Abstract
Study Objectives
The importance of sleep for health necessitates investigation of disparities in multiple aspects of sleep. Given the potential disruption to sleep posed by the well-documented discrimination experienced by sexual minorities, disparities related to sexual minority status warrant such attention. This study sought to (1) measure differences in same- and different-sex couples in sleep duration and perceived restedness, (2) examine how the link between sleep duration and restedness varied among same- and different-sex couples, and (3) assess variation in restedness across state-level sexual minority indicators.
Methods
Participants in the Wellbeing Module of the American Time Use Survey, assessed in 2010, 2012, and 2013 (n = 17378), completed time diaries assessing sleep duration and evaluated their own restedness.
Results
Multinomial and ordinal regression analyses showed no links between partner sex and sleep among men. Women with same-sex partners reported lower restedness than women with different-sex partners, and perceptions of restedness were more strongly linked to sleep duration for the former than the latter. Finally, women with the same-sex partners living in states more supportive of sexual minorities reported better restedness than those in less supportive states.
Conclusions
Women with same-sex partners were vulnerable to lower restedness, especially when they reported lower sleep duration or were in less supportive environments. Such disparities could underlie related disparities in health, as sleep health is predictive of health outcomes. Future research is needed to explore the role of sleep in explaining variation in health outcomes among sexual minority women.
Keywords: sexual minority, same-sex couples, sleep duration, restedness, public health, sleep and stress, sleep in women
Statement of Significance
Sexual minority populations are more vulnerable than heterosexual populations for negative outcomes associated with poor sleep health. This paper compares restedness and sleep duration among individuals in same-sex relationships and in different-sex relationships using data from the Health and Wellbeing Module of the American Time Use Survey. This is the first study to use time-diary data to compare sleep health among same- and different-sex couples, and to do so with nationally representative data. Women in same-sex couples reported less restedness than their peers in different-sex couples, and these differences were exacerbated by sleep duration and state-level differences in sexual minorities acceptance. No significant differences were observed among men. Sleep health may be important for understanding health disparities among sexual minority women.
Introduction
Insufficient sleep has been declared a public health problem by the Center for Disease Control [1]. This declaration reflects the associations of sleep health with depression, obesity, cardiovascular health problems, and all-cause mortality as well as the annual economic cost of poor sleep health, which is estimated at 411 billion dollars a year [2]. Because such health conditions tend to be over-represented in disadvantaged segments of the population, disparities in sleep health could reflect and drive broad patterns of health inequality in the United States, emphasizing the importance of identifying groups at heightened vulnerability that need special attention. Indeed, many historically disenfranchised and stigmatized groups in the United States do report worse sleep health compared with more privileged groups [3, 4], and the degree to which this pattern extends to a group of Americans receiving increasing public health attention—sexual minorities (e.g. individuals with nonheterosexual identities, who report same-sex sexual or romantic partners, or who report same sex attraction)—needs to be examined. A growing literature suggests that sexual minorities, including those living in same-sex couples, are at increased risk for poorer health outcomes across the lifecourse [5–9], and theory (e.g. minority stress) and past studies on related topics (e.g. poor health) suggest that sexual minorities are likely to be vulnerable for many of the negative health outcomes associated with problematic sleep duration and sleep quality [10–14]. This study, therefore, seeks to document various disparities in sleep duration and restedness related to living in same-sex couples within a sample that is nationally representative [15].
Sleep health is a multifacetted construct [16], and different assessments of sleep (e.g. duration and feelings of restedness) are differentially associated with health outcomes. Both under-sleeping (e.g. sleeping less than 7 hr a night) and over-sleeping (e.g. more than nine hours a night), as measured by sleep-diary data (such as the time-diary data in the ATUS), are associated with worse health outcomes [17]. Importantly, subjective assessments of sleep (i.e. perceived quality of sleep such as feelings of restedness), although only moderately linked with both self-rated sleep duration and other more objective measures of sleep quality (e.g. polysomnographic testing and actigraph testing) [12, 18], may be more strongly linked with health outcomes than sleep duration [19, 20]. Finally, individuals who report both not sleeping enough and low sleep quality, including low levels of restedness, have the worst health outcomes [19, 21, 22].
Given this link between sleep problems and poorer health, the question of why some people—and some groups of people—sleep less or less well than others is important. Many factors can disrupt sleep, but stress plays a key role [23–25]. Previous work has linked higher levels of stress to poorer perceptions of sleep quality [24, 26], suggesting that population groups experiencing more stress may be the most likely to negatively rate the quality of their sleep. Indeed, racial/ethnic minorities and other groups that experience the stress of discrimination tend to have poorer sleep health outcomes [27, 28], and recent work suggests that experiences of victimization partially mediate the association between sexual minority status and sleep quality among Chinese adolescents [9]. This pattern is in line with the basic tenets of minority stress theory and related perspectives on stigma, which argue that the strain associated with discrimination, anticipated discrimination, or internalized stigma increase vulnerability to negative health outcomes among sexual minority populations [29, 30]. Furthermore, in line with minority stress theory, risks to victims’ health and wellbeing will vary according to fluctuations in the prevalence and intensity of negative attitudes, resulting in differential treatment across local contexts [30–32].
The increasingly visible number of sexual minorities in the United States also experience substantial discrimination and related stress, but their sleep patterns vis-à-vis the general population are unclear and need to be studied. Of the studies that have explored sleep among sexual minority adults, three showed disparities in terms of sleep duration or quality [6–8], whereas two showed no differences after controlling for demographic characteristics [5, 33]. Past research has also shown that community-level indicators of sexual minority acceptance (e.g. attitudes toward sexual minorities and laws protecting sexual minority rights) are suggestive of protective contexts for sexual minority health, and that these indicators vary considerably by region [34]. Most importantly, variation in these indicators is linked with variation in health outcomes among sexual minorities [32, 35]. These indicators have not, however, been previously explored as moderators for sleep outcomes.
With this theoretical and empirical grounding, this study integrated time-diary assessments of sleep duration and self-reported restedness in a nationally representative sample of adults with data on state-level assessments of support for sexual minorities to test three hypotheses. The first hypothesis was that compared with individuals with different-sex partners, individuals with same-sex partners would report lower levels of restedness and more problematic sleep duration (e.g. sleeping more than 9 hr or less than 7 hr), especially the latter. The second was that living in a same-sex couple would moderate the association between sleep duration and restedness such that lower amounts of sleep would lead to less restedness for individuals in same-sex couples when compared with individuals in different-sex couples. The third hypothesis was that living in a same-sex couple be more strongly associated with lower levels of restedness in geographic areas less supportive of sexual minority issues. Notably, given evidence that women report more sleep problems than men [36], that subjective and objective assessments of sleep are more similar among men than among women [37], and that sexual minority women have more sleep problems than sexual minority men [6–8], these three hypotheses will be tested separately for men and women. In general, there was an expectation that the hypothesized patterns would be stronger and more consistent for women than men.
Methods
ATUS is a time-diary survey conducted by the U.S. Census Bureau and has been used to previously explore national trends in sleep health [38]. Respondents were randomly chosen from within households that were selected for participation in the Current Population Survey (CPS) [15]. Through semistructured and conversational-style phone interviews, respondents completed a time diary with detailed information on their activities over a 24 hr period. Sociodemographic information for themselves and other household members comes from both the CPS and ATUS. The analytical data for this study were drawn from 2010, 2012, and 2013, which were the years where participants also completed the Well-Being Module that contained additional questions on their health and wellbeing, including restedness.
