Abstract
The purpose of the study is to describe changes in mental health among women following an oil spill and to examine its association with the Deepwater Horizon Oil Spill (DHOS).
The WaTCH Study followed 2038 women in Louisiana after the DHOS. Subjects were interviewed in 2012–2014 and 2014–2016. Oil spill exposure was characterized using survey items about economic and physical exposures. Outcomes were depressive symptoms and mental distress.
After adjustment for relevant demographics, depressive symptoms increased over two time points following the DHOS, while symptoms of mental distress decreased. For every year increase in time since the DHOS, the rate ratio for depressive symptoms increased by a factor of 1.08. In contrast, the rate ratio for mental distress decreased by a factor of 0.97. In addition, initial associations between economic and physical exposure to the DHOS persisted up to 6 years after the spill; women who were more highly exposed experienced higher levels of depressive symptoms (rate ratios ranged from 1.08 to 1.11) and mental distress (rate ratios from 1.05 to 1.11) at each time point than women who were less exposed.
A better understanding of recovery patterns following an oil spill can help direct critical mental health response efforts.
Keywords: oil spill, disaster, longitudinal, mental health, women
Introduction
It is now well-established that disasters of all kinds severely impact mental health,[1, 2] and oil spills are no exception. There is ample evidence that higher levels of exposure to an oil spill, whether in the form of geographic proximity to the spill, vulnerable occupations (e.g., fishers, clean-up workers), or various means of indirect exposure (e.g., through job loss or property damage), are significantly associated with worse mental health outcomes. These results have been borne out in earlier studies such as the Exxon Valdez oil spill in 1989,[3–9] the Sea Empress spill in 1996,[10] the Prestige oil spill in 2002,[11, 12] and the Hebei Spirit spill in 2007.[13–16] Depression, anxiety, and PTSD appear to be the predominant manifestations of mental health impact.
The Deepwater Horizon Oil Spill (DHOS) resulted from an explosion on the British Petroleum-operated drilling rig 49 miles off the Louisiana coast on 20 April 2010, killing 11 people and causing almost 5 million barrels of oil to flow into the Gulf of Mexico. Covering over 68,000 square miles of land and sea, the DHOS is the largest marine oil spill in the history of the petroleum industry. In addition to causing widespread environmental and economic damage, the DHOS has also been linked to numerous harmful mental health effects.[17–25] For example, a survey of over 38,000 residents of Alabama, Florida, Louisiana, and Mississippi, conducted in the first year after the DHOS, assessed frequent mental distress and current depression.[20] This study observed that direct contact with the oil was positively associated with both mental health outcomes, while job and income loss were related just to current depression.[20]
Risk factors for poor mental health outcomes following disasters have been classified into categories of peri-disaster, pre-disaster, and post-disaster risk factors.[2] The main peri-disaster risk factor is degree of exposure to the event, as discussed above. However, pre-disaster risk factors for mental health also include individual characteristics such as female gender, younger age (e.g., children), middle age, low socioeconomic status, minority ethnic status, having children, having prior mental health problems, and having experienced traumatic or stressful events prior to the disaster.[2] Key predictors of the development and trajectories of disaster-related mental illness include post-disaster life stressors (such as job loss, property damage, and marital stress) and low levels of social support.[2] Both of these post-disaster risk factors can increase vulnerability to mental health conditions such as depression and PTSD.[2] Given this collection of risk factors, women are particularly susceptible to adverse mental health effects following a disaster, especially when they are caregivers or are of lower socioeconomic status.
