Abstract
Background
Polytobacco product use is suspected to be common, dynamic across time, and increase risk for adverse behavioral outcomes. We statistically modeled characteristic types of polytobacco use trajectories during mid-adolescence and tested their prospective association with substance use and mental health problems.
Methods
Adolescents (N = 3393) in Los Angeles, CA, were surveyed semiannually from 9th to 11th grade. Past 6-month combustible cigarette, e-cigarette, or hookah use (yes/no) over four assessments were analyzed using parallel growth mixture modeling to identify a parsimonious set of polytobacco use trajectories. A tobacco product use trajectory group was used to predict substance use and mental health at the fifth assessment.
Results
Three profiles were identified: (1) tobacco nonusers (N = 2291, 67.5%) with the lowest use prevalence (<3%) of all products across all timepoints; (2) polyproduct users (N = 920, 27.1%) with moderate use prevalence of each product (8–35%) that escalated for combustible cigarettes but decreased for e-cigarettes and hookah across time; and (3) chronic polyproduct users (N = 182, 5.4%) with high prevalence of each product use (38–86%) that escalated for combustible cigarettes and e-cigarettes. Nonusers, polyproduct users, and chronic polyproduct users reported successively higher alcohol, marijuana, and illicit drug use and ADHD at the final follow-up, respectively. Both tobacco using groups (vs. nonusers) reported greater odds of depression and anxiety at the final follow-up but did not differ from each other.
Conclusions
Adolescent polytobacco use may involve a common moderate risk trajectory and a less common high-risk chronic trajectory. Both trajectories predict substance use and mental health symptomology.
Implications
Variation in use and co-use of combustible cigarette, e-cigarette, and hookah use in mid-adolescence can be parsimoniously characterized by a small set common trajectory profiles in which polyproduct use are predominant patterns of tobacco product use, which predict adverse behavioral outcomes. Prevention and policy addressing polytobacco use (relative to single product use) may be optimal tobacco control strategies for youth, which may in turn prevent other forms of substance use and mental health problems.
Introduction
Combustible cigarette smoking among high school students has declined to its lowest level since 1991,1 however use of alternative tobacco products, such as electronic cigarette (e-cigarette) and hookah (tobacco water pipe) has increased in recent years.2,3 The widespread availability of conventional and alternative tobacco products has resulted in numerous, dynamic patterns of polytobacco product use (ie, use of three or more tobacco products) among youth.4–7 In 2015, 13.0% of high school students used two or more tobacco products in the past 30 days,4 and 64.6% of past 30-day e-cigarette users and 83.9% of past 30-day cigarette users, respectively, were polytobacco users.8
The numerous configurations of polyproduct use patterns pose a challenge to tobacco control efforts, as it is unclear which forms of polyproduct use should garner the highest priority. Identifying a more parsimonious set of common, homogenous tobacco use patterns can identify particular forms of poly use that can be targeted in prevention programs, policies, and surveillance. The small body of evidence to date suggests that there are distinct groups of adolescents who temporarily experiment with multiple tobacco products as well as others who may use one or more products across multiple time points.9–11 Previous research investigating youth tobacco product use trajectories has typically focused on a single tobacco product at a time,12 and there is little longitudinal research assessing complex developmental patterns of polytobacco use throughout adolescence. Person-centered statistical approaches, such as parallel process latent growth mixture modeling (GMM), which parsimoniously account for heterogeneity in the use and co-use patterns of multiple tobacco products over time, are needed to identify homogeneous subgroups of adolescents with similar longitudinal patterns of change in use and co-use of multiple tobacco products across adolescence.13
Identifying prototypical patterns of polytobacco use across adolescence is also important for understanding which configurations of polytobacco use patterns may be associated with adverse health outcomes. Tobacco product use among high school students has been shown to be associated with the use of alcohol and other illicit substances,14 with the level or prevalence of substance use increasing proportionally with the number of tobacco products used.15 Recent cross-sectional data suggests that polytobacco use is associated with increased likelihood of alcohol and marijuana use16–18 and mental health symptomology (ie, depression and anxiety).19 Additionally, prospective data indicates that more frequent e-cigarette and combustible cigarette use may also be associated with increased severity of depressive symptomology.20,21 However, it is unknown if specific polytobacco use trajectories are longitudinally associated with increases in substance use and mental health problems during mid-adolescence.
In this longitudinal study of Los Angeles area high school students, we examined heterogeneity in developmental patterns of polytobacco use across ages 14 to 16 years and identify profiles with distinct trajectories of use and co-use of the three tobacco products that are currently most popular among adolescents (ie, combustible cigarette, e-cigarette, and hookah).3 We also examine prospective associations of polytobacco use trajectories with substance use (ie, alcohol, marijuana, and illicit drugs) and mental health problems (ie, depression, anxiety, and attention deficit/hyperactivity disorder [ADHD]). Such data can inform product-specific targets for tobacco prevention interventions among youth who experiment with and regularly use popular tobacco products, and may also elucidate polytobacco use trajectories that confer risk for subsequent substance use and mental health problems.
