deep uterine vein invariably runs cranial and perpendicular to the hypogastric plexus (Fig. 2). However, the number of uterine veins may vary, and the deep uterine vein does not exactly represent the caudal limit of the paracervix. Figure 2 shows cellular paracervical tissue caudal to the deep uterine vein. The node-bearing tissue of the lateral part of the paracervix can be removed with preservation of the vessels and nerves as in any lymph node dissection. As stated by Palfalvi and Ungar,11 “the border between parametrial dissection and lymphadenectomy is artificial and can be located in different planes, but the same connective tissue is extirpated.” Unless gross disease is present, the question of how to excise the lateral part of the paracervix can be solved by the concept of parametrial node dissection.12,13
FIG. 1.
Paracervix showing deep uterine vein and inferior hypogastric plexus. Courtesy of Dr. Ghislaine Escourrou, University Hospital, Toulouse, France
FIG. 2.
Cellular yellow paracervical tissue caudal to the deep uterine vein (left side of pelvis)
Updating Process
We aimed to refine the principles and description of the different classes of radical hysterectomy defined in the Querleu–Morrow classification. All three authors independently examined the current literature and undertook a critical assessment of the original classification. Imaging and pathologic slides demonstrating different types of radical hysterectomy were examined. The Cibula 3-D concept,5 which has an impact on the definition of paracervical excision in the type C procedure described later, has been included in this update.
RESULTS
Proposed Updated Classification
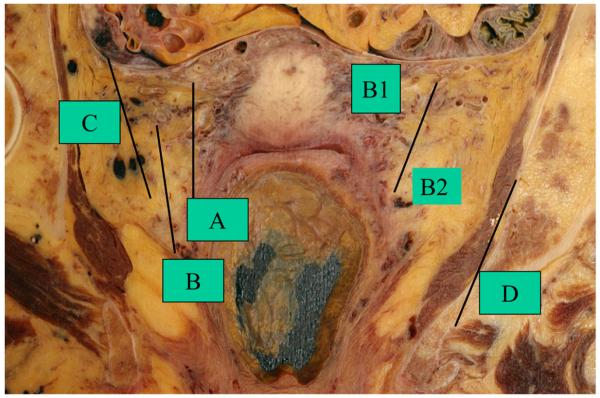
The Querleu–Morrow classification3 is based, for the purpose of simplification, on the lateral extent of resection only (Fig. 3). Stable anatomic landmarks, such as the crossing of the ureter with the uterine artery and paracervix, and the vascular plane of the internal iliac system are used to define the limits of resection.
FIG. 3.
Lateral extent of resection. Courtesy of Pr. Brigitte Mauroy, Institute of Anatomy, University of Lille, France. From Querleu and Morrow3
Type A: Limited Radical Hysterectomy
This tailored procedure (Fig. 4) is not accessible to general gynecologists without training in radical surgery. The goal of the operation is to ensure removal of the cervix in its entirety down to the vaginal fornix, together with a paracervical margin. This is crucial to the design of future trials testing the safety of reduced radicality. It can be used for (1) the management of selected low-risk IB1 invasive cervical cancers smaller than 2 cm with negative pelvic nodes, no deep stromal invasion, and no lymph-vascular space invasion and (2) the occasional completion surgery for advanced cervical cancers after radiation, chemotherapy, or both.
FIG. 4.
Specimen of resected paracervix. Right Type B. Left Type A
Existing evidence indicates that pelvic node involvement is a major independent predictor of parametrial involvement. This factor is not always identified at the time of surgery. However, in some centers, routine frozen section of sentinel nodes (or side-specific lymph node dissection when no sentinel nodes are detected on a given pelvic sidewall) is used as a decision tool, with excellent results.14 In other centers, tailoring is less practical. A less than radical surgery may be problematic if it is not known, with reasonable confidence, that the pelvic nodal status is negative.
