Abstract
Objective
To examine the association between caregiver proxy report of executive function (EF) and dysregulated eating behavior in children with obesity.
Methods
Participants were 195 youth with obesity aged 8–17 years, and their legal guardians. Youth height, weight, demographics, depressive symptoms, eating behaviors, and EF were assessed cross-sectionally during a medical visit. Analyses of covariance, adjusted for child age, gender, race/ethnicity, standardized BMI, depressive symptoms, and family income were used to examine differences in youth EF across caregiver and youth self-report of eating behaviors.
Results
Youth EF differed significantly by caregiver report of eating behavior but not youth self-report. Post hoc analyses showed that youth with overeating or binge eating had poorer EF than youth without these eating behaviors.
Conclusions
Executive dysfunction, as reported by caregivers, in youth with obesity may be associated with dysregulated eating behaviors predictive of poor long-term psychosocial and weight outcomes. Further consideration of EF-specific targets for assessment and intervention in youth with obesity may be warranted.
Keywords: adolescents, children, eating and feeding disorders, health behavior, obesity, neuropsychology, parents
Introduction
Pediatric obesity remains one of the leading preventable health problems in the United States because of epidemic levels in youth (Ogden et al., 2016) and consequent health and financial burdens (Finkelstein, Graham, & Malhotra, 2014; Reilly et al., 2003). The leading evidence-based intervention for pediatric obesity is family-based behavioral treatment, which involves dietary and activity modification with the support of behavioral skills (e.g., goal-setting, problem-solving, and self-monitoring) to improve weight status (Janicke et al., 2014). Clinically meaningful improvements in weight status have been observed in up to two-third of youth who complete these interventions (Epstein, Paluch, Roemmich, & Beecher, 2007; Reinehr et al., 2016); however, at least one-third of the youth do not achieve meaningful weight outcomes (Epstein et al., 2007). This substantial variability in treatment response warrants further examination to identify potentially modifiable factors that might contribute to poorer outcomes.
Children with overweight or obesity tend to have impairments in executive function (EF) (Nederkoorn, Braet, Van Eijs, Tanghe, & Jansen, 2006; Reinert, Po'e, & Barkin, 2013) or problems regulating behavior and emotion (i.e., behavioral regulation) and thought processes (i.e., metacognition). EFs undergo periods of rapid development during childhood and continue maturing into adolescence (Anderson, 2002). Thus, EF development can be vulnerable to a range of internal and external stressors during childhood, including obesity and its comorbidities, as well as other factors such as socioeconomic risk (Miller, Lee, & Lumeng, 2015; Rhoades, Greenberg, Lanza, & Blair, 2011). Deficits in EF commonly associated with pediatric obesity include impulsivity and poor inhibitory control, impaired working memory, and poor cognitive flexibility (Liang, Matheson, Kaye, & Boutelle, 2014; Reinert et al., 2013). Children with EF deficits, particularly impulsivity, have poorer weight outcomes in pediatric behavioral obesity treatment programs (Braet, 2006; Nederkoorn, Jansen, Mulkens, & Jansen, 2007). Various studies have investigated the associations between EF and weight-related behaviors, such as eating and physical activity patterns, which can help us better understand why children with EF impairments may be less likely to achieve more optimal weight outcomes in behavioral obesity treatment programs (Davis et al., 2011; de Groot, van den Akker, Rings, Delemarre-van de Waal, & van der Grond, 2016; Groppe & Elsner, 2015). The association between EF and eating behaviors may be a promising avenue of research, given that (1) dysregulated eating behaviors have a demonstrated impact on body mass index (BMI), excess weight gain, and psychosocial health (Goldschmidt, Aspen, Sinton, Tanofsky-Kraff, & Wilfley, 2008; Tanofsky-Kraff et al., 2011); and (2) EF may be modifiable in childhood and adolescence through targeted intervention (Davis et al., 2011; Verbeken, Braet, Goossens, & van der Oord, 2013).
In the context of obesity, two dysregulated eating behaviors that are more commonly observed or reported include overeating and binge eating (BE). Episodic overeating (EO) can be defined as eating an abnormally large amount of food within a short period of time (e.g., 2 hr), whereas BE includes the experience of loss of control over eating (LOC) with EO. Overeating has been associated with impulsivity and poor psychological health in children (Nederkoorn et al., 2006). However, a body of literature has emerged that emphasizes the importance of LOC in predicting psychological and weight outcomes in children (Tanofsky-Kraff et al., 2009; Tanofsky-Kraff et al., 2011). Further, there has been debate about whether LOC, regardless of overeating, is a more salient marker of eating pathology severity, as well as poorer weight and psychological outcomes (Goldschmidt et al., 2015b; Shomaker et al., 2010). Problems with EF, particularly emotional dysregulation, have been associated with LOC (Goldschmidt, Lavender, Hipwell, Stepp, & Keenan, 2016a; Goossens, Braet, Van Vlierberghe, & Mels, 2009). Moreover, EF predicted BMI changes in a large community-based sample of girls, and BE mediated this relationship such that girls with poorer planning and greater impulsivity were more likely to binge eat and subsequently gain excess weight (Goldschmidt, Hipwell, Stepp, McTigue, & Keenan, 2015a). When examining EF and weight-related problems in the context of obesity, similar findings have emerged. A recent study showed associations between unhealthy eating attitudes/behaviors and affective, behavioral, and cognitive dysregulation in adolescents and young adults with severe obesity (Gowey et al., 2016).
Research investigating the associations between EF and eating behavior in youth with obesity is growing; yet, there are still limitations to be addressed. Extant studies have often relied on limited measurements of eating and EF, such as single informant report of eating behaviors or specific domains of EF (Goldschmidt et al., 2015a; Maayan, Hoogendoorn, Sweat, & Convit, 2011). Yet, the high rate of child–caregiver disagreement on reports of disordered eating (Johnson, Grieve, Adams, & Sandy, 1999; Steinberg et al., 2004) suggests that a multiinformant method likely remains the most useful approach. Furthermore, various domains of EF have been associated with obesity and obesity-related behaviors in youth; yet, studies have used different measures, samples, and protocols; thus, it remains a challenge to consolidate and generalize these findings to provide a comprehensive understanding of the EF–eating behavior association in pediatric obesity. In summary, the current literature is largely limited by single-informant report of youth eating behavior and nonuniform measurement of EF. Thus, we proposed to address these limitations and build on extant literature of EF and eating behavior in youth with obesity by using a multiinformant measure of eating behavior and a validated, highly used measure of EF in a sample including a wide pediatric age range of ethnically/racially diverse youth. Specifically, the aim of the current study was to examine the association between caregiver proxy-reported EF (i.e., behavioral regulation and metacognition) and dysregulated eating behaviors per caregiver and self-report in a clinical sample of 8–17-year-olds with obesity. Based on previous studies (Goldschmidt et al., 2015a; Nederkoorn et al., 2006), we hypothesized that youth who experienced EO or BE (per self-report or caregiver report) would have poorer behavioral regulation and metacognition than those who did not experience dysregulated eating. Moreover, based on past findings that BE may be distinctly related to EF impairment via LOC (Goldschmidt et al., 2015a; Tanofsky-Kraff et al., 2011), we hypothesized that youth who exhibited BE would have poorer EF than youth who exhibited overeating without LOC.
