A perspective on how training programs can improve our pipeline of future physician-scientists is presented.
Keywords: physician scientist, medical scientist training program, diversity, pipeline
Abstract
Perhaps the most dramatic finding in the 2014 National Institutes of Health Physician-Scientist Workforce Working Group Report is the aging of the physician-scientist workforce. There are currently 1.6-fold more physician-scientists over the age of 61 than under the age of 50, indicating that our pipeline of physician-scientists is insufficient to maintain current numbers. Several factors likely contribute to this leaky pipeline, including the long training periods, poor compensation during training, diminished funding odds for young investigators, and lack of role models, particularly for women and underrepresented minorities. This perspective will present several ideas for how training programs can play a role in assuring a robust pipeline of future physician scientists.
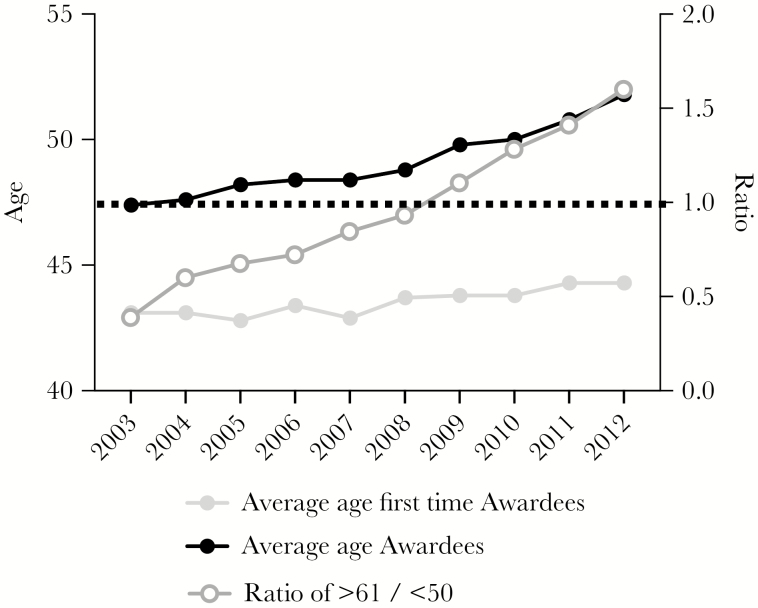
In 2014, the National Institutes of Health (NIH) released the Physician-Scientist Workforce Working Group Report [1]. This report particularly highlighted the aging of the physician-scientist workforce, continuing to sound an alarm originally raised by Dr. Wyngaarden in 1979, in which he famously described the clinical investigator as an endangered species [2]. The latest report indicates that from 2003 to 2012 the overall number of physician-scientists has been stable, but there have been substantial declines in the numbers of physician-scientists between 31 and 50 years of age, with corresponding increases in those over 61 years of age. In fact, there has been an inversion in the proportion of older to younger investigators in just one decade, at a rate which exceeds the aging of NIH grant recipients (Figure 1). These data suggest that we need better mechanisms to help young investigators compete with older ones for grants, but also raises a critical question about the future of the physician-scientist workforce. With 1.6-fold more investigators over the age of 61 than under the age of 50, who will replace these investigators as they retire?
Figure 1.
The aging of the physician-scientist workforce. The ratio of investigators ≥61 years to those ≤50 years, the age at first Research Project Grant (R01) for MD/PhDs, and the age of all MD/PhD awardees are displayed. Data are from [1].
In response to these troubling data, the Physician-Scientist Working Groups and several other individuals and organizations have released recommendations to confront this impending problem [3–5]. Rather than reiterate all these excellent recommendations, I would like to focus on my personal perspectives about how we can improve training programs to support the pipeline of physician investigators. The infectious disease community in particular has much to benefit from such efforts. With our focus on diseases that are often rare and/or neglected, and that disproportionately affect those in resource-poor settings, we need to encourage the best and brightest that a career as a physician-scientist is a rewarding, sustainable path to impart positive change in the world.