Measures
Sleep duration
Starting at 4:00 am and running for 24 hr, time diary participants reported when they began sleeping, what time they woke up, and whether they had any sleep interruptions. They also provided information on what time their last activity of the previous day commenced, even if that end time was outside the 24 hr time diary period. The time spent sleeping, starting the second night of the study, to the time they woke up in the morning, was used to assess sleep duration. Individuals (n = 557) were excluded from the current study if they reported less than 4 hr of sleep during that night for two primary reasons. First, a large portion of these respondents did not report going to bed before 3:59 am and so were recorded as having 0 hr sleep (a likely mismatch between the reporting period and actual typical sleep experience). Second, for respondents who reported going to sleep in the evening but for only a brief period (e.g. a disrupted sleep pattern of a shift worker), their night sleep is not indicative of their regular sleep experience throughout the day. Relying on the second night of sleep could be a limitation because respondents are asking about the restedness from the previous night’s sleep while assessing the duration of the subsequent night’s sleep. This approach offers the advantage of providing a more accurate understanding of hours of sleep in a single night, compared with combining parts of the previous and subsequent night’s sleep. Moreover, this measure was correlated with another measure of sleep that captured all sleep periods throughout the 24 hr period (i.e. 4:00 am to 3:59 am), indicating that sleep captured on the second night likely looks similar in a majority of cases to sleep experienced during a 24 hr period. Since both insufficient and too much sleep have been linked with poorer health outcomes [17], sleep duration had three categories for comparison: (1) under sleep (less than 7 hr); (2) normal (7 to 8 hr and 59 min of sleep); and (3) oversleep (9 hr of sleep or more).
Restedness
Participants reported how rested they felt on their diary day on a scale ranging from 1 (not at all) to 4 (very). This measure is similar to previous scales used to assess restdedness [19].
Sex of partner
Respondents reported (1) their own sex (options: male or female), and the sex of and their relationship to each household member. From this information, respondents were dummy coded as being women with other-sex partners (n = 8644), women with same-sex partners (n = 66), men with other-sex partners (n = 8058), or men with same-sex partners (n = 53). This method is frequently used in studies of sexual minority status health with government data [32, 39], and the percentage of individuals in same-sex couples are in line with previous work using similar data [40].
State-level indicators of sexual minority acceptance
Two measures of state-level acceptance of same-sex marriage were assigned to respondents’ based on their states of residence. State-level support of same-sex marriage was measured using aggregate survey data obtained from the Williams Institute that indicated the proportion of adults in each state in 2014 who supported marriage equality (continuous scale) [41]. This method has been used in previous research to assess the link between state-support of same-sex marriage and health outcomes [31]. State-level same-sex marriage laws were a binary measure indicating whether adults could legally marry someone of the same sex in their home state residence during their interview year [42].
Covariates
Several variables were measured to account for key confounds as well as demographic diversity in the sample, including employment status (full time, part time, unemployed, and not working), educational attainment (college degree or more vs. no college degree), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic white, and other race/ethnicity), age (continuous in years), whether respondent had children living in the home (1 = children present), family income (ordinal scale from 1 = less than $5000 through 16 = $150000 and more), geographic region (Northeast, Midwest, South, and West), residence in a metropolitan area (1 = metropolitan area), and time-diary information (whether the diary was recorded on a weekend, and which year [2010, 2012, or 2013]). Table 1 presents a description of these covariates by sexual minority status. Overall, respondents in same-sex partnerships were more socioeconomically and demographically advantaged (e.g. income and education) than those in other-sex partnerships.
Table 1.
Sample description
| Total | Women | Men | ||||
|---|---|---|---|---|---|---|
| Different sex | Same sex | Different sex | Same sex | |||
| n | %/Mean (SD) | %/Mean | ||||
| Actual sleep | ||||||
| 7–9 hr sleep | 8352 | 49.25 | 48.72 | 43.90 | 49.81 | 49.47 |
| Under sleep (less than 7 hr) | 3391 | 21.29 | 19.84* | 13.58 | 22.77† | 23.29 |
| Oversleep (9 hr or more) | 5078 | 29.46 | 31.45* | 42.52 | 27.41† | 27.24 |
| Feelings of restedness | ||||||
| Rested (1–4 scale) | 16821 | 3.16 | 3.13* | 2.89* | 3.20†,‡ | 2.96 |
| (0.85) | (0.88) | (0.79) | (0.83) | (0.90) | ||
| Contextual factors | ||||||
| Support for gay marriage (%) | 16821 | 43.64 | 43.66‡ | 45.24*,† | 43.61‡ | 43.27 |
| (7.19) | (7.16) | (7.84) | (7.22) | (7.41) | ||
| State allows same-sex marriage (0/1) | 2506 | 15.73 | 15.96‡ | 28.83*,†,§ | 15.46‡ | 8.71‡ |
| Covariates | ||||||
| College degree (0/1) | 6835 | 36.32 | 36.34‡,§ | 57.61*,† | 35.97‡,§ | 54.42*,† |
| Employment status | ||||||
| Full-time employed | 9303 | 54.41 | 42.69*,‡,§ | 58.57† | 65.82† | 67.72† |
| Part-time employed | 2215 | 12.89 | 18.12* | 12.18 | 7.74†,§ | 14.28* |
| Unemployed | 697 | 4.08 | 3.99 | 5.30 | 4.18 | 1.18 |
| Not in the labor force | 4605 | 28.61 | 35.19*,‡,§ | 23.95† | 22.26† | 16.82† |
| Family income (1–16 scale) | 16821 | 11.78 | 11.74‡,§ | 12.25 | 11.81†,§ | 12.66*,† |
| (3.53) | (3.56) | (3.59) | (3.49) | (3.73) | ||
| Parent (0/1) | 9281 | 42.09 | 42.21*,‡,§ | 13.68*,†,§ | 42.48†,‡,§ | 7.29*,†,‡ |
| Race/ethnicity | ||||||
| Non-Hispanic white | 12061 | 73.31 | 73.42§ | 79.75 | 73.04§ | 87.40*,† |
| Non-Hispanic black | 1369 | 6.93 | 6.61‡ | 0.46*,† | 7.34‡ | 0.65 |
| Hispanic white | 2245 | 13.19 | 13.16 | 14.77 | 13.23 | 9.11 |
| Other race/ethnicity | 1146 | 6.57 | 6.81* | 5.02 | 6.38† | 2.84 |
| Age (years) | 16821 | 48.82 | 47.94* | 44.15* | 49.78†,‡,§ | 42.24* |
| (15.17) | (15.05) | (14.53) | (15.25) | (10.47) | ||
| Metropolitan area | 13978 | 82.92 | 83.01 | 88.69 | 82.70 | 93.99 |
| Region | ||||||
| Northeast | 2885 | 17.94 | 17.64 | 19.97§ | 18.31§ | 7.10‡,§ |
| Midwest | 4157 | 24.45 | 24.01 | 29.75 | 24.91 | 13.97 |
| West | 3750 | 21.69 | 22.18§ | 27.57 | 21.11§ | 28.94*,† |
| South | 6029 | 35.92 | 36.17‡ | 22.71†,§ | 35.67 | 49.99‡ |
| Weekend | 4221 | 28.80 | 28.73 | 31.78* | 28.85‡ | 29.00 |
| Year | ||||||
| 2010 | 6089 | 33.13 | 32.91 | 31.09 | 33.39 | 28.41 |
| 2012 | 5621 | 33.32 | 33.26 | 35.20 | 33.38 | 30.37 |
| 2013 | 5111 | 33.56 | 33.83 | 33.70 | 33.23 | 41.22 |
| n | 16821 | 8644 | 66 | 8058 | 53 | |
Weighted %s, unweighted ns. Standard deviations in parentheses.
t-Tests and chi2-tests indicated statistically different at p < .05 from the following:
*Men with other-sex partners;
†Women with other-sex partners;
‡Women with same-sex partners;
§Men with same-sex partners.
