Abstract
Background
Despite increasing evidence for the benefits of psychological treatments (PTs) in low- and middle-income countries, few national health systems have adopted PTs as standard care. We aimed to evaluate the effectiveness of a group interpersonal psychotherapy (IPT-G) intervention, when delivered by lay community health workers (LCHWs) in a low-resource government health system in Uganda. The intended outcome was reduction of depression among caregivers of children with nodding syndrome, a neuropsychiatric condition with high morbidity, mortality and social stigma.
Methods
A non-randomized trial design was used. Caregivers in six villages (n = 69) received treatment as usual (TAU), according to government guidelines. Caregivers in seven villages (n = 73) received TAU as well as 12 sessions of IPT-G delivered by LCHWs. Primary outcomes were caregiver and child depression assessed at 1 and 6 months post-intervention.
Results
Caregivers who received IPT-G had a significantly greater reduction in the risk of depression from baseline to 1 month [risk ratio (RR) 0.25, 95% confidence interval (CI) 0.10–0.62] and 6 months (RR 0.33, 95% CI 0.11–0.95) post-intervention compared with caregivers who received TAU. Children of caregivers who received IPT-G had significantly greater reduction in depression scores than children of TAU caregivers at 1 month (Cohen’s d = 0.57, p = 0.01) and 6 months (Cohen’s d = 0.54, p = 0.03). Significant effects were also observed for psychological distress, stigma and social support among caregivers.
Conclusion
IPT-G delivered within a low-resource health system is an effective PT for common mental health problems in caregivers of children with a severe neuropsychiatric condition and has psychological benefits for the children as well. This supports national health policy initiatives to integrate PTs into primary health care services in Uganda.
Introduction
The implementation of evidence-based interventions for mental, neurological and substance use (MNS) disorders can reduce the substantial treatment gap in low- and middle-income countries (LMICs), where up to 90% of those in need do not have access to mental health services (Whiteford et al. 2013; Wainberg et al. 2017) and only 4–11% of persons with depression receive minimally adequate care (Thornicroft et al. 2017). The use of non-specialist health workers to deliver mental health treatments is a crucial component of reducing this treatment gap (Singla et al. 2017; Wainberg et al. 2017).This strategy is referred to as a ‘task-shifting’ or ‘task-sharing’ approach, in which components of traditionally specialized health care are delegated to existing or new cadres with either less training or narrowly tailored training for the required service (Fulton et al. 2011).
The World Health Organization (WHO) mental health Global Action Programme (mhGAP) (World Health Organization, 2016) and Disease Control Priorities network project (Patel et al. 2016) recommend that psychological treatments (PTs) be integrated into primary care and community services through task-sharing approaches. Despite this evidence, the use of lay community health workers (LCHWs) for the provision of mental health services in LMICs is not widespread and varies considerably across countries.
In Uganda, there is a unique opportunity to advance integration of PTs into the public health system because of an existing policy environment. The national health policy includes mental health as one of 12 components of the National Minimum Health Care Package to be provided at all levels of care (Kigozi et al. 2010). Following recommendations from the WHO, the Uganda Ministry of Health recently took steps to scale-up the provision of evidence-based PTs within primary care. LCHWs form the first tier of the health system in Uganda but their involvement to date in MNS programming is lacking (Kigozi et al. 2010; Bazos et al. 2015). Randomized controlled trials of PTs in Uganda indicated that group interpersonal psychotherapy (IPT-G), a WHO recommended treatment, had demonstrated effectiveness in the treatment of mental disorders when delivered by trained LCHWs (Bolton et al. 2003, 2007). However, these treatments were provided outside the government health system and delivered by paid non-governmental organization (NGO) staff who had high levels of supervision and support from mental health experts in high-income countries. There is a lack of studies demonstrating the effectiveness of PTs delivered by LCHWs in the Uganda government health system.
The objective of this study was to demonstrate that LCHWs within the government health system could effectively deliver a PT. The intended beneficiaries were caregivers and their children with nodding syndrome (NS), an unexplained neuropsychiatric disorder similar to epilepsy that afflicts more than 3000 children and adolescents in northern Uganda (Idro et al. 2013, 2016). NS is characterized by head nodding episodes, epileptic seizures, mental and physical deterioration (Idro et al. 2013). The cause is unknown; however, there is a strong epidemiological association with onchocerciasis (Idro et al. 2016; Johnson et al. 2017). The burden of NS is exacerbated by frequent co-occurrence of common mental health problems in both the affected child and his/her caregiver. A post-conflict setting in northern Uganda and substantial stigma serve as additional contextual risk factors for poor mental health (Idro et al. 2013; Buchmann, 2014; Mutamba et al. 2014; Mwaka et al. 2015; Nakigudde et al. 2016). Not only do depression and post-traumatic stress disorder (PTSD) remain prevalent in northern Uganda (Roberts et al. 2008; Mugisha et al. 2015a, d), but caregivers to children with neuropsychiatric disorders have been found to have high levels of psychiatric morbidity (Okewole et al. 2011). Caregiver mental health – by influencing factors such as connectedness, access to services and availability of social support – mediates child mental health and behavioural outcomes (Elbedour et al. 1993; Beardselee et al. 1998; Betancourt, 2011; Betancourt et al. 2012). Relatedly, parent-mediated interventions have shown evidence for improving mental health of the ill child (Rahman et al. 2008; Shaw et al. 2009; Stadnick et al. 2015) highlighting the key role of caregiver treatments in child and adolescent mental health interventions (Morris et al. 2011).
This study coincided with the roll-out of Uganda national management guidelines for NS, which advise a multidisciplinary treatment approach including psychosocial support for families affected by the disorder (Idro et al. 2013). The guidelines do not include, however, recommendations or protocols for PTs. Therefore, evaluation and subsequent implementation of a community psychosocial intervention using a task-shifting approach has potential to complement the government health response to NS and expand the evidence base for potential nationwide psychological services in government health care.
Method
This study was a non-randomized trial with caregivers in a control arm receiving treatment as usual (TAU) and caregivers in an experimental arm receiving IPT-G in addition to TAU. We employed a quasi-experimental design that ‘takes advantage of unplanned events to assess the impact of an exposure or an intervention on a well-defined group of people who happened to be affected by that event and where randomization may not be practical’ (Ford, 2003). A randomized trial was not considered feasible due to: restriction by the government to conduct the intervention in a particular area; the group format of the intervention; a high probability of contamination of intervention effects between IPT-G and ongoing NS psychosocial programmes by other agencies within the study district; and the diffuse social nature of stigma against NS. The study was conducted over a period of 18 months in northern Uganda between April 2013 and September 2014.
We obtained approval for the study from the Makerere University College of Health Sciences, School of Public Health Higher Degrees, Research and Ethics Committee, and the Uganda National Council of Science and Technology. Informed consent was obtained from all the participants after the purpose, procedures, risk and benefits of the study were explained. The trial was retrospectively registered (ISRCTN11382067; registration date: 6 June 2016).
Study participants and procedures
Thirteen villages in northern Uganda were selected for inclusion in the study. Using health facility (HF) records, seven villages were assigned to the IPT-G condition and six villages were assigned to TAU based on the number of families affected in a village. Caregivers were recruited by LCHWs referred to as village health team members (VHTs). A caregiver was included in the study if she/or he was an adult (≥;18 years of age) living in the selected study villages, was a primary caregiver for a child with NS and willingly provided informed written consent. A child was included if they had NS and a consenting caregiver with them. In families with more than one child with NS (approximately 30%), caregivers were asked to identify one of their children most affected by NS that would participate in the study. Following consent by the caregiver, trained health workers conducted assessments and recorded baseline demographic and outcome measures from both caregivers and children.