I’ll particularly focus on organized programs such as the NIH-funded Medical Scientist Training Program (MSTP), though I hope these perspectives resonate for faculty and trainees involved in physician-scientist training in all types of programs and at all levels. An important motivation for this perspective is that the number of students applying to, and matriculating into, the MSTP has remained stable in recent years—yet there are fewer making it into the workforce—indicating that we are losing many along the way. Many factors likely contribute to this drop-out, including worries about the ability to sustain research funding, the long length of training, personal debt, and increased pressure to perform clinical duties. In my experience, these pressures are often more acute for MDs performing research without a PhD, or for those who pursued both degrees independently. While there are no easy fixes, my goal is to begin a discussion about changes we can make now to limit the leakiness of this pipeline.
As outlined by others in this issue, physician-scientists are a critical component of our workforce who have made ground-breaking discoveries that have improved health and changed lives. One only needs to read Dr. Merigan’s perspective in this issue on how HIV/AIDS went, in a single generation, from a universally fatal disease to one compatible with a full life, to believe this. We have a responsibility as a community to nurture our trainees, and to make sure that they feel there is a future for them as a physician-scientist. While my views are shaped by my experiences as a former MSTP trainee and current associate MSTP program director, this perspective reflects my personal views, and should not be construed as programmatic recommendations.
FIGHT MISPERCEPTIONS THAT PHYSICIAN-SCIENTIST TRAINING PROGRAMS DON’T WORK
Perhaps my experiences are atypical, but I’ve had multiple very senior investigators (both MD and PhD trained) tell me that MSTP and other physician-scientist training programs don’t work because the vast majority of graduates don’t stay in research. This is simply not true, but if this kind of misinformation is floating around, it can only have a chilling effect on our trainees. Historically, organized programs like the MSTP have been very successful, with more than 80% of trainees remaining in biomedical research, and the programs have very low program attrition rates [6–8]. While here I have focused primarily on US-based programs, similar analyses of the Swiss and Canadian MD-PhD training programs reveal similar success rates [9, 10]. We must make it clear to our trainees and prospective trainees that such training programs are a viable career path.
ESTABLISH A DEDICATED PHYSICIAN-SCIENTIST ADVISOR
We all recognize that mentors are critical to our professional development, and I will be the first to tell students that choosing the best mentors is the most important part of their professional development. I would never be where I am today without the guidance from a remarkable array of physicians and scientists. Despite this, when I was a trainee I found the experience to be lonely and isolating at times, as I never fully fitted in with either my medical or graduate school colleagues. Transitions between the medical and research training can be particularly difficult to navigate. Such feelings can be exacerbated by separate mentors in the clinical and research realms, who may provide conflicting advice. To provide better continuity in navigating these training challenges, we have recently instituted a new program at Stanford in which each incoming MSTP student is assigned an advisor who is a dedicated physician-scientist to advise the student throughout the entire training program. This advisor must be committed to this task; our advisors are within our MSTP directorate. The advisor meets with the students regularly throughout the entire program, with particular attention in the early years and during transitions, to provide advice on selecting a laboratory, preparing for exams, navigating the re-entry to clinics, and choosing a residency. The advantage to the student is to have one person they can go to, at any time, who understands milestones of their dual degree program. While the program is only a few years old, we have received very positive feedback from our students, and hope that this will help us shorten the time to dual degree by anticipating and overcoming potential delays.
ENHANCE THE DIVERSITY OF OUR TRAINING PROGRAMS
As also discussed by Dr. Upinder Singh in this issue, enhancing the diversity of our physician-scientist workforce will play a critical role in sustaining the pipeline. Women and underrepresented minorities (URM) still make up a small fraction of the workforce, yet there are ample data from the business world that diverse groups function better [11]. This is particularly critical as science moves increasingly to a “Team Science” model, in which a diverse population, in terms of sex, gender, race, ethnicity, and training path, is more likely to drive innovation and discovery. We need to enhance our efforts to recruit and retain URM and female candidates in physician-scientist training programs.