An early review of longitudinal data in the disaster literature suggests that disaster survivors’ mental health generally improves as time passes, with the first year being the time of peak symptoms or effects.[26] However, none of the disasters considered in the review were oil spills. A subsequent review of only oil spills[27] highlighted a single longitudinal study[28] on psychological health effects, which found that psychological stress diminished after the first year following the Exxon Valdez. An update to that review reported no new longitudinal studies of oil spills.[29] A closer examination of Exxon Valdez oil spill studies, however, suggests that while residents in lesser exposed communities exhibited decreasing levels of stress over time, residents of more highly impacted communities of commercial fishers continued to exhibit signs of stress and disruption for 18 months subsequent to the spill,[4, 5] and signs of depression, anxiety, and posttraumatic stress disorder up to six years after the oil spill.[8] With respect to the Deepwater Horizon Oil Spill, less is known. An examination of BRFSS respondents in affected coastal communities in Mississippi and Alabama in 2011, one year after the oil spill, reported a smaller proportion of individuals with depressive symptoms compared to 2010, four months after the DHOS, though symptoms were still higher in these individuals compared to the rest of the population.[30] Another study of two coastal counties in Alabama and Florida observed no significant declines in anxiety and depression a year after the DHOS.[31] Notably, none of these studies used a general community-dwelling population in a truly longitudinal study design.
The objective of this study is to address the paucity of longitudinal data on the mental health effects of oil spill disasters by 1) describing the changes in depressive symptoms and mental distress among women living in coastal Louisiana following the DHOS over two time periods; and 2) examining the relationship between DHOS exposure and depressive symptoms, and DHOS exposure and mental distress over time.
Methods
Study Design and Population
The Women and Their Children’s Health (WaTCH) Study is a prospective cohort designed to assess the longitudinal health effects of the Deepwater Horizon oil spill (DHOS) on women in seven coastal Louisiana parishes. Women were selected as the population of interest because they represent an influential yet vulnerable and understudied population. They are often central to decision-making processes within households, particularly with respect to decisions regarding health, support, diet, and caregiving. Details of the study have been presented elsewhere (see Peters et al[32]). Briefly, women were randomly recruited through an address-based sampling frame and were eligible to participate if they were between 18 and 80 years old and lived in the study area at the time of the oil spill. A first round of telephone interviews was conducted between July 2012 and August 2014; follow-up data were collected by telephone between September 2014 and June 2016. 2852 women participated in the original survey, representing a Wave 1 response rate of 45%. 2038 of these women completed the follow-up survey at Wave 2, resulting in a retention rate of 72%.
The WaTCH Study was reviewed and approved by the Louisiana State University Health Sciences Center Institutional Review Board. Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at the Epidemiology Data Center at the LSUHSC School of Public Health.[33] REDCap is a secure, web-based application designed to support data capture for research studies, providing a) an intuitive interface for validated data entry; b) audit trails for tracking data manipulation and export procedures; c) automated export procedures for seamless data downloads to common statistical packages; and d) procedures for importing data from external sources.
Measures
Exposures
Exposure to the oil spill was estimated at Wave 1, as done in our previous analyses,[23, 32, 34] using nine self-reported items grouped into two factors that were identified through exploratory factor analysis. The first factor, consisting of items related to income loss, how hard participants perceived they were hit compared to others, and the oil spill’s influence on household finances, was labeled “economic exposure.” The second factor, consisting of the other six items, was labeled “physical exposure.” Within each factor, affirmative responses were summed to give total exposure scores. Table 1 shows the frequencies of individual items and total exposure scores. Time since oil spill, the other exposure of interest, was calculated as the number of years between each interview date and the date of the Deepwater Horizon oil spill (April 20, 2010).
Table 1.
Sociodemographic and Deepwater Horizon Oil Spill Exposure Characteristics at Wave 1, WaTCH Sample, N=2038, Louisiana, 2012–2016.
