Abstract
Objective
We examined BOLD (Blood-Oxygen-Level Dependent) activity reduction upon stimuli repetition of face-name pairs in older adults with amnestic (aMCI) and non-amnestic (naMCI) mild cognitive impairment diagnosed using a comprehensive actuarial method, and relationships between activity reduction and behavioral indices.
Method
Twenty-nine cognitively healthy older adults (CHs) and 20 with MCI (n = 12 aMCI; n = 8 naMCI) underwent functional MRI event-related imaging, a comprehensive neuropsychological battery, and 1-year follow-up exam. During scanning, participants were shown face-name pairs 1–3 times and administered a post-scan recognition task.
Results
The MCI group demonstrated less activity reduction upon repetition of face-name pairs within the MTL and other regions compared to CHs. Less activity reduction was associated with poorer Time 1 neuropsychological performance for the CH group and poorer post-scan recognition performance for the MCI group. Less activity reduction was related to poorer neuropsychological performance at Time 2 in the MCI group. Within MCIs, those with aMCI demonstrated less activity reduction upon repetition of face-name pairs than those with naMCI.
Conclusions
Distinct patterns of brain activity were identified in the MCI group compared to CHs, and aMCI compared to naMCI. Activated regions were not restricted to traditional memory circuitry, implicating a wider network of regions involved in the encoding of associative tasks. Findings add support to the hypothesis that lack of reduced BOLD activity reflects “faulty adaptation” to repeated stimuli and that reduction in activity represents successful encoding processes. They also provide further support for use of the face-name paradigm as a marker of prodromal Alzheimer's disease, and method to distinguish between MCI subtypes.
Keywords: Alzheimer's disease, Mild cognitive impairment, Functional neuroimaging
Introduction
The number of people worldwide living with dementia is nearing 50 million; a number expected to triple by 2050 due to the growing aging population (Prince, Guerchet, & Prina, 2015). Alzheimer's Disease (AD) is the most common form of dementia and affects approximately 10% of adults at age 65, with the prevalence increasing up to 40% by age 80 (Kukull et al., 2002). The search for prodromal markers of AD is predicated on key findings that neurodegeneration involving senile plaques and neurofibrillary tangles occurs well before the onset of the clinical features of the disease (Braak & Braak, 1991; Brewer & Moghekar, 2002), and that disease-modifying interventions would be most-effective if implemented before clinical symptoms appear (DeKosky & Marek, 2003). Successful intervention at this critical period has the potential to decrease the growing catastrophic effect on patients, their families, and the healthcare system (Alzheimer's Association, 2014).
An increased emphasis on early identification of AD led to the development of the concept of mild cognitive impairment (MCI) to characterize individuals with intact global cognition and daily functioning but impairment on cognitive tasks most commonly in the domain of episodic memory (Petersen, 2004). Mild cognitive impairment represents a risk factor for AD and other dementias and thus these individuals may provide useful information regarding the early cognitive and neural changes preceding AD. The earliest neuropathological changes in pre-clinical AD occur primarily in brain regions that subserve episodic memory including the hippocampus and entorhinal cortex (Hyman, Van Hoesen, Damasio, & Barnes, 1984; Jack et al., 1999). However, accumulating evidence suggests that the various subtypes of MCI (e.g., amnestic vs. non-amnestic) have varied cognitive profiles, neuropathological changes, and functional and predictive utility (Bangen et al., 2010; Bondi et al., 2014; Busse, Hensel, Gühne, Angermeyer, & Riedel-Heller, 2006; Jak et al., 2009a; Libon et al., 2011; Wolk et al., 2009).
Functional magnetic resonance imaging (fMRI) has been successfully used as a non-invasive technique to identify the early functional changes in neuronal activity in the medial temporal lobe (MTL) that may occur before the structural neural changes of AD (Dickerson & Sperling, 2008; Wierenga & Bondi, 2007). One fMRI paradigm used to investigate changes in episodic memory in individuals at-risk for AD is the face-name associative encoding task, which requires participants to encode face-name pairs while in the scanner. This task is ecologically relevant as difficulty remembering names is a common complaint of older adults presenting to memory clinics (Leirer, Morrow, Sheikh, & Pariante, 1990; Zelinski & Gilewski, 1988). Additionally, face-name associative encoding tasks require multi-modal visual and verbal integration, a role that is thought to involve the hippocampus—one of the earliest brain structures to deteriorate with AD (Eichenbaum, 2004; Sperling, 2007). Taken together, the use of face-name associative encoding tasks in at-risk older adults is ecologically relevant, has the potential to reveal pathophysiological changes prior to dementia diagnosis, and could provide a useful assay of brain response in susceptible regions and functions (Festa et al., 2005; Stoub, Stebbins, Leurgans, Bennett, & Shah, 2006).
Although fMRI studies of older adults with AD consistently demonstrate decreased activation in hippocampal structures compared to healthy comparison subjects during face-name encoding, studies examining neurofunctional differences between those with MCI and cognitively healthy (CH) have yielded variable results, with some studies demonstrating increased hippocampal activation in those with MCI and others demonstrating decreased hippocampal activation during face-name encoding (for reviews, see Sperling, 2007). These differences may be accounted for by the level of cognitive impairment of the MCI group, by varying MCI diagnostic techniques across studies, or from the inclusion of mixed MCI subtypes, among other reasons. Several studies utilizing the face-name associative encoding paradigm have varied the number of presentations of each face-name stimulus to investigate neural adaptation with repeated stimuli (Johnson et al., 2004; Pihlajamäki, O'Keefe, O’Brien, Blacker, & Sperling, 2011). Specifically, fMRI studies of healthy young adults have documented reduction of activity in areas of the MTL after repetition of stimuli (Dolan & Fletcher, 1999; Strange, Fletcher, Henson, Friston, & Dolan, 1999). This repetition-dependent activity reduction has been documented in human and non-human primates (Grunwald, Elger, Lehnertz, Van Roost, & Heinze, 1995; Grunwald, Lehnertz, Heinze, Helmstaedter, & Elger, 1998; Ringo, 1996) and is believed to be an indicator of learning (Baylis & Rolls, 1987; Brown, Wilson, & Riches, 1987; Desimone, 1996; Henson & Rugg, 2003; Riches, Wilson, & Brown, 1991; Wiggs & Martin, 1998). It has also been shown to be a predictor of subsequent memory performance, with greater repetition-dependent activity reduction after repeated stimuli associated with better memory performance (Elger et al., 1997; Fernández et al., 1999). Additionally, poor learning over repeated trials within the domain of episodic memory has been shown to be a strong predictor of progression to AD (Albert, Moss, Tanzi, & Jones, 2001; Chang et al., 2010).
Several studies have investigated repetition-dependent activity reduction using various fMRI paradigms to compare older adults with MCI (Johnson et al., 2004; Johnson, Schmitz, Asthana, Gluck, & Myers, 2008) and AD (Golby et al., 2005; Pihlajamäki, DePeau, Blacker, & Sperling, 2008) to CHs. These studies have demonstrated that MTL activity is sustained rather than reduced after multiple repetitions providing support for “faulty adaptation” to repeated stimuli in older adults with MCI. For example, one study by Johnson and colleagues (2004) utilized parametrically varied repetition of face-name pairs and demonstrated that hippocampal activity decreased in a systematic fashion with increasing repetitions of the face-name pairs in healthy older adults whereas those with amnestic MCI did not display the expected reduction or adaptation effect (individuals with non-amnestic MCI were not included). Furthermore, reductions in activation were associated with better learning, whereas a lack of expected reduction (i.e., “faulty adaptation”) was associated with poorer learning for task stimuli (Johnson et al., 2004). Pihlajamäki and colleagues (2011) replicated these results in those with AD and older adults with presumed MCI (global Clinical Dementia Rating score of 0.5), and found associations between greater MTL repeated activity and worse word list delayed recall performance. Taken together, these two studies demonstrate that “faulty adaptation,” defined as lack of repetition-dependent reductions in activity, may be useful in identifying early cognitive changes in prodromal AD, and may be an important predictor of future decline in objective memory performance.
Although these findings are compelling, to date, no study utilizing the face-name paradigm has investigated differences in neural activation between different MCI subtypes such as amnestic (aMCI) and non-amnestic (naMCI). Furthermore, the two fMRI studies that have investigated repetition-dependent activity reduction using a face-name paradigm in individuals with MCI (Johnson et al., 2004; Pihlajamäki et al., 2008), used varying methods of identifying individuals with MCI. Johnson and colleagues (2004) used a comprehensive neuropsychological assessment to diagnose amnestic MCI but the characterization of this was unclear, whereas Pihlajamäki and colleagues (2011) used a global Clinical Dementia Rating (CDR) score of 0.5. The use of comprehensive neuropsychological diagnostic schemes that are operationally defined is associated with more stable prevalence and progression rates, as well as better accordance with biological markers of AD (Bondi et al., 2014; Jak et al. 2009a, 2009b). Furthermore, inclusion of MCI subtypes such as aMCI versus naMCI has been shown to improve diagnostic accuracy and stability in biomarker studies of MCI (Bondi et al., 2014; Coutinho et al., 2015), and has also been shown to be helpful in predicting conversion to AD (Bondi et al., 2014) with the aMCI subtype being more likely to convert than naMCI subtypes (Espinosa et al., 2013; Fischer et al., 2007; Jungwirth, Zehetmayer, Hinterberger, Tragl, & Fischer, 2012; Petersen et al., 2009). Finally, neither the study by Johnson and colleagues (2004), nor the study by Pihlajamäki and colleagues (2011) assessed the predictive utility of this task with regard to future neuropsychological performance and specifically cognitive decline.
Thus, we investigated repetition-dependent Blood-Oxygen-Level Dependent (BOLD) activity reduction during a face-name encoding paradigm in which stimuli were presented only one time (Novel), two times (Repeated once; R1), or three times (Repeated twice; R2). The degree of repetition-dependent activity reduction for R2 vs. R1, R1 vs. Novel, and R2 vs. Novel trials was compared across different MCI subtypes diagnosed using comprehensive neuropsychological criteria and CH older adults in order to delineate functional differences between CHs and MCIs as well as the aMCI and naMCI subtypes. A secondary aim was to determine whether the level of activity reduction across repeated stimuli was a significant predictor of objective memory performance at the time of the scan and 1 year later. In line with previous research, we predicted that older adults with MCI would exhibit less activity reduction, perhaps suggesting “faulty adaptation” to repeated face-name pairs, as indicated by unchanged or increased activation in medial temporal regions after repeated pairs compared to CHs. Furthermore, we predicted that degree of activity reduction upon stimuli repetition would be predictive of current and future objective memory performance within the MCI and CH groups. Although the existing literature on fMRI tasks with MCI subtypes is limited, we predicted that both those with aMCI and naMCI would exhibit a pattern of “faulty adaptation” in medial temporal lobe regions, but those with naMCI would do so to a lesser degree given the hypothesized distinct neuropathological underpinnings of aMCI versus naMCI [i.e., cortical thinning of the temporal cortex vs. deep white matter lesions, respectively (Chua et al., 2009; Serra et al., 2013; Zhuang et al., 2010)].