Methods
Participants
The current sample included 195 youth between the ages of 8 and 17 years and their legal guardians. All youth had a BMI ≥85th percentile for age and gender norms published by the Centers for Disease Control and Prevention (CDC) (Kuczmarski et al., 2000), which is considered indicative of overweight or obesity. Youth were attending a regularly scheduled appointment at a primary care or specialty obesity clinic and accompanied by a legal guardian/caregiver. Exclusion criteria included children diagnosed with intellectual disability, psychotic disorder, or short stature, and children or accompanying guardians who did not speak and read English. Eligible families were approached by a physician or trained member of the research team in a private room to determine caregiver and child interest in research participation. Informed consent/assent were obtained from willing children and caregivers. Questionnaires were completed independently by youth and caregivers in ∼20–30 min. Families were compensated for their time and participation. The study was approved by the governing institutional review board.
Measures
Demographic Information
Caregivers completed a demographic questionnaire to report child age, gender, and race/ethnicity, as well as caregiver age, gender, height, weight, and family income. Caregiver BMI (kg/m2) was calculated using his/her self-reported height and weight.
Anthropometric Data
Youth height and weight were measured by trained medical staff at the clinic visit and obtained from the medical chart. Standardized BMI (zBMI) and BMI percentiles were derived from CDC norms adjusted for age and gender (Kuczmarski et al., 2000).
Depressive Symptoms
The Children’s Depression Inventory Short form (CDI:S) is a self-report screening instrument for depressive symptoms and severity in youth (Kovacs, 2003). Depressive symptoms/disorders have been associated with EF impairment (Wagner, Muller, Helmreich, Huss, & Tadic, 2015) and eating behavior in youth with obesity (Mooreville et al., 2014) and, thus, were included as a covariate in statistical models. The CDI:S has been validated for 7–17-year-olds and includes 10 items from the original 27-item CDI (Kovacs, 1992). Each item is associated with three response options, scored or reverse-scored as 0, 1, or 2 (highest severity), and converted into standardized T-scores based on age and gender. T-scores have a mean of 50 and a SD of 10. A score of ≥65 is considered indicative of potentially clinically significant depressive symptoms. The CDI:S has been recommended for use in time-limited pediatric settings and has demonstrated similar validity to the CDI in medically ill children (Allgaier et al., 2012; Kovacs, 2003). Cronbach’s alpha for the current sample was 0.84.
Executive Function
The Behavior Rating Inventory of Executive Function (BRIEF) (Gioia, Isquith, Guy, & Kenworthy, 2000) is an 86-item caregiver/parent-report measure that assesses impairment of EF in 5–18-year-olds. Caregivers/parents rate their children’s behaviors over the past 6 months on a 3-point Likert scale (Never, Sometimes, and Often). The BRIEF parent-report form scoring system produces a Global Executive Composite, two main indices (Behavioral Regulation Index, BRI, and Metacognition Index, MI), and eight clinical subscales of EF domains. The BRI and MI scores are used as primary outcomes in the current study because of interest in examining core EF domains and to reduce the number of statistical analyses. The BRI is a composite of three clinical subscales (Inhibit, Shift, and Emotional Control), while the MI is a composite of the remaining five scales (Initiate, Working Memory, Plan/Organize, Organization of Materials, and Monitor). To obtain an index score, the sum of the raw items of the scales within that index is taken. Higher scores indicate greater executive dysfunction. Corresponding T-scores and percentiles based on age and gender are assigned using raw scores. A score of ≥65 on any scale or index suggests potential clinical impairment (Gioia et al., 2000). The BRIEF has been validated for use with healthy and clinical pediatric populations. Internal consistency ratings have ranged from .82 to .98 with interrater reliability ratings ranging from .72 to .84 (Gioia et al., 2000; Mahone et al., 2002). The BRI and MI have Cronbach’s alphas in the current sample of 0.95 and 0.96, respectively.
Eating Behaviors
The Questionnaire of Eating and Weight Patterns-Adolescent (QEWP-A) and Questionnaire of Eating and Weight Patterns-Parent measures (Johnson et al., 1999) were used to assess youth dysregulated eating episodes over the past 6 months. The QEWP includes 12 items regarding eating and weight-related behavior, several of which include follow-up items if endorsed. Item response options are either “yes” or “no” format or rated on a Likert scale for frequency or intensity. Parent and adolescent forms are similar with slight wording changes to reflect perspective and developmental level. Responses and scoring protocol allow youth to be classified as experiencing no episode of dysregulated eating (NE; no dysregulated eating behavior), EO (ate an unusually large amount of food within short time period), nonclinical binge eating (NCB; overeating + LOC), or binge eating disorder (BED; overeating + LOC + related distress + average occurrence ≥2 days per week + at least three of six DSM-IV-associated characteristics) (Nangle, Johnson, Carr-Nangle, & Engler, 1994; Spitzer et al., 1993). Compensatory behavior was assessed including self-induced vomiting and laxative, diuretic, diet pill, or other supplement use to prevent weight gain after BE to differentiate bulimic behavior (BB) from the previously characterized types of dysregulated eating. In this study, eating episode categories were considered mutually exclusive and hierarchical, such that an individual could only be identified as belonging to one group that represented the most or highest severity of dysregulated eating symptoms endorsed. Dysregulated eating episode groups from highest to lowest symptoms/severity include: BB, BED, NCB, EO, and NE. The BB group was excluded from primary statistical analyses because of low frequency. For statistical reasons related to group size, the NCB and BED groups were combined and considered more broadly as BE in those contexts. The QEWP-A has adequate concurrent validity and moderate stability (Johnson et al., 1999; Johnson, Kirk, & Reed, 2001).