Type A is not a simple “extrafascial” hysterectomy. The position of the ureters must be determined by direct visualization (after opening of the ureteral tunnels) at the time of abdominal or laparoscopic surgery or by palpation at the time of vaginal surgery. The uterine pedicles can be transected at their crossing with the ureter, as in the original Wertheim operation, or at their origin. The paracervix is transected medial to the ureter but lateral to the cervix. The paracervix is excised halfway between the ureter and the cervix and caudally parallel to the cervix until the lateral vaginal fornix is reached and opened. Kinking or thermal injury of the distal ureter (related to the en bloc use of heat-generating devices) is a concern because the ureter is not fully mobilized. The rectovaginal ligaments and the vesicouterine ligaments are defined, then divided at a distance from the uterus, but not at the rectum or bladder. This involves an approximate 5-mm resection of the corresponding ligaments. No removal of the vaginal part of the paracervix (paracolpos) is involved. Vaginal resection is minimal, routinely less than 10 mm.
Obtaining a free exocervical margin without any invasive or preinvasive disease is a major objective of surgery in the setting of early cervical cancer. Although colpectomy may constitute overtreatment in some cases, without it there is a risk of involved margins or even incomplete resection of the cervical stroma. However, patients with preoperative in sano cone biopsy could be spared colpectomy.
Our goal is to define a new surgical option (i.e., “minimal radical surgery”), which is a smaller operation than the standard modified radical hysterectomy (type B, described in the next section), but a larger operation than a simple or extrafascial hysterectomy/trachelectomy. In general, we do not recommend any specific type of surgical radicality for every clinical situation. Although the trend toward conservative surgery in the setting of early cervical cancer may be justified, to date, no definitive evidence ensures that “simple” procedures are safe. Furthermore, we are concerned about disseminating the idea that early cervical cancer can be managed using a common, non-radical procedure. We fear that this may lead to suboptimal surgeries without adequate preoperative staging in non-specialized settings.
Type B: Resection of the Paracervix at the Ureter
This operation (Figs. 4, S4) includes two subtypes: types B1 and B2. Type B1 is the “modified” radical hysterectomy. The ureter is unroofed and mobilized laterally, permitting transection of the paracervix at the level of the ureteral tunnel.
The caudal limit must not involve the inferior hypogastric plexus (Fig. S4). Partial resection of the uterosacral peritoneal fold of the rectouterine ligament (dorsal parametrium) and the vesicouterine (ventral parametrium) ligament also is a standard component of this resection. Approximately 10 mm of the vagina from the caudal edge of the cervix or tumor is resected, without intent to radically resect the paravaginal tissues. The vesicovaginal ligament is not resected. As a result, the bladder nerves, which run within the vesicovaginal ligament caudal to the ureter and lateral to the vaginal fornix, are not at risk. The radicality of this operation can be increased without increasing the risk of hypogastric nerve injury.
Although the type B1 procedure does not involve resecting the nodes of the lateral part of the paracervix, a paracervical lymphadenectomy can be added to increase the radicality of node dissection. This results in a type B2 resection. Combined with pelvic lymphadenectomy, type B2 surgeries aim to remove the pelvic nodes as completely as possible. In this context, resection of the nodes located caudal to the obturator nerve and cranial to the sciatic nerve is part of the additional paracervical lymphadenectomy.
Adding a lateral paracervical nodal dissection to a proximal-type radical hysterectomy improves lateral radicality without increasing morbidity.8,12,13 The gluteal and pudendal nodes, which are caudal and lateral to the iliac vessels, are included in the template. The procedure may be refined by the use of indocyanine green navigation, which allows the surgeon to identify the lymph vessel and lymph node component of the paracervix more clearly.15
The goal is to incorporate recent developments associated with the use of ICG navigation, as published by others. We do not take sides in this regard because our objective is to make the proposed classification system adaptable to recent surgical variations.