Materials and Methods
Participants
The participants were 29 CH elderly controls (M age = 75.3; SD = 8.8) and 20 older adults with MCI (M age = 73.4; SD = 7.7). One year after the MRI scan, nine participants were lost to follow-up (3 CH, 5 aMCI, 1 naMCI) leaving 40 participants (14 with MCI and 26 CHs) for follow-up analyses. Participants were classified as CH or MCI using a comprehensive approach to diagnosis defined by at least two impaired scores (i.e., greater than one standard deviation below normative means) in a cognitive domain or at least one impaired score within three or more cognitive domains (see Jak et al., 2009b for full neuropsychological battery). Those in the MCI group were further classified as aMCI (n = 12; M age = 73.8; SD = 7.8) versus naMCI (n = 8; M age = 72.9; SD = 8.0) with the aMCI group defined as those with memory impairment (Jak et al., 2009b). Additionally, participants were required to have intact instrumental activities of daily living and global cognition as assessed by the Independent Living Scales (ILS; T-score ≥ 40; Loeb, 1996) and Dementia Rating Scale (DRS; total raw score ≥ 127; Mattis, 1998), respectively. Participants were also excluded if they had a history of significant head trauma, presence of other neurological or psychiatric disorders (e.g., schizophrenia, bipolar disorder, developmental learning disorder, alcohol or substance abuse), history of stroke, presence of diabetes or respiratory disease, or any contraindications to undergoing an MRI. The Geriatric Depression Scale (GDS; Yesavage et al., 1983) and the Framingham Stroke Risk Profile (FSRP; D'Agostino, Wolf, Belanger, & Kannel, 1994) were used to measure level of self-reported depression and vascular risk factors, respectively. Genomic DNA was collected on all participants using buccal swab to obtain APOE ε4 allele presence. All participants were volunteers in a larger longitudinal study of older adults which recruited through newspaper advertisements and community lectures. All procedures were approved by the Institutional Review Board of the University of California, San Diego and written informed consent was obtained from all participants.
Neuropsychological Testing
The following neuropsychological tests were selected from a larger battery of tests in the domains of memory, attention, language, visuospatial functioning, and executive functioning given within three months of the fMRI scan (Time 1) and 1 year after scanning (Time 2) for their sensitivity to the memory impairments commonly observed in those with MCI: Wechsler Memory Scale—Revised (WMS-R) Logical Memory Immediate and Delayed recall and Visual Reproduction Immediate and Delayed recall subtests (Wechsler, 1987) and the California Verbal Learning Test-Second Edition (CVLT-II) List A 1–5 Total and Long Delay Free Recall scores (Delis, Kramer, Kaplan, & Ober, 1999). The WMS-R Logical Memory Immediate and Delayed recall and Visual Reproduction Immediate and Delayed recall subtests assess structured verbal and visual learning and memory, respectively. The CVLT-II List A 1–5 Total score is a measure of immediate word list learning ability and the Long Delay Free Recall score measures spontaneous recall of the word list after a 20 min delay.
Face-Name Associative Encoding Task and Behavioral Task
The event-related face-name associative encoding task was adapted from work published by Sperling and colleagues (2003). Before entering the scanner, participants were administered a practice test with alternate stimuli to ensure they understood the task. During both the practice and experimental tasks, participants were instructed to view each face-name pair and to try to remember it (Fig. 1). To ensure adequate attention to each stimulus, a prompt at the top of the screen asked participants to make a subjective judgment, “Does this name fit this face?” to which they responded “fit” or “not fit” via a handheld button box. Performance during the scan was monitored by button presses to ensure that participants were awake and attentive. Faces were standardized in terms of age, gender, image size, and minimization of identifying features unrelated to the face (e.g., glasses, jewelry). During the scan, participants were administered five runs total, each lasting 5 min and 12 s. Six face-name pairs occurred once (Novel), 6 occurred twice (Repeated once [R1]), and 6 occurred three times (Repeated twice [R2]) for a total of 36 events per run. Each face-name pair was shown for 6 s and a cross-hair fixation varying in length from .5 to 9 s was interspersed throughout each run. The order of run presentation was counterbalanced yielding five different presentation possibilities. (One subject had a different run order. Three subjects had only four runs and thus their behavioral post-scan recognition data was not analyzed.) The number of stimuli and presentations were based on previous research (Rand-Giovannetti et al., 2006; Vannini, Hedden, Sullivan, & Sperling, 2013; Vannini et al., 2011) that has shown successful encoding and repetition suppression with fewer than four stimuli repetitions. Immediately following the task, participants were given a forced-choice recognition task outside of the scanner consisting of the 90 faces that were presented during scanning and 30 “foils” that were not presented during scanning for a total of 120 trials. Each trial during the recognition task consisted of two questions. Participants were presented with a face and asked to select one of three response choices including the correct name for the face, an incorrect name, or “neither of these”.
Fig. 1.
Examples of stimuli used in the face-name associative encoding task.
Scanning Procedure
Imaging was performed on a General Electric EXCITE 3.0 Tesla whole body imager with an eight-channel receive-only head coil. A high-resolution T1-weighted anatomical scan was acquired at 1 mm3 resolution using a fast spoiled gradient-echo pulse sequence. Functional images were obtained with a 1-shot gradient-echo EPI scan (22 cm FOV, 64×64 matrix, 3.4 mm×3.4 mm in-plane resolution, TR = 3000 ms, TE = 30 ms, flip angle = 90°). Fifty 3.7-mm slices covering the whole brain were acquired obliquely. Two field maps were collected to correct for distortions in EPI images due to inhomogeneities in the static magnetic field. During the five BOLD runs, cardiac and respiratory activity were monitored using a pulse oximeter and respiratory belt, and the waveforms were recorded using Invivo physiological monitoring system.
Data Analyses
All fMRI data were analyzed and overlaid onto structural images using the Analysis of Functional Neuroimaging (AFNI) software package from the National Institutes of Health (Cox, 1996). The AFNI 3D volume registration program was used to minimize the small effects of head motion, whereas larger motion effects were corrected by replacing the mean value of adjacent repetitions in voxels with residual motion in place of motion-corrupted scans. Finally, a signal-intensity threshold-value was used to exclude low intensity values usually located outside the brain. Slice timing correction was applied and the five imaging runs were detrended of low frequency signal drifts (Birn, Saad, & Bandettini, 2001).
Statistical analyses were performed using a general linear model (GLM), with individual events (Novel, repeated once [R1], and repeated twice [R2]) modeled using AFNI's 3dDeconvolve TENT function on each participant's time-series. The following predictors were included in the model: a constant, a linear trend, three parameters indicating the degree of motion correction performed in three rotational angles, and stimulus functions indicating whether the presented face-name pairs were Novel, repeated once (R1), or repeated twice (R2). Adaptation response was modeled using the following contrasts: novel face-name pairs versus those repeated once (NovelvsR1), novel face-name pairs versus those repeated twice (NovelvsR2) and face-name pairs repeated once versus repeated twice (R1vsR2). Thus, higher scores on each contrast represented increased repetition-dependent activity reduction, whereas lower scores represented a lack of repetition-dependent reduction in activity. Functional data were scaled to percent signal change (PSC) and spatially smoothed with a Gaussian kernel of 4mm full-width at half-maximum. The T1-weighted anatomic images and the functional activation maps were warped to the coordinates of the co-planar stereotactic atlas of Talairach and Tournoux (1988) and resampled at a 4 mm3 resolution.
Between-group comparisons (MCI vs. CH, aMCI vs. naMCI) of each of the three contrasts (NovelvsR1, NovelvsR2, and R1vsR2) were conducted using voxel-wise student's t-tests with PSC as the dependent variable. To guard against false-positive errors due to multiple comparisons, Monte-Carlo simulations using 3dClustSim with a per voxel threshold of p < 0.02 and a cluster-size alpha threshold of p < 0.05, indicated that clusters larger than 14 contiguous voxels (896 mm3) were considered significant. Only clusters within the supratentorial region were interpreted.
To examine associations between PSC in significant clusters and cognitive performance variables, mean PSC was extracted from significant clusters resulting from the contrast “NovelvsR2” (reflecting full potential for activity reduction) for each individual and entered into linear regressions to determine whether level of “adaptation” was associated with: (i) behavioral performance on the post-scan recognition task, (ii) neuropsychological performance at Time 1, and (iii) neuropsychological performance at Time 2. For the model using post-scan recognition data as the dependent variable, age, education, gender, diagnosis (diagnosis was coded as −.5 for MCI and .5 for CH), PSC, and a diagnosis by PSC interaction term were entered into four separate linear regressions with the four recognition trial types as the dependent variables (Foil, Novel, R1, and R2). Because Time 1 neuropsychological tests were used to diagnose participants as CH or MCI, the linear regressions using Time 1 neuropsychological data as the dependent variable were run separately for each group (MCI, CH) to reduce circularity. A total of six regressions were run within the CH and MCI groups with WMS-R Logical Memory and Visual Reproduction Immediate and Delayed recall subtests and CVLT-II List A 1–5 Total and Long Delay Free Recall scores as dependent variables controlling for age, education, and gender at a Bonferroni-corrected p-value of .017. To investigate whether adaptation was associated with cognitive change, the model including Time 2 neuropsychological data as the dependent variable combined the CH and MCI groups and included Time 1 neuropsychological performance to model change in performance over time (i.e., for the regression evaluating Visual Reproduction Immediate recall at Time 2, Visual Reproduction Immediate recall at Time 1 was included in the model). Age, education, gender, diagnosis, PSC, and a diagnosis by PSC interaction were regressed onto six Time 2 neuropsychological tests.