Methods
Sample and Procedure
Data were drawn from the Happiness & Health Study, a longitudinal cohort survey of substance use and mental health among high school students in the Los Angeles metropolitan area.22 Forty public high schools were approached to participate in the study due to their demographic characteristics, proximity, and willingness to participate in research; 10 schools agreed to participate in the study (see Supplementary Table S1 for characteristics of participating schools in reference to Los Angeles county public schools).
Of the 4100 eligible 9th grade students, 3396 students and their parents provided active written or verbal assent and consent, respectively, to enroll in the study. Data collection involved five semiannual assessments: baseline (fall 9th grade, 2013; N (surveyed) = 3383, 99.6%), 6-month (spring 9th grade, 2014; N = 3292, 96.9%), 12-month (fall 10th grade, 2014; N = 3281, 96.6%), 18-month (spring 10th grade, 2015; N = 3251, 95.7%), and 24-month (fall 11th grade, 2015; N = 3232, 95.2%) follow-ups. At each assessment, paper-and-pencil surveys were administered onsite in students’ classrooms. Students not in class during data collections completed surveys by telephone, Internet, or mail (6-month follow-up: N = 49, 12-month follow-up: N = 142, 18-month follow-up: N = 216, 24-month follow-up: N = 247). The University of Southern California Health Sciences Review Board approved this study.
Measures
Tobacco Product Use
At each assessment, items based on the Youth Behavior Risk Surveillance (YRBS)23 and Monitoring the Future (MTF)3 surveys assessed the past 6-month use of combustible cigarettes (described as even a few-puffs), e-cigarettes, and hookah. Use of each tobacco product was dichotomously coded as 0 (No) and 1 (Yes) to indicate the prevalence of past 6-month use of each product.
Substance Use Outcomes
At the baseline and 24-month assessments, past 30-day use of alcohol (“one full drink of alcohol and not just a few sips for religious purposes”), marijuana, and other illicit drugs (eg, illicit and prescription stimulants, prescription painkillers) were measured using well-validated items assessing the number of days used each substance was used in the past 30 days (forced choice with 9 ordinal options ranging from 1 [0 days] to 9 [all 30 days]).23 These response categories were recoded into quantitative count variables by taking the mean value of each ordinal category: 0 (0 days), 2 (1–2 days), 4 (3–5 days), 8 (6–9 days), 12 (10–14 days), 17 (15–19 days), 22 (20–24 days), 27 (25–29 days), and 30 (all 30 days).
Mental Health Outcomes
At the baseline and 24-month assessments, depressive symptomology was assessed with the Center for Epidemiologic Studies Depression Scale (CESD).24 The CESD is a 20-item measure of depressive symptoms experienced over the past week, rated on a 4-point Likert scale, ranging from 0 (Rarely or None of the time; 0–1 days) to 3 (Most or all of the time; 5–7 days). The total sum score of the 20 items was computed (Cronbach’s αs = .81 and .83 for baseline and 24-month follow-up, respectively) and was dichotomized (yes/no) based on the measure’s recommended cutoff for clinical depression.25 The Revised Children’s Anxiety and Depression Scale (RCADS)26 was used to assess respondents’ generalized anxiety. Raw sum scores of six items (αs>.89) were converted into gender- and age-normed standardized T-scores and were dichotomously coded for the borderline clinical cutoff of the Generalized Anxiety Disorder (GAD). The 18-item Current Symptoms Scale-Self Report Form measure of DSM-IV ADHD27 assessed current ADHD symptoms (αs > .92), with nine items measuring the inattention and hyperactivity-impulsivity symptom dimensions of ADHD. Respondents rated how frequently they experienced each individual symptom during the past 6 months from 0 (never or rarely) to 3 (very often). If 12 or more items were endorsed at ratings of 2 or higher, ADHD was dichotomously coded above clinical cutoff. Because ADHD measures were not added to the assessment battery until the 6-month follow-up assessment, the ADHD score at the 6-month follow-up was used as the baseline score for this analysis.
Covariates
A priori covariates were selected based on their association with tobacco use or mental health outcomes in the extant literature.28,29 At baseline, time-invariant sociodemographic covariates including age, gender, race/ethnicity, and highest parental education level were assessed with investigator-defined forced-choice items (see response categories in Table 1). Past 6-month use of other tobacco products (ie, smokeless tobacco, cigars, cigarillos, dissolvable) at baseline was assessed with four items from the YRBS and MTF studies. This other tobacco use covariate was dichotomously coded (0 = no use; 1 = any use of other forms of tobacco).
Table 1.