There are several actions we can take immediately to improve our recruitment and retention of diverse candidates. First, all admissions committee members should receive training in bias (conscious and unconscious) and how to recognize and limit it. Second, we should improve our efforts to expose URM candidates and women to research at a younger age. Qualitative research from the NIH working report indicates that URM students are far less likely to have been exposed to research and/or recognize the possibility of a research career until they enter medical school, while most MSTP applicants are white and decided to pursue MSTP early (often in high school), based on their personal experiences [1]. To try to close this gap, physician-scientists should make an effort to visit high schools and colleges that serve URM populations to discuss their career and its possibilities. Many undergraduates at colleges without medical school affiliation do not even realize that combined degree training is possible. Further, physician-scientist mentors should be strongly encouraged (and even incentivized, if the institution is willing) to allow these young students opportunities for summer laboratory internships. Third, we should continue to support and expand pipeline programs, such as those at Stanford or Weill Cornell’s Gateway Program, that target URM to bring them into the lab in high school or college [12]. Finally, offering later entry into physician-scientist training programs can provide opportunities for those who were not exposed to research until medical school. Many MSTPs, such as those at Stanford and University of California, San Francisco, offer an “internal MSTP track” to apply in the first or second year of medical school. This can provide a critical pathway for those who may not have been exposed to research until medical school.
BE A POSITIVE ROLE MODEL ABOUT PHYSICIAN-SCIENTIST CAREERS
I suspect I am not the only physician-scientist who complains about the stresses surrounding funding, balancing clinical, research, and teaching time, and attaining work-life balance. By the same token, I suspect that most of us who are involved in the training of physician-scientists do it because we love it. So, while it is reasonable to present the advantages and disadvantages of the physician-scientist career, we need to make sure that we are presenting the positives as well as the negatives so that we don’t dismay our trainees, regardless of the current funding climate.
ASSURE SUFFICIENT MENTORING AND RESOURCES FOR RECIPIENTS OF INDIVIDUAL NRSAS
One of the major recommendations of the physician-scientist workforce that has already been implemented was to increase funding for individual National Research Service Awards (NRSAs), shifting some of the focus away from institutional T32 awards. I sincerely hope this shift has the desired effect of increasing program diversity and training opportunities for a broad array of physician-scientists. However, we need to ensure that sufficient institutional resources and mentoring are in place to guarantee a successful training program for these individual training grant recipients, particularly if their institution does not have a T32. Every effort should be made to establish a sense of community for physician-scientist trainees at institutions lacking a MSTP. This community should focus on developing mentorship networks and funding support to foster the careers of physician-scientist trainees. Training grants typically provide only 20%–25% of the support needed for the student, and having research and clinical mentors who are engaged and supportive is critical. Data should be collected on outcomes from individuals training at programs with and without institutional MSTPs to identify factors associated with a successful training program.
COUNSEL ABOUT CHOOSING APPROPRIATE RESIDENCY AND FELLOWSHIP PROGRAMS
As our trainees prepare to move on, we must also provide them the tools to evaluate which future paths will support an investigative career. We need to make sure our trainees are prepared to ask the right questions when they interview for residencies and fellowships. They should ask specific questions about protected time for research, the availability of mentors, and the availability of funding to support such efforts. Further, we need to educate chairs and division chiefs about the benefits of recruiting physician-scientists to their ranks in light of the unique perspectives they can add, even if divisional or departmental clinical revenues may be diminished.
SHORTEN LENGTH OF TRAINING
This has been a highly contentious issue and there is no easy solution. However, better integration of medical school and graduate school curriculum could shorten training periods and simultaneously reduce the costs of medical education. Allowing flexibility in course requirements and sequencing can have a significant impact in this arena. For instance, at Stanford we promote flexibility, allowing our students to select a laboratory for thesis work early in their training, without a set requirement for the length and number of rotations in different labs. Many students are able to do a series of minirotations in their first year of medical school, giving them a jump start on their thesis research in their second year of medical school, translating to significant streamlining of their combined degree program. We also offer students the opportunity to do some of their clinical clerkships early, which can be particularly helpful during periods of down-time during research, such as time waiting for reagents, animal husbandry, or ethics approvals. These clerkships can occur prior to or during the PhD studies. Finally, many universities are exploring curriculum reform in an effort to streamline course requirements, and such efforts should be supported by physician-scientists.