Results
Group Differences
There were no group differences between the CH and MCI groups or the aMCI and naMCI groups in age, gender, level of education, handedness, APOE ε4 allele presence, level of depression as measured by the GDS, FSRP percentage, or ILS Money and Health and Safety tests (all p's > .11). Similarly, there were no group differences in whole brain, gray matter, or white matter volume (all p's > .27). There were significant groups differences between the CHs and MCI group on a measure of premorbid intelligence (American National Adult Reading Test; ANART) and the DRS (p's < .05) in which the CHs outperformed MCI group on the DRS and the ANART. Many neuropsychological measures differed between the groups as expected due to inclusion in diagnostic classification (p's < .05). See Table 1 for demographic, clinical, and cognitive characteristics of each group for each time point. None of the participants in the MCI group converted to dementia at Time 2, and only one participant in the MCI group declined by greater than six-points on the DRS at Time 2, which is considered reliable change in a 1-year period (Pedraza et al., 2007).
Table 1.
Demographic, clinical, and cognitive characteristics
| Mean (SD) or N | t or χ2 | p | Mean (SD) or N | t or χ2 | p | |||
|---|---|---|---|---|---|---|---|---|
| CH (n = 29) | MCI (n = 20) | aMCI (n = 12) | naMCI (n = 8) | |||||
| Demographic and clinical characteristics | ||||||||
| Age (years) | 75.3 (8.8) | 73.4 (7.7) | .79 | .436 | 73.8 (7.8) | 72.9 (8.0) | −.24 | .811 |
| Gender (male/female) | 22/7 | 13/7 | .68 | .524 | 5/7 | 2/6 | .59 | .642 |
| Education (years) | 16.5 (2.2) | 16.2 (2.6) | .54 | .594 | 15.4 (2.6) | 17.3 (2.2) | 1.64 | .119 |
| Handedness (R/L) | 27/2 | 19/1 | .07 | 1.00 | 11/1 | 8/0 | .70 | 1.00 |
| APOE (non-ɛ4/ ɛ4) | 19/9 | 13/6 | <.01 | 1.00 | 7/4 | 6/2 | .28 | 1.00 |
| GDS | 2.9 (2.9) | 4.2 (4.0) | 1.31 | .198 | 4.3 (4.3) | 3.9 (3.7) | −.25 | .808 |
| FSRP Stroke Risk (%) | 11.9 (8.1) | 9.3 (6.2) | 1.21 | .233 | 9.3 (5.3) | 9.3 (7.0) | −.01 | .994 |
| ILS Money T-score | 56.2 (3.5) | 54.5 (4.0) | 1.60 | .118 | 54.5 (3.9) | 54.4 (4.5) | −.03 | .976 |
| ILS Health/Safety T-score | 55.1 (5.0) | 53.1 (6.0) | 1.24 | .220 | 52.8 (5.2) | 53.3 (6.8) | −.20 | .841 |
| Neuropsychological performance Year 1 | ||||||||
| Premorbid Estimate (ANART VIQ) | 121.3 (4.7) | 118.1 (6.2) | 2.07 | .044* | 117.3 (6.3) | 119.1 (6.3) | .67 | .510 |
| DRS | 140.7 (3.3) | 138.0 (5.0) | 2.11 | .043* | 136.9 (5.6) | 139.6 (3.8) | 1.19 | .250 |
| LM Immediate | 30.6 (6.3) | 21.9 (8.0) | 4.25 | <.001* | 19.2 (8.2) | 25.9 (6.2) | 1.97 | .064 |
| LM Delayed | 28.3 (7.2) | 16.0 (9.0) | 5.30 | <.001* | 11.8 (7.8) | 22.4 (7.0) | 3.10 | .006* |
| VR Immediate | 33.1 (4.8) | 28.9 (6.1) | 2.65 | .011* | 28.3 (4.9) | 29.9 (7.8) | .58 | .570 |
| VR Delayed | 29.1 (6.2) | 16.2 (10.1) | 5.41 | <.001* | 12.8 (8.2) | 21.4 (11.0) | 2.01 | .059 |
| CVLT-II List A 1–5 Total | 50.7 (9.9) | 38.6 (9.2) | 4.30 | <.001* | 34.4 (8.9) | 44.9 (5.4) | 2.95 | .009* |
| CVLT-II Long Delay Free Recall | 11.7 (3.0) | 6.8 (3.9) | 4.90 | <.001* | 5.3 (3.7) | 9.1 (3.2) | 2.40 | .027* |
| Neuropsychological performance Year 2 | ||||||||
| DRS | 141.5 (1.9) | 140.0 (5.1) | 1.03 | .317 | 138.7 (6.6) | 141.3 (2.9) | .94 | .366 |
| LM Immediate | 32.9 (6.5) | 23.4 (9.5) | 3.32 | .003* | 18.7 (7.8) | 28.1 (9.2) | 2.07 | .061 |
| LM Delayed | 30.5 (7.3) | 16.9 (9.7) | 4.99 | <.001* | 11.9 (8.5) | 22.0 (8.4) | 2.24 | .045* |
| VR Immediate | 34.1 (3.3) | 29.6 (4.5) | 3.59 | .001* | 28.0 (4.7) | 31.3 (3.9) | 1.43 | .180 |
| VR Delayed | 29.6 (6.8) | 18.6 (11.6) | 3.26 | .004* | 15.6 (13.2) | 21.7 (9.7) | .99 | .341 |
| CVLT-II List A 1–5 Total | 52.4 (9.2) | 40.9 (13.1) | 3.23 | .003* | 35.7 (13.4) | 46.1 (11.4) | 1.57 | .143 |
| CVLT-II Long Delay Free Recall | 11.7 (3.0) | 8.1 (5.3) | 2.37 | .030* | 6.1 (5.5) | 10.0 (4.7) | 1.42 | .182 |
*Significant difference at p < .05 level. One participant was missing APOE ɛ4 allele status. GDS = Geriatric Depression Scale; FSRP = Framingham Stroke Risk Profile; ILS = Independent Living Scales; ANART = American National Adult Reading Test; DRS = Dementia Rating Scale; LM = Wechsler Memory Scale—Revised Logical Memory subtest; VR = Wechsler Memory Scale—Revised Visual Reproduction subtest; CVLT-II = California Verbal Learning Test—2nd Edition.
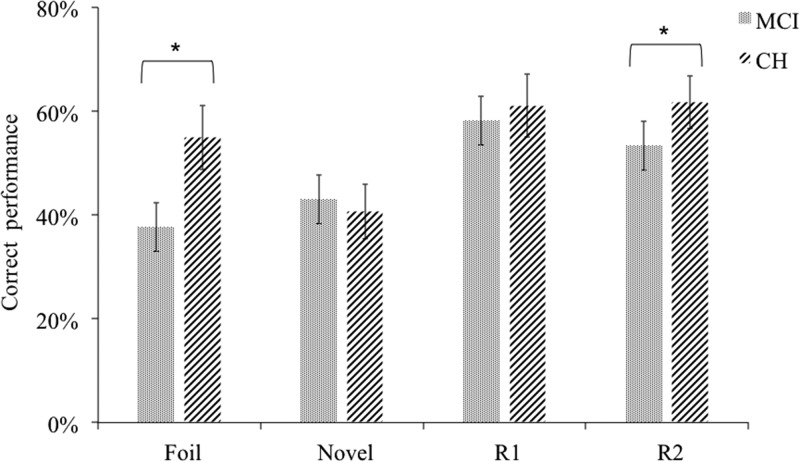
Analysis of Post-Scan Recognition Data
Compared to CHs, the MCI group made a greater number of errors overall on the post-MRI recognition task (t = 2.70, df = 44, p = .01, Cohen's d = 0.81). Specifically, the CH group outperformed the MCI group in accurately rejecting foils (t = 2.55, df = 44, p = .016, Cohen's d = 0.87) and on correct recognition of R2 stimuli (t = 2.69, df = 44, p = .01, Cohen's d = 0.81). Performance on the remaining trial types (Novel, R1) were not significantly different between the two groups (p’s > .017; see Fig. 2). There were no significant differences between the aMCI and naMCI groups on recognition task performance across all four trial types (p’s > .017).
Fig. 2.
Recognition performance across groups.
*Denotes significance at p < .017 level. CH = cognitively healthy comparison; MCI = mild cognitive impairment.
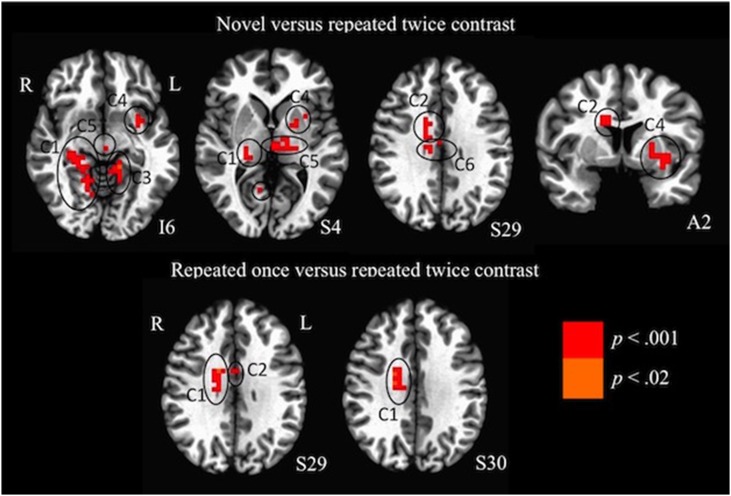
Analysis of fMRI results
Six significant clusters were identified for the NovelvsR2 contrast in which MCIs showed increased activation for face-name pairs repeated twice compared to novel face-name pairs in the parahippocampal gyrus, thalamus, fusiform gyrus, cingulate and caudate (all corrected ps < .02; volume threshold 896 mm3; see Table 2). CHs showed the opposite pattern in those regions, reflecting greater repetition-dependent activity reduction to the face-name pairs in CHs compared to MCIs. A similar pattern was observed for the R1vsR2 condition in that MCIs showed increased activation in two significant clusters in the caudate, cingulate, and thalamus, and CHs showed the opposite pattern, again reflecting repetition-dependent activity reduction to the face-name pairs in CHs (all corrected ps < .02; volume threshold 896 mm3; see Table 2 and Fig. 3). No significant clusters were identified for the NovelvsR1 condition (volume threshold 896 mm3).
Table 2.