Sample Characteristics at Baseline by Polytobacco Use Trajectory Groups
| Multiple tobacco product trajectory groups | |||||
|---|---|---|---|---|---|
| Total (N = 3393, 100.0%) | Chronic polyproduct usersd (N = 182, 5.4%) | Polyproduct userse (N = 920, 27.1%) | Tobacco nonusers (N = 2291, 67.5%) | p | |
| Sociodemographics/Other tobacco use | |||||
| Sexa | 3393 (100.0) | 182 (100.0) | 920 (100.0) | 2291 (100.0) | .15 |
| Female | 1811 (53.4) | 95 (52.2) | 467 (50.8) | 1249 (54.5) | |
| Male | 1582 (46.6) | 87 (47.8) | 453 (49.2) | 1042 (45.5) | |
| Ageb | 14.58 (.40) | 14.56 (.41)f | 14.63 (.41)f | 14.55 (.40)f | <.001 |
| Race/ethnicitya | 3310 (100.0) | 173 (100.0) | 895 (100.0) | 2242 (100.0) | <.001 |
| White | 520 (15.7) | 29 (16.8) | 129 (14.4) | 362 (16.1) | |
| Hispanic | 1557 (47.0) | 96 (55.5) | 492 (55.0) | 969 (43.2) | |
| Black | 165 (5.0) | 4 (2.3) | 44 (4.9) | 117 (5.2) | |
| Asian | 535 (16.2) | 12 (6.9) | 87 (9.7) | 436 (19.4) | |
| Other | 533 (16.1) | 32 (18.5) | 143 (16.0) | 358 (16.0) | |
| Parental education levela, c | 2491 (100.0) | 125 (100.0) | 665 (100.0) | 1701 (100.0) | <.001 |
| ≤8th grade | 76 (3.1) | 4 (3.2) | 21 (3.2) | 51 (3.0) | |
| Some high school | 204 (8.2) | 13 (10.4) | 77 (11.6) | 114 (6.7) | |
| High school graduate | 393 (15.8) | 25 (20.0) | 125 (18.8) | 243 (14.3) | |
| Some college | 491 (19.7) | 30 (24.0) | 141 (21.2) | 320 (18.8) | |
| College graduate | 818 (32.8) | 36 (28.8) | 201 (30.2) | 581 (34.2) | |
| Graduate degree | 509 (20.4) | 17 (13.6) | 100 (15.0) | 392 (23.0) | |
| Other tobacco products usea | 3359 (100.0) | 179 (100.0) | 907 (100.0) | 2273 (100.0) | <.001 |
| No use | 3243 (96.5) | 135 (75.4) | 844 (93.1) | 2264 (99.6) | |
| Any use | 116 (3.5) | 44 (24.6) | 63 (6.9) | 9 (0.4) | |
aAvailable (nonmissing) data for respective variable and, for categorical variables, denominator for within-column percentages. n (%). Based on χ2 test of association. bMean (SD). Based on the ANOVA test of association. cParticipants who marked “don’t know” response (N = 422) recoded as missing. dEscalating Cigarette & e-Cigarette / High Hookah. eEscalating cigarette / Decreasing e-cigarette & hookah. fLSD post hoc analyses results.
Analytic Plan
To characterize trajectories of past 6-month combustible cigarette, e-cigarette, and hookah use across the first four assessments, we conducted a series of growth mixture modeling (GMM) analyses—an analytic technique that allows for the estimation of subgroups of individuals within the population who differ in terms of their initial levels and rates of change for a specific outcome over time.13 We utilized a “parallel process” application of GMM, which generates classes based on covariation across three separate sets of latent intercepts and linear slopes (ie, one set of growth factors per tobacco product).30 The number of classes that best fit the data for the three tobacco use outcomes was selected based on model fit comparisons using a series of standard fit indices: Bayesian Information Criterion (BIC), sample-size-adjusted BIC (SSA-BIC), Akaike Information Criterion (AIC), Lo–Mendell–Rubin (LMR) likelihood ratio test, and entropy.31 Optimal models were chosen on the basis of goodness of fit and parsimony.
After identifying the polytobacco use trajectory profiles, participants were assigned to their most probable trajectory class. We then utilized regression modeling to test associations of polytobacco use trajectory class memberships across baseline to 18-month follow-up with substance use and mental health outcomes at the 24-month follow-up, with separate models for each outcome. As the substance use outcomes (ie, the number of days each substance was used in the past 30 days) were zero-inflated and over-dispersed, we utilized negative binomial regression modeling for these outcomes.32 The negative binomial regression coefficients were exponentiated to obtain incidence rate ratios (IRRs). Binary logistic regression modeling was applied for each mental health outcome (dichotomously coded above or below clinical cutoff). For all tests, we controlled for the aforementioned sociodemographic covariates and each respective substance use or mental health outcome at baseline.
All analyses were conducted in Mplus33 version 7 with statistical significance set at p < .05. As respondents were clustered within schools, a complex analysis was used to adjust parameter standard errors for interdependence in the data (ie, the error terms of regression models were not independent) to avoid an underestimation of standard errors. Missing data were managed with full information likelihood estimation (FIML).
Results
Preliminary Analyses
Among study enrollees, 3393 students provided at least one data point for the tobacco product use outcomes in the primary GMM analyses (99.9%), and were included in the analytic sample (see Table 1 for Ns of available data). We first examined differences in study variables among participants who completed (N = 3232, 95.2%) and did not complete (N = 164, 4.8%) the 24-month follow-up. No significant differences among study variables between these two groups were detected (ps = .07−.42). As depicted in Table 1, the sample was balanced on gender and was sociodemographically diverse. The prevalence of past 6-month tobacco use in each assessment is presented in Supplementary Table S2 of the online supplemental materials. Also, the prevalence of substance use and mental health symptomology outcomes at baseline is presented in Supplementary Table S3 of the online supplemental materials.