Study intervention
Group interpersonal psychotherapy
We used the Replicating Effective Programs (REP) framework (Kilbourne et al. 2007) to identify, adapt, implement and evaluate an appropriate intervention. IPT-G was selected as the PT of choice because it is a WHO-endorsed psychosocial intervention for LMICs (World Health Organization, 2016) and has an evidence base of prior randomized controlled trials conducted in Uganda (Bolton et al. 2003, 2007).
Interpersonal psychotherapy (IPT) is a brief attachment-focused PT that was initially designed to treat depressive symptoms by improving interpersonal functioning and social support (Klerman et al. 1984; Weissman et al. 2000). It was originally developed as an individual therapy but can be delivered in group format (Bolton et al. 2003, 2007; Petersen et al. 2012). IPT involves the therapist and client conceptualizing the patient’s difficulties in relation to the patient’s key relationships and focusing on one of four problem areas: interpersonal dispute, grief and loss, role transitions and interpersonal sensitivity (Weissman et al. 2000). In a meta-analysis of 90 IPT studies, including 22 that used group format, the therapy had a moderate to large effect size (g = 0.60; 95% confidence interval (CI) = 0.45–0.75) for acute-phase depression and there is no evidence that it is less effective than cognitive behaviour therapy and other PTs (Cuijpers et al. 2016).
Table 1 provides an overview of the implementation adaptations to make delivery feasible in government health services.
Table 1.
Adaptations of group interpersonal therapy (IPT-G) for delivery in government health systems
| Prior implementation of IPT-G by non-governmental organizations (NGO) in Uganda (Bolton et al. 2003, 2007, Verdeli et al. 2003, 2008) | Adaptations for IPT-G in Uganda government health system | |
|---|---|---|
| Setting | Rural communities and internally displaced camps in southwest and northern Uganda | Rural communities in northern Uganda |
| Delivery agent | Compensated NGO workers with English-language proficiency and literacy without prior health training | Volunteer government community health workers without literacy requirements and with prior 2–5 days training in basic physical health prevention and promotion |
| Training | 13–14 days training delivered by high-income country psychologists with expertise in IPT | 7 days initial training plus 2-day refresher training delivered by Ugandan IPT-G experts |
| Supervision | Delivered in person by high-income country psychologist with expertise in IPT | Delivered by primary health workers working at government health facilities with no prior training in IPT, in conjunction with IPT-G experts and a clinical psychologist from Uganda |
| Beneficiaries | Community members living with HIV/AIDs in southwest Uganda and survivors of political violence in northern Uganda | Survivors of political violence with children affected by NS in northern Uganda |
| Content of IPT-G | Culturally adapted IPT-G, with removal of ‘interpersonal deficits’ component for the adult intervention but retained for adolescents | Same content as NGO version with revision to address VHT needs, and addition of NS-specific content |
| Duration of IPT-G | 16 weekly 90–120 min sessions | 12 weekly 90–120 min sessions |
Caregivers in the intervention villages received 12 weekly 90–120 min IPT-G sessions in addition to usual care for NS (see TAU description below). IPT-G sessions were of mixed-gender and consisted of 10–16 individuals per group. Group sessions were held at jointly agreed meeting places in the community and delivered by IPT-G trained LCHWs. A 7-day training for LCHWs was led by IPT experts in Uganda who had previously participated in NGO delivery of IPT (Bolton et al. 2003, 2007). Supervision was conducted by government health workers who attended the same training. Both the LCHWs and primary health workers attended a weekly, joint supervision meeting facilitated by the IPT-G experts.
Treatment as usual
All health workers at HFs in the study sites received training on the medical management of children with NS. Caregivers in the TAU and experimental-arm villages received usual care as provided for in the national management guidelines for NS (Idro et al. 2013). TAU included health education about NS, syndromic management of children with pharmacological agents (typically sodium valproate or carbamazepine), caregiver education and supportive counselling (Idro et al. 2013). The LCHWs received separate training on community case identification and health promotion for NS, provided by government health workers.
Instruments
All caregivers completed a battery of instruments at three time points: baseline, 1 month post-treatment and 6 months post-treatment. Interviews were conducted in-person by trained research assistants and lasted an average of 45 min. Caregivers completed a battery of mental health and psychosocial instruments for one index child with NS. Older children of at least 10 years of age and adolescents (more than 80% in both arms) were encouraged to participate in the interview process to provide additional details when caregivers lacked information or were unaware of specific mental health complaints. Training of research assistants in the application of the different study instruments was done by a psychiatrist fluent in Luo – the local language spoken by participants. All instruments were translated from English to Luo and back-translated and piloted. The study instrument included the following battery of assessments:
Caregiver outcomes
Depression, generalized anxiety disorder (GAD), PTSD and suicide risk assessment were measured using the MINI Neuropsychiatric interview (Version 5.0) (Sheehan et al. 1998). The MINI has been used in several Ugandan populations (Abbo et al. 2009; Kinyanda et al. 2011) including Luo (Nakimuli-Mpungu et al. 2015; Mugisha et al. 2015b, c).
Psychological distress was assessed using the Self Report Questionnaire (SRQ-20).The instrument has been validated and widely used in Uganda (Nakigudde et al. 2005; Nakimuli-Mpungu et al. 2013) with high internal reliability of α = 0.97 in a similar study population (Nakimuli-Mpungu et al. 2013).
Functional impairment was assessed using the Assessment of Functioning questionnaire, a locally developed dimensional tool with a Cronbach α of 0.71 in this population. The scale consists of five categories of tasks including household (e.g. washing clothes), field (e.g. grazing animals), social (e.g. attending social events) and job-related or school-related tasks (e.g. participating in income-generating activities, attending school) and tasks related to personal hygiene (e.g. bathing) (Nakimuli-Mpungu, 2012; Nakimuli-Mpungu et al. 2013, 2015).
Hazardous alcohol use was assessed using the Alcohol Use Disorders Identification Test (AUDIT). The AUDIT consists of 10 items addressing the frequency, quantity and effect of drinking with a recall period of the previous 1 year. The AUDIT has been used in similar populations in northern Uganda with high internal reliability (α = 0.91) (Roberts et al. 2011).
Social support was measured using the adapted version of the Multidimensional Scale of Perceived Social Support (MSPSS) (Zimet et al. 1988). The MSPSS psychometric properties have been tested in Uganda and found to have good internal consistency and validity in a Ugandan population (α = 0.83) (Nakigudde et al. 2009).
Perceived stigma was assessed using the Devaluation of Consumer Scale, which estimates the extent to which caregivers believe that people devalue families that include one or more persons who have serious mental illness (Struening et al. 2001). The scale has been used in two studies involving caregivers to patients with Schizophrenia and Epilepsy in Uganda (Aganyira, 2013; Ayikoru, 2015).
Number and history of war-related traumatic events was assessed using the traumatic events checklist, a 16-item, locally developed tool which inquires as to whether a participant has a war-related traumatic experience or not (Nakimuli-Mpungu et al. 2013).