Brain areas showing a significantly greater brain response for face-name pairs in older adults with MCI compared to healthy controls (BA = Brodmann's Area; R = right; L = left; C = cluster ≥ 896 mm3; PSC = Percent Signal Change)
| Anatomical location | BA/subregion | Volume (mm3) | Center (x,y,z) | T-value at peak intensity | PSC MCI | PSC CH | Cohen's d | ||
|---|---|---|---|---|---|---|---|---|---|
| Novel vs. Repeated Twice Contrast | |||||||||
| C1 | Focus Point | Right Cerebellar Tonsil | 6976 | R26, A37, I32 | 2.66 | −0.56 | 0.12 | 0.78 | |
| Cerebellum | Right Culmen | ||||||||
| Right Cerebellum (IX) | |||||||||
| Subcortical | Right Parahippocampal Gyrus | R BA 27, 30, 35 | |||||||
| Right Thalamus | |||||||||
| Right Pulvinar | |||||||||
| Temporal | Right Fusiform Gyrus | ||||||||
| Occipital | Right Lingual Gyrus | R BA 18, 19 | |||||||
| C2 | Focus Point | Cingulate | 2112 | R2, P1, S20 | 2.78 | −0.80 | −0.06 | 0.81 | |
| Basal Ganglia | Caudate | ||||||||
| Right Caudate Body | |||||||||
| Subcortical | Thalamus | ||||||||
| Corpus Callosum | |||||||||
| C3 | Focus Point | Left Parahippocampal Gyrus | L BA 30 | 1536 | L14, P37, I4 | 2.79 | −0.59 | 0.14 | 0.81 |
| Cerebellum | Left Culmen | ||||||||
| Subcortical | Left Thalamus | ||||||||
| C4 | Focus Point | Left Lentiform Nucleus | 1344 | L22, P1, S4 | 2.60 | −0.42 | 0.20 | 0.76 | |
| Basal Ganglia | Left Putamen | ||||||||
| Subcortical | Left Parahippocampal Gyrus | ||||||||
| Cerebellum | Left Culmen | ||||||||
| C5 | Focus Point | Thalamus | 1344 | L2, P17, S4 | 2.55 | −0.53 | 0.15 | 0.74 | |
| Left Red Nucleus | |||||||||
| Posterior Commissure | |||||||||
| Subcortical | Left Medial Dorsal Nucleus | ||||||||
| Left Mammilary Body | |||||||||
| Left Ventral Posterior Lateral Nucleus | |||||||||
| C6 | Focus Point | Cingulate Gyrus | 896 | R2, P13, S24 | 2.66 | −0.82 | 0.19 | 0.78 | |
| Repeated Once vs. Twice Contrast | |||||||||
| C1 | Focus Point | Right Caudate | 1728 | R10, P1, S20 | 2.64 | −0.55 | 0.29 | 0.77 | |
| Subcortical | Right Cingulate Gyrus | ||||||||
| Basal Ganglia | Right Caudate Body | ||||||||
| C2 | Focus Point | Corpus Callosum | 896 | L2, P1, S16 | 2.68 | −0.79 | 0.28 | 0.78 | |
| Subcortical | Cingulate Gyrus | ||||||||
| Left Thalamus | |||||||||
| Basal Ganglia | Left Caudate | ||||||||
Clusters shown survived our cluster threshold alpha-protection procedure (clusters: individual voxel p < 0.02, volume 896 mm3, whole brain p < .05; see text for details).
Fig. 3.
Brain areas showing a significantly greater brain response for face-name pairs that were repeated once or twice vs. novel face-name pairs or those repeated once in older adults with MCI compared to cognitively healthy controls (R = Right; L = Left; I = Inferior; S = Superior; A = Anterior).
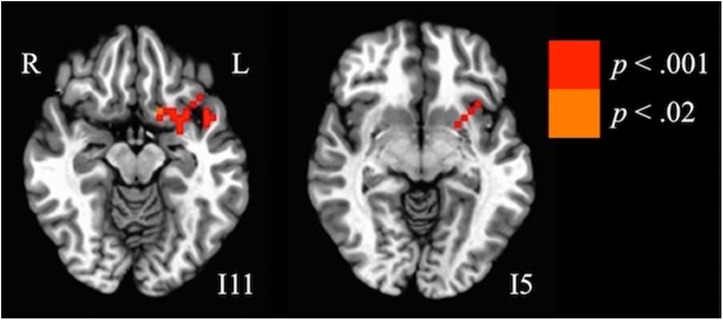
Analysis of fMRI Results by MCI Subtype
With regards to the aMCI and naMCI analyses, one significant cluster was identified for the NovelvsR1 condition in which older adults with aMCI showed a pattern of equal or greater activation during R1 trials compared to novel trials, while the naMCI group showed a pattern similar to that of CHs—greater activation during Novel than R1, reflecting repetition-dependent activity reduction in the naMCI group. The clusters incorporated regions within the left inferior frontal gyrus and left hippocampal gyrus (all corrected ps < .02; volume threshold 896 mm3; see Table 3 and Fig. 4).
Table 3.
Brain areas in which older adults with amnestic MCI showed significantly greater brain response for face-name pairs repeated once vs. novel face-name pairs compared to those with non-amnestic MCI (BA = Brodmann's Area; R = right; L = left; C = cluster ≥ 896 mm3; PSC = Percent Signal Change)
| Anatomical location | BA/subregion | Volume (mm3) | Center (x,y,z) | T-value at peak intensity | PSC MCI | PSC CH | Cohen's d | |
|---|---|---|---|---|---|---|---|---|
| Focus Point | Left Inferior Frontal Gyrus | L BA 47 | 1536 | L26, A7, I16 | 3.09 | −0.51 | 1.27 | 0.90 |
| Basal Ganglia | Left Claustrum | |||||||
| Left Lentiform Nucleus | ||||||||
| Left Putamen | ||||||||
| Subcortical | Left Insula | L BA 13 | ||||||
| Left Thalamus | ||||||||
| Left Subcallosal Gyrus | ||||||||
| Left Parahippocampal Gyrus | L BA 34 | |||||||
| Left Amygdala |
Fig. 4.
Brain areas in which older adults with amnestic MCI showed significantly greater brain response for face-name pairs repeated once vs. novel face-name pairs compared to those with non-amnestic MCI (R = Right; L = Left; I = Inferior).
Associations Between fMRI and Post-Scan Recognition Data
The NovelvsR2 contrast was selected for the analyses that included behavioral performance as our hypotheses were specifically related to adaptation after repeated stimuli, and this contrast is most likely to reflect full adaptation. Three clusters from the NovelvsR2 contrast (clusters 1, 3, and 4—see Table 2) were selected for linear regression analyses based on inclusion of regions that were hypothesized a priori to underlie information encoding (parahippocampal regions). We investigated the interaction between PSC in clusters 1, 3, and 4 and diagnosis (MCI vs. CH) on each of the four trial types of the post-scan task (Novel, R1, and R2 face-name pairs and foils) controlling for age, education, and gender. Given the large number of comparisons across fMRI, behavioral, and neuropsychological test data, we controlled for Type I error using a family-wise Bonferroni-corrected level of p < .017 (.05/3 clusters) for all analyses. Three significant interactions between diagnosis and PSC were observed at the Bonferroni-corrected p-value of .017 (Table 4). Specifically in Cluster 1 (parahippocampal gyrus, thalamus, fusiform, and lingual gyrus), better performance on the post-scan recognition behavioral task for stimuli that were repeated once during the scan was associated with increased repetition-dependent activity reduction (lower PSC for the repeated twice vs. novel stimuli) for the MCI group (B = −.33, p = .017). There were no significant associations between PSC in Cluster 1 and other post-scan stimuli (foils, novel, or R2; all p’s > .017). The same interaction was observed in Cluster 3 (parahippocampal gyrus, thalamus), in which increased repetition-dependent activity reduction was associated with better performance for stimuli that were repeated once (B = −.42, p = .003) and twice (B = −.36, p = .016) specifically for the MCI group after controlling for age, education, and gender. There were no significant associations between PSC in Cluster 3 and other post-scan stimuli (foils, novel; all p’s > .017). No significant interactions or main effects were observed between post-scan recognition data and Cluster 4 at the Bonferroni-corrected p-value (p’s > .017).
Table 4.
Associations between fMRI and post-scan recognition data
| Novel | Repeated once | Repeated twice | Foils | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | R2 | df | p | β | R2 | df | p | β | R2 | df | p | β | R2 | df | p | |
| Regression 1 | .391 | 39 | .002 | .413 | 39 | .001 | .311 | 39 | .019 | .191 | 39 | .192 | ||||
| NovelvsR2 C1 | −.603 | <.001* | −.238 | .132 | −.262 | .127 | −.070 | .703 | ||||||||
| Diagnosis | .314 | .048 | .233 | .131 | .478 | .006 | .407 | .027 | ||||||||
| C1xDiagnosis | −.076 | .569 | −.325 | .017* | −.166 | .247 | −.164 | .870 | ||||||||
| Regression 2 | .251 | 39 | .065 | .427 | 39 | .001 | .356 | 39 | .006 | .233 | 39 | .093 | ||||
| NovelvsR2 C3 | −.290 | .107 | .009 | .955 | −.025 | .881 | −.212 | .242 | ||||||||
| Diagnosis | .135 | .450 | .075 | .629 | .300 | .076 | .539 | .005 | ||||||||
| C3xDiagnosis | −.163 | .294 | −.418 | .003* | −.359 | .016* | .192 | .223 | ||||||||
| Regression 3 | .270 | 39 | .045 | .345 | 39 | .008 | .279 | 39 | .038 | .217 | 39 | .125 | ||||
| NovelvsR2 C4 | −.344 | .047 | −.077 | .632 | −.100 | .551 | −.175 | .319 | ||||||||
| Diagnosis | .184 | .276 | .194 | .226 | .412 | .017 | .489 | .007 | ||||||||
| C4xDiagnosis | −.122 | .423 | −.255 | .081 | −1.131 | .265 | .144 | .363 | ||||||||
*p-value is significant at Bonferroni-corrected value of .017; Each regression included age, gender, and education as covariates. NovelvsR2 C1 = Level of activation in Cluster 1 for the novel vs. repeated twice conditions; β = Beta; R2= R squared; df = degrees of freedom; NovelvsR2 C3 = Level of activation in Cluster 3 for the novel vs. repeated twice conditions; NovelvsR2 C4 = Level of activation in Cluster 4 for the novel vs. repeated twice conditions; C1xDiagnosis = Interaction term which was generated by multiplying activation in Cluster 1 and diagnosis coded as −.5 for the mild cognitive impairment group and .5 for the healthy control group; C3xDiagnosis = Interaction term which was generated by multiplying activation in Cluster 3 and diagnosis coded as −.5 for the mild cognitive impairment group and .5 for the healthy control group; C4xDiagnosis = Interaction term which was generated by multiplying activation in Cluster 4 and diagnosis coded as −.5 for the mild cognitive impairment group and .5 for the healthy control group.