Trajectory Groups of Combustible Cigarette, E-cigarette, and Hookah Use
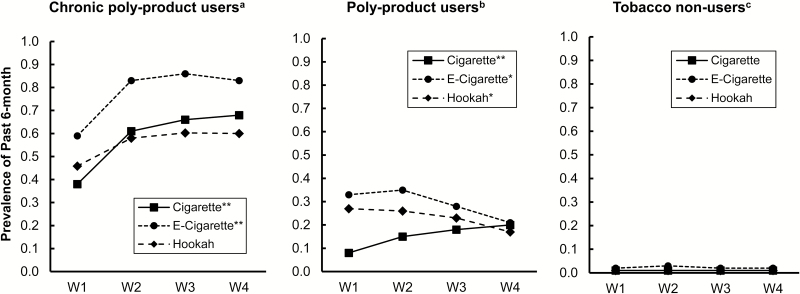
Fit indices for parallel GMM analyses (presented in Table 2) converged to suggest the superiority of a three-class solution fitting the data best (SSA-BIC = 22040.438; Entropy = 0.850; LMR p = .014). Figure 1 presents the observed trajectories of polytobacco product use prevalence across assessments after individuals were assigned to each respective group. Approximately 67.5% of adolescents were identified as the “Tobacco nonusers” group (N = 2291). Tobacco nonusers reported a negligible prevalence of combustible cigarette, e-cigarette, and hookah use in the past 6 months at each assessment (<3%), and their prevalence of use of each tobacco product did not significantly change during the study observation period (see Figure 1).
Table 2.
Fit Indices for Growth Mixture Models
| Class # | AIC | BIC | SSA-BIC | Entropy | LMR p |
|---|---|---|---|---|---|
| 1 | 26759.696 | 26796.473 | 26777.408 | — | — |
| 2 | 22446.874 | 22526.557 | 22485.250 | 0.825 | 0.0001 |
| 3 | 21981.398 | 22103.988 | 22040.438 | 0.850 | 0.0144 |
| 4 | 21901.071 | 22066.567 | 21980.775 | 0.816 | 0.5705 |
| 5 | 21831.845 | 22040.247 | 21932.213 | 0.804 | 0.5592 |
AIC = Akaike Information Criterion. BIC = Bayesian Information Criterion. SSA-BIC = sample-size-adjusted BIC. LMR p = The Lo–Mendell–Rubin (LMR) likelihood ratio test p value.
Figure 1.
Observed trajectories of combustible cigarette, e-cigarette, and hookah use by three groups. N = 3393. W1 = Baseline (Mean age = 14 years). W2 = 6-month follow-up. W3 = 12-month follow-up. W4 = 18-month follow-up. The significance of slope mean estimate of each tobacco product use is indicated in the legends: *p < 0.05, **p < 0.01. aChronic polyproduct users: Escalating cigarette & e-cigarette / High stable hookah (N = 182, 5.4%). bPolyproduct users: Escalating cigarette / Decreasing e-cigarette & hookah (N = 920, 27.1%). cTobacco nonusers (N = 2291, 67.5%).
The “Polyproduct users” group (N = 920, 27.1%) displayed disparate trajectories of combustible cigarette use and alternative tobacco product (ie, e-cigarette, hookah) use. Polyproduct users displayed a low prevalence of combustible cigarette use at baseline (7.7%), but their prevalence of combustible cigarette use significantly increased over follow-up, reaching 19.9% at the 18-month follow-up (Slope mean = 0.176, p < .001). However, their prevalence of e-cigarette use significantly decreased from 32.5% to 20.8% and their prevalence of hookah use significantly decreased from 27.1% to 17.2% from baseline to the 18-month follow-up assessment (Slope mean = −0.085, p = 0.02 for e-cigarette; Slope mean = −0.157, p = 0.01 for hookah).
The “Chronic polyproduct users” group was comprised of 182 adolescents (5.4%) who displayed the highest prevalence of use of each tobacco product at baseline and significantly increased their prevalence of combustible cigarette use (Slope mean = 0.355, p < .001) and e-cigarette use (Slope mean = 0.389, p < .001) across the follow-up period. Their prevalence of combustible cigarette use increased from 38.2% at baseline to 67.8% at the 18-month follow-up, and their prevalence of past 6-month e-cigarette use increased from 58.9% at baseline to 83.3%. The prevalence of hookah use in this group increased from 45.8% to 60.4% across the follow-ups, but the change over time was not significantly different from zero (Slope mean = 0.138, p = .19).
Associations of Polytobacco Use Trajectory Groups With Substance Use and Mental Health
Table 3 presents the associations of polytobacco use trajectory groups with changes in substance use and mental health outcomes from baseline to the 24-month follow-up. Compared with Tobacco nonusers, Chronic polyproduct users and Polyproduct users used alcohol, marijuana, and other illicit drugs a greater number of days at the 24-month follow-up after adjusting for respective baseline levels and demographics (ps < .01; Table 3). Also, Chronic polyproduct users, compared with Polyproduct users, reported significantly more days of alcohol (IRR [95%CI] = 1.90 [1.14, 2.67]; p = .004), marijuana (IRR [95%CI] = 2.16 [1.50, 2.82]; p < .001), and other illicit drug use (IRR [95%CI] = 2.37 [1.60, 3.14]; p < 0.001) at follow-up. In Table 3, we present IRR estimates for each substance use outcome and polytobacco use trajectory group contrast.