Analytic plan
The three steps in the analyses were to examine as follows: (1) whether sex of partner predicted sleep duration and restedness; (2) whether the negative associations between not enough and too much sleep and restedness was stronger among those with same-sex partners compared with those with other-sex partners (with sexual minority status x sleep duration interactions); and (3) whether state-level indicators of sexual minority acceptance moderated the association between sex of partner and sleep duration (with context variables x sexual minority status interactions). Multinomial logistic regressions were used for the first step, and ordinal logistic regressions were employed for the second two steps. Stata’s vce(cluster) option estimated all models to obtain robust variance estimates adjusting for within-state correlations [43]. This approach allowed for individual-level residual errors to be correlated within-state (but not among individuals across states), accounting for state-level differences, such as social welfare regimes or political leaning, that might be correlated with both restedness and our measures of same-sex context (i.e. same-sex marriage support and legislation). All analyses were conducted separately for women and men, with list-wise deletion for the small amount of item-level missing data on income and metropolitan residence (n = 419; no respondents with a same-sex respondent were dropped by listwise deletion), in line with other ATUS studies [44, 45]. The final survey weight [TUFNWGTP] accounted for the survey design and to generate population-level estimates.
Results
Bivariate statistics (Table 1) show that women in same-sex partnerships were the least likely to report sleeping less than 7 hr (14%), followed by women in different-sex couples (20%), and men in either same- or different-sex couples (23%). Women in same-sex couples were more likely to report oversleeping (43% slept 9 hr or more), followed by women in different-sex couples (31%), with again, men in, regardless of the sex of their partner, least likely to report oversleeping (27%). Yet, men with different-sex partners reported feeling the most rested (3.2 on a scale of 1 to 4), followed by women with different-sex partners (3.1), and men with same-sex partners (3.0). Women with same-sex partners reported the lowest levels of restedness (2.9).
Same- and different-sex couples, sleep duration, and restedness
Beginning with the first hypothesis examining disparities between individuals with same- and different-sex partners in two key indicators of sleep, Table 2 presents results for sleep duration from a multinomial logistic regression. Among both women and men, sex of partner did not significantly predict the likelihood of reporting under sleep or oversleep versus average sleep. Table 3 presents results for women’s feelings of restfulness from the ordinal logistic regressions. There were two key findings. First, reports of under-sleeping (i.e. less than 7 hr at night) were associated with lower levels of restfulness than reports of sleeping 7–9 hr at night (B = −0.49, p < .001, 95% confidence interval [CI] = −0.62, −0.36). Second, women with same-sex partners reported feeling significantly less rested than women with different-sex partners (B = −0.56, p < .05, CI = −1.02, −0.10; Model 1). Sex of partner did not significantly predict either sleep outcome among men (results in Table 4).
Table 2.
Multinomial regression predicting time spent sleeping (reference: 7–8 hr of sleep)
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Undersleep | Oversleep | Undersleep | Oversleep | |||||
| B (SE) | 95% CI | B (SE) | 95% CI | B (SE) | 95% CI | B (SE) | 95% CI | |
| Same-sex partner (ref: Different sex) | −0.25(0.39) | (−1.03, 0.52) | 0.40(0.37) | (−0.32, 1.12) | 0.08(0.46) | (−0.81, 0.98) | −0.05(0.32) | (−0.68, 0.58) |
| College degree (ref: No college degree) | −0.16+(0.09) | (−0.33, 0.01) | −0.26**(0.08) | (−0.41, −0.10) | −0.17*(0.08) | (−0.33, −0.00) | −0.17**(0.06) | (−0.29, −0.04) |
| Employment (ref: Full-time employed) | ||||||||
| Part-time employed | −0.29* | (−0.54, −0.04) | 0.11 | (−0.14, 0.36) | −0.29* | (−0.56, −0.02) | 0.40** | (0.14, 0.66) |
| (0.13) | (0.13) | (0.14) | (0.13) | |||||
| Unemployed | 0.10 | (−0.31, 0.33) | 0.53** | (0.20, 0.87) | −0.48** | (−0.80, −0.16) | 0.44** | (0.13, 0.74) |
| (0.16) | (0.17) | (0.16) | (0.15) | |||||
| Not in the labor force | −0.28** | (−0.44, −0.12) | 0.49*** | (0.35, 0.63) | −0.41** | (−0.72, −0.10) | 0.65*** | (0.42, 0.87) |
| (0.08) | (0.07) | (0.16) | (0.12) | |||||
| Family income (1–16 scale) | 0.01 | (−0.02, 0.04) | −0.03** | (−0.06, −0.01) | 0.01 | (−0.01, 0.04) | −0.03* | (−0.06, −0.01) |
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Parent (ref: No children in the home) | 0.09(0.09) | (−0.10, 0.28) | −0.27***(0.07) | (−0.42, 0.13) | −0.06(0.10) | (−0.25, 0.13) | −0.16+(0.09) | (−0.33, 0.00) |
| Race/ethnicity (ref: Non-Hispanic white) | ||||||||
| Non-Hispanic black | 0.42*** | (0.20, 0.64) | −0.06 | (−0.23, 0.11) | 0.45*** | (0.23, 0.68) | −0.24* | (−0.44, −0.05) |
| (0.11) | (0.09) | (0.11) | (0.10) | |||||
| Hispanic white | −0.05 | (−0.29, 0.20) | 0.13 | (−0.08, 0.35) | −0.03 | (−0.26, 0.20) | 0.42*** | (0.23, 0.61) |
| (0.12) | (0.11) | (0.12) | (0.10) | |||||
| Other race/ethnicity | −0.03 | (−0.32, 0.26) | −0.03 | (−0.23, 0.17) | 0.06 | (−0.19, 0.31) | 0.20 | (−0.15, 0.55) |
| (0.15) | (0.10) | (0.13) | (0.18) | |||||
| Age (years) | 0.01* | (0.00, 0.01) | −0.01*** | (−0.02, −0.01) | 0.00 | (−0.01, 0.01) | −0.01* | (−0.01, −0.00) |
| (0.00) | (0.00) | (0.00) | (0.00) | |||||
| Metropolitan area | 0.14 | (−0.09, 0.36) | 0.07 | (−0.09, 0.24) | −0.03 | (−0.19, 0.12) | −0.03 | (−0.18, 0.12) |
| (0.12) | (0.08) | (0.08) | (0.08) | |||||
| Region (ref: Northeast) | ||||||||
| Midwest | −0.23** | (−0.40, −0.06) | −0.01 | (−0.18, 0.16) | −0.09 | (−0.27, 0.08) | −0.05 | (−0.30, 0.20) |
| (0.09) | (0.09) | (0.09) | (0.13) | |||||
| West | −0.12+ | (−0.24, 0.01) | 0.08 | (−0.13, 0.30) | −0.34*** | (−0.51, −0.17) | 0.07 | (−0.17, 0.32) |
| (0.07) | (0.11) | (0.09) | (0.13) | |||||
| South | −0.17** | (−0.28, −0.06) | 0.06 | (−0.10, 0.22) | −0.12 | (−0.29, 0.05) | 0.04 | (−0.23, 0.31) |
| (0.06) | (0.08) | (0.09) | (0.14) | |||||
| Weekend | −0.10 | (−0.23, 0.02) | 0.26*** | (0.16, 0.35) | −0.21** | (−0.33, −0.08) | 0.48*** | (0.36, 0.59) |
| (0.06) | (0.05) | (0.06) | (0.06) | |||||
| Year (ref: 2010) | ||||||||
| 2012 | −0.13 | (−0.28, 0.03) | 0.15* | (0.02, 0.29) | −0.03 | (−0.19, 0.14) | 0.12+ | (−0.00, 0.24) |
| (0.08) | (0.07) | (0.08) | (0.06) | |||||
| 2013 | −0.04 | (−0.17, 0.09) | 0.07 | (−0.09, 0.23) | −0.06 | (−0.23, 0.12) | 0.16* | (0.03, 0.29) |
| (0.07) | (0.08) | (0.09) | (0.07) | |||||
| Constant | −1.05*** | (−1.56, −0.54) | 0.35 | (−0.12, 0.82) | −0.54* | (−1.04, −0.05) | −0.29 | (−0.85, 0.28) |
| (0.26) | (0.24) | (0.25) | (0.29) | |||||
| Observations | 8710 | 8710 | 8111 | 8111 | ||||
B = Unstandardized coefficients.