Associations Between fMRI and Neuropsychological Test Data
Time 1. We investigated the relationship between PSC in clusters 1, 3, and 4 from the NovelvsR2 contrast and Time 1 neuropsychological test performance (Table 5). In the CH group, lower PSC for the NovelvsR2 contrast (i.e., increased repetition-dependent activity reduction) in Cluster 1 (parahippocampal gyrus, thalamus, fusiform, and lingual gyrus) was associated with significantly better performance on Visual Reproduction Immediate recall (B = .59, p = .003); there was a nonsignificant trend for Visual Reproduction Delayed recall (B = .37, p = .052). Also for CHs, there was a nonsignificant trend for association between greater repetition-dependent activity reduction in Clusters 3 (parahippocampal gyrus, culmen, thalamus) and 4 (left lentiform nucleus, left parahippocampal gyrus) and better performance on WMS-R Visual Reproduction Immediate recall (C3: B = .45, p = .029; C4: B = .48, p = .016). There was also a nonsignificant trend for greater repetition-dependent activity reduction in Cluster 4 to be associated with better performance on WMS-R Visual Reproduction Immediate recall for the MCI group (B = .65, p = .038).
Table 5.
Associations between fMRI and neuropsychological test data
| VR1 | VR2 | LM1 | LM2 | CVLT 1–5 | CVLT LDFR | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | R2 | df | p | β | R2 | df | p | β | R2 | df | p | β | R2 | df | p | β | R2 | df | p | β | R2 | df | p | |
| Year 1 | ||||||||||||||||||||||||
| MCI | ||||||||||||||||||||||||
| Regression 1 | .201 | 15 | .467 | .214 | 15 | .429 | .285 | 15 | .254 | .365 | 15 | .124 | .357 | 15 | .134 | .194 | 15 | .487 | ||||||
| NovelvsR2 C1 | .452 | .159 | . 281 | .368 | .201 | .497 | .202 | .470 | −.075 | .786 | −.003 | .992 | ||||||||||||
| Regression 2 | .233 | 15 | .376 | .203 | 15 | .461 | .268 | 15 | .291 | .350 | 15 | .144 | .355 | 15 | .137 | .204 | 15 | .456 | ||||||
| NovelvsR2 C3 | .493 | .108 | .236 | .434 | −.099 | .730 | .115 | .670 | −.625 | .853 | .695 | .665 | ||||||||||||
| Regression 3 | .318 | 15 | .192 | .269 | 15 | .287 | .351 | 15 | .142 | .435 | 15 | .059 | .365 | 15 | .124 | .212 | 15 | .433 | ||||||
| NovelvsR2 C4 | .653 | .038† | .428 | .171 | .403 | .172 | .413 | .135 | .143 | .615 | .181 | .566 | ||||||||||||
| CH | ||||||||||||||||||||||||
| Regression 1 | .376 | 22 | .029 | .388 | 22 | .024 | .085 | 24 | .696 | .052 | 24 | .853 | .153 | 24 | .386 | .131 | 24 | .479 | ||||||
| NovelvsR2 C1 | .587 | .003* | .366 | .052† | −.110 | .603 | .029 | .893 | −.042 | .835 | −.109 | .596 | ||||||||||||
| Regression 2 | .257 | 22 | .146 | .341 | 22 | .048 | .078 | 24 | .730 | .057 | 24 | .831 | .155 | 24 | .379 | .120 | 24 | .525 | ||||||
| NovelvsR2 C3 | .447 | .029† | .277 | .138 | −.064 | .753 | .076 | .711 | .794 | .763 | −.010 | .990 | ||||||||||||
| Regression 3 | .289 | 22 | .098 | .284 | 22 | .105 | .085 | 24 | .695 | .052 | 24 | .855 | .397 | 24 | .370 | .120 | 24 | .524 | ||||||
| NovelvsR2 C4 | .477 | .016* | .120 | .522 | −.107 | .597 | −.018 | .929 | −.078 | .686 | −.018 | .928 | ||||||||||||
| Year 2 | ||||||||||||||||||||||||
| Regression 1 | .354 | 30 | .049 | .636 | 30 | <.001 | .766 | 32 | <.001 | .906 | 32 | <.001 | .764 | 32 | <.001 | .699 | 32 | <.001 | ||||||
| NovelvsR2 C1 | .115 | .107 | . 140 | .378 | .156 | .193 | .057 | .447 | .055 | .643 | .100 | .459 | ||||||||||||
| Diagnosis | .310 | .132 | .017 | .923 | .039 | .764 | .092 | .284 | .007 | .957 | −.089 | .550 | ||||||||||||
| C1xDiagnosis | −.019 | .908 | −.263 | .042† | −.024 | .804 | −.087 | .169 | −.206 | .042† | −.175 | .128 | ||||||||||||
| Regression 2 | .359 | 30 | .045 | .617 | 30 | <.001 | .757 | 32 | <.001 | .903 | 32 | <.001 | .739 | 32 | <.001 | .684 | 32 | <.001 | ||||||
| NovelvsR2 C3 | .155 | .496 | .160 | .344 | .042 | .734 | .024 | .757 | .050 | .698 | .079 | .583 | ||||||||||||
| Diagnosis | .292 | .142 | .028 | .875 | .119 | .342 | .117 | .164 | .041 | .755 | −.064 | .663 | ||||||||||||
| C3xDiagnosis | −.097 | .597 | −.238 | .099 | .041 | .707 | −.064 | .355 | −.108 | .338 | −.121 | .335 | ||||||||||||
| Regression 3 | .382 | 30 | .029 | .624 | 30 | <.001 | .753 | 32 | <.001 | .903 | 32 | <.001 | .733 | 32 | <.001 | .692 | 32 | <.001 | ||||||
| NovelvsR2 C4 | .256 | .214 | .166 | .278 | .020 | .863 | .044 | .552 | .018 | .883 | .048 | .720 | ||||||||||||
| Diagnosis | .280 | .124 | .108 | .520 | .122 | .303 | .128 | .107 | .082 | .514 | −.018 | .898 | ||||||||||||
| C4xDiagnosis | −.060 | .722 | −.240 | .076 | .011 | .921 | −.063 | .358 | −.048 | .662 | −.159 | .192 | ||||||||||||
*p-value is significant at Bonferroni-corrected value of .017; †p-value is significant at trend level; Each regression included age, gender, and education as covariates; NovelvsR2 C1 = Level of activation in Cluster 1 for the novel vs. repeated twice conditions; β = Beta; R2= R squared; df = degrees of freedom; NovelvsR2 C3 = Level of activation in Cluster 3 for the novel vs. repeated twice conditions; NovelvsR2 C4 = Level of activation in Cluster 4 for the novel vs. repeated twice conditions; C1xDiagnosis = Interaction term which was generated by multiplying activation in Cluster 1 and diagnosis coded as −.5 for the mild cognitive impairment group and .5 for the healthy control group; C3xDiagnosis = Interaction term which was generated by multiplying activation in Cluster 3 and diagnosis coded as −.5 for the mild cognitive impairment group and .5 for the healthy control group; C4xDiagnosis = Interaction term which was generated by multiplying activation in Cluster 4 and diagnosis coded as −.5 for the mild cognitive impairment group and .5 for the healthy control group.
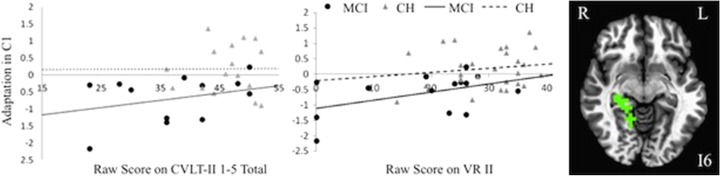
Time 2. The MCI and CH groups were combined, and age, education, gender, Time 1 neuropsychological performance on each specific test, diagnosis, PSC, and a diagnosis by PSC interaction were regressed onto six Time 2 neuropsychological tests. An interaction between diagnosis and repetition-dependent activity reduction in Cluster 1 (parahippocampal gyrus, thalamus, fusiform gyrus, lingual gyrus) was observed. After controlling for age, gender, and education, the relationship between activity reduction (lower PSC for the repeated twice vs. novel stimuli) and Time 2 performance on WMS-R Visual Reproduction Delayed recall (B = −.26, p = .042) and CVLT-II List A 1–5 Total (B = −.21, p = .042) was greater for those with MCI than the CH group, however, these did not survive Bonferroni correction for multiple comparisons (p < .017; see Fig. 5). The main effects for group were not significant in any analyses (all p's > .017). (The 9 participants (3 CHs and 6 with MCI) that were lost to follow-up did not significantly differ from the 40 participants who remained in the study on demographic variables (e.g., age, education, gender). Further, the 6 participants with MCI that were lost to follow-up did not significantly differ from the 14 participants that remained in the study on demographic (e.g., age, education, gender) or cognitive variables (e.g., DRS, WMS-R Visual Reproduction Immediate or Delayed Recall, WMS-R Verbal Reproduction Immediate Delayed Recall, CVLT-II List A 1–5 Total or Long Delay Free Recall scores).
Fig. 5.
Relationship between adaptation and neuropsychological test performance at Year 2 scan (R = Right; L = Left; I = Inferior; CVLT-II = California Verbal Learning Test-Second Edition Trials 1–5 Total Raw score; VR II = Wechsler Memory Scale—Revised Visual Reproduction Delayed recall subtest).
Discussion
As hypothesized, decreased BOLD activation upon repeated stimuli in MTL regions was preferentially observed for CHs versus older adults with MCI. Within the MCI group, repetition-dependent activity reduction was observed to a greater degree for the naMCI group, compared to the aMCI group, suggesting that naMCIs are more similar to CHs and that the aMCI group may have driven the MCI versus CH group differences. Furthermore, greater repetition-dependent activity reduction was significantly associated with better recognition of face-name pairs on the post-scan behavioral task in the MCI group, but not the CHs.