| Characteristic | n | % |
|---|---|---|
| Race/ethnicity | ||
| Non-Hispanic White | 1123 | 55.13 |
| Non-Hispanic African American | 732 | 35.94 |
| Hispanic/multi/other | 182 | 8.93 |
| Education | ||
| Less than high school | 232 | 11.39 |
| High school graduate | 1189 | 58.37 |
| College or higher | 616 | 30.24 |
| Pre-DHOS household income | ||
| <= $20K/year | 472 | 24.72 |
| $20K–$50K/year | 581 | 30.43 |
| $50–$80K/year | 399 | 20.90 |
| >=$80K/year | 457 | 23.94 |
| Age at time of oil spill (mean, SD) | 43.5 | 12.36 |
| Economic Exposure | ||
| Lost HH income as a result of employment disruption/closing of business due to oil spill | 521 | 25.69 |
| Hit harder by oil spill than others in community | 127 | 6.34 |
| Oil spill had somewhat or very negative influence on HH financial situation | 752 | 37.36 |
| Physical Exposure | ||
| Oil spill caused damage to areas fished commercially | 141 | 6.92 |
| Could smell the oil | 758 | 38.75 |
| Came into physical contact with oil in other ways (e.g., during home, recreation, hunting, fishing, or other activities | 437 | 21.6 |
| Oil spill directly affected recreational hunting/fishing/other activities of household | 706 | 34.81 |
| Worked on any oil spill clean-up activities | 36 | 1.77 |
| Any property lost or damaged because of oil spill or cleanup | 50 | 2.46 |
| Total Economic Exposure Score (mean, SD)a | 0.69 | 0.87 |
| Total Physical Exposure Score (mean, SD)a | 0.93 | 1.08 |
Missing data: race/ethnicity (n=1); education (n=1); income (n=129); lost income (n=10); hit harder (n=34); negative influence (n=25); smell (n=82); physical contact (n=15); recreational activities (n=10); lost/damaged property (n=2)
Total scores calculated as sum of affirmative responses
Outcomes
Two mental health outcomes were assessed in both waves of data collection: depressive symptoms and mental distress. Depressive symptoms were measured with the 20-item Center for Epidemiological Studies Depression (CESD) Scale, which was designed for epidemiological studies to measure depressive symptoms, including those due to major depressive disorder, minor depression, secondary depression, situational depressive reaction, and transient mood variations.[35] Respondents were asked how often they had experienced a series of depressive symptoms in the past week, such as whether they were bothered by things that don’t usually bother them, or whether they felt happy. Higher scores indicated greater levels of depressive symptoms. The CESD was used in our models as a continuous outcome; for descriptive purposes, a score with a cut-off greater than or equal to 16 indicates depressive symptoms.[35] The Kessler-6 (K6) scale of non-specific psychological distress was used to screen for anxiety and mood disorders occurring within 30 days of the interview.36,37 Respondents were asked how often during the past 30 days they felt nervous, hopeless, restless or fidgety, depressed, that everything was an effort, and worthless. Higher scores indicated greater likelihood of mental distress. The K6 was also used in our models as a continuous outcome; for descriptive purposes, scores with a cut-off greater than or equal to 13 indicated probable serious mental distress, and scores between 8 and 12 indicated probable moderate mental distress.[36]
Covariates
Potential confounders were selected based on a review of the literature. Race was grouped into three categories: non-Hispanic white, non-Hispanic African American, and Hispanic/multiracial/other (which also included Asian/Pacific Islanders and Native Americans). Education at Wave 1 was measured as less than high school, high school graduate, and college or higher. Household income was reported at Wave 1 for the year immediately preceding the oil spill and at Wave 2 for the current year; it was grouped into four categories: ≤$20,000/year, between $20,000 and $50,000/year, between $50,000 and $80,000/year, and >$80,000/year. Age at the time of the oil spill was assessed at Wave 1 in years as a continuous variable.
Statistical Analysis
Descriptive statistics such as means and proportions were calculated for mental health outcomes, exposure items, and all covariates. Wilcoxon-signed rank tests were used to compare depressive symptoms and mental distress scores between two waves of data collection. Rate ratios were estimated for the association between oil spill exposure, time since the oil spill, and the mental health outcomes of depressive symptoms and mental distress scores using generalized estimating equations (GEE). Since the CESD and K6 scores were highly right-skewed, we assumed that both scores’ means and variance structure are from the Poisson distribution with log link in our GEE models with an unstructured working correlation matrix. Note that GEE methods are robust to an assigned correlation structure. All models were adjusted for age at oil spill, race, income, education, and time since the oil spill. We assumed a missing completely at random (MCAR) structure for missing variables in the final models. Although not presented here, we also assessed interactions between time and exposures in both models; none of the interactions were significant. All statistical analyses were performed using SAS 9.4.[37]
Results
Table 1 describes the sociodemographic and exposure characteristics of participating women at Wave 1. Women were White (55%) or African American (36%), high school graduates (58%), had a pre-oil spill household income of $20,000-$50,000/year (30%), and were on average 43.5 years old (SD 12.36) at the time of the oil spill. At Wave 1, women were interviewed on average 3.1 (SD 0.38, range 2.3–4.3) years after the oil spill; at Wave 2, they were interviewed on average 5.3 (SD 0.46, range 4.4–6.1) years after the oil spill.