*p < .05, + p < .10; **p < .01; *** p < .001.
Table 3.
Ordinal logistic regression predicting restedness among women
| (1) | (2) | (3) | (4) | |||||
|---|---|---|---|---|---|---|---|---|
| B (std. err.) | 95% CI | B (std. err.) | 95% CI | B (std. err.) | 95% CI | B (std. err.) | 95% CI | |
| Same-sex partner (ref: Different sex) | −0.56* | (−1.02, −0.10) | −0.30 | (−0.72, 0.13) | −3.19** | (−5.36, −1.02) | −0.74** | (−1.27, −0.21) |
| (0.23) | (0.22) | (1.11) | (0.27) | |||||
| Sleep x Same-sex partner status | ||||||||
| Actual sleep (ref:7–8 hr) | ||||||||
| Undersleep | −0.49*** | (−0.62, −0.36) | −0.48*** | (−0.61, −0.35) | −0.49*** | (−0.61, −0.36) | −0.49*** | (−0.62, −0.36) |
| (0.06) | (0.06) | (0.06) | (0.06) | |||||
| Oversleep | 0.07 | (−0.03, 0.18) | 0.07 | (−0.03, 0.18) | 0.07 | (−0.03, 0.17) | 0.07 | (−0.03, 0.17) |
| (0.05) | (0.05) | (0.05) | (0.05) | |||||
| Same-sex partner status x undersleep | −1.51** | (−2.64, −0.38) | ||||||
| (0.58) | ||||||||
| Same-sex partner status x oversleep | −0.17 | (−0.68, 0.35) | ||||||
| (0.26) | ||||||||
| Contextual factor: State-level support for same-sex marriage | ||||||||
| Support for gay marriage | 0.01 | (−0.01, 0.02) | ||||||
| (0.01) | ||||||||
| Same-sex partner x support for gay,arrmarriage | 0.06* | (0.01, 0.11) | ||||||
| (0.03) | ||||||||
| Contextual factor: State allows same-sex marriage | ||||||||
| State allows same-sex marriage | 0.13* | (0.02, 0.24) | ||||||
| (0.05) | ||||||||
| Same-sex partner x State allows same-sex marriage | 0.56 | (−0.15, 1.26) | ||||||
| (0.36) | ||||||||
| Covariates | ||||||||
| College degree (ref: No college degree) | 0.05 | (−0.05, 0.14) | 0.05 | (−0.05, 0.14) | 0.04 | (−0.06, 0.14) | 0.04 | (−0.06, 0.14) |
| (0.05) | (0.05) | (0.05) | (0.05) | |||||
| Employment (ref: Full-time employed) | ||||||||
| Part-time employment | 0.14 | (−0.04, 0.31) | 0.14 | (−0.03, 0.32) | 0.14 | (−0.03, 0.31) | 0.14 | (−0.03, 0.32) |
| (0.09) | (0.09) | (0.09) | (0.09) | |||||
| Unemployed | 0.21+ | (−0.04, 0.45) | 0.22+ | (−0.04, 0.48) | 0.21 | (−0.04, 0.47) | 0.21 | (−0.04, 0.46) |
| (0.13) | (0.13) | (0.13) | (0.13) | |||||
| Not in the labor force | 0.08 | (−0.06, 0.22) | 0.08 | (−0.06, 0.22) | 0.09 | (−0.05, 0.22) | 0.08 | (−0.06, 0.22) |
| (0.07) | (0.07) | (0.07) | (0.07) | |||||
| Family income (1–16 scale) | 0.01 | (−0.01, 0.02) | 0.01 | (−0.01, 0.02) | 0.01 | (−0.01, 0.02) | 0.01 | (−0.01, 0.02) |
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Parent (ref: No children in the home) | −0.07 | (−0.20, 0.05) | −0.07 | (−0.20, 0.05) | −0.07 | (−0.20, 0.05) | −0.07 | (−0.19, 0.05) |
| (0.06) | (0.06) | (0.06) | (0.06) | |||||
| Race/ethnicity (ref: Non-Hispanic white) | ||||||||
| Non-Hispanic black | 0.16* | (0.01, 0.30) | 0.16* | (0.01, 0.30) | 0.15* | (0.01, 0.29) | 0.15* | (0.01, 0.30) |
| (0.07) | (0.07) | (0.07) | (0.07) | |||||
| Hispanic white | 0.35*** | (0.16, 0.55) | 0.35*** | (0.16, 0.55) | 0.35*** | (0.16, 0.55) | 0.35*** | (0.15, 0.55) |
| (0.10) | (0.10) | (0.10) | (0.10) | |||||
| Other race/ethnicity | 0.33*** | (0.17, 0.50) | 0.33*** | (0.17, 0.50) | 0.33*** | (0.16, 0.49) | 0.33*** | (0.16, 0.49) |
| (0.09) | (0.09) | (0.08) | (0.08) | |||||
| Age (years) | 0.02*** | (0.01, 0.03) | 0.02*** | (0.01, 0.03) | 0.02*** | (0.01, 0.03) | 0.02*** | (0.01, 0.03) |
| (0.00) | (0.00) | (0.00) | (0.00) | |||||
| Metropolitan area | −0.06 | (−0.17, 0.05) | −0.06 | (−0.17, 0.05) | −0.07 | (−0.19, 0.05) | −0.06 | (−0.17, 0.05) |
| (0.06) | (0.06) | (0.06) | (0.06) | |||||
| Region (ref: Northeast) | ||||||||
| Midwest | 0.07 | (−0.11, 0.24) | 0.07 | (−0.11, 0.24) | 0.13 | (−0.05, 0.31) | 0.13 | (−0.05, 0.31) |
| (0.09) | (0.09) | (0.09) | (0.09) | |||||
| West | 0.09 | (−0.04, 0.22) | 0.09 | (−0.04, 0.21) | 0.11 | (−0.02, 0.23) | 0.14+ | (−0.00, 0.28) |
| (0.07) | (0.07) | (0.07) | (0.07) | |||||
| South | 0.07 | (−0.06, 0.20) | 0.07 | (−0.05, 0.20) | 0.17+ | (−0.00, 0.34) | 0.14+ | (−0.02, 0.30) |
| (0.07) | (0.07) | (0.09) | (0.08) | |||||
| Weekend | 0.22*** | (0.13, 0.31) | 0.22*** | (0.12, 0.31) | 0.22*** | (0.12, 0.31) | 0.22*** | (0.13, 0.31) |
| (0.05) | (0.05) | (0.05) | (0.05) | |||||
| Year (ref: 2010) | ||||||||