Table 3.
Associations of Polytobacco Use Trajectory Groups With Substance Use and Mental Health Outcomes at 24-Month Follow-Up
| Outcomes (W5) | Tobacco use trajectory groups | |||||
|---|---|---|---|---|---|---|
| Chronic polyproduct users vs. Tobacco nonusers (ref) | Polyproduct users vs. Tobacco nonusers (ref) | Chronic polyproduct users vs. Polyproduct users (ref) | ||||
| Past month substance use | IRR | 95% CI | IRR | 95% CI | IRR | 95% CI |
| Alcohol use | 5.632** | 2.775, 8.489 | 3.524** | 2.888, 4.160 | 1.902** | 1.138, 2.667 |
| Marijuana use | 7.425** | 2.512, 12.338 | 5.344** | 2.256, 8.431 | 2.159** | 1.498,2.820 |
| Other illicit drug use | 9.286** | 5.424, 13.148 | 7.485** | 3.292, 11.677 | 2.366** | 1.598, 3.135 |
| Mental health outcomes | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Depression (CESD) | 1.469** | 1.146, 1.792 | 1.334** | 1.080, 1.588 | 1.101 | 0.714, 1.488 |
| Anxiety (RCADS-GAD) | 1.572** | 1.133, 2.011 | 1.236* | 1.043, 1.426 | 1.127 | 0.984, 1.277 |
| ADHD | 2.597** | 1.830, 3.364 | 1.394* | 1.053, 1.735 | 1.663** | 1.272, 2.054 |
N = 3393. IRR = Incidence Rate Ratio. OR = Odds Ratio. CI = Confidence Interval. Adjusted for parental education level, youth age, gender, ethnicity, other tobacco products use (eg, smokeless tobacco, cigars/cigarillos, dissolvable) in the past 6 months, and each outcome indicator at baseline. W5 = 24-month follow-up. Mental health outcomes were coded by 0 = Scores below the clinical cutoff and 1 = Scores above the clinical cutoff. Past month substance use outcomes were coded as a count variable indicating number of days of substance use in the past month. *p < 0.05, **p < 0.01.
Chronic polyproduct users and Polyproduct users (vs. Tobacco nonusers) were more likely to report depression, anxiety, and ADHD symptoms that reached the clinical cutoff at the 24-month follow-up, after controlling for sociodemographic factors and baseline mental health problems (Table 3). For instance, compared to Tobacco nonusers, the odds of Chronic polyproduct users reporting symptoms that reached the clinical cutoff for depression at the final follow-up were 47% higher (OR [95%CI] = 1.47 [1.15, 1.79]; p < .001). Compared with Polyproduct users, Chronic polyproduct users were 66% more likely to report ADHD symptoms that reached the clinical cutoff (OR [95%CI] = 1.66 [1.27, 2.05], p < .01); however, they were not significantly more likely to report clinical symptoms of depression (OR [95%CI] = 1.10 [0.71, 1.49], p = .58) or generalized anxiety (OR [95%CI] = 1.13 [0.98, 1.28]; p = .43). Table 3 presents OR estimates for each mental health outcome and tobacco product use trajectory group contrast.
Sensitivity Analyses
A series of sensitivity analyses were conducted to assess if the results remained consistent when different subsets of the sample were excluded. Associations of polytobacco use trajectory groups with changes in substance use and mental health outcomes from baseline to the 24-month follow-up did not differ when: (1) students (N = 55, 1.6%) whose reports were of questionable validity were removed (eg, reported use of a fictitious drug); (2) students (N = 377, 11.1%) who completed a follow-up survey by an alternate mode of survey administration other than in-class paper surveys (ie, telephone, internet, or mail) were removed; and (3) only the subsample of students (N = 3082, 90.8%) who completed all five assessments were included (see supplemental materials). We did not find any meaningful differences from the results using the total sample (N = 3393).
Discussion
To our knowledge, this is the first study to provide a parsimonious characterization of the broad variation in use and co-use of popular tobacco products across an important developmental period of risk (ie, mid-adolescence). Using an empirically derived modeling approach, this study identified three profiles with distinct trajectories that explained the heterogeneity in developmental patterns of use and poly use of tobacco products among adolescents: (1) Chronic polyproduct users; (2) Polyproduct users; and (3) Tobacco nonusers. A key finding from this analysis is that prototypical patterns of use of tobacco products across mid-adolescence in this sample either involve the use of no products or some form of polytobacco product use. A single product user trajectory was not identified in the data. Hence, poly use is the norm and single product use is the exception, suggesting that a comprehensive approach to tobacco control in adolescents that addresses multiple products is warranted.
Consistent with results from national surveys,3 the majority of youth in this sample (67.5%) did not use any tobacco products, or had a negligible prevalence of past 6-month combustible cigarette, e-cigarette, and hookah use across mid-adolescence. Youth in the Chronic polyproduct and Polyproduct user groups displayed distinct patterns in their polytobacco use trajectories. Chronic polyproduct users (approximately 5% of the sample) had the highest prevalence of past 6-month combustible cigarette, e-cigarette, and hookah use at each assessment with escalating trajectories of combustible cigarette (38% to 68% across follow-up) and e-cigarette use (59% to 83% across follow-up) during mid-adolescence. These youths may reflect those whose tobacco product consumption persists over time without discontinuation for all products, which would presumably increase cumulative exposure to nicotine and potentially risk for dependence on one or more products.