Table 2 displays the mental health outcomes observed in the WaTCH population at each wave of data collection. Mean scores for depressive symptoms significantly increased over time from 11.9 (SD 12.52) at Wave 1 to 14.5 (SD 13.50) at Wave 2. Women who scored 16 or higher on the CESD scale, which is suggestive of depressive symptoms, comprised 28.2% of the sample at Wave 1 and 35.5% of the sample at Wave 2. Meanwhile, mean scores for mental distress significantly decreased from 6.2 (SD 5.28) at Wave 1 to 5.9 (SD 5.38) at Wave 2. Women who scored 13 or higher on the K6, suggestive of probable serious mental distress, comprised 12.9% of the sample at Wave 1 and 13.2% of the sample at Wave 2; while those who scored between 8 and 12 on the K6, suggestive of moderate mental distress, comprised 20.0% of the sample at Wave 1 and 15.8% of the sample at Wave 2.
Table 2.
Mental Health Outcomes at Waves 1 and 2, WaTCH Sample, N=2038, Louisiana, 2012–2016.
| Wave 1 | Wave 2 | ||||
|---|---|---|---|---|---|
| Characteristic | Mean | SD | Mean | SD | |
| Depressive Symptoms | 11.9 | 12.52 | 14.5 | 13.50 | *** |
| Presence of depressive symptoms (CESC >= 16) (n, %) | 572 | 28.2 | 722 | 35.5 | |
| No depressive symptoms (CESD < 16) (n, %) | 1459 | 71.8 | 1310 | 64.5 | |
| Mental Distress | 6.2 | 5.28 | 5.9 | 5.38 | *** |
| Severe mental distress (K6 >= 13) (n, %) | 262 | 12.9 | 268 | 13.2 | |
| Moderate mental distress (K6 = 8–12) (n, %) | 406 | 20.0 | 321 | 15.8 | |
| No mental distress (K6 < 8) (n, %) | 1359 | 67.0 | 1446 | 71.1 | |
p<0.05,
p<0.001,
p<0.0001 from Wilcoxon-signed rank tests between Waves 1 and 2
Missing data: Depressive symptoms (W1 n=7, W2 n=6); mental distress (W1 n=11, W2 n=3)
Note: Depressive symptoms measured with the Centers for Epidemiological Studies-Depression (CESD) scale; mental distress measured with the K6 scale.
Table 3 shows the results of GEE models of the associations over time between oil spill exposure and depressive symptoms and mental distress; results are presented in terms of rate ratios. For depressive symptoms, years elapsed since the oil spill, as well as both physical and economic exposure to the DHOS, were significantly associated with increasing depressive symptoms after adjustment for race/ethnicity, education, household income, and age at the time of the DHOS. For every unit increase in physical exposure score, the expected rate ratio for depressive symptoms increased by a factor of 1.11 (95% CI 1.06–1.14), while for every unit increase in economic exposure score, the expected rate ratio for depressive symptoms increased by a factor of 1.08 (95% CI 1.04–1.13). In addition, for every year increase in time since the oil spill, the expected rate ratio for depressive symptoms increased by a factor of 1.08 (95% CI 1.06–1.11). Similarly for mental distress, time since the oil spill as well as both physical and economic exposure to the DHOS were significantly associated with mental distress after adjustment for race/ethnicity, education, household income, and age at time of DHOS. For every unit increase in physical exposure score, the expected rate ratio for mental distress increased by a factor of 1.11 (95% CI 1.07–1.13); while for every unit increase in economic exposure score, the expected rate ratio for mental distress increased by a factor of 1.05 (95% CI 1.01–1.08). In contrast to depressive symptoms, however, for every year increase in time since the oil spill, the expected rate ratio for mental distress decreased by a factor of 0.97 (95% CI 0.95–0.99)).