Statistical Analysis
All statistical analyses were conducted using SPSS 23.0 for Windows (IBM Corporation, 2015). Analyses were performed on a sample of 195 caregiver–child dyads. There were eight participants (6.2%) missing one or more scales from the BRIEF. The SPSS HOTDECK macro (Myers, 2011) was used for multiple imputation to address missing values. Descriptive statistics including means, SDs, and frequencies were used to characterize the sample. The BRI and MI variables were log-transformed to correct positive skewness. Youth who engaged in compensatory (bulimic) behavior per self-report (n = 8) or caregiver report (n = 16) were excluded from relevant analyses. Analyses of covariance were conducted to examine whether EF differed across dysregulated eating behaviors (NE, EO, and BE). Covariates of relevance based on extant literature were included in all analyses. Bonferroni-adjusted post hoc comparisons were conducted to examine EF differences between groups exhibiting different eating behaviors (NE vs. EO; NE vs. BE; and EO vs. BE).
Results
Descriptive Data
Descriptive characteristics of the sample are displayed in Table I. The sample consisted of 8–17-year-olds who were primarily female. Approximately half of the sample identified as non-Hispanic Caucasian, one-third as non-Hispanic African-American, and the remainder as Hispanic or Latino, Mixed, Asian, Asian-American, or Other. The majority of children (87.69%) had obesity (≥95th BMI percentile). Child self-report of depressive symptoms on the CDI:S was considered in the typical range (Kovacs, 2003) for most youth, although a small subset of the sample (8.72%) endorsed clinically significant levels of depressive symptoms, which is consistent with other studies that identified up to 7–13% of similar-aged children with obesity who had depressive symptom scores indicative of potential clinical significance (Hannon et al., 2014; Mooreville et al., 2014). The majority of caregivers were females in their 30s and 40s with overweight or obesity (88.69%; BMI ≥ 25 kg/m2). Family income ranged from <$20,000 to >$80,000 with a median range of $20,000–$29,000.
Table I.
Sample Characteristics (N = 195)
| Child characteristics | M ± SD (%) |
|---|---|
| Age | 12.97 ± 2.47 |
| Female | 60.00% |
| Race/ethnicity | |
| Non-Hispanic Caucasian | 48.21% |
| Non-Hispanic African-American | 33.85% |
| Hispanic | 8.72% |
| Mixed race | 7.69% |
| Asian, Asian-American, and Other | 1.54% |
| BMI | 33.91 ± 7.86 |
| Percentile (BMI%) | 97.81 ± 2.63 |
| Z-score (zBMI) | 2.23 ± 0.44 |
| CDI:S depressive symptoms T-scorea | 47.93 ± 9.33 |
| Caregiver characteristics | |
| Age | 41.80 ± 9.20 |
| Female | 93.85% |
| BMI | 34.27 ± 7.92 |
| Family income | |
| <$20,000 | 37.44% |
| $20,000–39,999 | 30.26% |
| $40,000–59,999 | 14.87% |
| $60,000–79,999 | 6.15% |
| >$80,000 | 11.28% |
T-scores (M = 50, SD = 10) ≥65 are clinically significant.
BMI = body mass index; CDI:S = Children’s Depression Inventory Short form; zBMI = standardized BMI.
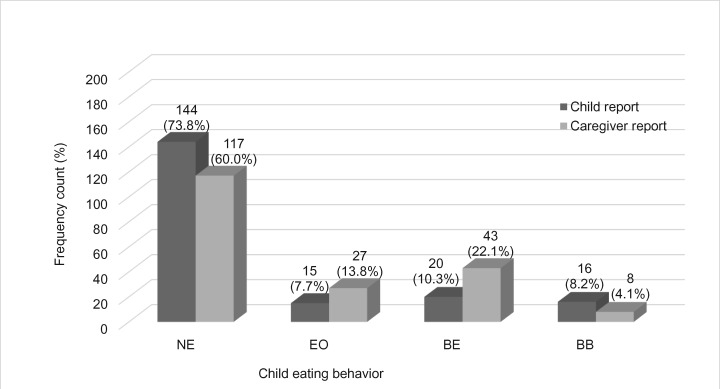
Descriptive data for EF are reported in Table II. Caregiver proxy report on the BRIEF suggested that nearly 30% of children and adolescents in the sample exhibited clinically significant executive dysfunction in everyday life, with comparable functioning across domains of behavioral regulation and metacognition. Figure 1 presents caregiver proxy and youth self-report of eating behavior. Almost three quarters of youth indicated that they did not experience any dysregulated eating episodes. However, responses of a smaller group of children (∼8%) indicated EO, with 1 in 10 youth reporting BE. Within this group, BED was not common per youth responses (n = 4; 2%). Caregiver reports of youth dysregulated eating episodes were higher. While over half of caregivers indicated that their children did not exhibit any dysregulated eating, 40% reported some type of dysregulated eating in their child. They reported observing almost double the rates of EO (14%) and BE (22%) that their children did. However, BED was rarely reported (n = 4; 2%), and these occurrences were not the same cases as those reported by children.
Table II.
Descriptive Data for Caregiver Proxy Report of Child Executive Functioning (N = 195)
| Child domain | M ± SD | Clinically impaired (%) |
|---|---|---|
| Global EF T-scorea | 57.25 ± 13.10 | 27.69 |
| Behavioral regulation T-scorea | 56.89 ± 13.82 | 27.69 |
| Metacognition T-scorea | 57.23 ± 13.03 | 29.74 |
T-scores (M = 50, SD = 10) ≥65 are clinically significant.
Note. Higher scores indicate poorer EF. EF = executive functioning.
Figure 1.
Child and caregiver reports of youth eating behavior.
Note. NE = no episode; EO = episodic overeating; BE = binge eating; BB = bulimic/compensatory behavior.
Cohen kappa statistics were calculated to estimate interrater agreement between children/adolescents and caregivers on eating behavior reporting. Kappa statistics range from 0 (poor agreement) to 1 (perfect agreement) (Landis & Koch, 1977). Together, children and adolescents (N = 195) had slight agreement with caregivers (kappa=.16) on their eating behavior. When examining children and adolescents separately in terms of their agreement with caregivers on eating behavior, both children (aged 8–11 years; N = 65) and adolescents (aged 12–17 years; N = 130) had slight agreement with caregivers (child–caregiver kappa=.18; adolescent–caregiver kappa=.15).
There was a general increase in zBMI across eating behavior groups. However, these differences were most salient for the BE (NCB) group. Specifically, zBMI of the NCB group [M (SE) = 2.46 (.065)] was significantly higher than the EO group [M (SE) = 2.14 (.082), p = .003] and the NE group [M (SE) = 2.16 (.039), p < .001], whereas there were no significant differences in zBMI between the EO and NE group.