Polyproduct users (27.1% of the sample) had moderate prevalence of past 6-month combustible cigarette, e-cigarette, and hookah use across the follow-up assessments, and displayed decreasing trajectories of e-cigarette (33% to 21% across follow-up) and hookah use (27% to 17% across follow-up) but increasing prevalence of combustible cigarette use (8% to 20% across follow-up). An appreciable proportion of adolescents initiate tobacco product use with e-cigarettes,34,35 and use of e-cigarettes or hookah among noncigarette smoking youth is associated with combustible cigarette initiation in bi-variate analyses of associations of use of these products with combustible cigarette use.22,36–39 The (nonchronic) polytobacco use trajectory identified in this study may be emblematic of such transitions and suggests temporary time limited use of hookah or e-cigarettes and with moderate risk of subsequent transition over to combustible cigarettes.
Extending extant cross-sectional data,16,17,19,40–42 the three polytobacco use trajectory groups identified in this prospective study followed a risk gradient for engaging in substance use behaviors and reporting clinical levels of mental health symptomology with: (1) Chronic polyproduct users displaying the highest risk; (2) Polyproduct experimenters displaying moderate risk; and (3) Tobacco nonusers with the lowest risk. Research examining polytobacco use prior to when e-cigarettes and hookah were available or popular had studied concurrent use of combustible cigarettes and smokeless tobacco products and found strong associations between polytobacco use and substance use, with polytobacco users more than 30 times as likely to subsequently use alcohol, marijuana, and cocaine.43 The results of the current study show that future substance use risk may also be elevated using diverse patterns of poly use of emerging tobacco products that are currently popular among adolescents.
Nicotine exposure during adolescence alters neurodevelopment and may increase vulnerability to substances of abuse45–47 as well as impacting mood and mental health.48 Given prior evidence that polytobacco use (vs. single product use) is positively associated with increased nicotine dependence,5,49 and polytobacco users have been shown to engage in more frequent smoking and vaping than single-product users,42 increased exposure to nicotine may confer risk for substance use and mental health symptomology. However, it is also possible that risk factors not accounted for in the current analysis explain the observed association between polytobacco use trajectories and substance use and mental health. Polytobacco use may be a risk marker for subsequent substance use and mental health problems with chronic polytobacco product users representing high-risk adolescents,50 and less frequent polyproduct users being “lower-risk” teens with moderate levels of mental health and behavioral problems.
These findings could be used to inform interventions tailored to risky polyproduct user groups. For chronic polyproduct users, who present with the highest levels of subsequent and mental health problems, more intensive, multidimensional prevention programming (eg, mental health counseling in addition to substance use prevention/cessation programs) may be fruitful for preventing a myriad of adverse risk outcomes. For the larger segment of youth who experiment e-cigarettes and hookah primarily at the outset of high school (similar to the polyproduct users in this study), escalating combustible cigarette use risk may be a concern that warrants additional intervention focus as well as a considering programming to address the moderate increase in risk of substance use and mental health problems. Future research should examine potential mechanisms of protective factors for developing targeted interventions based on multidimensional characterizations of polytobacco product use. Also, consistent with prior research indicating that use of e-cigarettes and multiple tobacco products is prevalent in Hispanic youth,4 we found that Hispanic youth constitute more than 50% of the Chronic polyproduct user and Polyproduct user groups. This finding reinforces the need for research focusing on tobacco-related health disparities among ethnic minority groups, particularly during adolescence.
Strengths of this study include the large and demographically diverse sample, repeated follow-up assessment strategy over a 2-year period, low attrition rate, modeling of complex patterns of comorbid tobacco trajectories, and adjustment for baseline outcomes as well as potential confounders. To minimize participant burden on students and schools, this study only included self-report measures, which can result in measurement limitations. Although the past 6-month use of each tobacco product was reported only as a binary outcome (yes/no), we also examined past 30-day frequency of product use where data was available—and these responses closely matched the past 6-month cigarette use prevalence (see Supplementary Table S2). Future research should utilize past 30-day frequency of tobacco product use in GMM models to capture greater variability in more frequent patterns of use. Additionally, e-cigarettes and hookah may contain variable amounts of nicotine,46 and adolescents may not be aware if the e-cigarettes or hookah they are using contain nicotine;51 hence, the extent to which these findings reflect targets for regulatory policy targeting products with nicotine is not known.
These limitations notwithstanding, the present study could serve as a methodological and conceptual template for future work investigating developmental patterns of polytobacco use among youth at a time of increasing diversity of tobacco products. More broadly, research like the current study that increases understanding of diverse developmental patterns of polytobacco use and their relations with subsequent health risks can inform researchers and policy makers regarding the prevalence and potential consequences of concurrent use of multiple tobacco products. If the associations demonstrated here were eventually determined to be causal, these results suggest that policy and prevention reducing the appeal of and access to various tobacco products may reduce the substance use and mental health burden in current and future generations of youth. In an increasingly diverse market place in which tobacco products and their use patterns are becoming more complex, it will be important to continue characterizing patterns of use and co-use of multiple tobacco products in ongoing surveillance of adolescents. As the marketplace and policy landscape continues to evolve, such evidence will be necessary to determine whether, amongst youth, polyproduct use remains the norm and increases risk of adverse substance use and mental health outcomes.