| 2012 | 0.12+ | (−0.00, 0.25) | 0.13* | (0.00, 0.25) | 0.13* | (0.00, 0.25) | 0.12+ | (−0.00, 0.24) |
| (0.06) | (0.06) | (0.06) | (0.06) | |||||
| 2013 | 0.10 | (−0.01, 0.21) | 0.10+ | (−0.01, 0.21) | 0.10+ | (−0.01, 0.21) | 0.07 | (−0.05, 0.18) |
| (0.05) | (0.05) | (0.06) | (0.06) | |||||
| Constant: Cut 1 | −1.53*** | (−1.98, −1.08) | −1.52*** | (1.97, −1.07) | −1.25*** | (−1.99, −0.50) | −1.47*** | (−1.93, −1.01) |
| (0.23) | (0.23) | (0.38) | (0.24) | |||||
| Constant: Cut 2 | −0.13 | (−0.55, 0.29) | −0.12 | (−0.54, 0.30) | 0.16 | (−0.55, 0.86) | −0.07 | (−0.50, 0.36) |
| (0.21) | (0.21) | (0.36) | (0.22) | |||||
| Constant: Cut 3 | 1.73*** | (1.26, 2.20) | 1.73*** | (1.27, 2.20) | 2.01*** | (1.27, 2.75) | 1.79*** | (1.31, 2.26) |
| (0.24) | (0.24) | (0.38) | (0.24) | |||||
| Observations | 8,710 | 8,710 | 8,710 | 8,710 | ||||
*p < .05, + p < .10; ** p < .01; ***p < .001.
Table 4.
Ordinal logistic regression predicting restedness among men
| (1) | (2) | (3) | (4) | |||||
|---|---|---|---|---|---|---|---|---|
| B (std. err.) | 95% CI | B (std. err.) | 95% CI | B (std. err.) | 95% CI | B (std. err.) | 95% CI | |
| Same-sex partner (ref: Different sex) | −0.39 | (−0.90, 0.12) | −0.09 | (−0.81, 0.63) | 0.71 | (−1.62, 3.05) | −0.38 | (−0.91, 0.16) |
| (0.26) | (0.37) | (1.19) | (0.27) | |||||
| Sleep x Same-sex partner status | ||||||||
| Actual sleep (ref:7, 8 hr) | ||||||||
| Undersleep | −0.34*** | (−0.48, −0.20) | −0.34*** | (−0.47, −0.20) | −0.34*** | (−0.48, −0.20) | −0.34*** | (−0.48, −0.20) |
| (0.07) | (0.07) | (0.07) | (0.07) | |||||
| Oversleep | 0.06 | (−0.08, 0.20) | 0.06 | (−0.07, 0.20) | 0.06 | (−0.08, 0.20) | 0.06 | (−0.08, 0.20) |
| (0.07) | (0.07) | (0.07) | (0.07) | |||||
| Same-sex partner status x undersleep | −0.51 | (−2.07, 1.06) | ||||||
| (0.80) | ||||||||
| Same-sex partner status x oversleep | −0.77 | (−2.65, 1.10) | ||||||
| (0.96) | ||||||||
| Contextual factor: State-level support for same-sex marriage | ||||||||
| Support for gay marriage | −0.01+ | (−0.02, 0.00) | ||||||
| (0.01) | ||||||||
| Same-sex partner x support for gay marriage | −0.03 | (−0.08, 0.03) | ||||||
| (0.03) | ||||||||
| Contextual factor: State allows same-sex marriage | ||||||||
| State allows same-sex marriage | 0.04 | (−0.11, 0.19) | ||||||
| (0.08) | ||||||||
| Same-sex partner x State allows same- sex marriage | −0.17 | (−2.35, 2.00) | ||||||
| (1.11) | ||||||||
| Covariates | ||||||||
| College degree (ref: No college degree) | −0.01 | (−0.11, 0.10) | −0.01 | (−0.11, 0.10) | −0.00 | (−0.11, 0.10) | −0.01 | (−0.11, 0.10) |
| (0.05) | (0.05) | (0.05) | (0.05) | |||||
| Employment (ref: Full-time employed) | ||||||||
| Part-time employment | 0.12 | (−0.10, 0.34) | 0.12 | (−0.11, 0.34) | 0.11 | (−0.11, 0.34) | 0.12 | (−0.10, 0.34) |
| (0.11) | (0.11) | (0.11) | (0.11) | |||||
| Unemployed | 0.08 | (−0.18, 0.33) | 0.07 | (−0.18, 0.33) | 0.08 | (−0.17, 0.34) | 0.07 | (−0.18, 0.33) |
| (0.13) | (0.13) | (0.13) | (0.13) | |||||
| Not in the labor force | −0.12 | (−0.30, 0.05) | −0.12 | (−0.30, 0.05) | −0.12 | (−0.30, 0.05) | −0.12 | (−0.30, 0.05) |
| (0.09) | (0.09) | (0.09) | (0.09) | |||||
| Family income (1–16 scale) | 0.01 | (−0.01, 0.03) | 0.01 | (−0.01, 0.03) | 0.01 | (−0.01, 0.03) | 0.01 | (−0.01, 0.03) |
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Parent (ref: No children in the home) | −0.19** | (−0.32, −0.07) | −0.19** | (−0.32, −0.07) | −0.19** | (−0.32, -0.07) | −0.19** | (−0.32, −0.07) |
| (0.06) | (0.06) | (0.06) | (0.06) | |||||
| Race/ethnicity (ref: Non-Hispanic white) | ||||||||
| Non-Hispanic black | 0.56*** | (0.37, 0.75) | 0.56*** | (0.37, 0.75) | 0.57*** | (0.38, 0.76) | 0.56*** | (0.37, 0.75) |
| (0.10) | (0.10) | (0.10) | (0.10) | |||||
| Hispanic white | 0.38*** | (0.21, 0.54) | 0.38*** | (0.21, 0.54) | 0.38*** | (0.22, 0.54) | 0.37*** | (0.21, 0.54) |
| (0.09) | (0.09) | (0.08) | (0.09) | |||||
| Other race/ethnicity | 0.04 | (−0.17, 0.24) | 0.03 | (−0.17, 0.24) | 0.04 | (−0.16, 0.24) | 0.03 | (−0.17, 0.24) |
| (0.10) | (0.10) | (0.10) | (0.11) | |||||
| Age (years) | 0.02*** | (0.01, 0.02) | 0.02*** | (0.01, 0.02) | 0.02*** | (0.01, 0.02) | 0.02*** | (0.01, 0.02) |
| (0.00) | (0.00) | (0.00) | (0.00) | |||||