Table 3.
GEE Models Predicting Mental Health Outcomes of Depressive Symptoms and Mental Distress, Waves 1 and 2, WaTCH Sample, Louisiana, 2012–2016.
| Depressive Symptoms (N=1848) | Mental Distress (N=1851) | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Rate Ratio | 95% CI | Rate Ratio | 95% CI | ||||
| Exposure to DHOS | ||||||||
| Physical exposure | 1.11 | 1.06 | 1.14 | *** | 1.11 | 1.07 | 1.13 | *** |
| Economic exposure | 1.08 | 1.04 | 1.13 | *** | 1.05 | 1.01 | 1.08 | * |
| Years since DHOS | 1.08 | 1.06 | 1.11 | *** | 0.97 | 0.95 | 0.99 | ** |
| Race/ethnicity (ref= Non-Hispanic White) | ||||||||
| Non-Hispanic African American | 1.04 | 0.96 | 1.14 | 0.98 | 0.91 | 1.06 | ||
| Hisp/multi/oth | 1.11 | 0.98 | 1.25 | 1.00 | 0.90 | 1.12 | ||
| Education (ref=College+) | ||||||||
| LT High school diploma | 1.62 | 1.43 | 1.82 | *** | 1.51 | 1.35 | 1.70 | *** |
| High school grad | 1.17 | 1.07 | 1.30 | ** | 1.13 | 1.04 | 1.22 | * |
| Income (ref=$80K+/yr) | ||||||||
| <$20K/yr | 1.77 | 1.57 | 1.97 | *** | 1.63 | 1.49 | 1.80 | *** |
| $20–$50K/yr | 1.40 | 1.27 | 1.57 | *** | 1.30 | 1.19 | 1.42 | *** |
| $50–$80K/yr | 1.21 | 1.09 | 1.34 | ** | 1.15 | 1.05 | 1.26 | * |
| Age at DHOS, years | 1.00 | 0.99 | 1.00 | ** | 0.99 | 0.99 | 1.00 | *** |
p<0.05,
p<0.001,
p<0.0001 from GEE models with Poisson distribution
Note: Samples sizes do not total to 2038 due to missing data.
To illustrate the model results, we grouped economic exposure into two categories (none (0) and any (1)) and physical exposure into three categories (none (0), one (1), and greater than one (2)) (see Table 1). Figure 1 shows the relationship between depressive symptoms and time by economic exposure category (panel A) and by physical exposure category (panel B). Predicted values of depressive symptoms increased over time, and for each type of exposure at each time point, those who experienced more exposure (economic or physical) had approximately 30% higher depression scores than those who experienced less exposure 6 years after the DHOS, when all covariates were fixed at their mean value or baseline category. Panels C and D show the relationship between mental distress and categories of economic and physical exposure. In this case, predicted values of mental distress decreased with time, although those who experienced more exposure (economic or physical) still had higher mental distress scores at each time point (approximately 11% for economic exposure and 29% for physical exposure 6 years after the DHOS). Interaction terms to test for changes in the exposure-outcome relationship were non-significant (data not shown).
Figure 1.