Type C: Transection of the Paracervix at Its Junction with the Internal Iliac Vascular System
This operation corresponds to the classical radical hysterectomy. It is adapted to International Federation of Gynecology and Obstetrics (FIGO) stage IB1 lesions with deep stromal invasion and IB2-2A or early 2B cervical cancers. The lateral border is defined as the medial aspect of the internal iliac artery and vein.
Transection of the rectovaginal and rectouterine ligaments is performed at the rectum. Transection of the ventral parametrium ligament is performed at the bladder. Both the vesicouterine and vesicovaginal ligaments are resected. The ureter is completely mobilized and lateralized. The length of the vaginal cuff is adjusted to the vaginal extent of the tumor.
In type C procedures, the decision about autonomic nerve preservation is crucial. Two subcategories are defined in the following sections.
Type C1: Nerve-preserving Radical Hysterectomy
The dorsal parametrium is transected after the dorsal segment of the autonomic nerve system has been separated (Fig. S2). The inferior hypogastric plexus is systematically identified and preserved by transecting only the uterine branches of the pelvic plexus at the time the lateral parametrium is transected. Ventrally, the bladder branches of the pelvic plexus are preserved in the vesicovaginal ligament. Then, only the medial part of the ventral parametrium is resected, and the bladder branches of the hypogastric plexus caudal to the course of the ureter are identified and preserved.
Type C2: No Preservation of Autonomic Nerves
The paracervix is completely transected. The inferior hypogastric plexus, together with the sacral splanchnic nerves, is divided lateral to the rectum. Type C2 requires a complete dissection of the ureter from the ventral parametria (vesicovaginal ligament). The ventral parametria are resected at the level of the bladder wall (Fig. S5). Bladder branches of the hypogastric plexus are sacrificed, so it is not necessary to identify them. Laterally, the resection continues alongside the medial aspect of the internal iliac vessels down to the pelvic floor.
The medial pararectal (sacrouterine), lateral pararectal, and lateral paravesical spaces are unified by transecting the pelvic attachment of the paracervix together with the splanchnic nerves in the caudal part (Fig. S6). Parts of the vaginal component of the paracervix (paracolpium) are removed. The removal of the dorsal parametrium is extended caudally to the sacral attachment.
Type C is the standard operation for bulky or high-risk tumors. Type C1 has become the mainstay. Type C2 can be justified only for anatomic reasons.
Type D: Laterally Extended Resection
These less common surgeries feature additional ultra-radical procedures, in which structures lateral to the paracervix are resected. Two subtypes are described in the following sections.
Type D1: Resection of the Entire Paracervix at the Pelvic Sidewall Together With the Hypogastric and Obturator Vessels, Exposing the Roots of the Sciatic Nerve. The resection plane is lateral to the internal iliac vessels, interrupting branches of gluteal superior, gluteal inferior, and pudendal vessels. This procedure corresponds to the Palfalvi–Ungar laterally extended parametrectomy11 and may be used for stage 2B tumors.
Type D2: D1 Plus Resection of the Adjacent Fascial/Muscular Structures. These structures include, when necessary, the obturator fascia and obturator muscle ventrally, the coccygeus muscle and pelvic part of the piriformis muscle dorsally, and the sacrospinous ligament and acetabulum laterally. This procedure corresponds to the laterally extended endopelvic resection described by Höckel.16 It usually is performed for laterally recurrent tumors as a separate procedure.
Table 1 defines the different classes of radical hysterectomy.
TABLE 1.