| Metropolitan area | −0.12* | (−0.24, −0.00) | −0.12* | (−0.24, −0.00) | −0.11+ | (−0.23, 0.01) | −0.12* | (−0.24, −0.00) |
| (0.06) | (0.06) | (0.06) | (0.06) | |||||
| Region (ref: Northeast) | ||||||||
| Midwest | 0.08 | (−0.02, 0.19) | 0.08 | (−0.02, 0.19) | −0.01 | (−0.13, 0.12) | 0.10 | (−0.12, 0.18) |
| (0.05) | (0.05) | (0.06) | (0.07) | |||||
| West | 0.02 | (−0.12, 0.16) | 0.02 | (−0.12, 0.16) | −0.01 | (−0.13, 0.12) | 0.03 | (−0.12, 0.18) |
| (0.07) | (0.07) | (0.06) | (0.08) | |||||
| South | 0.08 | (−0.02, 0.18) | 0.08 | (−0.02, 0.18) | −0.07 | (−0.27, 0.12) | 0.10 | (−0.03, 0.22) |
| (0.05) | (0.05) | (0.10) | (0.06) | |||||
| Weekend | 0.25*** | (0.15, 0.35) | 0.25*** | (0.15, 0.35) | 0.25*** | (0.15, 0.34) | 0.25*** | (0.15, 0.35) |
| (0.05) | (0.05) | (0.05) | (0.05) | |||||
| Year (ref: 2010) | ||||||||
| 2012 | 0.06 | (−0.06, 0.18) | 0.06 | (−0.06, 0.18) | 0.06 | (−0.06, 0.17) | 0.06 | (−0.06, 0.18) |
| (0.06) | (0.06) | (0.06) | (0.06) | |||||
| 2013 | 0.06 | (−0.06, 0.18) | 0.06 | (−0.06, 0.18) | 0.06 | (−0.06, 0.18) | 0.05 | (−0.09, 0.19) |
| (0.06) | (0.06) | (0.06) | (0.07) | |||||
| Constant: Cut 1 | −2.16*** | (−2.56, −1.75) | −2.16*** | (−2.56, −1.75) | −2.66*** | (−3.28, −2.04) | −2.15*** | (−2.51, −1.74) |
| (0.21) | (0.21) | (0.32) | (0.20) | |||||
| Constant: Cut 2 | −0.61*** | (−0.97, −0.25) | −0.61*** | (−0.97, −0.25) | −1.11*** | (−1.70, −0.52) | −0.59** | (−0.95, −0.22) |
| (0.18) | (0.18) | (0.30) | (0.18) | |||||
| Constant: Cut 3 | 1.34*** | (0.98, 1.70) | 1.34*** | (0.98, 1.70) | 0.84** | (0.24, 1.43) | 1.35*** | (0.99, 1.72) |
| (0.18) | (0.19) | (0.30) | (0.19) | |||||
| Observations | 8111 | 8111 | 8111 | 8111 | ||||
*p < .05, + p < .10; **p < .01; ***p < .001.
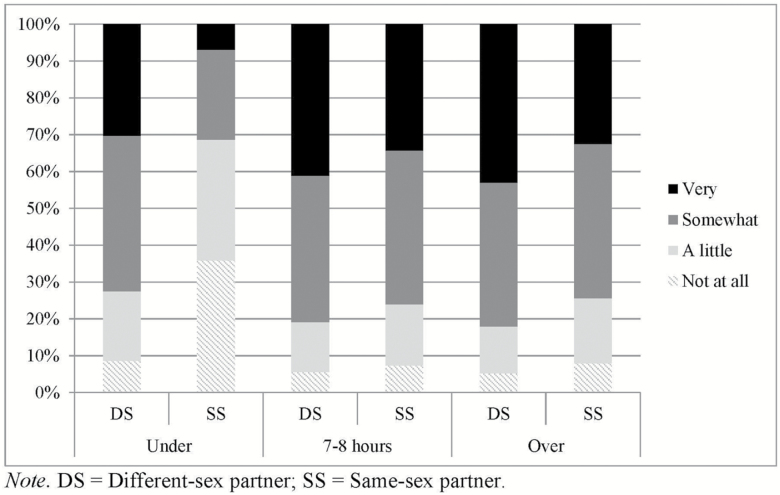
The second hypothesis explored whether there were differences between women with same- and different-sex partners in the link between sleep duration and restedness, finding that under-sleeping (compared with average sleep) for women with same-sex partners was associated with lower restedness compared with women with different-sex partners (as evidenced by the significant interaction term, presented in Model 2, Table 3). For example, an estimated 31 per cent of women with same-sex partners who slept less than 7 hr reported feeling very or somewhat rested compared with 73 per cent of women with other-sex partners with the same reported sleep duration (predicted estimates based off coefficients from Model 2 in Table 3 and presented in Figure 1). Sexual minority status did not significantly interact with sleep duration to predict restedness among men (results presented in Table 4).
Figure 1.
Predicted feelings of restedness by amount of sleep among women with different-sex and same-sex partners (n = 8710).
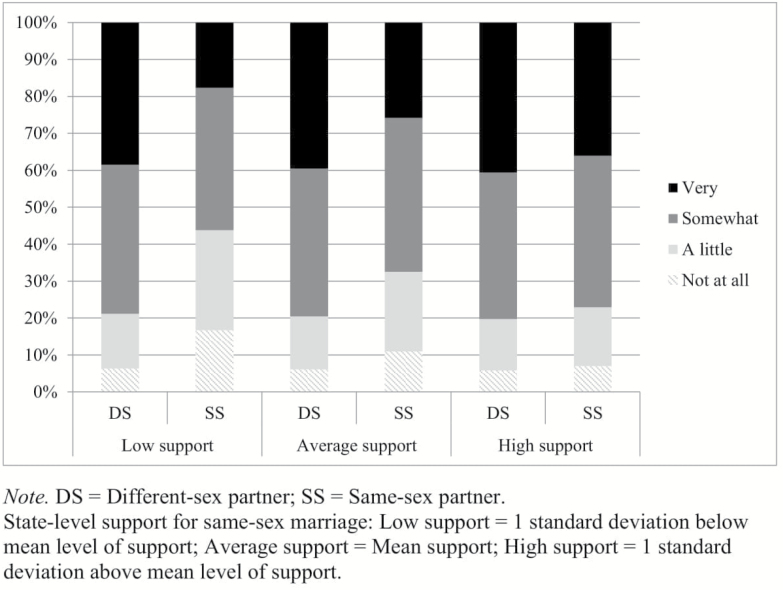
Sexual minority status and restedness across state contexts
To test the third hypothesis concerning the role of sexual minority–related contextual factors in shaping the association between sex of partner and restedness, interactions between sex of partner and state-level sexual minority support were added to the model for restedness. Among women, having a same-sex partner significantly interacted with state-level support for same-sex marriage (Model 3, Table 3). Figure 2 plots the predicted feelings of restedness among women at different levels of state-level support for same-sex marriage, using the coefficients from Model 3 in Table 2. In states with low levels of support for same-sex marriage, women in same-sex couples were twice as likely to report feeling a little or not at all rested (44%) compared with women in different-sex couples (21%). Women in same-sex couples residing in states that were high on support for same-sex marriage, however, reported similar levels of restfulness when they were compared with women in different-sex couples (23% vs. 20% feeling a little or not at all rested, respectively). The interaction between sex of partner and living in a state with legal same-sex marriage was not significant (Model 4, Table 3). No sexual minority status by state-level context interactions was significant among men (Table 4).