Primary Analyses: Executive Function Differences Across Youth Eating Behavior per Caregiver and Self-Report
Analysis of covariance (ANCOVA) was conducted to examine differences in caregiver proxy report of EF between children who exhibited BE, EO, or no dysregulated eating behavior. Child age, gender, race/ethnicity, zBMI, depressive symptoms, and family income were included as covariates in all models. Results of the ANCOVAs examining child EF and eating behavior reported by caregivers and children are displayed in Tables III and IV, respectively.
Table III.
Analysis of Covariance Results of Differences in Executive Function Across Eating Behavior Groups Per Caregiver Proxy Report
| Caregiver proxy report (QEWP-P) | No episode |
Episodic overeating |
Binge eating |
F(2, 178) | p | ηp2 | R2 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |||||
| Behavioral regulation | 52.63 | 11.22 | 60.37 | 14.68 | 64.53 | 14.64 | 14.12 | <.001 | .14 | .19 |
| Metacognition | 53.67 | 11.12 | 59.26 | 12.71 | 64.30 | 14.52 | 9.55 | <.001 | .10 | .19 |
Note. Covariates in each analysis include child age, gender, race/ethnicity, zBMI, depressive symptoms, and family income.
QEWP-P = Questionnaire of Eating and Weight Patterns-Parent version.
Higher scores indicate poorer EF. Behavioral regulation and metacognition mean and SD scores derived from raw values to increase interpretability. Analyses of covariance were conducted using log-transformed data.
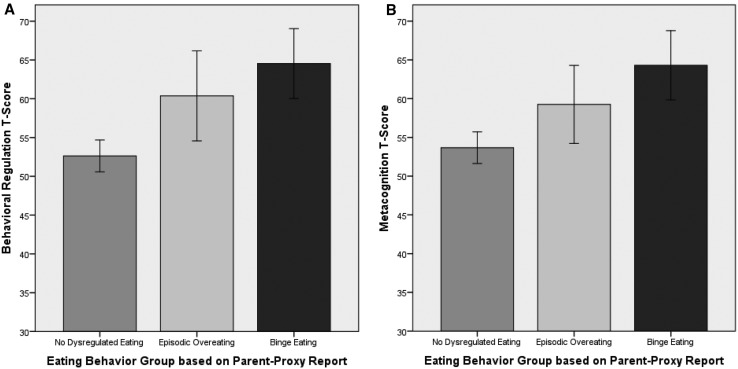
EF differed significantly based on caregiver proxy report of youth eating behavior (Table III). Specifically, per caregiver report, there was significant variation in behavioral regulation and metacognition across eating behavior groups. When examining the mean scores of each eating behavior group, a similar trend was observed for both EF domains. Children who exhibited BE in the sample had the highest mean scores (i.e., more problems with EF) for behavioral regulation and metacognition, respectively [M (SD) = 64.43 (14.64); M (SD) = 64.30 (14.52)], followed by children who engaged in EO [M (SD) = 60.37 (14.63); M (SD) = 59.26 (12.71)], and then NE [M (SD) = 52.63 (11.22); M (SD) = 53.67 (11.12)]. Significance tests for these between-group differences are described in the post hoc section below. The main effects of youth eating behavior on EF were generally small yet significant, where the adjusted models with caregiver-reported child eating behavior accounted for ∼19% of the variability in EF. Partial eta-squared estimates suggest that eating behaviors alone (unadjusted models) account for ∼13.7 and 9.7% of variability in behavioral regulation and metacognition, respectively.
Alternatively, no statistically significant differences in behavioral regulation or metacognition were identified based on youth self-report of eating behavior (Table IV). Although not statistically significant, similar mean score trends were observed for behavioral regulation and metacognition across type of self-reported eating behavior as those described earlier for caregiver-reported youth eating behavior. Children who self-reported BE had the highest EF scores, followed by children who reported EO, and finally, children who reported NE.
Table IV.
Analysis of Covariance Results of Differences in Executive Function Across Eating Behavior Groups Per Child Self-Report
| Child self-report (QEWP-A) | No episode |
Episodic overeating |
Binge eating |
F(2, 170) | p | ηp2 | R2 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |||||
| Behavioral regulation | 55.71 | 14.05 | 55.80 | 10.71 | 61.55 | 11.98 | 1.49 | .22 | .02 | .06 |
| Metacognition | 56.09 | 12.68 | 57.00 | 12.78 | 63.00 | 12.14 | 1.54 | .22 | .02 | .10 |
Note. Covariates in each analysis include child age, gender, race/ethnicity, zBMI, depressive symptoms, and family income.
QEWP-A = Questionnaire of Eating and Weight Patterns-Adolescent version.
Higher scores indicate poorer EF. Behavioral regulation and Metacognition mean and SD scores derived from raw values to increase interpretability. Analyses of covariance were conducted using log-transformed data.
Post Hoc Analyses: Executive Function Differences Across Youth Eating Behavior
Post hoc comparisons were conducted to examine caregiver proxy-reported EF differences between each type of caregiver-reported youth eating behavior (NE vs. EO; NE vs. BE; and EO vs. BE), which are visually represented in Figure 2A and B. Per caregiver report, children who exhibited BE had poorer behavioral regulation (p < .001) and metacognition (p < .001) than children with NE. Similarly, children who experienced EO had poorer behavioral regulation compared with children with NE (p = .015). In line with these findings, children with EO compared with those with NE had poorer metacognition, though this effect was only near statistical significance (p = .051). However, between children who exhibited BE vs. OE, there were no differences in behavioral regulation or metacognition (p = .661; p = .110, respectively). No post hoc comparisons were conducted for child self-report of eating behavior, as main effects for these data were not significant (see Table IV).
Figure 2.
Bonferroni-corrected post hoc comparisons of EF across youth eating behaviors per caregiver report. (A) Behavioral regulation in youth with obesity based on parent proxy report of child eating behavior. (B) Metacognition in youth with obesity based on parent proxy report of child eating behavior.
Note. Higher scores indicate poorer EF. Unadjusted (raw) mean values are presented in figures.
Discussion
This study extends the literature on the involvement of EF in pediatric obesity in the following three ways. First, we identify modifiable eating behavior correlates of executive dysfunction in children and adolescents with obesity that have been shown to impact long-term weight status and psychosocial health (Goldschmidt et al., 2015a; Goldschmidt, Wall, Zhang, Loth, & Neumark-Sztainer, 2016b; Sonneville et al., 2013). Second, we use multiple informant assessment methods for eating behavior, which is important given the low agreement rates between caregivers and youth that have previously been demonstrated in the types of eating behaviors we assessed (Johnson et al., 1999; Steinberg et al., 2004). Third, we include a racially/ethnically diverse sample of children with obesity spanning a broad age range. The development of EF across childhood is a complex process, which may be even more complicated and vulnerable to impairment in youth with obesity because of a variety of factors (Miller et al., 2015; Reinert et al., 2013). This study focuses on one of these factors (i.e., dysregulated eating behavior) to improve our understanding of the association between EF and obesity in youth.