There was some evidence that increased repetition-dependent activity reduction to face-name stimuli was associated with better performance on neuropsychological tests of visual memory during Time 1 (the year of the scan) for CHs, and to a lesser degree for the MCI group. Finally, increased repetition-dependent activity reduction during the scan was predictive of better visual and verbal memory 1 year after the scan in those with MCI (although this finding should be interpreted with caution because it did not reach significance after Bonferroni correction was applied). The pattern of findings in this study suggest that repetition-dependent activity reduction reflects “successful adaptation” to, or encoding of, repeated face-name stimuli in the CH and naMCI groups, and lack of this reduction may reflect “faulty adaptation” and lack of encoding in the aMCI group. The notion that repetition-dependent reduced neural activity is indicative of successful encoding and memory consolidation is supported by the fact that the CH group outperformed the MCI group during the post-scan recognition task for face-name pairs that were repeated twice as well as for those that were never seen. Additionally, increased repetition-dependent activity reduction in MTL regions during the face-name associative encoding task was positively associated with better post-scan recognition memory performance for repeated face-name pairs preferentially for those with MCI, suggesting that repetition-dependent activity reduction was indicative of successful encoding and consolidation of task stimuli in the MCI group, and represents “successful adaptation” to repeated face-name pairs. This finding has also been supported by past research, which has found less repetition-dependent activity reduction in those with MCI and associated decreases in memory for that stimuli (Pihlajamäki et al., 2011). It is unclear why we found a relationship between repetition-dependent activity reduction and post-scan recognition memory performance in the MCI group, but not the CH group. Examining the range of recognition scores and PSC of the clusters in the CH group suggests that restricted range or ceiling effects did not impact our ability to detect a relationship in the CH group. Although speculative, one possibility is that there may be a threshold of repetition-dependent activity reduction above which degree of activity reduction no longer benefits successful encoding performance. In other words, once a specific threshold of activity reduction is surpassed, its benefit on successful encoding is no longer incurred. It is possible that most CHs surpassed this hypothetical threshold. Given lower activity reduction overall in the MCI group, this may explain the differential relationship between recognition performance and activity reduction in MCIs but not HCs. Future studies should investigate this hypothesis if the present study is replicated.
Further support for the idea that repetition-dependent activity reduction represents successful encoding is the positive relationships between increased repetition-dependent activity reduction (i.e., adaptation) and better performance on neuropsychological measures (immediate and delayed visual memory in the CH group and immediate visual memory in the MCI group). Conversely, less repetition-dependent activity reduction was related to poorer performance on Time 2 memory measures in the MCI group, after controlling for Time 1 performance. Although this finding did not reach significance when Bonferroni correction was applied, if replicated in future studies with larger sample sizes it supports the notion that a lack of activity reduction to repeated stimuli is predictive of future cognitive decline. We did not observe any significant relationships between increased activity reduction and verbal memory measures administered at the time of the scan. It is possible that the visual nature of the task makes it more likely to be predictive of performance on tasks of visual memory. In contrast to our findings, Pihlajamäki and colleagues (2011) found a significant relationship between greater activity reduction to repeated face-name stimuli and better performance on delayed recall of verbal memory when combining older adults with MCI and CHs, but they did not include a measure of visual memory. However, we conducted separate analyses within the MCI and CH groups to reduce circularity, which may have reduced power to detect significant effects for verbal memory.
There was also less repetition-dependent activity reduction in the MCI group compared to CHs for face-name pairs repeated twice compared to those that were novel or repeated once in various temporal and subcortical regions, including the MTL. Past research has also demonstrated this in older adults with MCI compared to healthy controls in MTL regions (Johnson et al., 2004; Pihlajamäki et al., 2011), however, these studies did not evaluate regions outside of the MTL. Our findings revealed various regions outside of the MTL activated to a significantly greater degree in the MCI group compared to CHs after repeated stimuli, including the thalamus, caudate, fusiform gyrus, and cingulate. These regions have been implicated in successful memory encoding and/or retrieval in healthy older adults and those with MCI (Hampstead, Khoshnoodi, Yan, Deshpande, & Sathia, 2016; S.D. Han, et al., 2012; Machulda et al., 2009; Xie et al., 2016). Our findings suggest that, in addition to MTL regions, these non-MTL regions are also involved in adjusting to repeated stimuli for the MCI group and may contribute to the encoding and consolidation of information. A pattern of reduced activation in hippocampal regions and increase activity in other brain regions has been observed in previous fMRI studies of MCI and has been suggested to reflect compensation (Gigi, Babai, Penker, Hendler, & Korczyn, 2010). However, the present study did not directly test this hypothesis.
The greatest between-group neuroimaging differences in repetition effects, and the greatest association between neuroimaging and cognitive decline, were lateralized to the right hemisphere. The significance of this right-sided laterality is unclear. However, this set of results is potentially consistent with the “right hemi-aging model” (Dolcos, Rice, & Cabeza, 2002), which suggests that age-associated pathological changes impact right hemisphere functions earlier than left hemisphere functions. Previous work from our research group detected differences in right hippocampal activity according to genetic risk for AD (APOE ε4 allele presence) among older adults without dementia (Han et al., 2007). In the present study, differences between the MCI and CH groups in BOLD activity to repeated face-name stimuli were observed in predominantly right hemisphere regions. Furthermore, these neuroimaging findings are linked with longitudinal performance on a measure of visual memory, commonly attributed to right hemisphere functions. Altogether, the results from the present study suggest some support for this hypothesis.
In comparing activation patterns across repeated stimuli between the MCI subtypes, we found that the naMCI group showed decreased activation in the left hippocampus and left inferior frontal gyrus for face-name pairs repeated once versus novel pairs whereas the aMCI group did not. Given these findings, it is possible that the aMCI group was driving group differences between those with MCI and CHs. Current research suggests that individuals with an amnestic subtype of MCI (single or multi-domain) are more likely to develop AD than other subtypes of MCI (e.g., non-amnestic MCI; Espinosa et al., 2013; Jungwirth et al., 2012; Ravaglia et al., 2005; Yaffe, Petersen, Lindquist, Kramer, & Miller, 2006). Although there is evidence that both amnestic and non-amnestic subtypes are more likely to convert to AD than other neurodegnerative conditions (J. W. Han et al., 2012; Rountree et al., 2007), research also points to the possibility that non-amnestic subtypes are early manifestations of other neurodegenerative diseases (e.g., dementia with Lewy bodies, frontotemporal dementia, vascular dementia; Petersen et al., 2009). Very few studies have directly evaluated aMCI and naMCI groups using fMRI memory encoding paradigms, but one study that employed a complex visual encoding and recognition task in which pictures were shown once to participants failed to find differences in activation between the two MCI subtypes (Machulda et al., 2009). It is possible that utilization of encoding paradigms that allow for the examination of neural activity over repeated stimuli may be particularly well suited to detect differences between MCI subtypes.
One possibility for decreased repetition-dependent activity reduction in older adults with MCI compared to CHs relates to decreased integrity of functional networks. Research points to the possibility that impaired functional connectivity in regions within the default mode network such as the posterior cingulate cortex may be responsible for cognitive decline in prodromal AD (De Vogelaere, Santens, Achten, Boon, & Vingerhoets, 2012). Consistent with our findings that naMCI show greater repetition-dependent activity reduction than aMCI, Dunn and colleagues (2014) found associations between poor episodic verbal memory and reduced functional connectivity between the hippocampus and the posterior cingulate in older adults with aMCI but not those with naMCI, even after controlling for hippocampal volume. This decrease in functional connectivity may impair the ability of the hippocampus to successfully communicate with other regions important for memory encoding and consolidation, thus impacting the ability of these regions to adapt to repeated stimuli over time. Future research is warranted to evaluate whether these changes in connectivity underlie “faulty adaptation” to repeated stimuli in older adults with aMCI.
The present study had several limitations that should be noted. The sample sizes of the two MCI subgroups were small, and therefore replication of these results is necessary with larger samples. Although there have been recent concerns raised in committing Type I errors when using less stringent p-values, research using clinical populations in which smaller sample sizes are the norm is also susceptible to a greater likelihood of missing important relationships (Lieberman & Cunningham, 2009). Given our clinically relevant longitudinal data in individuals with MCI, taken together with large effect sizes of significant clusters (d = .74–.9), we believe that using a less stringent p-value allows us to present important findings regarding the neurofunctional and behavioral changes associated with prodromal AD which will provide other research groups the transparency needed to further test these questions. Additionally, a subset of the neuropsychological measures used to create the diagnostic groups were used as outcome measures. Of note, our study utilized a comprehensive diagnostic system that required at least two performances within a cognitive domain to be greater than one standard deviation below age-appropriate norms and thus groups were not solely classified based on performance on one memory measure. This comprehensive technique has been shown to be more stable over time and to have better associations with biomarkers and clinical outcomes (Bondi et al., 2014; Edmonds et al., 2016; Jak et al. 2009b). Additionally, because analyses investigating relationships between adaptation during the fMRI task and neuropsychological test performance were conducted within each diagnostic group, circularity was likely avoided. Furthermore, although the MCI and CH groups were combined when evaluating associations between neuropsychological performance 1 year post-scan, diagnosis and the neuropsychological test data from the previous year were included as covariates in the analyses in order to detect change in performance over time. Another potential limitation of our study is the fact that ANART scores were slightly higher for the CHs than the MCI group. The neuropsychological regression results were replicated with ANART scores as a covariate in place of education level; thus, it is unlikely that this accounts for the present findings. Additionally, because the same neuropsychological tests were given 1 year apart, it is possible that practice effects were present. Finally, although a portion of the participants did not return for the Time 2 neuropsychological assessment, there were no significant differences in demographic or clinical variables between that group and those who did return for follow-up testing. Therefore, it is unlikely that selective attrition accounted for the longitudinal findings.