Summary of the main landmarks in each type of radical hysterectomy on each part of the parametria
| Dimension Type of radical hysterectomy |
Paracervix or lateral parametrium | Ventral parametrium | Dorsal parametrium |
|---|---|---|---|
| A | Halfway between the cervix and ureter (medial to the ureter–ureter identified but not mobilized) |
Minimal excision | Minimal excision |
| B1 | At the ureter (at the level of the ureteral bed–ureter mobilized from the cervix and lateral parametrium) |
Partial excision of the vesicouterine ligament | Partial resection of the rectouterine-rectovaginal ligament and uterosacral peritoneal fold |
| B2 | Identical to B1 plus paracervical lymphadenectomy without resection of vascular/nerve structures |
Partial excision of the vesicouterine ligament | Partial resection of the rectouterine-rectovaginal ligament and uterosacral fold |
| C1 | At the iliac vessels transversally, caudal part is preserved |
Excision of the vesicouterine ligament at the bladder. Proximal part of the vesicovaginal ligament (bladder nerves are dissected and spared) |
At the rectum (hypogastric nerve is dissected and spared) |
| C2 | At the level of the medial aspect of iliac vessels completely (including the caudal part) |
At the bladder (bladder nerves are sacrificed) | At the sacrum (hypogastric nerve is sacrificed) |
| D | At the pelvic wall, including resection of the internal iliac vessels and/or components of the pelvic sidewall |
At the bladder. Not applicable if part of exenteration | At the sacrum. Not applicable if part of exenteration |
DISCUSSION
The popular Piver–Rutledge–Smith classification,17 published in 1974, describes five classes of radical hysterectomy. The original paper does not refer to clear anatomic landmarks and international anatomic definitions. Excessive vaginal resections, from one third to three fourths of the vagina, are included in some templates. Class 1 is not a radical hysterectomy, and class 5 is no longer used. The rationale and anatomy differentiating classes 3 and 4 are not clear. Finally, the Piver–Rutledge–Smith classification applies only to open surgery and was developed at a time when minimally invasive and fertility-sparing operations did not exist. It fails to take into account the concept of nerve preservation and ignores the vaginal approach.
An interesting tumor-node-metastasis (TNM)-like description of the operation that defines three classes of radicality in all directions has been developed.18 However, the model results in 91 possible subtypes.
Two metrics define the outcomes of radical hysterectomy: (1) adverse effects such as bladder and rectal dysfunction and (2) the curative effect of the surgery. The more extensive the surgery is, the higher the risk of complications. However, small surgeries may undertreat high-risk tumors, whereas big surgeries may overtreat low-risk tumors. The Querleu–Morrow classification provides a simple and universal tool for assigning different levels of radicality to a limited number of categories. Some surgeries may be asymmetric. The same classification applies to fertility-sparing surgeries (type B, as in the Dargent operation, and type A in new variants adapted to minimal disease or after neoadjuvant chemotherapy).
Because it is impossible to describe all variations of these procedures, the use of a simple classification system does not preclude a careful description of any single operation. The list of required information should be a component of quality control in the surgical management of cervical cancers. The following items should appear in the operative report:
All components defining the type of radical hysterectomy. The management of the lateral, ventral, and dorsal attachments of the cervix must be described.
Mode of management of the uterine artery, which is routinely divided at its origin from the internal iliac artery but may be divided at the ureter in type A (management of the adjacent lymph node-bearing tissue).
Assessment of the surgical and pathologic length of the lateral extent of the resection. The surgical length should be measured on the fresh specimen without stretching. The pathologic length should be measured after fixation. However, the ventral and dorsal dimensions are difficult to assess. Measurements should be taken independently by someone other than the surgeon.
The surgical and pathologic minimum length of vagina removed and, when applicable, the minimum distance between the tumor and the margin of resection. Again, measurements should be taken independently on the fresh specimen, without stretching, after fixation.
In fertility-preserving surgery, information regarding the pathologic distance between the tumor and the endocervical resection margin.
The manner in which hemostasis is achieved also must be described to evaluate the impact of new techniques or devices on radicality and outcome, such as blood loss or complication rates. Notably, it has been demonstrated that the achievement of lateral resection is dependent on hemostasis technique. This highlights the importance of technical improvements, irrespective of classification.19 A precise description of technique should appear in the operative report.
CONCLUSION
Radical hysterectomy is not a single operation. The variations of this procedure must balance curative effects with the risk of adverse consequences. An internationally accepted classification system of radical hysterectomy that will be accepted and used by individual surgeons, study groups, and national and international societies is clearly needed. Evaluation of techniques and quality control should be a basic component of every surgical activity.