Child outcomes
Depression was assessed using the 18-item Depression Self-rating Scale (DSRS) (Birleson, 1981). The DSRS has shown good validity and reliability in low-resourced settings (Kohrt et al. 2011).
General psychological distress was assessed by the Strengths and Difficulties Questionnaire (SDQ) (Goodman et al. 2000). The SDQ has 25 items organized under five scales of five items each, scored on a three-point Likert scale. It has been used in similar settings in Uganda (Okello et al. 2007; Kinyanda et al. 2013) with a sensitivity of ≥60% and adequate specificity in a child/adolescent population in north and east Uganda (Kinyanda et al. 2013).
Child perception of parental relationships was assessed with the Inventory of Parent and Peer Attachment (IPPA) (Gullone & Robinson, 2005; Okello et al. 2014). Questions were restricted to the participating caregiver and did not include the peer attachment scale. Among school going adolescents in northern Uganda, the Cronbach α for the mother and father sections of the IPPA was 0.85 and 0.88, respectively (Okello et al. 2014).
PTSD symptoms were measured with the Revised Child Impact of Event Scale (CRIES-13), which consists of 13 items on intrusion, avoidance and arousal symptoms scored on a four-point scale (Perrin et al. 2005).
We used the Adverse Childhood Exposure (ACE) questionnaire (Bruffaerts et al. 2010) at study baseline to examine six context-specific intra-familial childhood adversities before the age of 13 years. The Cronbach α for a sample of adolescents living in a similar setting was 0.94 (Okello et al. 2013, 2014).
Separation anxiety disorder (SAD), GAD and attention-deficit hyperactivity disorder (ADHD) were measured among children using a diagnostic/categorical tool: the MINI International Neuropsychiatric Interview for Children and Adolescents (M.I.N.I.-KID) (Sheehan et al. 2010). It has not been validated for use in Uganda but has been used in similar populations in the country (Okello et al. 2007; Kinyanda et al. 2013).
Statistical analyses
To estimate the sample size for the study, we assumed a 55% prevalence of mild-to-moderate depression among people in northern Uganda (Ovuga et al. 2005) and estimated that the IPT-G intervention would reduce depression in the caregivers by 50% (Bolton et al. 2003). With a level of precision of 5% and power of 80%, the sample size for each arm was calculated to be 57 persons. With an expected attrition of up to 15%, the total sample size was estimated to be 132 people, 66 from each arm.
Data were entered using Epidata 3.1 and analysed using Stata statistical software, version 13 (Stata Corp). We explored completeness of data and the missing data mechanism. Study dropout was associated with gender (male caregivers more likely to drop out, p < 0.01) and number of children (caregivers with greater number of children more likely to drop out, p < 0.01). We therefore assumed that data were missing at random and conducted imputation procedures (10 datasets) using multiple imputation with chained equations (Azur et al. 2011). Linear mixed-effects models were estimated for continuous outcomes (SDQ, IPPA, DSRS, CRIES-13, SRQ, AUDIT, functioning, social support, stigma and suicide score) and generalized linear mixed-effects models with a log link and Poisson distribution were estimated for the binary outcomes (SAD, GAD, ADHD, PTSD, major depression and suicide risk) (Zou, 2004). Random effects in all models included participant and village. Fixed effects included treatment group (IPT-G or control), time (baseline or follow-up) and an interaction term of group x time. Additional covariates were included in the model if there was a significant baseline difference between treatment groups, or if the covariate was associated with mean change in the outcome from baseline to follow-up. For the linear mixed-effects models, Cohen’s d statistic was calculated as an estimate of effect size by dividing the group x time interaction term by the baseline pooled standard deviation. For the generalized models, relative risk was calculated with associated 95% CIs. All models used p < 0.05 as a statistical significance threshold. All participants were included in the intent-to-treat analysis.
Results
Table 2 displays socio-demographic characteristics of the 142 eligible caregivers. Caregivers were predominantly female (76.8%) with an average age of 43; almost all (>98%) were peasant farmers. Caregivers in the TAU arm reported a significantly (p = 0.04) higher mean number of traumatic events (8.2) compared with caregivers in the IPT-G arm (6.8). Otherwise, there were no significant differences in the caregiver characteristics. Child participants were 52.8% female with an average age of 14 years, with no significant differences between groups.
Table 2.
Baseline characteristics of study sample (n=142 caregiver/child dyads)
| Caregiver characteristic | IPT-G (n=73) | TAU control (n=69) | χ2 or t-test |
|---|---|---|---|
|
|
|
||
| N (%) or mean (SD) | |||
|
|
|
|
|
| Female | 59 (80.8) | 50 (72.5) | 1.39 |
| Age | 43.4 (9.0) | 41.8 (12.3) | −0.85 |
| Marital status | |||
| Single/Separated/Divorced | 24 (32.9) | 18 (26.1) | |
| Married/Monogamous | 33 (45.2) | 31 (44.9) | 1.25 |
| Married/Polygamous | 16 (21.9) | 20 (29.0) | |
| Formal education | 39 (53.4) | 44 (63.8) | 1.56 |
| Employment | |||
| Unemployed | 0 (0.0) | 1 (1.5) | |
| Peasant farmer | 73 (100) | 67 (97.1) | 2.15 |
| Other employment | 0 (0.0) | 1 (1.5) | |
| Religion | |||
| Protestant | 9 (12.3) | 14 (20.3) | |
| Catholic | 57 (78.1) | 50 (72.5) | 1.77 |
| Pentecostal | 7 (9.6) | 5 (7.3) | |
| Number of children | 6.4 (2.2) | 6.6 (2.5) | 0.46 |
| Number of trauma types | 6.8 (3.7) | 8.2 (4.2) | 2.07* |
| Child characteristics | |||
|
| |||
| Female | 38 (52.1) | 37 (53.6) | 0.04 |
| Age | 14.3 (2.5) | 13.6 (2.0) | −1.94 |
| Currently in school | 21 (28.8) | 23 (33.3) | 0.35 |
| Mother alive | 71 (97.3) | 62 (89.9) | 3.28 |
| Father alive | 54 (74.0) | 54 (78.3) | 0.36 |
| Number of adverse events | 6.5 (1.9) | 6.7 (2.1) | 0.71 |
Means, SDs, N’s, and % based on all available data at each time point
p<.05
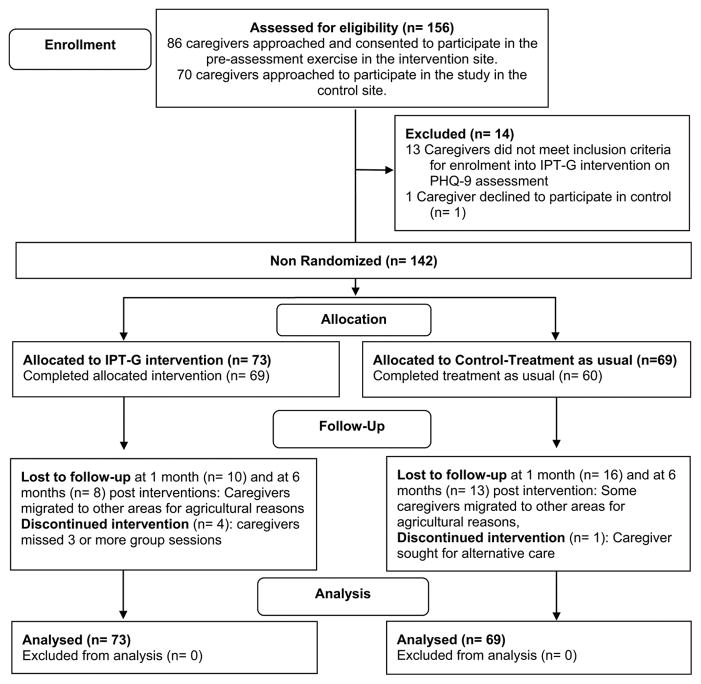
Participant retention is summarized in the CONSORT diagram (Fig. 1). Of the 142 participants enrolled, 116 (81.7%) completed a 1-month post-assessment and 121 (85.2%) completed a 6-month post-assessment.