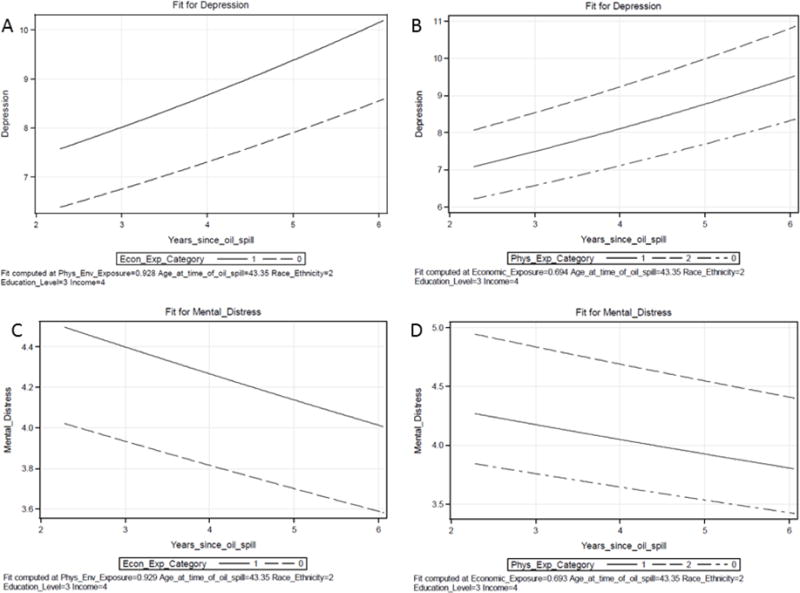
Illustration of relationship between mental health outcomes and exposure to the DHOS, over time. WaTCH Sample, Louisiana, 2012–2016. Panel A shows the relationship between depressive symptoms and years since the oil spill, by economic exposure category. Panel B shows the relationship between depressive symptoms and years since the oil spill, by physical exposure category. Panel C shows the relationship between mental distress and years since the oil spill, by economic exposure category. Panel D shows the relationship between mental distress and years since the oil spill, by physical exposure category.
Discussion
The objectives of this study were to 1) describe the changes in depressive symptoms and mental distress among women living in coastal Louisiana over two time periods following the DHOS; and 2) examine the relationship between DHOS exposure and the two mental health outcomes over time. We found that depressive symptoms among Louisiana coastal women had increased from Wave 1 (approximately 2–4 years after the oil spill) to Wave 2 (after 4–6 years of follow-up), while symptoms of mental distress had decreased in that same time period. We also found that initial associations between economic and physical exposure to the oil spill and both mental health outcomes have persisted up to six years after the spill, with women who were more highly exposed to the oil spill experiencing higher levels of depressive symptoms and mental distress at each time point.
The generalization that the greatest level of mental health symptoms occurs in the first year after a disaster[26] has not been affirmed in the present study with respect to depression. Our study reinforces other analyses of the DHOS of shorter duration.[30, 31, 38] For example, Hansel et al assessed recovery in 314 Gulf Coast residents in the first year following the DHOS (2010–11) and again just after the second anniversary (2012). Using the same measure of depression we did, they found that depression scores between the two time periods remained largely unchanged.[38] Our results show an increase in depressive symptoms after a longer time interval and thus begin to provide some definitive evidence to support long-term health impacts of oil spills.[39]
A possible explanation for the increase in depressive scores in the present study centers around the already heightened vulnerability of the study population due to previous disasters. The impact of Hurricanes Katrina and Rita in 2005 was extensive, with mental health consequences still being experienced years later. Indeed, an early study of the mental health effects of the DHOS found that prior exposure to Hurricane Katrina was associated with anxiety, depression, and posttraumatic stress, making residents even more vulnerable to the effects of the DHOS,[17] and highlighting the complexity of disentangling the cumulative effects from each disaster. A limitation of the current study is that almost all participants had been exposed to the 2005 hurricanes.[32]
Another possible explanation for the increase in depressive scores is the impact of oil spills on social ties. Reductions in social support are associated with post-disaster psychological symptoms.[26] Extensive research from the Exxon Valdez oil spill demonstrated the disruption of social relations that occurred in affected communities, leading to long-lasting psychological effects.[39] Our own analyses of the WaTCH sample from the first wave of data collection revealed the negative impact that oil spill exposure had on social capital and social support, coping resources that would normally protect against depression.[40] It is possible that these social resources continued to deteriorate and ultimately led to higher depressive scores even six years after the event.