To date, no evidence exists to support any recommendation regarding the distance from central tumor to margins. Only one randomized, controlled study has compared less extensive primary surgeries with more extensive primary surgeries in terms of morbidity, overall and disease-free survival, and relapse.20 However, the study was underpowered to detect differences in outcomes for different stages and substages of early cervical cancer. In addition, a substantial proportion of the patients had undergone adjuvant radiation therapy, thus contradicting the generally accepted principle that patients should be spared the discomfort and potential complications associated with combined surgery and radiation therapy.
The most precise indicator of the risk of occult lymphatic involvement of pericervical structures, including the paracervix and the ventral and dorsal parametria, is described in two studies of giant pathologic sections.21,22 These studies suggest that the risk of visceral lymph node involvement is associated with tumor size and stage, clearly supporting the concept that the extent of excision should increase, or widen, as stage and tumor size increase. However, both studies were based on specimens derived from type C operations. Neither study was designed to document the clinical use of less radical surgeries for low-risk cervical cancers.
Our proposed classification is not a guideline, but rather a standardized description of different surgeries performed worldwide, independent of underlying theoretical objectives or the surgeon’s choice of approach in individual cases. Two major objectives are constant: (1) excision of the central tumor with clear margins and (2) removal of any potential site of node metastasis. Future randomized studies designed to document the need for extended or reduced radicality in the surgical management of cervical cancer should be based on precise, universally accepted descriptions.
Supplementary Material
ACKNOWLEDGEMENT
This study was funded in part through the NIH/NCI Support Grant P30 CA008748 (Nadeem R. Abu-Rustum).
Footnotes
DISCLOSURE Denis Querleu received travel expenses for the 2014 IGCS meeting (Melbourne) from Karl Storz GmBH. He has consulted for Roche Inc. Other authors declares no conflicts of interest.
Electronic supplementary material The online version of this article (doi:10.1245/s10434-017-6031-z) contains supplementary material, which is available to authorized users.
REFERENCES
- 1.Landoni F, Bocciolone L, Perego P, Maneo A, Bratina G, Mangioni C. Cancer of the cervix, FIGO stages IB and IIA: patterns of local growth and paracervical extension. Int J Gynecol Cancer. 1995;5:329–34. [DOI] [PubMed] [Google Scholar]
- 2.Kinney WK, Hodge DO, Edward V, Egorshin MD, Ballard DJ, Podratz KC. Identification of a low-risk subset of patients with stage IB invasive squamous cancer of the cervix possibly suited to less radical surgical treatment. Gynecol Oncol. 1995;57:3–6. [DOI] [PubMed] [Google Scholar]
- 3.Querleu D, Morrow CP. Classification of radical hysterectomy. Lancet Oncol. 2008;9:297–300. [DOI] [PubMed] [Google Scholar]
- 4.NCCN Clinical Practice Guidelines in Oncology: Cervical Cancer. Version 1 2017. Accessed 19 October 2016 at NCCN.org. [Google Scholar]
- 5.Cibula D, Abu-Rustum NR, Benedetti-Panici P, Köhler C, Raspagliesi F, Querleu D, Morrow CP. New classification system of radical hysterectomy: emphasis on a three-dimensional anatomic template for parametrial resection. Gynecol Oncol. 2011;122:264–8. [DOI] [PubMed] [Google Scholar]
- 6.Whitmore I. Terminologia anatomica: new terminology for the new anatomist. Anat Rec. 1999;257:50–3. [DOI] [PubMed] [Google Scholar]