Supplementary Material
Supplementary data are available at Nicotine & Tobacco Research online.
Funding
This research was supported by National Institutes of Health grant R01-DA033296. The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Declaration of Interests
None declared.
Acknowledgments
JC is the principal investigator responsible for study conception and conducted the analyses. JC, NIG, and AML lead the conceptualization of the study and wrote most the manuscript text. RM, JLB, CC, SYS, NRR, and MDS aided in study conceptualization and provided feedback on drafts. MDS and JC oversaw data management and processing. AML and JC had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Supplement Sponsorship
This supplement was sponsored by the Center for the Evaluation and Coordination of Training and Research for Tobacco Regulatory Science (5U54CA189222).
References
- 1. Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance - United States, 2015. MMWR Surveill Summ. 2016;65(6):1–174. [DOI] [PubMed] [Google Scholar]
- 2. Wang B, King BA, Corey CG, Arrazola RA, Johnson SE. Awareness and use of non-conventional tobacco products among U.S. students, 2012. Am J Prev Med. 2014;47(2 Suppl 1):S36–S52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Johnston LD, O’Malley PM, Miech RA.. Monitoring the Future National Survey Results on Drug Use: 1975–2016: Overview of key Findings on Adolescent Drug Use. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2017. [Google Scholar]
- 4. Singh T. Tobacco use among middle and high school students—United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2016; 65(14);361–367 [DOI] [PubMed] [Google Scholar]
- 5. Ali M, Gray TR, Martinez DJ, Curry LE, Horn KA. Risk profiles of youth single, dual, and poly tobacco users. Nicotine Tob Res. 2016;18(7):1614–1621. [DOI] [PubMed] [Google Scholar]
- 6. Kowitt SD, Patel T, Ranney LM, Huang LL, Sutfin EL, Goldstein AO. Polytobacco use among high school students. Int J Environ Res Public Health. 2015;12(11):14477–14489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mermelstein RJ. Adapting to a changing tobacco landscape: research implications for understanding and reducing youth tobacco use. Am J Prev Med. 2014;47(2 Suppl 1):S87–S89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Collins LK, Villanti AC, Pearson JL, et al. Frequency of youth E-Cigarette, tobacco, and poly-use in the United States, 2015: update to villanti et al., “frequency of youth E-Cigarette and tobacco use patterns in the united states: measurement precision is critical to inform public health”. Nicotine Tob Res. 2017;19(10):1253–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gilreath TD, Leventhal A, Barrington-Trimis JL, et al. Patterns of alternative tobacco product use: emergence of hookah and E-cigarettes as preferred products amongst youth. J Adolesc Health. 2016;58(2):181–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Huh J, Leventhal AM. Progression of polytobacco product use patterns in adolescents. Am J Prev Med. 2016;51(4):513–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arrazola RA, Kuiper NM, Dube SR. Patterns of current use of tobacco products among US high school students for 2000–2012—findings from the National Youth Tobacco Survey. J Adolesc Health. 2014;54(1):54–60. e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nelson SE, Van Ryzin MJ, Dishion TJ. Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: demographic correlates and young adult substance use problems. Dev Psychopathol. 2015;27(1):253–277. [DOI] [PubMed] [Google Scholar]
- 13. Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24(6):882–891. [PubMed] [Google Scholar]
- 14. Gilpin EA, Pierce JP. Concurrent use of tobacco products by California adolescents. Prev Med. 2003;36(5):575–584. [DOI] [PubMed] [Google Scholar]
- 15. Everett SA, Malarcher AM, Sharp DJ, Husten CG, Giovino GA. Relationship between cigarette, smokeless tobacco, and cigar use, and other health risk behaviors among U.S. high school students. J Sch Health. 2000;70(6):234–240. [DOI] [PubMed] [Google Scholar]
- 16. McCabe SE, West BT, Veliz P, Boyd CJ. E-cigarette use, cigarette smoking, dual use, and problem behaviors among U.S. adolescents: results from a national survey. J Adolesc Health. 2017;61(2):155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Creamer MR, Portillo GV, Clendennen SL, Perry CL. Is adolescent polytobacco use associated with alcohol and other drug use?Am J Health Behav. 2016;40(1):117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cavazos‐Rehg PA, Krauss MJ, Spitznagel EL, Grucza RA, Bierut LJ. Youth tobacco use type and associations with substance use disorders. Addiction. 2014;109(8):1371–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Leventhal AM, Strong DR, Sussman S, et al. Psychiatric comorbidity in adolescent electronic and conventional cigarette use. J Psychiatr Res. 2016;73:71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lechner WV, Janssen T, Kahler CW, Audrain-McGovern J, Leventhal AM. Bi-directional associations of electronic and combustible cigarette use onset patterns with depressive symptoms in adolescents. Prev Med. 2017;96:73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bandiera FC, Loukas A, Li X, Wilkinson AV, Perry CL. Depressive symptoms predict current E-Cigarette use among college students in Texas. Nicotine Tob Res. 2017;19(9):1102–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Eaton DK, Kann L, Kinchen S, et al. ; Centers for Disease Control and Prevention (CDC). Youth risk behavior surveillance - United States, 2009. MMWR Surveill Summ. 2010;59(5):1–142. [PubMed] [Google Scholar]