Overall, caregiver proxy report of youth EF problems was highly prevalent in this sample, with one in four youth exhibiting clinically significant levels of executive dysfunction. This is substantially higher than the 6–8% of children considered at clinically significant risk for executive dysfunction identified in a previous study of youth with untreated, newly diagnosed hypertension (aged 10–18 years; N = 32); however, only 53% of the children in that sample had obesity (Lande et al., 2009). Together, these findings lend support to further research examining physiological mechanisms of obesity that may contribute to executive dysfunction in childhood, such as hypertension (Lande et al., 2009), glucose metabolism (Jastreboff et al., 2016), or other biomarkers potentially underlying EF problems (Miller et al., 2015). Nonetheless, the high rate of executive dysfunction reported in the current study is problematic, as EF is an integral part of medical self-management and adherence (Lansing & Berg, 2014; McNally, Rohan, Pendley, Delamater, & Drotar, 2010). Furthermore, EF problems have been associated with poorer health behaviors, health-related quality of life, and psychological and academic functioning in children (Gerst, Cirino, Fletcher, & Yoshida, 2015; Schraegle & Titus, 2016; Snyder, 2013; Stautz, Pechey, Couturier, Deary, & Marteau, 2016).
Our findings suggest that poorer EF is also associated with obesogenic eating behaviors across a large age range of youth. Specifically, poorer EF was associated with overeating as well as BE, when compared with an absence of dysregulated eating behavior. This is consistent with previous studies that have demonstrated cross-sectional and longitudinal associations between impulsivity, BE, and BMI/weight status in children or adolescents (Goldschmidt et al., 2015a; Nederkoorn et al., 2006). Similar cross-sectional associations between behavioral and cognitive dysregulation and unhealthy eating behaviors have been demonstrated in adolescents and young adults (aged 15–21 years) with severe obesity (Gowey et al., 2016). In addition, our findings demonstrate that zBMI was highest among youth who engaged in BE compared with those who engaged in overeating or those who did not engage in any dysregulated eating behavior. These findings are in line with the recent studies discussed, which suggest an association between BE and excess weight in a broad pediatric age range and diverse racial/ethnic sample. LOC over eating is the key component differentiating BE from overeating that seems to be associated with higher weight status in the current sample. This is consistent with previous literature suggesting that children and adolescents with LOC demonstrate greater weight gain, poorer health indicators, and poorer psychological functioning than children without LOC (Goldschmidt et al., 2015b; Tanofsky-Kraff et al., 2009).
Surprisingly, however, no differences in EF were identified in individuals who engaged in overeating compared with those who exhibited BE. Previous studies have identified LOC over eating as a distinct correlate and predictor of poorer psychological and cognitive function (Goldschmidt et al., 2015b; Goldschmidt et al., 2016a; Goossens et al., 2009). In the current study, we used a dichotomous measure of eating behavior, which decreases the variability of these constructs and, thus, may have decreased our ability to identify differences of smaller magnitudes, particularly when paired with smaller group sizes. However, it is also possible that there were no substantive differences in EF based on eating behavior type, which could be explored with further research to determine whether specific assessment and/or targeted treatment strategies need to be developed. The findings of the current study extend the literature by providing a comprehensive and ecologically valid conceptualization of EF and its association with obesity-promoting eating behavior across a wide age range of ethnically/racially diverse youth who are overweight and obese. Together, these factors increase the generalizability of findings regarding the associations of EF with dysregulated eating behaviors in pediatric obesity.
While behavioral regulation and metacognition were associated with overeating and BE per caregiver observations, these associations were not apparent when youth self-reported their eating behaviors. This is consistent with previous studies conducted using community- and school-based samples that demonstrated only slight agreement (e.g., kappa = .19) between child and caregiver report of disordered eating behavior (Johnson et al., 2001; Landis & Koch, 1977; Steinberg et al., 2004). The current study expands these findings to a diverse, clinical sample. There are several potential reasons for the discrepancy between youth and caregiver reports: the possibility that youth did not perceive their eating behaviors to be problematic, failure to report dysregulated eating behaviors because of social desirability bias or shame, or difficulty understanding concepts or items (e.g., LOC) on the questionnaires. Furthermore, caregiver report can capture important information that may be missed when children self-report their behavior because of lack of insight or self-awareness, particularly if EF problems (Steward, Tan, Delgaty, Gonzales, & Bunner, 2017) or disordered eating behavior such as BE (Heatherton & Baumeister, 1991) is present. Alternatively, relying on caregiver observations alone has been criticized for various reasons, including the potential bias of caregiver distress or psychopathology to affect reports of their child’s behavior (Briggs-Gowan, Carter, & Schwab-Stone, 1996; Familiar et al., 2016). Thus, further support is needed to replicate the caregiver-observed association of child eating behavior and EF in this sample using additional types of methodologies. These findings should be interpreted in the context of several limitations. While the cross-sectional, observational design provides useful comprehensive information on cognitive processes that are associated with obesity-promoting behaviors in a wide range of youth, it does not provide any information on the directionality of these findings. Drawing from previous prospective research on EF and eating behaviors (Goldschmidt et al., 2015a; Goldschmidt et al., 2016a), we speculate that preceding EF problems may lead to overeating and BE, but longitudinal research is needed to support these assertions. Furthermore, subjective reports of EF and eating behaviors were used in the current study and only caregiver report of EF was collected. As noted previously, caregiver proxy report has certain limitations including potential bias of the caregiver’s distress on the ratings of their child’s behavior (Briggs-Gowan et al., 1996; Familiar et al., 2016). Future designs should consider using multimethod assessment approaches including objective measures of these constructs, in addition to subjective measures, to provide a more comprehensive understanding of EF–eating behavior associations to maximize internal and external validity. More objective measures, such as performance-based, neuropsychological testing for EF as well as comprehensive clinical eating disorder interviews or laboratory-based eating behavior paradigms, would be particularly useful in addressing two limitations of this study: (1) utilization of a subjective questionnaire to measure EF, and (2) diagnostic classification of eating behavior/disorder categories (e.g., BED) using questionnaires. Notably, we did not target a population with preidentified dysregulated eating behavior, which limited our ability to examine the associations between EF and eating behavior in greater detail. The broad age range of youth included in the current study may limit the interpretation of findings, given the potential variation in prevalence of eating behaviors and accuracy of reporting across childhood and adolescence. Furthermore, it appeared that older youth also had higher BMIs, and reported and/or were reported by caregivers to engage in more dysregulated eating in the current study. Thus, designing adequately powered longitudinal studies to examine predictors of dysregulated eating across youth of different ages and weight statuses is an important next step.