- 7.Ercoli A, Delmas V, Fanfani F, Gadonneix P, Ceccaroni M, Fagotti A, et al. Terminologia Anatomica versus unofficial descriptions and nomenclature of the fasciae and ligaments of the female pelvis: a dissection-based comparative study. Am J Obstet Gynecol. 2005;193:1565–73. [DOI] [PubMed] [Google Scholar]
- 8.Höckel M, Horn LC, Fritsch H. Association between the mesenchymal compartment of uterovaginal organogenesis and local tumor spread in stage IB-IIB cervical carcinoma: a prospective study. Lancet Oncol. 2005;6:751–6. [DOI] [PubMed] [Google Scholar]
- 9.Fujii S, Tanakura K, Matsumura N, Higuchi T, Yura S, Mandai M, Baba T. Precise anatomy of the vesico-uterine ligament for radical hysterectomy. Gynecol Oncol. 2007;104:186–91. [DOI] [PubMed] [Google Scholar]
- 10.Yabuki Y, Asamoto A, Hoshiba T, Nishimoto H, Satou N. A new proposal for radical hysterectomy. Gynecol Oncol. 1996;62:370–8. [DOI] [PubMed] [Google Scholar]
- 11.Palfalvi L, Ungar L. Laterally extended parametrectomy (LEP), the technique for radical pelvic sidewall dissection: feasibility, technique, and results. Int J Gynecol Cancer. 2003;13:914–7. [DOI] [PubMed] [Google Scholar]
- 12.Höckel M, Konerding MA, Heussel CP. Liposuction-assisted nerve-sparing extended radical hysterectomy: oncologic rationale, surgical anatomy, and feasibility study. Am J Obstet Gynecol. 1998;178:971–6. [DOI] [PubMed] [Google Scholar]
- 13.Querleu D, Narducci F, Poulard V, Lacaze S, Occelli B, Leblanc E, Cosson M. Modified radical vaginal hysterectomy with or without laparoscopic nerve-sparing dissection: a comparative study. Gynecol Oncol. 2002;85:154–8. [DOI] [PubMed] [Google Scholar]
- 14.Kyo S, Mizumoto Y, Takakura M, et al. Nerve-sparing abdominal radical trachelectomy: a novel concept to preserve uterine branches of pelvic nerves. Eur J Obstet Gynecol Reprod Biol. 2015;193:5–9. [DOI] [PubMed] [Google Scholar]
- 15.Kimmig R, Aktas B, Buderath P, Rusch P, Heubner M. Intra-operative navigation in robotically assisted compartmental surgery of uterine cancer by visualisation of embryologically derived lymphatic networks with indocyanine-green (ICG). J Surg Oncol. 2016;113:554–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Höckel M. Laterally extended endopelvic resection: surgical treatment of infrailiac pelvic wall recurrences of gynecologic malignancies. Am J Obstet Gynecol. 1999;180:306–12. [DOI] [PubMed] [Google Scholar]
- 17.Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstet Gynecol. 1974;44:265–72. [PubMed] [Google Scholar]
- 18.Trimbos JB. TNM-like classification of radical hysterectomy. Gynecol Oncol. 2009;113:397–8. [DOI] [PubMed] [Google Scholar]
- 19.Benedetti-Panici P, Scambia G, Baiocchi G, Maneschi F, Greggi S, Mancuso S. Radical hysterectomy: a randomized study comparing two techniques for resection of the cardinal ligament. Gynecol Oncol. 1993;50:226–31. [DOI] [PubMed] [Google Scholar]
- 20.Landoni F, Maneo A, Zapardiel I, Zanagnolo V, Mangioni C. Class I versus class III radical hysterectomy in stage IB1-IIA cervical cancer: a prospective randomized study. Eur J Surg Oncol. 2012;38:203–9. [DOI] [PubMed] [Google Scholar]
- 21.Girardi F, Lichtenegger W, Tamussino K, Haas J. The importance of parametrial lymph nodes in the treatment of cervical cancer. Gynecol Oncol. 1989;34:206–11. [DOI] [PubMed] [Google Scholar]
- 22.Benedetti-Panici P, Maneschi F, D’Andrea G, et al. Early cervical carcinoma: the natural history of lymph node involvement redefined on the basis of thorough parametrectomy and giant section study. Cancer. 2000;88:2267–74. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.