- 24. Radloff LS. The use of the center for epidemiologic studies depression scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149–166. [DOI] [PubMed] [Google Scholar]
- 25. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 26. Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the revised child anxiety and depression scale in a clinical sample. Behav Res Ther. 2005;43(3):309–322. [DOI] [PubMed] [Google Scholar]
- 27. Barkley RA, . Attention-deficit Hyperactivity Disorder: A Clinical Workbook. Medifocus_com Inc; 1991. [Google Scholar]
- 28. Cardenas VM, Breen PJ, Compadre CM, et al. The smoking habits of the family influence the uptake of e-cigarettes in US children. Ann Epidemiol. 2015;25(1):60–62. [DOI] [PubMed] [Google Scholar]
- 29. Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control. 1998;7(4):409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Muthén B, Asparouhov T. Growth mixture modeling: analysis with non-Gaussian random effects. In: Fitzmaurice, ed. Longitudinal Data Analysis. Boca Raton, FL: CRC Press; 2008:143–165. [Google Scholar]
- 31. Muthén B. Statistical and substantive checking in growth mixture modeling: comment on Bauer and Curran (2003). Psychol Methods. 2003;8(3):369–77. [DOI] [PubMed] [Google Scholar]
- 32. Wagner B, Riggs P, Mikulich-Gilbertson S. The importance of distribution-choice in modeling substance use data: a comparison of negative binomial, beta binomial, and zero-inflated distributions. Am J Drug Alcohol Abuse. 2015;41(6):489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Muthén LK, Muthén BO. Mplus User’s Guide: Statistical Analysis with Latent Variables, 7th ed. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 34. Westling E, Rusby JC, Crowley R, Light JM. Electronic cigarette use by youth: prevalence, correlates, and use trajectories from middle to high school. J Adolesc Health. 2017;60(6):660–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Barnett TE, Soule EK, Forrest JR, Porter L, Tomar SL. Adolescent electronic cigarette use: associations with conventional cigarette and hookah smoking. Am J Prev Med. 2015;49(2):199–206. [DOI] [PubMed] [Google Scholar]
- 36. Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatr. 2015;169(11):1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control. 2016: doi: 10.1136/tobaccocontrol-2015-052705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Barrington-Trimis JL, Urman R, Berhane K, et al. E-cigarettes and future cigarette use. Pediatrics. 2016;138(1):e20160379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Miech R, Patrick ME, O’Malley PM, Johnston LD. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob Control. 2017: doi: 10.1136/tobaccocontrol-2016-053291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Brown RA, Lewinsohn PM, Seeley JR, Wagner EF. Cigarette smoking, major depression, and other psychiatric disorders among adolescents. J Am Acad Child Adolesc Psychiatry. 1996;35(12):1602–1610. [DOI] [PubMed] [Google Scholar]
- 41. Cohn A, Villanti A, Richardson A, et al. The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addict Behav. 2015;48:79–88. [DOI] [PubMed] [Google Scholar]
- 42. Demissie Z, Everett Jones S, Clayton HB, et al. Adolescent risk behaviors and use of electronic vapor products and cigarettes. Pediatrics. 2017;139(2):e20162921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Everett SA, Malarcher AM, Sharp DJ, Husten CG, Giovino GA. Relationship between cigarette, smokeless tobacco, and cigar use, and other health risk behaviors among U.S. high school students. J Sch Health. 2000;70(6):234–240. [DOI] [PubMed] [Google Scholar]
- 44. Cameron JM, Howell DN, White JR, Andrenyak DM, Layton ME, Roll JM. Variable and potentially fatal amounts of nicotine in e-cigarette nicotine solutions. Tob Control. 2014;23(1):77–78. [DOI] [PubMed] [Google Scholar]
- 45. Dwyer JB, McQuown SC, Leslie FM. The dynamic effects of nicotine on the developing brain. Pharmacol Ther. 2009;122(2):125–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Counotte DS, Goriounova NA, Li KW, et al. Lasting synaptic changes underlie attention deficits caused by nicotine exposure during adolescence. Nat Neurosci. 2011;14(4):417–419. [DOI] [PubMed] [Google Scholar]
- 47. Goriounova NA, Mansvelder HD. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb Perspect Med. 2012;2(12): a012120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Parrott AC. The Psychobiological Problems of Continued Nicotine Dependency in E-Cigarette ‘Vapers’. Commentary: “Electronic Cigarettes”. Front Psychiatry. 2015;6:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Dutra LM, Glantz SA. Electronic cigarettes and conventional cigarette use among U.S. adolescents: a cross-sectional study. JAMA Pediatr. 2014;168(7):610–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wills TA. E-cigarettes and adolescents’ risk status. Pediatrics. 2017;139(2):e20163736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Morean ME, Kong G, Cavallo DA, Camenga DR, Krishnan-Sarin S. Nicotine concentration of e-cigarettes used by adolescents. Drug Alcohol Depend. 2016;167:224–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.