Fig. 1.
CONSORT 2010 flow diagram.
Table 3 displays caregiver outcome scores by treatment arm. Caregiver participants who received IPT-G had a greater reduction in the risk of depression from baseline to 1 and 6 months (both p < 0.05) post-intervention compared with caregiver participants who received TAU. Among the other caregiver outcomes, IPT-G participants had a significantly greater reduction in psychological distress at 1 month (SRQ; p < 0.01), reported less stigma at 6 months (p = 0.02) and increased social support at 6 months (p < 0.0001) compared with TAU participants. There were no other significant differences in caregiver outcome change between groups.
Table 3.
IPT treatment effects 1 month and 6 months after the end of treatment among adult caregiver participants
| Outcome (continuous) | Control | IPT | Treatment effect | |
|---|---|---|---|---|
|
|
|
|
||
| Mean (SD)a | Cohen’s db | p valued | ||
|
|
|
|
|
|
| SRQ | ||||
| Baseline | 10.2 (5.2) | 10.8 (4.7) | - | - |
| 1 month post-treatment | 8.7 (4.6) | 4.5 (3.5) | 0.80 | <.01 |
| 6 months post-treatment | 5.9 (5.1) | 3.5 (3.4) | 0.46 | .06 |
| Alcohol (AUDIT) | ||||
| Baseline | 1.8 (5.3) | 1.6 (4.0) | - | - |
| 1 month post-treatment | 2.3 (5.5) | 3.0 (6.2) | 0.11 | .60 |
| 6 months post-treatment | 1.3 (3.0) | 2.4 (5.4) | 0.24 | .29 |
| Stigma | ||||
| Baseline | 18.3 (3.1) | 17.8 (3.8) | - | - |
| 1 month post-treatment | 17.6 (3.4) | 16.3 (2.5) | 0.16 | .56 |
| 6 months post-treatment | 19.4 (2.7) | 16.2 (2.3) | 0.65 | .02 |
| Functioning | ||||
| Baseline | 6.6 (2.4) | 7.1 (2.6) | - | - |
| 1 month post-treatment | 7.0 (2.3) | 8.8 (2.0) | 0.44 | .13 |
| 6 months post-treatment | 8.1 (2.3) | 8.8 (1.7) | .03 | .90 |
| Social Support | ||||
| Baseline | 32.6 (7.9) | 33.1 (7.7) | - | - |
| 1 month post-treatment | 34.5 (9.5) | 38.4 (7.2) | 0.36 | .09 |
| 6 months post-treatment | 33.8 (9.2) | 40.4 (6.1) | 0.56 | <.0001 |
| Suicide Score | ||||
| Baseline | 4.1 (11.5) | 3.9 (9.4) | - | - |
| 1 month post-treatment | 2.2 (6.1) | 1.3 (4.8) | 0.07 | .71 |
| 6 months post-treatment | 3.1 (8.7) | 0.8 (5.5) | 0.14 | .32 |
| Outcome (binary) | N (%)a | Risk Ratio (95% CI)c | p valued | |
|
|
|
|
|
|
| Depression | ||||
| Baseline | 30 (43.5) | 39 (53.4) | - | - |
| 1 month post-treatment | 12 (23.5) | 4 (6.4) | 0.25 (0.10, 0.62) | <.01 |
| 6 months post-treatment | 10 (18.5) | 4 (6.3) | 0.33 (0.11, 0.95) | .04 |
| PTSD | ||||
| Baseline | 25 (36.2) | 23 (31.5) | - | - |
| 1 month post-treatment | 28 (52.8) | 25 (40.3) | 0.88 (0.50,1.56) | .65 |
| 6 months post-treatment | 15 (26.8) | 20 (30.8) | 1.17 (0.51, 2.67) | .72 |
| Anxiety | ||||
| Baseline | 30 (43.5) | 31 (42.5) | - | - |
| 1 month post-treatment | 10 (18.9) | 17 (27.4) | 1.37 (0.79, 2.46) | .25 |
| 6 months post-treatment | 10 (17.9) | 6 (9.2) | 0.52 (0.23, 1.16) | .11 |
| Suicide risk | ||||
| Baseline | 8 (11.6) | 12 (16.4) | - | - |
| 1 month post-treatment | 4 (7.6) | 3 (4.8) | 0.42 (0.11, 1.53) | .19 |
| 6 months post-treatment | 6 (10.7) | 2 (3.1) | 0.25 (0.06, 1.04) | .06 |
Means, s.d., N and % based on all available data at each time point.
Cohen’s d effect size was calculated by dividing the group x time interaction term from the linear mixed-effects model by the pooled s.d.
P value is the significance level of the group x time interaction term from the linear (or generalized linear) mixed-effects model indicating statistical significance of the difference in change of outcome score (or risk) between the treatment and control groups from baseline to post-assessment. Separate models were estimated comparing change from baseline to 1 month post-treatment and baseline to 6 months post-treatment. Models included fixed effects of group, time and group x time interaction, and random effects of village and individual participant over time. Demographic characteristics that differed significantly between groups at baseline or predicted change in symptom over time were also included in the models as covariates. All models included all participants at each time point following multiple imputation procedures.
Risk ratios are the exponentiated form of the group x time interaction term from the generalized linear mixed-effects model with Poisson distribution and log link. This coefficient can be interpreted as a ratio of risk ratios. Specifically, it represents the risk ratio comparing risk at follow-up to risk baseline among IPT-G divided by the risk ratio comparing risk at follow-up to risk at baseline among TAU.
Table 4 displays caregiver reported child outcome scores by treatment arm. For the primary outcome of depression, child participants whose caregiver received IPT-G had a significantly greater reduction in depression symptoms at 1 month (p = 0.01) and 6 months (p = 0.03) compared with children whose caregiver received TAU.
Table 4.