Severe mental distress, on the other hand, actually did improve slightly over time in the present study, lending support to a more resilient recovery process whereby symptoms begin to decline following an acute period early post-disaster. This process is similar to patterns of mental health recovery observed after other disasters, where an immediate increase in symptoms in the first post-disaster year yields to subsequent declines thereafter.[26] For example, in a 27-year longitudinal follow-up of the capsizing of a North Sea oil rig, nonspecific distress was high in the first year after the disaster, but decreased by 14 months and leveled out after about 5 years.[41] Similarly, findings from a study of low-income parents in New Orleans demonstrated an increase in severe mental distress approximately a year after Hurricane Katrina,[42] with declines registered five years later, though they had not returned to pre-hurricane levels.[43] Results from the present study suggest a similar pattern of high levels of mental distress symptoms early post-disaster that later declined somewhat, lending support to the general rule for symptoms improving as time passes.[26] While it can be debated whether or not the observed decline in mental distress is meaningful in a clinical sense, we suggest that a population perspective that focuses on lowering the mean level of risk factors, or shifting the whole distribution of exposure in a favorable direction,[44] is more appropriate. Even a small change in the mental distress score, given the prevalence of the condition in our study, could translate into a meaningful differece when considered from a population perspective.
This study also found that the association between DHOS exposure and both types of mental health symptoms did not weaken over time, regardless of whether the symptoms increased or decreased. This finding lends more support to the conclusion that increased DHOS exposure is associated with worse mental health symptoms, as those with higher levels of exposure consistently exhibited more psychological symptoms, even up to six years after the disaster. For technological disasters such as oil spills, the exposure can be long-lasting, even after the immediate oil spill is contained and clean-up has been completed. Ongoing issues such as job or income loss, disruptions in subsistence and commercial activities such as fishing, and even the litigation process itself do not resolve themselves immediately and serve to keep the disaster prominent in survivors’ minds long after the acute experience has ended. In the case of the Exxon Valdez Oil Spill, where litigation continued for nearly 20 years, research showed that intrusive stress levels for litigants were higher eleven years after the spill than they were in the first few years, and involvement in oil spill litigation became a relatively stronger predictor of intrusive stress over time.[45] While the DHOS litigation ended after five years with the largest settlement in US history,[46] it was still ongoing at the time of the present study, and may account for the persistent relationship noted between oil spill exposure and mental health. Future studies are needed to identify the precise trends in mental health recovery and continuing associations with oil spill exposure.
This study is not without limitations. One is the lack of pre-oil spill baseline data, making it difficult to unravel the residual and cumulative mental health effects from previous disasters or other stressors. While our study does provide a longitudinal perspective, it is limited by its use of only two follow-up assessments. More research is needed with additional time points to understand the exact trajectories of post-disaster mental health symptoms. Nevertheless, few longitudinal studies of oil spill survivors exist with multiple follow-ups, and ours is the first to examine mental health as late as six years after the Deepwater Horizon oil spill. It is also the only study to examine mental health in a large community-dwelling sample of women distributed over seven coastal Louisiana parishes.
Conclusion
Future disaster mitigation and response planning must take into account the duration and nature of mental health symptoms. Understanding the post-disaster recovery patterns of affected residents can help direct critical mental health response efforts, and programs to decrease susceptibility to mental health problems can be developed and targeted.
Acknowledgments
The authors wish to thank the study participants and the Women and Their Children’s Health (WaTCH) Study staff. This research was supported by the National Institute of Environmental Health Sciences, National Institutes of Health (grant 1U01ES021497) with additional support from the Louisiana State University Health Sciences Center School of Public Health Epidemiology Program and Office of Research.