Conclusions
Previous research has demonstrated that older adults with MCI do not exhibit the pattern of repetition-dependent reduction in MTL activity with exposure to repeated stimuli that is characteristic of CHs. We replicated previous studies reporting reduced repetition-dependent activity reduction in MCIs, extending the phenomenon to regions outside of MTL structures, and relating it to performance on a behavioral version of the task and on neuropsychological measures. Our findings also support the notion that repetition-dependent activity reduction likely represents successful encoding and consolidation of memories, and that lack thereof may reflect “faulty adaptation” to repeated stimuli. Additionally, we differentiated between patterns of activation to repeated stimuli in older adults with aMCI versus naMCI, highlighting the importance of assessing MCI subtypes and validating the use of our actuarial criteria for diagnosing subtypes of MCI. Our findings also provide support for the utility of face-name encoding paradigms in investigating distinct underlying neurobiological substrates related to subtypes of MCI. Finally, although findings did not survive Bonferroni correction and require replication, longitudinal follow-up of the participants suggest that associative encoding tasks may be predictive of future cognitive decline and thus prove useful in identifying those individuals at most risk of developing AD. Studies with larger samples and the use of functional connectivity techniques, biomarkers, and longitudinal data are recommended to further our understanding of “faulty adaptation” and its clinical implications for individuals with prodromal AD.
Funding
This work was supported by the Alzheimer's Association [grant number IIRG 07–59343], and the National Institute on Aging [K24 AG026431 and R01 AG049810].
Conflict of Interest
None declared.
Acknowledgments
The authors report there are no conflict of interest disclosures.
References
- Albert M. S., Moss M. B., Tanzi R., & Jones K. (2001). Preclinical prediction of AD using neuropsychological tests. Journal of the International Neuropsychological Society, 7, 631–639. [DOI] [PubMed] [Google Scholar]
- Alzheimer's Association. (2014). 2014 Alzheimer's disease facts and figures. Alzheimer's & Dementia, 10, e47–e92. [DOI] [PubMed] [Google Scholar]
- Bangen K. J., Jak A. J., Schiehser D. M., Delano-Wood L., Tuminello E., Han S., et al. (2010). Complex activities of daily living vary by mild cognitive impairment subtype. Journal of the International Neuropsychological Society, 16, 630–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylis G., & Rolls E. (1987). Responses of neurons in the inferior temporal cortex in short term and serial recognition memory tasks. Experimental Brain Research, 65, 614–622. [DOI] [PubMed] [Google Scholar]
- Birn R. M., Saad Z. S., & Bandettini P. A. (2001). Spatial heterogeneity of the nonlinear dynamics in the FMRI BOLD response. Neuroimage, 14, 817–826. [DOI] [PubMed] [Google Scholar]
- Bondi M. W., Edmonds E. C., Jak A. J., Clark L. R., Delano-Wood L., McDonald C. R., et al. (2014). Neuropsychological criteria for mild cognitive impairment improves diagnostic precision, biomarker associations, and progression rates. Journal of Alzheimer's Disease, 42, 275–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braak H., & Braak E. (1991). Neuropathological stageing of Alzheimer-related changes. Acta Neuropathologica, 82, 239–259. [DOI] [PubMed] [Google Scholar]
- Brewer J. B., & Moghekar A. (2002). Imaging the medial temporal lobe: exploring new dimensions. Trends in Cognitive Sciences, 6, 217–223. [DOI] [PubMed] [Google Scholar]
- Brown M., Wilson F., & Riches I. (1987). Neuronal evidence that inferomedial temporal cortex is more important than hippocampus in certain processes underlying recognition memory. Brain Research, 409, 158–162. [DOI] [PubMed] [Google Scholar]
- Busse A., Hensel A., Gühne U., Angermeyer M., & Riedel-Heller S. (2006). Mild cognitive impairment long-term course of four clinical subtypes. Neurology, 67, 2176–2185. [DOI] [PubMed] [Google Scholar]
- Chang Y. L., Bondi M. W., Fennema-Notestine C., McEvoy L. K., Hagler D. J., Jacobson M. W., et al. (2010). Brain substrates of learning and retention in mild cognitive impairment diagnosis and progression to Alzheimer's disease. Neuropsychologia, 48, 1237–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua T. C., Wen W., Chen X., Kochan N., Slavin M. J., Trollor J. N., et al. (2009). Diffusion tensor imaging of the posterior cingulate is a useful biomarker of mild cognitive impairment. The American Journal of Geriatric Psychiatry, 17, 602–613. [DOI] [PubMed] [Google Scholar]
- Coutinho A. M., Porto F. H., Duran F. L., Prando S., Ono C. R., Feitosa E. A., et al. (2015). Brain metabolism and cerebrospinal fluid biomarkers profile of non-amnestic mild cognitive impairment in comparison to amnestic mild cognitive impairment and normal older subjects. Alzheimer's Research & Therapy, 7 (1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox R. W. (1996). AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Computers and Biomedical Research, 29, 162–173. [DOI] [PubMed] [Google Scholar]
- D'agostino R. B., Wolf P. A., Belanger A. J., & Kannel W. B. (1994). Stroke risk profile: adjustment for antihypertensive medication. The Framingham Study. Stroke, 25(1), 40–43. [DOI] [PubMed] [Google Scholar]
- De Vogelaere F., Santens P., Achten E., Boon P., & Vingerhoets G. (2012). Altered default-mode network activation in mild cognitive impairment compared with healthy aging. Neuroradiology, 54, 1195–1206. [DOI] [PubMed] [Google Scholar]
- DeKosky S. T., & Marek K. (2003). Looking backward to move forward: early detection of neurodegenerative disorders. Science (New York, NY), 302, 830–834. [DOI] [PubMed] [Google Scholar]
- Delis D., Kramer J., Kaplan E., & Ober B. (1999). California Verbal Learning Test—Second Edition (CVLT–II) manual. San Antonio, TX: The Psychological Cooperation: Harcourt Assessment, Inc. [Google Scholar]
- Desimone R. (1996). Neural mechanisms for visual memory and their role in attention. Proceedings of the National Academy of Sciences, 93, 13494–13499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson B. C., & Sperling R. A. (2008). Functional abnormalities of the medial temporal lobe memory system in mild cognitive impairment and Alzheimer's disease: insights from functional MRI studies. Neuropsychologia, 46, 1624–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan R., & Fletcher P. (1999). Encoding and retrieval in human medial temporal lobes: An empirical investigation using functional magnetic resonance imaging (fMRI). Hippocampus, 9, 25–34. [DOI] [PubMed] [Google Scholar]
- Dolcos F., Rice H. J., & Cabeza R. (2002). Hemispheric asymmetry and aging: Right hemisphere decline or asymmetry reduction. Neuroscience & Biobehavioral Reviews, 26, 819–825. [DOI] [PubMed] [Google Scholar]
- Dunn C. J., Duffy S. L., Hickie I. B., Lagopoulos J., Lewis S. J., Naismith S. L., et al. (2014). Deficits in episodic memory retrieval reveal impaired default mode network connectivity in amnestic mild cognitive impairment. NeuroImage: Clinical, 4, 473–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmonds E. C., Delano-Wood L., Jak A. J., Galasko D. R., Salmon D. P., & Bondi M. W. (2016). “Missed” mild cognitive impairment: High false-negative error rate based on conventional diagnostic criteria. Journal of Alzheimer's Disease, 52(2), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichenbaum H. (2004). Hippocampus: Cognitive processes and neural representations that underlie declarative memory. Neuron, 44, 109–120. [DOI] [PubMed] [Google Scholar]
- Elger C. E., Grunwald T., Lehnertz K., Kutas M., Helmstaedter C., Brockhaus A., et al. (1997). Human temporal lobe potentials in verbal learning and memory processes. Neuropsychologia, 35, 657–667. [DOI] [PubMed] [Google Scholar]
- Espinosa A., Alegret M., Valero S., Vinyes-Junqué G., Hernández I., Mauleón A., et al. (2013). A longitudinal follow-up of 550 mild cognitive impairment patients: Evidence for large conversion to dementia rates and detection of major risk factors involved. Journal of Alzheimer's Disease, 34, 769–780. [DOI] [PubMed] [Google Scholar]
- Fernández G., Effern A., Grunwald T., Pezer N., Lehnertz K., Dümpelmann M., et al. (1999). Real-time tracking of memory formation in the human rhinal cortex and hippocampus. Science (New York, NY), 285, 1582–1585. [DOI] [PubMed] [Google Scholar]
- Festa E. K., Insler R. Z., Salmon D. P., Paxton J., Hamilton J. M., & Heindel W. C. (2005). Neocortical disconnectivity disrupts sensory integration in Alzheimer's disease. Neuropsychology, 19, 728. [DOI] [PubMed] [Google Scholar]
- Fischer P., Jungwirth S., Zehetmayer S., Weissgram S., Hoenigschnabl S., Gelpi E., et al. (2007). Conversion from subtypes of mild cognitive impairment to Alzheimer dementia. Neurology, 68, 288–291. [DOI] [PubMed] [Google Scholar]
- Gigi A., Babai R., Penker A., Hendler T., & Korczyn A. D. (2010). Prefrontal compensatory mechanism may enable normal semantic memory performance in mild cognitive impairment (MCI). Journal of Neuroimaging, 20, 163–168. [DOI] [PubMed] [Google Scholar]
- Golby A., Silverberg G., Race E., Gabrieli S., O'shea J., Knierim K., et al. (2005). Memory encoding in Alzheimer's disease: an fMRI study of explicit and implicit memory. Brain, 128, 773–787. [DOI] [PubMed] [Google Scholar]
- Grunwald T., Elger C. E., Lehnertz K., Van Roost D., & Heinze H. (1995). Alterations of intrahippocampal cognitive potentials in temporal lobe epilepsy. Electroencephalography and Clinical Neurophysiology, 95, 53–62. [DOI] [PubMed] [Google Scholar]
- Grunwald T., Lehnertz K., Heinze H. J., Helmstaedter C., & Elger C. E. (1998). Verbal novelty detection within the human hippocampus proper. Proceedings of the National Academy of Sciences, 95, 3193–3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampstead B. M., Khoshnoodi M., Yan W., Deshpande G., & Sathian K. (2016). Patterns of effective connectivity during memory encoding and retrieval differ between patients with mild cognitive impairment and healthy older adults. NeuroImage, 124, 997–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han J. W., Kim T. H., Lee S. B., Park J. H., Lee J. J., Huh Y., et al. (2012). Predictive validity and diagnostic stability of mild cognitive impairment subtypes. Alzheimer's & Dementia, 8, 553–559. [DOI] [PubMed] [Google Scholar]