IPT treatment effects 1 month and 6 months after the end of treatment among child participants
| Outcome (continuous) | Control | IPT | Between group treatment effect | |
|---|---|---|---|---|
|
|
|
|
||
| Mean (SD)a | Cohen’s db | p value | ||
|
|
|
|
|
|
| Depression (DSRS) | ||||
| Baseline | 15.2 (5.5) | 16.9 (5.6) | - | - |
| 1 month post-treatment | 14.6 (6.7) | 12.9 (4.8) | 0.57 | .01 |
| 6 months post-treatment | 13.5 (7.0) | 12.2 (6.5) | 0.46 | .03 |
| Strengths & Difficulties | ||||
| Baseline | 15.4 (6.9) | 15.6 (5.8) | - | - |
| 1 month post-treatment | 15.6 (7.4) | 13.8 (7.4) | 0.25 | .31 |
| 6 months post-treatment | 12.0 (5.5) | 11.1 (5.4) | 0.07 | .74 |
| Attachment | ||||
| Baseline | 34.2 (8.2) | 33.3 (6.0) | - | - |
| 1 month post-treatment | 34.0 (10.7) | 37.4 (8.0) | 0.55 | .05 |
| 6 months post-treatment | 36.2 (7.3) | 37.0 (6.7) | 0.22 | .47 |
| CRIES | ||||
| Baseline | 7.3 (11.2) | 8.6 (11.2) | - | - |
| 1 month post-treatment | 3.4 (7.5) | 3.1 (8.5) | 0.18 | .25 |
| 6 months post-treatment | 2.5 (6.5) | 2.4 (7.6) | 0.11 | .53 |
| Outcome (binary) | N (%)a | Difference in risk ratios (95% CI)c | p value | |
|
|
|
|
|
|
| SAD | ||||
| Baseline | 21 (30.4) | 18 (24.7) | - | - |
| 1 month post-treatment | 6 (11.3) | 8 (12.7) | 1.4 (0.35, 5.67) | .63 |
| 6 months post-treatment | 1 (1.8) | 5 (7.7) | 5.64 (0.92, 34.4) | .06 |
| GAD | ||||
| Baseline | 23 (33.3) | 15 (20.6) | - | - |
| 1 month post-treatment | 15 (28.3) | 19 (30.2) | 1.17 (0.74, 4.15) | .48 |
| 6 months post-treatment | 7 (12.5) | 4 (6.2) | 0.85 (0.31, 2.37) | .76 |
| ADHD | ||||
| Baseline | 13 (18.8) | 17 (23.3) | - | - |
| 1 month post-treatment | 10 (18.9) | 0 (0.0) | 0.09 (0.01, 0.76) | .03 |
| 6 months post-treatment | 2 (3.6) | 2 (3.1) | 0.76 (0.11, 5.10) | .78 |
Means, s.d., N and % based on all available data at each time point.
Cohen’s d effect size was calculated by dividing the group x time interaction term from the linear mixed-effects model by the pooled s.d.
P value is the significance level of the group x time interaction term from the linear (or generalized linear) mixed-effects model indicating statistical significance of the difference in change of outcome score (or risk) between the treatment and control groups from baseline to post-assessment. Separate models were estimated comparing change from baseline to 1 month post-treatment and baseline to 6 months post-treatment. Models included fixed effects of group, time and group x time interaction, and random effects of village and individual participant over time. Demographic characteristics that differed significantly between groups at baseline or predicted change in symptom over time were also included in the models as covariates. All models included all participants at each time point following multiple imputation procedures.
Risk ratios are the exponentiated form of the group x time interaction term from the generalized linear mixed-effects model with Poisson distribution and log link. This coefficient can be interpreted as a ratio of risk ratios. Specifically, it represents the risk ratio comparing risk at follow-up to risk at baseline among IPT-G divided by the risk ratio comparing risk at follow-up to risk at baseline among TAU.
Discussion
For caregivers of children affected by NS, IPT-G delivered by LCHWs working in the government health system, resulted in significant reductions in the risk of depression, psychological distress and stigma, and significant improvement in social support among caregivers compared with those who received TAU. Notably, there was a significant improvement in their children’s mental health, indicated by reduction in depression symptoms, compared with the TAU group.
IPT-G targets depression specifically, and in our study, caregivers who received IPT-G had an 88% reduction in risk for MDD from baseline to the 1-month post-intervention assessment compared with a 46% reduction in risk among TAU caregivers. Treatment effects appeared to be sustained over time: at the 6-month follow-up, IPT-G participants’ depression risk remained reduced by 88% from baseline compared with a 57% reduction in risk among controls. These findings are in line with previous studies of IPT-G in South Africa (Petersen et al. 2012, 2014). Our study compares favourably with other group PTs in similar settings. In their study among HIV-positive adults in northern Uganda, Nakimuli-Mpungu et al. (2015) found no difference in mean depression scores between group support psychotherapy (GSP) and group HIV education (GHE) immediately after intervention, though participants in the GSP group had significantly lower mean depression scores than those in the GHE group 6 months after intervention (Nakimuli-Mpungu et al. 2015).
Caregivers who received IPT-G had significantly higher levels of social support at 1 and 6 months post-intervention. Parent-to-parent programmes, as was the case with IPT-G for NS, provide emotional, informational and instrumental support (Tracy & Whittaker, 1987). Consistent with the literature, group psychological interventions result in improved social support among participants and have many potential benefits, including the instillation of hope, acceptance, belonging and altruism (Hogan et al. 2002; Petersen et al. 2012; Nakimuli-Mpungu et al. 2015). Peer support and self-help groups allow members to provide and receive support, and rebuild lasting social networks after a crisis (Tracy & Whittaker, 1987). Interventions that emphasize reciprocal support (e.g. both giving and receiving support) show more encouraging results than those where one only receives support, and more so for diseases considered stigmatizing (Hogan et al. 2002). There appears to be a positive relationship between social support and family outcomes including parenting behaviours, parenting attitudes, parent–child interactions and child development (Tracy & Whittaker, 1987).
The significant reduction in perceived stigma levels at 6 months among caregivers who received IPT-G could also be explained by improved social support. As an adaptation to perceived stigmatization, caregivers may withdraw from potential support networks which in turn negatively affects their mental health and coping effectiveness (Perlick et al. 2007). IPT-G has been noted to contribute to improved personal agency, resilience and coping (Petersen et al. 2012) which could result in decreased levels of perceived stigma and psychological distress.
This study also suggests that PTs delivered to caregivers improve psychological outcomes for their children. Mean depression scores were significantly lower at both time points in children whose caregivers received IPT-G. These findings are consistent with previous research, which showed that reductions in maternal depression mediated improvements in child externalizing and internalizing problem behaviour (Shaw et al. 2009).
There were no significant effects of IPT-G on PTSD, GAD, suicide risk, alcohol use and level of functioning among the caregivers. IPT-G is designed specifically to address depressive symptomatology and may require further adaptation than what was conducted in this study to have an effect on PTSD (Campanini et al. 2010) or anxiety disorders. Though the scores were higher in the treatment group at 1 and 6 months post-intervention, there were no significant differences in the level of functioning in the caregivers. This is similar to Nakimuli-Mpungu et al.’s finding for a group support (GSP) intervention using a similar measure and conducted in a similar context (Nakimuli-Mpungu et al. 2013, 2015). The measure of functioning is based on the performance of activities of daily living and social obligations which have to be met, and hence levels of functioning may not be affected by levels of distress, especially for caregivers who have dependent sick children (Nakimuli-Mpungu, 2012). In our study, there were low rates of alcohol use disorder among caregivers compared with previous findings in similar populations (Roberts et al. 2011). Cognizant of the limitations of using interviewer-administered assessments of alcohol use, our results could also be explained by the demands and obligations for families affected by NS (Nakigudde et al. 2016). Given the trends in some of the caregiver outcomes, our study could also have been underpowered to detect effects on a number of measures.
This effectiveness study is a model for how PTs can be adapted for government health systems in low-resource settings. It is within the recommendations of Thornicroft et al. (2016) who call for community mental health care with service provision by staff in primary care and community settings (Thornicroft et al. 2010, 2016). Our findings suggest that community-based interventions for promoting child and adolescent mental health should incorporate strategies to promote caregiver mental health. This study demonstrates that an evidence-based psychotherapy intervention can be delivered effectively and with fidelity by lay counsellors and, critically, that the effects of the intervention on the primary depression outcome were sustained over a 6-month period following the end of the treatment. Lewandowski & others (2016) provide more evidence of sustained effects of IPT-G: positive changes in quality of life and a range of non-mental health outcomes were attributed to the treatment 10 years after the intervention (Lewandowski et al. 2016).