There are many additional changes we can all make to enhance the recruitment and retention of the next generation of physician-scientists, such as helping our students select excellent mentors and sponsors; supporting the mental health of our trainees during the long, arduous training program; making sure research-oriented faculty play a role in medical school decisions; and having (likely difficult) conversations at the institutional levels about the relative sizes of graduate programs versus physician-scientist training programs. I hope that this perspective can serve to begin a conversation for actions we can take now to improve the pipeline of physician-scientists for the future.
Notes
Acknowledgments. I would like to thank the present and past leadership of the Stanford MSTP, Drs Paul J. (PJ) Utz, Katrin Chua, Matthew Porteus, Dean Felsher, and Julien Sage for helpful discussions and their thoughtful approach to MSTP leadership. I would also like to thanks Drs Utz and Singh for critical reading of the manuscript and highly fruitful discussions. Thanks also to Dr Mathieu Le Gars for assistance with the figure.
Financial support. Dr Blish is supported by the Talia and John Morgridge Faculty Scholar from thek Stanford Child Heath Research Institute, NIH Director’s New Innovator Award (grant number DP2AI11219301), and NIH (grant numbers U01AI131302, R56AI124788, R21AI130523), and is a Chan Zuckerberg Investigator.
Supplement sponsorship. This work is part of a supplement sponsored by the Ragon Institute of MGH, MIT, and the Harvard University Center for AIDS Research P30 AI060354.
Potential conflicts of interest. No reported conflicts of interest. The author has submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Feldman AM. The National Institutes of Health Physician-Scientist Workforce Working Group report: a roadmap for preserving the physician-scientist. Clin Transl Sci 2014; 7:289–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wyngaarden JB. The clinical investigator as an endangered species. N Engl J Med 1979; 301:1254–9. [DOI] [PubMed] [Google Scholar]
- 3. Milewicz DM, Lorenz RG, Dermody TS, Brass LF; National Association of MD-PhD Programs Executive Committee Rescuing the physician-scientist workforce: the time for action is now. J Clin Invest 2015; 125:3742–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Garrison HH, Deschamps AM. NIH research funding and early career physician scientists: continuing challenges in the 21st century. FASEB J 2014; 28:1049–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Furuya H, Brenner D, Rosser CJ. On the brink of extinction: the future of translational physician-scientists in the United States. J Transl Med 2017; 15:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Akabas MH, Brass LF. A closer look at attrition in MD-PhD programs. Acad Med 2014; 89:958. [DOI] [PubMed] [Google Scholar]
- 7. Brass LF, Akabas MH, Burnley LD, Engman DM, Wiley CA, Andersen OS. Are MD-PhD programs meeting their goals? An analysis of career choices made by graduates of 24 MD-PhD programs. Acad Med 2010; 85:692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jeffe DB, Andriole DA, Wathington HD, Tai RH. Educational outcomes for students enrolled in MD-PhD programs at Medical School Matriculation, 1995–2000. Acad Med 2014; 89:84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Skinnider MA, Squair JW, Twa DDW, et al. Characteristics and outcomes of Canadian MD/PhD program graduates: a cross-sectional survey. CMAJ Open 2017; 5:E308–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kuehnle K, Winkler DT, Meier-Abt PJ. Swiss national MD-PhD-program: an outcome analysis. Swiss Med Wkly 2009; 139:540–6. [DOI] [PubMed] [Google Scholar]
- 11. Phillips KW. How diversity works. Sci Am 2014; 311:42–7. [DOI] [PubMed] [Google Scholar]
- 12. Gotian R, Raymore JC, Rhooms SK, Liberman L, Andersen OS. Gateways to the laboratory: how An MD-PhD program increased the number of minority physician-scientists. Acad Med 2017; 92:628–34. [DOI] [PubMed] [Google Scholar]