Figure 2.
Predicted feelings of restedness by state-level support for same-sex marriage among women with different- and same-sex partners (n = 8710).
Discussion
Examining disparities in sleep duration and restedness among individuals in same- and different-sex couples and exploring how sexual minority–specific contextual variables moderate these associations provide important initial insight into how this day-in-day-out process may render some sexual minority individuals more vulnerable to negative health outcomes. In line with the first hypothesis, poorer restedness was reported by women with same-sex partners when compared with women with different-sex partners, although no differences were observed for sleep duration. No significant differences by sex of partner were observed among men. These findings are largely in line with the literature suggesting that psychosocial stressors such as discrimination are more closely linked with assessments of sleep quality such as restedness than sleep duration [12, 28], as well as previous findings suggesting that sexual minority women, more so than sexual minority men, may be particularly vulnerable to worse sleep outcomes [6–8].
Turning to the second hypothesis, women with same-sex partners who reported under sleeping were more likely to report lower levels of restedness than women with other-sex partners with the same sleep durations. Although more research is needed, the interaction between sexual minority status and sleep duration may reflect previous work suggesting that higher levels of stress are associated with poorer self-rated indicators of sleep quality such as restedness [12, 14]. In other words, following the minority stress framework, women with same-sex partners may feel less rested because they experience more daily stress. Although many factors may contribute to the differences in restedness between sexual minority and heterosexual women, depressive symptoms may be an important factor for future research. Women’s greater vulnerability to depressive symptoms, compared with men, has been highlighted as one mechanism for explaining higher levels of sleep problems in women compared with men [46]. Sexual minority women are significantly more likely to report depressive symptoms when compared with their heterosexual peers [47, 48]. Future research is needed to better understand the role of depressive symptoms in vulnerability to poor sleep outcomes among sexual minority women. Finally, the finding that sexual minority women were more likely to rate their low levels of sleep as the less restful is particularly troubling as individuals who report both low sleep duration and low sleep quality, including restedness, may be vulnerable to the worst health outcomes, such as cardiovascular disease and overall psychosocial functioning [19–21]. Future research is needed to understand the role that sleep problems play in explaining the commonly identified health disparities between heterosexual and sexual minority women.
Finally, living in states with more popular support for same-sex marriage was associated with better restedness among women with same-sex partners, but not women with different-sex partners. These findings are in line with previous work linking contextual support for sexual minorities with more positive health outcomes among sexual minority populations [31, 35]. Conversely, same-sex marriage laws were only marginally associated with differences in restedness. Everyday social stressors (e.g. living in a community that holds negative attitudes towards same-sex marriage) that condition the individual’s regular interpersonal exchanges, rather than the broader legislative context (e.g. marriage equality), may be more important for shaping this sleep outcome.
Notably, partner sex did not significantly predict either sleep duration or restedness among men, and there was no variation according to sexual minority–related contextual factors. Previous research has identified gender differences in terms of how men and women evaluate restedness [37]. That sexual minority status was associated with restedness among women but not among men may reflect previous work suggesting that women’s sleep is more negatively affected by stressors than men’s sleep [49, 50]. The current findings may ultimately underscore how different health processes may contribute to health inequalities among sexual minority men compared with sexual minority women.
Strengths and limitations
This study expanded on the existing literature in several important ways. First, despite the importance of sleep for health, very few studies examine sleep health disparities between individuals with same- and different-sex partners. Second, by assessing sexual minority–related contextual factors as moderators, these findings push beyond identifying the existence of health disparities to exploring the factors that exacerbate vulnerability among sexual minority populations and identifying the locations where such disparities need the most intervention. These findings contribute to a growing body of literature showing that sexual minority–specific contextual variables are associated with sexual minority health processes and outcomes [31]. Third, very little nationally representative data look at sleep outcomes using time-diary data, which are more closely linked with objective assessments of sleep compared with other reports of sleep duration [51]. The inclusion of time diaries, along with a wide variety of pertinent control variables, provides an important opportunity to understand how same-sex partnership is associated with sleep health, using a nationally representative sample of respondents.
Despite these strengths, the results of this study need to be interpreted with several limitations in mind. One limitation was that sex of partner was used to assess sexual minority status. Although previous large-scale health studies have used sex of partner to assess sexual minority status [32], we do not know the sexual identities of individuals in ATUS, nor can we extrapolate these findings to sexual minority individuals who are not in same-sex partnerships. Similarly, as individuals were only asked about binary sexes (i.e. if they were male or female), we were unable to assess how diversity in gender identity was associated with sleep duration or restedness, an important avenue for future research. Another limitation is that the percentage and number of individuals with same-sex partners was small, creating an issue of low statistical power that makes it more difficult to assess whether null findings were a result of no differences by sexual minority status or due to a small sample size. A third limitation was that although we assessed one continuous night of sleep, we excluded any participant who reported 4 hr or less sleep during that night (i.e. individuals who did not get at least 4 hr of sleep before 4:00 am) and may have failed to capture individuals who reported waking up, but then went back to sleep in the morning. Future research can clarify these findings by including both subjective and objective assessments of restedness and sleep duration over multiple nights.
Conclusions
The link between sleep and health outcomes underscores the importance of understanding if and how sleep health varies among individuals with same- and different-sex partners. Sexual minority women, but not sexual minority men, may be particularly vulnerable to poorer restedness. This vulnerability is exacerbated by sexual minority–related contextual variables, suggesting the need for future work exploring the role of psychosocial stressors generally, and experiences of discrimination specifically, for understanding disparities in restedness between sexual minority and heterosexual women. Ultimately, these findings underscore why we need to better understand sexual minority–related disparities in health processes, as well as for health outcomes, for informing intervention and prevention efforts.
Funding
The authors acknowledge grants from the National Institute of Child Health and Human Development (F32 HD086994-01, PI: Kate Prickett, University of Chicago; R24 HD42849, PI: Mark Hayward, University of Texas at Austin). This research was undertaken, in part, thanks to funding from the Canada Research Chairs program to the first author (Canada Research Chair in Stigma and Psychosocial Development). Opinions reflect those of the authors and not necessarily those of the granting agency.
Notes
Conflict of interest statement. None declared.