In comparison to a similar intervention (Petersen et al. 2014), the low rate of attrition in our study provides evidence of IPT-G as a feasible and effective PT for moderate-to-severe depression when delivered by trained LCHWs within a task-shifting approach in low-resource settings. Though there are concerns about fidelity and other barriers to effective IPT-G delivery (Lewandowski et al. 2016), integration within government health system structures may provide the right platform for sustainable service provision.
Limitations
The trial was non-randomized, thus introducing the potential for bias. Our results indicate that the treatment groups were comparable with respect to baseline values for demographic characteristics and mental health outcomes. That said, lack of randomization increases the likelihood that an unmeasured covariate within the treatment blocks influenced the group differences in outcomes. Because of the context of government roll out of services for NS, randomization was not possible at the time of our study. Quasi-experimental designs allow the flexibility required to test interventions within community service settings for conditions like NS, which have ethical and socio-political considerations precluding randomization (Stadnick et al. 2015).
Although we used some locally developed measures, most of our outcome measures for adults and children have not been validated for the local population. In addition, some of the child assessments were based on caregiver reports and this could have influenced the outcome measures. Parents’ perceptions of their child’s behaviours and their own functioning may have been influenced by a number of factors such as parenting stress and their expectations of and experiences with services they have received (Stadnick et al. 2015). Our study lacks additional informants on children’s behaviour and psychological well-being. We are therefore unable to parse changes in caregiver’s perception of their children’s well-being v. changes in child outcomes that could be independently verified by another family or community members. Because many children with NS were not attending school, it was not possible to obtain teacher reports of psychological well-being pre- and post-intervention. We were also not able to enrol more than one child per family to assess the impact on other child family members due to financial and logistical barriers. This should be addressed in future studies. Finally, although the study was adequately powered to observe significant changes in the depression primary outcome, the sample size may have limited our ability to observe statistically significant changes in the secondary outcomes.
In conclusion, this study represents the first application of a PT addressing mental health problems associated with NS, a neuropsychiatric condition with high morbidity and mortality in northern Uganda and South Sudan. Our implementation of IPT-G for NS demonstrates how a PT initially delivered through a highly structured, supervised and well-funded NGO can also be effective when adapted for use in the real-world conditions of low-resourced government health systems. In comparison to TAU, it resulted in significant reduction in the number of adults and children with depression and other mental health outcomes, demonstrating the ‘dual’ benefits of this intervention. Although results from this study informed the WHO mhGAP pilot in Uganda, a larger randomized study is required to generate further evidence of effectiveness, utility for uptake and scale up of PTs within the public health system.
Acknowledgments
The authors are very grateful to the caregivers and their children who participated in the study. The authors also wish to thank their dedicated and passionate team of research assistants, IPT-G experts and village health team members. The authors thank Anvita Bhardwaj for assistance in manuscript preparation.
This project was funded by Grand Challenges Canada (Grant #S4_0232_01, BBM, Principal Investigator). Co-authors were supported by the US National Institutes of Health: T32DA007292 (JCK) and K01MH104310 (BAK). The content is solely the responsibility of the authors and does not represent the official views of the funding agency. The funding agencies had no role in the study design; collection, analysis and interpretation of data; writing of the report; and the decision to submit the paper for publication.
Footnotes
Declaration of interest
The authors declare no conflicts of interest.
Ethical standards
‘The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.’
Contributor Information
Byamah B. Mutamba, Butabika National Mental Hospital, Kampala, Uganda., Amsterdam Institute of Social Science Research, Faculty of Social and Behavioural Sciences, University of Amsterdam.
Jeremy C. Kane, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health
Joop de Jong, Amsterdam Institute of Social Science Research, Faculty of Social and Behavioural Sciences, University of Amsterdam.
James Okello, Department of Psychiatry, Gulu University, Uganda.
Seggane Musisi, Department of Psychiatry, College of Health Sciences, Makerere University, Kampala, Uganda.
Brandon A. Kohrt, Department of Psychiatry, George Washington University
References
- Abbo C, Ekblad S, Waako P, Okello E, Musisi S. The prevalence and severity of mental illnesses handled by traditional healers in two districts in Uganda. African Health Sciences. 2009;9(Suppl 1):S16–S22. [PMC free article] [PubMed] [Google Scholar]
- Aganyira R. Stigma and Associated Factors in Caregivers of Patients Diagnosed with Schizophrenia Attending Butabika National Referral Mental Hospital in Nakawa Division, Kampala District. Kampala, Uganda: Diploma in Clinical Psychiatry, Butabika School of Psychiatric Clinical Officers; 2013. [Google Scholar]
- Ayikoru T. Perceived Stigma and Associated Factors in Caregivers of Patients Diagnosed with Epilepsy Attending the out-Patients Mental Health Clinic at Entebbe District Hospital in Uganda. Butabika, Kampala, Uganda: Diploma in Clinical Psychiatry, School of Psychiatric Clinical Officers; 2015. [Google Scholar]
- Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? International Journal of Methods in Psychiatric Research. 2011;20:40–49. doi: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazos DA, Lafave LRA, Suresh G, Shannon KC, Nuwaha F, Splaine ME. The gas cylinder, the motorcycle and the village health team member: a proof-of-concept study for the use of the Microsystems Quality Improvement Approach to strengthen the routine immunization system in Uganda. Implementation Science. 2015;10:1. doi: 10.1186/s13012-015-0215-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardselee WR, Versage EM, Giadstone TR. Children of affectively ill parents: a review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Betancourt TS. Attending to the mental health of war-affected children: the need for longitudinal and developmental research perspectives. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:323–325. doi: 10.1016/j.jaac.2011.01.008. [DOI] [PubMed] [Google Scholar]
- Betancourt TS, Yudron M, Wheaton W, Smith-Fawzi MC. Caregiver and adolescent mental health in Ethiopian Kunama refugees participating in an emergency education program. Journal of Adolescent Health. 2012;51:357–365. doi: 10.1016/j.jadohealth.2012.01.001. [DOI] [PubMed] [Google Scholar]
- Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale: a research report. Journal of Child Psychology and Psychiatry. 1981;22:73–88. doi: 10.1111/j.1469-7610.1981.tb00533.x. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass J, Betancourt T, Speelman L, Onyango G, Clougherty KF, et al. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. Journal of the American Medical Association. 2007;298:519–527. doi: 10.1001/jama.298.5.519. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, et al. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. Journal of the American Medical Association. 2003;289:3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- Bruffaerts R, Demyttenaere K, Borges G, Haro JM, Chiu WT, Hwang I, et al. Childhood adversities as risk factors for onset and persistence of suicidal behaviour. British Journal of Psychiatry. 2010;197:20–27. doi: 10.1192/bjp.bp.109.074716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmann K. ‘You sit in fear’: understanding perceptions of nodding syndrome in post-conflict northern Uganda. Global Health Action. 2014;7:25069. doi: 10.3402/gha.v7.25069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campanini RF, Schoedl AF, Pupo MC, Costa ACH, Krupnick JL, Mello MF. Efficacy of interpersonal therapy-group format adapted to post-traumatic stress disorder: an open-label add-on trial. Depression and Anxiety. 2010;27:72–77. doi: 10.1002/da.20610. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Donker T, Weissman MM, Ravitz P, Cristea IA. Interpersonal psychotherapy for mental health problems: a comprehensive meta-analysis. American Journal of Psychiatry. 2016;173:680–687. doi: 10.1176/appi.ajp.2015.15091141. [DOI] [PubMed] [Google Scholar]
- Elbedour S, Ten Bensel R, Bastien DT. Ecological integrated model of children of war: individual and social psychology. Child Abuse & Neglect. 1993;17:805–819. doi: 10.1016/s0145-2134(08)80011-7. [DOI] [PubMed] [Google Scholar]
- Ford T. Introduction to epidemiological study designs. In: Martin Prince RS, Ford T, Hotopf M, editors. Practical Psychiatric Epidemiology. Great Britain: Oxford University Press; 2003. pp. 85–96. [Google Scholar]
- Fulton BD, Scheffler RM, Sparkes SP, Auh EY, Vujicic M, Soucat A. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Human Resources for Health. 2011;9:1. doi: 10.1186/1478-4491-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. The British Journal of Psychiatry. 2000;177:534–539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- Gullone E, Robinson K. The inventory of parent and peer attachment – revised (IPPA-R) for children: a psychometric investigation. Clinical Psychology & Psychotherapy. 2005;12:67–79. [Google Scholar]
- Hogan BE, Linden W, Najarian B. Social support interventions: do they work? Clinical Psychology Review. 2002;22:381–440. doi: 10.1016/s0272-7358(01)00102-7. [DOI] [PubMed] [Google Scholar]
- Idro R, Musubire KA, Byamah MB, Namusoke H, Muron J, Abbo C, et al. Proposed guidelines for the management of nodding syndrome. African Health Sciences. 2013;13:219–225. doi: 10.4314/ahs.v13i2.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idro R, Opar B, Wamala J, Abbo C, Onzivua S, Mwaka DA, et al. Is nodding syndrome an Onchocerca volvulus-induced neuroinflammatory disorder? Uganda’s story of research in understanding the disease. International Journal of Infectious Diseases. 2016;45:112–117. doi: 10.1016/j.ijid.2016.03.002. [DOI] [PubMed] [Google Scholar]
- Johnson TP, Tyagi R, Lee PR, Lee M-H, Johnson KR, Kowalak J, et al. Nodding syndrome may be an autoimmune reaction to the parasitic worm Onchocerca volvulus. Science Translational Medicine. 2017;9:eaaf6953. doi: 10.1126/scitranslmed.aaf6953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kigozi F, Ssebunnya J, Kizza D, Cooper S, Ndyanabangi S. An overview of Uganda’s mental health care system: results from an assessment using the world health organization’s assessment instrument for mental health systems (WHO-AIMS) International Journal of Mental Health Systems. 2010;4:1. doi: 10.1186/1752-4458-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilbourne AM, Neumann MS, Pincus HA, Bauer MS, Stall R. Implementing evidence-based interventions in health care: application of the replicating effective programs framework. Implementation Science. 2007;2:1. doi: 10.1186/1748-5908-2-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinyanda E, Hoskins S, Nakku J, Nawaz S, Patel V. Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district, Uganda. BMC Psychiatry. 2011;11:1. doi: 10.1186/1471-244X-11-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinyanda E, Kizza R, Abbo C, Ndyanabangi S, Levin J. Prevalence and risk factors of depression in childhood and adolescence as seen in 4 districts of north-eastern Uganda. BMC International Health and Human Rights. 2013;13:1. doi: 10.1186/1472-698X-13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klerman G, Weissman M, Rounsaville B, Chevron E. Interpersonal Psychotherapy of Depression. SC: BasicBooks; 1984. [Google Scholar]
- Kohrt BA, Jordans MJ, Tol WA, Luitel NP, Maharjan SM, Upadhaya N. Validation of cross-cultural child mental health and psychosocial research instruments: adapting the Depression Self-Rating Scale and Child PTSD Symptom Scale in Nepal. BMC Psychiatry. 2011;11:1. doi: 10.1186/1471-244X-11-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowski R, Bolton P, Feighery A, Bass J, Hamba C, Haroz E, et al. Local perceptions of the impact of group interpersonal psychotherapy in rural Uganda. Global Mental Health. 2016;3:e23. doi: 10.1017/gmh.2016.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J, Belfer M, Daniels A, Flisher A, Villé L, Lora A, et al. Treated prevalence of and mental health services received by children and adolescents in 42 low-and-middle-income countries. Journal of Child Psychology and Psychiatry. 2011;52:1239–1246. doi: 10.1111/j.1469-7610.2011.02409.x. [DOI] [PubMed] [Google Scholar]
- Mugisha J, Muyinda H, Malamba S, Kinyanda E. Major depressive disorder seven years after the conflict in northern Uganda: burden, risk factors and impact on outcomes (The Wayo-Nero Study) BMC Psychiatry. 2015a;15:48. doi: 10.1186/s12888-015-0423-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugisha J, Muyinda H, Malamba S, Kinyanda E. Major depressive disorder seven years after the conflict in northern Uganda: burden, risk factors and impact on outcomes (The Wayo-Nero Study) BMC Psychiatry. 2015b;15:1. doi: 10.1186/s12888-015-0423-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugisha J, Muyinda H, Wandiembe P, Kinyanda E. Prevalence and factors associated with posttraumatic stress disorder seven years after the conflict in three districts in northern Uganda (The Wayo-Nero Study) BMC Psychiatry. 2015c;15:1. doi: 10.1186/s12888-015-0551-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugisha J, Muyinda H, Wandiembe P, Kinyanda E. Prevalence and factors associated with posttraumatic stress disorder seven years after the conflict in three districts in northern Uganda (The Wayo-Nero Study) BMC Psychiatry. 2015d;15:170. doi: 10.1186/s12888-015-0551-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutamba B, Abbo C, Muron J, Idro R, Mwaka A. Stereotypes on nodding syndrome: responses of health workers in the affected region of northern Uganda. African Health Sciences. 2014;13:986–991. doi: 10.4314/ahs.v13i4.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwaka AD, Okello ES, Abbo C, Odwong FO, Olango W, Etolu JW, et al. Is the glass half full or half empty? A qualitative exploration on treatment practices and perceived barriers to biomedical care for patients with nodding syndrome in post-conflict northern Uganda. BMC Research Notes. 2015;8:386. doi: 10.1186/s13104-015-1323-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakigudde J, Musisi S, Ehnvall A, Airaksinen E, Agren H. Adaptation of the multidimensional scale of perceived social support in a Ugandan setting. African Health Sciences. 2009;9(Suppl 1):S35–S41. [PMC free article] [PubMed] [Google Scholar]
- Nakigudde J, Mutamba BB, Bazeyo W, Musisi S, James O. An exploration of caregiver burden for children with nodding syndrome (lucluc) in northern Uganda. BMC Psychiatry. 2016;16:255. doi: 10.1186/s12888-016-0955-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakigudde J, Tugumisirize J, Musisi S. Validation of the SRQ-20 in primary care in Uganda. Proceedings of the First Annual Makerere University Faculty of Medicine Scientific Conference.2005. [Google Scholar]