Executive dysfunction in youth with obesity was associated with overeating and BE in the current study, and these eating behaviors have previously been associated with longitudinal weight gain and poor psychosocial and treatment outcomes. Despite the rapid growth in the literature on the role of EF in eating behavior and obesity, there remains a dearth of longitudinal studies to disentangle the associations between eating behavior, EF, obesity, and other contextual factors (e.g., socioeconomic status and parenting behaviors; Rhoades et al., (2011). Yet, the current findings interpreted in the context of the literature suggest that it may be beneficial to address aspects of EF in the assessment and treatment of youth with obesity. Preliminary evidence suggests that targeting EF in pediatric obesity treatment may be a promising approach for sustainable weight improvements (Verbeken et al., 2013). Targeting physical activity could also be a potential avenue for improving neurocognition in children with obesity (Davis et al., 2011). However, further evidence is needed to support intervention approaches that address EF and weight management in this population. Identification of specific EF domains and age-specific EF impairments that could help tailor treatments warrants further attention.
Additionally, a closer examination of the differences in child and caregiver report of eating behavior and their associations with EF would help to elucidate best methods for assessment. Multiple informants and objective measures should be used when possible for assessing youth eating behaviors and other relevant health behaviors. Efforts have been made to develop reliable, valid, and accessible assessment measures for pediatric perceived physical and psychological health (e.g., PROMIS) (Cella et al., 2007) and performance-based cognitive function (e.g., NIH Toolbox Cognition Battery; Weintraub et al., 2013). Methodological advances now allow for a multidimensional approach to assess EF in youth using neuroimaging, performance-based tests, and subjective reports. However, pediatric assessment measures for (1) dysregulated eating in children with obesity and (2) EF in the context of food/eating have yet to be developed, adapted, and/or used consistently, despite a demonstrated need (Jensen, Duraccio, Barnett, & Stevens, 2016; Jensen & Kirwan, 2015).
Acknowledgments
The authors are grateful to all of the families who participated in the study.
Funding
This work was supported by the University of Florida Center for Pediatric Psychology and Family Studies. M.A.G. is supported by a National Institutes of Health training grant (grant number T32DK062710). The content is the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of interest: None declared.
References
- Allgaier A. K., Frühe B., Pietsch K., Saravo B., Baethmann M., Schulte-Körne G. (2012). Is the Children's Depression Inventory short version a valid screening tool in pediatric care? A comparison to its full-length version. Journal of Psychosomatic Research, 73, 369–374. doi: 10.1016/j.jpsychores.2012.08.016 [DOI] [PubMed] [Google Scholar]
- Anderson P. (2002). Assessment and development of Executive Function (EF) during childhood. Child Neuropsychology, 8, 71–82. doi:10.1076/chin.8.2.71.8724 [DOI] [PubMed] [Google Scholar]
- Braet C. (2006). Patient characteristics as predictors of weight loss after an obesity treatment for children. Obesity, 14, 148–155. doi:10.1038/oby.2006.18 [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan M. J., Carter A. S., Schwab-Stone M. (1996). Discrepancies among mother, child, and teacher reports: Examining the contributions of maternal depression and anxiety. Journal of Abnormal Child Psychology, 24, 749–765. [DOI] [PubMed] [Google Scholar]
- Cella D., Yount S., Rothrock N., Gershon R., Cook K., Reeve B., Ader D., Fries J. F., Bruce B., Rose M.; PROMIS Cooperative Group. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap Cooperative Group during its first two years. Medical Care, 45, S3–S11. doi:10.1097/01.mlr.0000258615.42478.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C. L., Tomporowski P. D., McDowell J. E., Austin B. P., Miller P. H., Yanasak N. E., Allison J. D., Naglieri J. A. (2011). Exercise improves executive function and achievement and alters brain activation in overweight children: A randomized, controlled trial. Health Psychology, 30, 91–98. doi:10.1037/a0021766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Groot C. J., van den Akker E. L., Rings E. H., Delemarre-van de Waal H. A., van der Grond J. (2016). Brain structure, executive function and appetitive traits in adolescent obesity. Pediatric Obesity, doi:10.1111/ijpo.12149. [DOI] [PubMed] [Google Scholar]
- Epstein L. H., Paluch R. A., Roemmich J. N., Beecher M. D. (2007). Family-based obesity treatment, then and now: Twenty-five years of pediatric obesity treatment. Health Psychology, 26, 381–391. doi:10.1037/0278-6133.26.4.381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Familiar I., Nakasujja N., Bass J., Sikorskii A., Murray S., Ruisenor-Escudero H., Bangirana P., Opoka R., Boivin M. J. (2016). Caregivers' depressive symptoms and parent-report of child executive function among young children in Uganda. Learning and Individual Differences, 46, 17–24. doi:10.1016/j.lindif.2015.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein E. A., Graham W. C., Malhotra R. (2014). Lifetime direct medical costs of childhood obesity. Pediatrics, 133, 854–862. doi:10.1542/peds.2014-0063 [DOI] [PubMed] [Google Scholar]
- Gerst E. H., Cirino P. T., Fletcher J. M., Yoshida H. (2015). Cognitive and behavioral rating measures of executive function as predictors of academic outcomes in children. Child Neuropsychology, 23, 381–407. doi:10.1080/09297049.2015.1120860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia G., Isquith P., Guy S., Kenworthy L. (2000). Behavior rating inventory of executive function. Child Neuropsychology, 6, 235–238. doi:10.1076/chin.6.3.235.3152 [DOI] [PubMed] [Google Scholar]
- Goldschmidt A. B., Aspen V. P., Sinton M. M., Tanofsky-Kraff M., Wilfley D. E. (2008). Disordered eating attitudes and behaviors in overweight youth. Obesity, 16, 257–264. doi:10.1038/oby.2007.48 [DOI] [PubMed] [Google Scholar]