Work Performed: Département de Psychoéducation, Université de Sherbrooke, Pavillon A7, 2500 Boul. De L’Université, Sherbrooke, Quebec, Canada
References
- 1. Liu Y, et al. Prevalence of healthy sleep duration among adults—United States. Morb Mortal Wkly Rep. 2014;65:137–141. [DOI] [PubMed] [Google Scholar]
- 2. Hafner M, et al. Why sleep matters—the economic costs of insufficient sleep: a cross-country comparative analysis. Santa Monica, CA: RAND Corporation; 2016. https://www.rand.org/pubs/research_reports/RR1791.html. Accessed November 8, 2018. [PMC free article] [PubMed] [Google Scholar]
- 3. Whinnery J, et al. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37(3):601–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grandner MA, et al. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Blosnich JR, et al. Health inequalities among sexual minority adults: evidence from ten U.S. states, 2010. Am J Prev Med. 2014;46(4):337–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chen JH, et al. Sexual Orientation and Sleep in the U.S.: A National Profile. Am J Prev Med. 2017;52(4):433–442. [DOI] [PubMed] [Google Scholar]
- 7. Dai H, et al. Sleep deprivation and chronic health conditions among sexual minority adults. Behav Sleep Med. 2017;Jul 23:1–5. doi:10.1080/15402002.2017.1342166 [DOI] [PubMed] [Google Scholar]
- 8. Fredriksen-Goldsen KI, et al. Chronic health conditions and key health indicators among lesbian, gay, and bisexual older US adults, 2013-2014. Am J Public Health. 2017;107(8):1332–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li P, et al. Is sexual minority status associated with poor sleep quality among adolescents? Analysis of a national cross-sectional survey in Chinese adolescents. BMJ Open. 2017;7(12):e017067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Caceres BA, et al. A systematic review of cardiovascular disease in sexual minorities. Am J Public Health. 2017;107(4):e13–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Conron KJ, et al. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jackowska M, et al. Psychosocial factors and sleep efficiency: discrepancies between subjective and objective evaluations of sleep. Psychosom Med. 2011;73(9):810–816. [DOI] [PubMed] [Google Scholar]
- 13. Knudsen HK, et al. Job stress and poor sleep quality: data from an American sample of full-time workers. Soc Sci Med. 2007;64(10):1997–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Winzeler K, et al. Daily stress, presleep arousal, and sleep in healthy young women: a daily life computerized sleep diary and actigraphy study. Sleep Med. 2014;15(3):359–366. [DOI] [PubMed] [Google Scholar]
- 15. Bureau of Labor Statistics. American Time Use Survey user’s guide: Understanding ATUS 2003 to 2013. Washington, DC, US: US Department of Labor; 2014. [Google Scholar]
- 16. Buysse DJ. Sleep health: can we define it? Does it matter?Sleep. 2014;37(1):9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cappuccio FP, et al. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Åkerstedt T, et al. The meaning of good sleep: a longitudinal study of polysomnography and subjective sleep quality. J Sleep Res. 1994;3(3):152–158. [DOI] [PubMed] [Google Scholar]
- 19. Chandola T, et al. The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: a prospective study from the Whitehall II cohort. Sleep. 2010;33(6):739–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tavernier R, et al. Bidirectional associations between sleep (quality and duration) and psychosocial functioning across the university years. Dev Psychol. 2014;50(3):674–682. [DOI] [PubMed] [Google Scholar]
- 21. Hoevenaar-Blom MP, et al. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep. 2011;34(11):1487–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kumari M, et al. Self-reported sleep duration and sleep disturbance are independently associated with cortisol secretion in the Whitehall II study. J Clin Endocrinol Metab. 2009;94(12):4801–4809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Akerstedt T, et al. Sleep disturbances, work stress and work hours: a cross-sectional study. J Psychosom Res. 2002;53(3):741–748. [DOI] [PubMed] [Google Scholar]
- 24. Hall MH, et al. Chronic stress is prospectively associated with sleep in midlife women: the SWAN sleep study. Sleep. 2015;38(10):1645–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Linton SJ, et al. The effect of the work environment on future sleep disturbances: a systematic review. Sleep Med Rev. 2015;23:10–19. [DOI] [PubMed] [Google Scholar]
- 26. Åkerstedt T, Orsini N, Petersen H, Axelsson J, Lekander M, Kecklund G. Predicting sleep quality from stress and prior sleep–a study of day-to-day covariation across six weeks. Sleep Med. 2012;13(6):674–9. [DOI] [PubMed] [Google Scholar]
- 27. Fuller-Rowell TE, et al. Racial discrimination mediates race differences in sleep problems: A longitudinal analysis. Cultur Divers Ethnic Minor Psychol. 2017;23(2):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Slopen N, et al. Discrimination and sleep: a systematic review. Sleep Med. 2016;18:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hatzenbuehler ML, et al. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hatzenbuehler ML, et al. Social attitudes regarding same‐sex marriage and LGBT health disparities: results from a national probability sample. J Soc Issues. 2017;73(3):508–528. [Google Scholar]
- 32. Kail BL, et al. State-level marriage equality and the health of same-sex couples. Am J Public Health. 2015;105(6):1101–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jackson CL, et al. Sexual orientation identity disparities in health behaviors, outcomes, and services use among men and women in the United States: a cross-sectional study. BMC Public Health. 2016;16(1):807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pew Research Center, Support for Same-Sex Marriage at Record High, but Key Segments Remain Opposed. 2015. http://www.people-press.org/2015/06/08/support-for-same-sex-marriage-at-record-high-but-key-segments-remain-opposed/. Accessed October 2, 2017.
- 35. Hatzenbuehler ML, et al. Structural stigma and all-cause mortality in sexual minority populations. Soc Sci Med. 2014;103:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. van den Berg JF, et al. Sex differences in subjective and actigraphic sleep measures: a population-based study of elderly persons. Sleep. 2009;32(10):1367–1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Vitiello MV, et al. Age-related sleep change: gender and estrogen effects on the subjective-objective sleep quality relationships of healthy, noncomplaining older men and women. J Psychosom Res. 2004;56(5):503–510. [DOI] [PubMed] [Google Scholar]
- 38. Basner M, et al. Sleep duration in the United States 2003–2016: first signs of success in the fight against sleep deficiency?Sleep. 2018. doi:10.1093/sleep/zsy012 [DOI] [PubMed] [Google Scholar]
- 39. Gonzales G, et al. National and state-specific health insurance disparities for adults in same-sex relationships. Am J Public Health. 2014;104(2):e95–e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lofquist D. Same-sex couple households. Maryland: US Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau; 2011. [Google Scholar]
- 41. Flores AR, et al. 2015. Trends in public support for same-sex couples by state 2015. Los Angeles: The Williams Institute; https://williamsinstitute.law.ucla.edu/wp-content/uploads/Trends-in-Public-Support-for-Same-Sex-Marriage-2004–2014.pdf. Accessed November 8, 2017. [Google Scholar]
- 42. Pew Research Forum. Gay marriage state by state Washington D.C; 2016. http://www.pewforum.org/2015/06/26/same-sex- marriage-state-by-state/.procon.org/view.resource.php?resourceID=004857. Accessed November 7, 2017. [Google Scholar]
- 43. Rogers W. Regression standard errors in clustered samples. Stata J. 1994;3(13):19–23. [Google Scholar]
- 44. Kalil A, et al. Diverging destinies: maternal education and the developmental gradient in time with children. Demography. 2012;49(4):1361–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Musick K, et al. How parents fare: mothers’ and fathers’ subjective well-being in time with children. Am Sociol Rev. 2016;81(5):1069–1095. [Google Scholar]
- 46. Mallampalli MP, et al. Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. J Womens Health (Larchmt). 2014;23(7):553–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cochran SD, et al. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol. 2003;71(1):53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Plöderl M, et al. Mental health of sexual minorities. A systematic review. Int Rev Psychiatry. 2015;27(5):367–385. [DOI] [PubMed] [Google Scholar]
- 49. Bassett E, et al. Neighbourhood disadvantage, network capital and restless sleep: is the association moderated by gender in urban-dwelling adults?Soc Sci Med. 2014;108: 185–193. [DOI] [PubMed] [Google Scholar]
- 50. Nordin M, et al. Psychosocial factors, gender, and sleep. J Occup Health Psychol. 2005;10(1):54–63. [DOI] [PubMed] [Google Scholar]
- 51. Fichten CS, et al. Time estimation in good and poor sleepers. J Behav Med. 2005;28(6):537–553. [DOI] [PubMed] [Google Scholar]