- Nakimuli-Mpungu E. Development of a local function assessment tool: a field-based example from the Peter C Alderman Foundation Psycho-Trauma Clinics in northern Uganda. Proceedings from the 5th PCAF Pan African Psycho trauma Conference; 2012. pp. 16–20. [Google Scholar]
- Nakimuli-Mpungu E, Okello J, Kinyanda E, Alderman S, Nakku J, Alderman JS, et al. The impact of group counseling on depression, post-traumatic stress and function outcomes: a prospective comparison study in the Peter C. Alderman trauma clinics in northern Uganda. Journal of Affective Disorders. 2013;151:78–84. doi: 10.1016/j.jad.2013.05.055. [DOI] [PubMed] [Google Scholar]
- Nakimuli-Mpungu E, Wamala K, Okello J, Alderman S, Odokonyero R, Mojtabai R, et al. Group support psychotherapy for depression treatment in people with HIV/AIDS in northern Uganda: a single-centre randomised controlled trial. The Lancet HIV. 2015;2:e190–e199. doi: 10.1016/S2352-3018(15)00041-7. [DOI] [PubMed] [Google Scholar]
- Okello J, Nakimuli-Mpungu E, Musisi S, Broekaert E, Derluyn I. War-related trauma exposure and multiple risk behaviors among school-going adolescents in northern Uganda: the mediating role of depression symptoms. Journal of Affective Disorders. 2013;151:715–721. doi: 10.1016/j.jad.2013.07.030. [DOI] [PubMed] [Google Scholar]
- Okello J, Nakimuli-Mpungu E, Musisi S, Broekaert E, Derluyn I. The association between attachment and mental health symptoms among school-going adolescents in northern Uganda: the moderating role of war-related trauma. PLoS ONE. 2014;9:e88494. doi: 10.1371/journal.pone.0088494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okello J, Onen T, Misisi S. Psychiatric disorders among war-abducted and non-abducted adolescents in Gulu district, Uganda: a comparative study. African Journal of Psychiatry. 2007;10:225–231. doi: 10.4314/ajpsy.v10i4.30260. [DOI] [PubMed] [Google Scholar]
- Okewole A, Dada M, Ogun O, Bello-Mojeed M, Usoh T. Prevalence and correlates of psychiatric morbidity among caregivers of children and adolescents with neuropsychiatric disorders in Nigria. African Journal of Psychiatry. 2011;14:306–309. doi: 10.4314/ajpsy.v14i4.8. [DOI] [PubMed] [Google Scholar]
- Ovuga E, Boardman J, Wasserman D. The prevalence of depression in two districts of Uganda. Social Psychiatry and Psychiatric Epidemiology. 2005;40:439–445. doi: 10.1007/s00127-005-0915-0. [DOI] [PubMed] [Google Scholar]
- Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities. The Lancet. 2016;387:1672–1685. doi: 10.1016/S0140-6736(15)00390-6. [DOI] [PubMed] [Google Scholar]
- Perlick DA, Miklowitz DJ, Link BG, Struening E, Kaczynski R, Gonzalez J, et al. Perceived stigma and depression among caregivers of patients with bipolar disorder. The British Journal of Psychiatry. 2007;190:535–536. doi: 10.1192/bjp.bp.105.020826. [DOI] [PubMed] [Google Scholar]
- Perrin S, Meiser-Stedman R, Smith P. The Children’s Revised Impact of Event Scale (CRIES): validity as a screening instrument for PTSD. Behavioural and Cognitive Psychotherapy. 2005;33:487. [Google Scholar]
- Petersen I, Bhana A, Baillie K Consortium MRP. The feasibility of adapted group-based interpersonal therapy (IPT) for the treatment of depression by community health workers within the context of task shifting in South Africa. Community Mental Health Journal. 2012;48:336–341. doi: 10.1007/s10597-011-9429-2. [DOI] [PubMed] [Google Scholar]
- Petersen I, Hancock JH, Bhana A, Govender K. A group-based counselling intervention for depression comorbid with HIV/AIDS using a task shifting approach in South Africa: a randomized controlled pilot study. Journal of Affective Disorders. 2014;158:78–84. doi: 10.1016/j.jad.2014.02.013. [DOI] [PubMed] [Google Scholar]
- Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. The Lancet. 2008;372:902–909. doi: 10.1016/S0140-6736(08)61400-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiatry. 2008;8:38. doi: 10.1186/1471-244X-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E. Alcohol disorder amongst forcibly displaced persons in northern Uganda. Addictive Behaviors. 2011;36:870–873. doi: 10.1016/j.addbeh.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology. 2009;21:417–439. doi: 10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, et al. Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID) The Journal of Clinical Psychiatry. 2010;71:313–326. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- Singla DR, Kohrt BA, Murray LK, Anand A, Chorpita BF, Patel V. Psychological treatments for the world: lessons from low- and middle-income countries. Annual Review of Clinical Psychology. 2017 Apr;13:5.1–5.33. doi: 10.1146/annurev-clinpsy-032816-045217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadnick NA, Stahmer A, Brookman-Frazee L. Preliminary effectiveness of Project ImPACT: a parent-mediated intervention for children with autism spectrum disorder delivered in a community program. Journal of Autism and Developmental Disorders. 2015;45:2092–2104. doi: 10.1007/s10803-015-2376-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Struening EL, Perlick DA, Link BG, Hellman F, Herman D, Sirey JA. Stigma as a barrier to recovery: the extent to which caregivers believe most people devalue consumers and their families. Psychiatric Services. 2001;52(12):1633–1638. doi: 10.1176/appi.ps.52.12.1633. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Alem A, Santos RA, Barley E, Drake RE, Gregorio G, et al. WPA guidance on steps, obstacles and mistakes to avoid in the implementation of community mental health care. World Psychiatry. 2010;9:67–77. doi: 10.1002/j.2051-5545.2010.tb00276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, et al. Undertreatment of people with major depressive disorder in 21 countries. The British Journal of Psychiatry. 2017;210(2):119–124. doi: 10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G, Deb T, Henderson C. Community mental health care worldwide: current status and further developments. World Psychiatry. 2016;15:276–286. doi: 10.1002/wps.20349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy EM, Whittaker JK. The evidence base for social support interventions in child and family practice: emerging issues for research and practice. Children and Youth Services Review. 1987;9:249–270. [Google Scholar]
- Verdeli H, Clougherty K, Bolton P, Speelman L, Lincoln N, Bass J, et al. Adapting group interpersonal psychotherapy for a developing country: experience in rural Uganda. World Psychiatry. 2003;2(2):114–120. [PMC free article] [PubMed] [Google Scholar]
- Verdeli H, Clougherty K, Onyango G, Lewandowski E, Speelman L, Betancourt TS, et al. Group Interpersonal Psychotherapy for depressed youth in IDP camps in Northern Uganda: adaptation and training. Child and Adolescent Psychiatric Clinics of North America. 2008;17(3):605–624. doi: 10.1016/j.chc.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Wainberg ML, Scorza P, Shultz JM, Helpman L, Mootz JJ, Johnson KA, et al. Challenges and opportunities in Global Mental Health: a research-to-practice perspective. Current Psychiatry Reports. 2017;19:28. doi: 10.1007/s11920-017-0780-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Markowitz JC, Klerman GL. Comprehensive Guide to Interpersonal Psychotherapy. New York: Basic Books; 2000. [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- World Health Organization. mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings – Version 2.0. Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52:30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- Zou G. A modified Poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]