- Han S. D., Arfanakis K., Fleischman D. A., Leurgans S. E., Tuminello E. R., Edmonds E. C., et al. (2012). Functional connectivity variations in mild cognitive impairment: associations with cognitive function. Journal of the International Neuropsychological Society, 18, 39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han S. D., Houston W. S., Jak A. J., Eyler L. T., Nagel B. J., Fleisher A. S., et al. (2007). Verbal paired-associate learning by APOE genotype in non-demented older adults: fMRI evidence of a right hemispheric compensatory response. Neurobiology of Aging, 28, 238–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henson R., & Rugg M. (2003). Neural response suppression, haemodynamic repetition effects, and behavioural priming. Neuropsychologia, 41, 263–270. [DOI] [PubMed] [Google Scholar]
- Hyman B. T., Van Hoesen G. W., Damasio A. R., & Barnes C. L. (1984). Alzheimer's disease: Cell-specific pathology isolates the hippocampal formation. Science (New York, N.Y.), 225, 1168–1170. [DOI] [PubMed] [Google Scholar]
- Jack C., Petersen R. C., Xu Y. C., O'Brien P. C., Smith G. E., Ivnik R. J., et al. (1999). Prediction of AD with MRI-based hippocampal volume in mild cognitive impairment. Neurology, 52, 1397–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jak A. J., Bangen K. J., Wierenga C. E., Delano‐Wood L., Corey‐Bloom J., & Bondi M. W. (2009. a). Contributions of neuropsychology and neuroimaging to understanding clinical subtypes of mild cognitive impairment. International Review of Neurobiology, 84, 81–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jak A. J., Bondi M. W., Delano-Wood L., Wierenga C., Corey-Bloom J., Salmon D. P., et al. (2009. b). Quantification of five neuropsychological approaches to defining mild cognitive impairment. The American Journal of Geriatric Psychiatry, 17, 368–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson S. C., Baxter L. C., Susskind-Wilder L., Connor D. J., Sabbagh M. N., & Caselli R. J. (2004). Hippocampal adaptation to face repetition in healthy elderly and mild cognitive impairment. Neuropsychologia, 42, 980–989. [DOI] [PubMed] [Google Scholar]
- Johnson S. C., Schmitz T. W., Asthana S., Gluck M. A., & Myers C. (2008). Associative learning over trials activates the hippocampus in healthy elderly but not mild cognitive impairment. Aging, Neuropsychology, and Cognition, 15, 129–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jungwirth S., Zehetmayer S., Hinterberger M., Tragl K. H., & Fischer P. (2012). The validity of amnestic MCI and non-amnestic MCI at age 75 in the prediction of Alzheimer's dementia and vascular dementia. International Psychogeriatrics, 24, 959–966. [DOI] [PubMed] [Google Scholar]
- Kukull W. A., Higdon R., Bowen J. D., McCormick W. C., Teri L., Schellenberg G. D., et al. (2002). Dementia and Alzheimer disease incidence: a prospective cohort study. Archives of Neurology, 59, 1737–1746. [DOI] [PubMed] [Google Scholar]
- Leirer V. O., Morrow D. G., Sheikh J. I., & Pariante G. M. (1990). Memory skills elders want to improve. Experimental Aging Research, 16, 155–158. [DOI] [PubMed] [Google Scholar]
- Libon D. J., Bondi M. W., Price C. C., Lamar M., Eppig J., Wambach D. M., et al. (2011). Verbal serial list learning in mild cognitive impairment: A profile analysis of interference, forgetting, and errors. Journal of the International Neuropsychological Society, 17, 905–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman M. D., & Cunningham W. A. (2009). Type I and Type II error concerns in fMRI research: Re-balancing the scale. Social Cognitive and Affective Neuroscience, 4, 423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb P. (1996). ILS: Independent living scales manual. San Antonio, TX: Psychological Corp: Harcourt Brace Jovanovich. [Google Scholar]
- Machulda M. M., Senjem M. L., Weigand S. D., Smith G. E., Ivnik R. J., Boeve B. F., et al. (2009). Functional MRI changes in amnestic and non-amnestic MCI during encoding and recognition tasks. Journal of the International Neuropsychological Society, 15, 372–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattis S. (1988). Dementia rating scale: DRS: Professional Manual: PAR.
- Pedraza O., Smith G. E., Ivnik R. J., Willis F. B., Ferman T. J., Petersen R. C., et al. (2007). Reliable change on the dementia rating scale. Journal of the International Neuropsychological Society, 13, 716–720. [DOI] [PubMed] [Google Scholar]
- Petersen R. C. (2004). Mild cognitive impairment as a diagnostic entity. Journal of Internal Medicine, 256, 183–194. [DOI] [PubMed] [Google Scholar]
- Petersen R. C., Roberts R. O., Knopman D. S., Boeve B. F., Geda Y. E., Ivnik R. J., et al. (2009). Mild cognitive impairment: ten years later. Archives of Neurology, 66, 1447–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pihlajamäki M., DePeau K. M., Blacker D., & Sperling R. A. (2008). Impaired medial temporal repetition suppression is related to failure of parietal deactivation in Alzheimer disease. The American Journal of Geriatric Psychiatry, 16, 283–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pihlajamäki M., O'Keefe K., O’Brien J., Blacker D., & Sperling R. A. (2011). Failure of repetition suppression and memory encoding in aging and Alzheimer's disease. Brain Imaging and Behavior, 5, 36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M., Guerchet M., & Prina M. (2015). The epidemiology and impact of dementia: Current state and future trends. Geneva: World Health Organization. [Google Scholar]
- Rand-Giovannetti E., Chua E. F., Driscoll A. E., Schacter D. L., Albert M. S., & Sperling R. A. (2006). Hippocampal and neocortical activation during repetitive encoding in older persons. Neurobiology of Aging, 27, 173–182. [DOI] [PubMed] [Google Scholar]
- Ravaglia G., Forti P., Maioli F., Martelli M., Servadei L., Brunetti N., et al. (2005). Conversion of mild cognitive impairment to dementia: Predictive role of mild cognitive impairment subtypes and vascular risk factors. Dementia and Geriatric Cognitive Disorders, 21, 51–58. [DOI] [PubMed] [Google Scholar]
- Riches I., Wilson F., & Brown M. W. (1991). The effects of visual stimulation and memory on neurons of the hippocampal formation and the neighboring parahippocampal gyrus and inferior temporal cortex of the primate. The Journal of Neuroscience, 11, 1763–1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringo J. L. (1996). Stimulus specific adaptation in inferior temporal and medial temporal cortex of the monkey. Behavioural Brain Research, 76, 191–197. [DOI] [PubMed] [Google Scholar]
- Rountree S. D., Waring S. C., Chan W. C., Lupo P. J., Darby E. J., & Doody R. S. (2007). Importance of subtle amnestic and nonamnestic deficits in mild cognitive impairment: Prognosis and conversion to dementia. Dementia and Geriatric Cognitive Disorders, 24, 476–482. [DOI] [PubMed] [Google Scholar]
- Serra L., Giulietti G., Cercignani M., Spanò B., Torso M., Castelli D., et al. (2013). Mild cognitive impairment: Same identity for different entities. Journal of Alzheimer's Disease, 33, 1157–1165. [DOI] [PubMed] [Google Scholar]
- Sperling R., Chua E., Cocchiarella A., Rand-Giovannetti E., Poldrack R., Schacter D. L., et al. (2003). Putting names to faces: Successful encoding of associative memories activates the anterior hippocampal formation. Neuroimage, 20, 1400–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperling R. (2007). Functional MRI studies of associative encoding in normal aging, mild cognitive impairment, and Alzheimer's disease. Annals of the New York Academy of Sciences, 1097, 146–155. [DOI] [PubMed] [Google Scholar]
- Stoub T. R., Stebbins G. T., Leurgans S., Bennett D. A., & Shah R. C. (2006). Hippocampal disconnection contributes to memory dysfunction in individuals at risk for Alzheimer's disease. Proceedings of the National Academy of Sciences, 103, 10041–10045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strange B., Fletcher P., Henson R., Friston K., & Dolan R. (1999). Segregating the functions of human hippocampus. Proceedings of the National Academy of Sciences, 96, 4034–4039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talairach P., & Tournoux J. (1988). A stereotactic coplanar atlas of the human brain: Stuttgart: Thieme.
- Vannini P., Hedden T., Sullivan C., & Sperling R. A. (2013). Differential functional response in the posteromedial cortices and hippocampus to stimulus repetition during successful memory encoding. Human Brain Mapping, 34, 1568–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vannini P., O'brien J., O’keefe K., Pihlajamäki M., Laviolette P., & Sperling R. A. (2011). What goes down must come up: Role of the posteromedial cortices in encoding and retrieval. Cerebral Cortex, 21, 22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. (1987). WMS-R: Wechsler memory scale-revised: Psychological Corporation.
- Wierenga C. E., & Bondi M. W. (2007). Use of functional magnetic resonance imaging in the early identification of Alzheimer's disease. Neuropsychology Review, 17, 127–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggs C. L., & Martin A. (1998). Properties and mechanisms of perceptual priming. Current Opinion in Neurobiology, 8, 227–233. [DOI] [PubMed] [Google Scholar]
- Wolk D. A., Price J. C., Saxton J. A., Snitz B. E., James J. A., Lopez O. L., et al. (2009). Amyloid imaging in mild cognitive impairment subtypes. Annals of Neurology, 65, 557–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie L., Dolui S., Das S. R., Stockbower G. E., Daffner M., Rao H., et al. (2016). A brain stress test: Cerebral perfusion during memory encoding in mild cognitive impairment. NeuroImage: Clinical, 11, 388–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe K., Petersen R. C., Lindquist K., Kramer J., & Miller B. (2006). Subtype of mild cognitive impairment and progression to dementia and death. Dementia and Geriatric Cognitive Disorders, 22, 312–319. [DOI] [PubMed] [Google Scholar]
- Yesavage J. A., Brink T. L., Rose T. L., Lum O., Huang V., Adey M., & Leirer V. O. (1983). Development and validation of a geriatric depression screening scale: a preliminary report. Journal of Psychiatric Research, 17(1), 37–49. [DOI] [PubMed] [Google Scholar]
- Zelinski E., & Gilewski M. (1988). Assessment of memory complaints by rating scales and questionnaires. Psychopharmacology Bulletin, 24, 523. [PubMed] [Google Scholar]
- Zhuang L., Wen W., Zhu W., Trollor J., Kochan N., Crawford J., et al. (2010). White matter integrity in mild cognitive impairment: a tract-based spatial statistics study. Neuroimage, 53, 16–25. [DOI] [PubMed] [Google Scholar]