- Goldschmidt A. B., Hipwell A. E., Stepp S. D., McTigue K. M., Keenan K. (2015a). Weight gain, executive functioning, and eating behaviors among girls. Pediatrics, 136, e856–e863. doi:10.1542/peds.2015-0622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt A. B., Lavender J. M., Hipwell A. E., Stepp S. D., Keenan K. (2016a). Emotion regulation and loss of control eating in community-based adolescents. Journal of Abnormal Child Psychology, doi:10.1007/s10802-016-0152-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt A. B., Loth K. A., MacLehose R. F., Pisetsky E. M., Berge J. M., Neumark-Sztainer D. (2015b). Overeating with and without loss of control: Associations with weight status, weight-related characteristics, and psychosocial health. The International Journal of Eating Disorders, 48, 1150–1157. doi:10.1002/eat.22465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt A. B., Wall M. M., Zhang J., Loth K. A., Neumark-Sztainer D. (2016b). Overeating and binge eating in emerging adulthood: 10-year stability and risk factors. Developmental Psychology, 52, 475–483. doi:10.1037/dev0000086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goossens L., Braet C., Van Vlierberghe L., Mels S. (2009). Loss of control over eating in overweight youngsters: The role of anxiety, depression and emotional eating. European Eating Disorders Review, 17, 68–78. doi:10.1002/erv.892 [DOI] [PubMed] [Google Scholar]
- Gowey M. A., Reiter-Purtill J., Becnel J., Peugh J., Mitchell J. E., Zeller M. H. (2016). Weight-related correlates of psychological dysregulation in adolescent and young adult (AYA) females with severe obesity. Appetite, 99, 211–218. doi:10.1016/j.appet.2016.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groppe K., Elsner B. (2015). The influence of hot and cool executive function on the development of eating styles related to overweight in children. Appetite, 87, 127–136. doi:10.1016/j.appet.2014.12.203 [DOI] [PubMed] [Google Scholar]
- Hannon T. S., Li Z., Tu W., Huber J. N., Carroll A. E., Lagges A. M., Gupta S. (2014). Depressive symptoms are associated with fasting insulin resistance in obese youth. Pediatric Obesity, 9, e103–e107. doi:10.1111/ijpo.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton T. F., Baumeister R. F. (1991). Binge eating as escape from self-awareness. Psychological Bulletin, 110, 86–108. [DOI] [PubMed] [Google Scholar]
- IBM Corporation. (2015). IBM SPSS Statistics for Windows (Version 23.0). Armonk, NY: IBM Corporation.
- Janicke D. M., Steele R. G., Gayes L. A., Lim C. S., Clifford L. M., Schneider E. M., Carmody J. K., Westen S. (2014). Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. Journal of Pediatric Psychology, 39, 809–825. doi:10.1093/jpepsy/jsu023 [DOI] [PubMed] [Google Scholar]
- Jastreboff A. M., Sinha R., Arora J., Giannini C., Kubat J., Malik S., Van Name M. A., Santoro N., Savoye M., Duran E. J., Pierpont B., Cline G., Constable R. T., Sherwin R. S., Caprio S. (2016). Altered brain response to drinking glucose and fructose in obese adolescents. Diabetes, 65, 1929–1939. doi:10.2337/db15-1216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen C. D., Duraccio K. M., Barnett K. A., Stevens K. S. (2016). Appropriateness of the food-pics image database for experimental eating and appetite research with adolescents. Eating Behaviors, 23, 195–199. doi: 10.1016/j.eatbeh.2016.10.007 [DOI] [PubMed] [Google Scholar]
- Jensen C. D., Kirwan C. B. (2015). Functional brain response to food images in successful adolescent weight losers compared with normal-weight and overweight controls. Obesity, 23, 630–636. doi:10.1002/oby.21004 [DOI] [PubMed] [Google Scholar]
- Johnson W. G., Grieve F. G., Adams C. D., Sandy J. (1999). Measuring binge eating in adolescents: Adolescent and parent versions of the questionnaire of eating and weight patterns. The International Journal of Eating Disorders, 26, 301–314. [DOI] [PubMed] [Google Scholar]
- Johnson W. G., Kirk A. A., Reed A. E. (2001). Adolescent version of the questionnaire of eating and weight patterns: Reliability and gender differences. The International Journal of Eating Disorders, 29, 94–96. [DOI] [PubMed] [Google Scholar]
- Kovacs M. (1992). The children's depression inventory. North Tonawanda, NY: Mulit-Health Systems. [Google Scholar]
- Kovacs M. (2003). Children's Depression Inventory (CDI): Technical manual update. North Tonawanda, NY: Multi-Health Systems. [Google Scholar]
- Kuczmarski R. J., Ogden C. L., Grummer-Strawn L. M., Flegal K. M., Guo S. S., Wei R., Mei Z., Curtin L. R., Roche A. F., Johnson C. L. (2000). CDC growth charts: United States. Advance Data, 314, 1–27. [PubMed] [Google Scholar]
- Lande M. B., Adams H., Falkner B., Waldstein S. R., Schwartz G. J., Szilagyi P. G., Hongyuem W., Palumbo D. (2009). Parental assessments of internalizing and externalizing behavior and executive function in children with primary hypertension. The Journal of Pediatrics, 154, 207–212. doi:10.1016/j.jpeds.2008.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis J. R., Koch G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33, 159–174. [PubMed] [Google Scholar]
- Lansing A. H., Berg C. A. (2014). Topical review: Adolescent self-regulation as a foundation for chronic illness self-management. Journal of Pediatric Psychology, 39, 1091–1096. doi:10.1093/jpepsy/jsu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J., Matheson B. E., Kaye W. H., Boutelle K. N. (2014). Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. International Journal of Obesity, 38, 494–506. doi:10.1038/ijo.2013.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maayan L., Hoogendoorn C., Sweat V., Convit A. (2011). Disinhibited eating in obese adolescents is associated with orbitofrontal volume reductions and executive dysfunction. Obesity, 19, 1382–1387. doi:10.1038/oby.2011.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahone E. M., Cirino P. T., Cutting L. E., Cerrone P. M., Hagelthorn K. M., Hiemenz J. R., Singer H. S., Denckla M. B. (2002). Validity of the behavior rating inventory of executive function in children with ADHD and/or Tourette syndrome. Archives of Clinical Neuropsychology, 17, 643–662. doi: 10.1016/S0887-6177(01)00168-8 [DOI] [PubMed] [Google Scholar]
- McNally K., Rohan J., Pendley J. S., Delamater A., Drotar D. (2010). Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care, 33, 1159–1162. doi:10.2337/dc09-2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A. L., Lee H. J., Lumeng J. C. (2015). Obesity-associated biomarkers and executive function in children. Pediatric Research, 77, 143–147. doi:10.1038/pr.2014.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooreville M., Shomaker L. B., Reina S. A., Hannallah L. M., Adelyn Cohen L., Courville A. B., Kozlosky M., Brady S. M., Condarco T., Yanovski S. Z., Tanofsky-Kraff M., Yanovski J. A. (2014). Depressive symptoms and observed eating in youth. Appetite, 75, 141–149. doi:10.1016/j.appet.2013.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers T. A. (2011). Goodbye, listwise deletion: Presenting hot deck imputation as an easy and effective tool for handling missing data. Communication Methods and Measures, 5, 297–310. [Google Scholar]
- Nangle D. W., Johnson W. G., Carr-Nangle R. E., Engler L. B. (1994). Binge eating disorder and the proposed DSM-IV criteria: Psychometric analysis of the questionnaire of eating and weight patterns. The International Journal of Eating Disorders, 16, 147–157. [DOI] [PubMed] [Google Scholar]
- Nederkoorn C., Braet C., Van Eijs Y., Tanghe A., Jansen A. (2006). Why obese children cannot resist food: The role of impulsivity. Eating Behaviors, 7, 315–322. doi:10.1016/j.eatbeh.2005.11.005 [DOI] [PubMed] [Google Scholar]
- Nederkoorn C., Jansen E., Mulkens S., Jansen A. (2007). Impulsivity predicts treatment outcome in obese children. Behaviour Research and Therapy, 45, 1071–1075. doi: 10.1016/j.brat.2006.05.009 [DOI] [PubMed] [Google Scholar]
- Ogden C. L., Carroll M. D., Lawman H. G., Fryar C. D., Kruszon-Moran D., Kit B. K., Flegal K. M. (2016). Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA, 315, 2292–2299. doi:10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly J. J., Methven E., McDowell Z. C., Hacking B., Alexander D., Stewart L., Kelnar C. J. H. (2003). Health consequences of obesity. Archives of Disease in Childhood, 88, 748–752. doi:10.1136/adc.88.9.748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinehr T., Lass N., Toschke C., Rothermel J., Lanzinger S., Holl R. W. (2016). Which amount of BMI-SDS reduction is necessary to improve cardiovascular risk factors in overweight children? The Journal of Clinical Endocrinology and Metabolism, 101, 3171–3179. jc20161885. doi:10.1210/jc.2016-1885 [DOI] [PubMed] [Google Scholar]
- Reinert K. R., Po'e E. K., Barkin S. L. (2013). The relationship between executive function and obesity in children and adolescents: A systematic literature review. Journal of Obesity, 2013, 820956. doi:10.1155/2013/820956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhoades B. L., Greenberg M. T., Lanza S. T., Blair C. (2011). Demographic and familial predictors of early executive function development: Contribution of a person-centered perspective. Journal of Experimental Child Psychology, 108, 638–662. doi:10.1016/j.jecp.2010.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schraegle W. A., Titus J. B. (2016). Executive function and health-related quality of life in pediatric epilepsy. Epilepsy and Behavior, 62, 20–26. doi:10.1016/j.yebeh.2016.06.006 [DOI] [PubMed] [Google Scholar]
- Shomaker L. B., Tanofsky-Kraff M., Elliott C., Wolkoff L. E., Columbo K. M., Ranzenhofer L. M., Roza C. A., Yanovski S. Z., Yanovski J. A. (2010). Salience of loss of control for pediatric binge episodes: Does size really matter? The International Journal of Eating Disorders, 43, 707–716. doi:10.1002/eat.20767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder H. R. (2013). Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: A meta-analysis and review. Psychological Bulletin, 139, 81–132. doi:10.1037/a0028727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonneville K. R., Horton N. J., Micali N., Crosby R. D., Swanson S. A., Solmi F., Field A. E. (2013). Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: Does loss of control matter? JAMA Pediatrics, 167, 149–155. doi:10.1001/2013.jamapediatrics.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R. L., Yanovski S., Wadden T., Wing R., Marcus M. D., Stunkard A., Devlin M., Mitchell J., Hasin D., Horne R. L. (1993). Binge eating disorder: Its further validation in a multisite study. The International Journal of Eating Disorders, 13, 137–153. [PubMed] [Google Scholar]
- Stautz K., Pechey R., Couturier D. L., Deary I. J., Marteau T. M. (2016). Do executive function and impulsivity predict adolescent health behaviour after accounting for intelligence? Findings from the ALSPAC cohort. PLoS One, 11, e0160512. doi:10.1371/journal.pone.0160512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg E., Tanofsky-Kraff M., Cohen M. L., Elberg J., Freedman R. J., Semega-Janneh M., Yanovski S. Z., Yanovski J. A. (2004). Comparison of the child and parent forms of the questionnaire on eating and weight patterns in the assessment of children's eating-disordered behaviors. The International Journal of Eating Disorders, 36, 183–194. doi:10.1002/eat.20022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steward K. A., Tan A., Delgaty L., Gonzales M. M., Bunner M. (2017). Self-awareness of executive functioning deficits in adolescents with ADHD. Journal of Attention Disorders, 21, 316–322. doi:10.1177/1087054714530782 [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M., Shomaker L. B., Olsen C., Roza C. A., Wolkoff L. E., Columbo K. M., Raciti G., Zocca J. M., Wilfley D. E., Yanovski S. Z., Yanovski J. A. (2011). A prospective study of pediatric loss of control eating and psychological outcomes. Journal of Abnormal Psychology, 120, 108–118. doi:10.1037/a0021406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M., Yanovski S. Z., Schvey N. A., Olsen C. H., Gustafson J., Yanovski J. A. (2009). A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. The International Journal of Eating Disorders, 42, 26–30. doi:10.1002/eat.20580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbeken S., Braet C., Goossens L., van der Oord S. (2013). Executive function training with game elements for obese children: A novel treatment to enhance self-regulatory abilities for weight-control. Behaviour Research and Therapy, 51, 290–299. doi: 10.1016/j.brat.2013.02.006 [DOI] [PubMed] [Google Scholar]
- Wagner S., Muller C., Helmreich I., Huss M., Tadic A. (2015). A meta-analysis of cognitive functions in children and adolescents with major depressive disorder. European Child and Adolescent Psychiatry, 24, 5–19. doi:10.1007/s00787-014-0559-2 [DOI] [PubMed] [Google Scholar]
- Weintraub S., Dikmen S. S., Heaton R. K., Tulsky D. S., Zelazo P. D., Bauer P. J., Kozlosky M., Brady S. M., Condarco T., Yanovski S. Z., Tanofsky-Kraff M., Gershon R. C. (2013). Cognition assessment using the NIH Toolbox. Neurology, 80(11 Suppl 3), S54–S64. 10.1212/WNL.0b013e3182872ded [DOI] [PMC free article] [PubMed] [Google Scholar]