References
- 1.Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry. 2002;65:240–60. doi: 10.1521/psyc.65.3.240.20169. [DOI] [PubMed] [Google Scholar]
- 2.Goldmann E, Galea S. Mental Health Consequences of Disasters. Annual Review of Public Health. 2014;35:169–83. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- 3.Palinkas LA, Russell J, Downs MA, et al. Ethnic differences in stress, coping, and depressive symptoms after the Exxon Valdez oil spill. J Nerv Ment Dis. 1992;180:287–95. doi: 10.1097/00005053-199205000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Picou JS, Gill DA, Dyer CL, et al. Disruption and stress in an Alaskan fishing community: initial and continuing impacts of the Exxon Valdez oil spill. Industrial Crisis Quarterly. 1992;6:235–57. [Google Scholar]
- 5.Picou JS, Gill DA. The Exxon Valdez oil spill and chronic psychological stress. American Fisheries Society Symposium. 1996;18:879–93. [Google Scholar]
- 6.Palinkas LA, Petterson JS, Russell J, et al. Community patterns of psychiatric disorders after the Exxon Valdez oil spill. Am J Psychiatry. 1993;150:1517–23. doi: 10.1176/ajp.150.10.1517. [DOI] [PubMed] [Google Scholar]
- 7.Palinkas LA, Downs MA, Petterson JS, et al. Social, Cultural, and Psychological Impacts of the Exxon Valdez Oil Spill. Human Organization. 1993;52:1–13. [Google Scholar]
- 8.Arata CM, Picou JS, Johnson GD, et al. Coping with technological disaster: an application of the conservation of resources model to the Exxon Valdez oil spill. Journal of Traumatic Stress. 2000;13:23–39. doi: 10.1023/A:1007764729337. [DOI] [PubMed] [Google Scholar]
- 9.Palinkas LA, Petterson JS, Russell JC, et al. Ethnic differences in symptoms of post-traumatic stress after the Exxon Valdez oil spill. Prehospital & Disaster Medicine. 2004;19:102–12. doi: 10.1017/s1049023x00001552. [DOI] [PubMed] [Google Scholar]
- 10.Lyons RA, Temple JM, Evans D, et al. Acute health effects of the Sea Empress oil spill. J Epidemiol Community Health. 1999;53:306–10. doi: 10.1136/jech.53.5.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carrasco JM, Perez-Gomez B, Garcia-Mendizabal MJ, et al. Health-related quality of life and mental health in the medium-term aftermath of the Prestige oil spill in Galiza (Spain): a cross-sectional study. BMC Public Health. 2007;7:245. doi: 10.1186/1471-2458-7-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabucedo JM, Arce C, Senra C, et al. Symptomatic profile and health-related quality of life of persons affected by the Prestige catastrophe. Disasters. 2010;34:809–20. doi: 10.1111/j.1467-7717.2010.01170.x. [DOI] [PubMed] [Google Scholar]
- 13.Lee CH, Kang YA, Chang KJ, et al. Acute Health Effects of the Hebei Oil Spill on the Residents of Taean, Korea. J Prev Med Public Health. 2010;43:166–73. doi: 10.3961/jpmph.2010.43.2.166. [DOI] [PubMed] [Google Scholar]
- 14.Song M, Hong YC, Cheong HK, et al. Psychological Health in Residents Participating in Clean-up Works of Hebei Spirit Oil Spill. J Prev Med Public Health. 2009;42:82–8. doi: 10.3961/jpmph.2009.42.2.82. [DOI] [PubMed] [Google Scholar]
- 15.Kim YM, Park JH, Choi K, et al. Burden of disease attributable to the Hebei Spirit oil spill in Taean, Korea. BMJ Open. 2013;3:e003334. doi: 10.1136/bmjopen-2013-003334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi K-H, Lim M-H, Ha M, et al. Psychological vulnerability of residents of communities affected by the Hebei Spirit oil spill. Disaster Medicine and Public Health Preparedness. 2016;10:51–8. doi: 10.1017/dmp.2015.68. [DOI] [PubMed] [Google Scholar]
- 17.Osofsky H, Osofsky J, Hansel T. Deepwater Horizon Oil Spill: Mental Health Effects on Residents in Heavily Affected Areas. Disaster Medicine and Public Health Preparedness. 2011;5:280–6. doi: 10.1001/dmp.2011.85. [DOI] [PubMed] [Google Scholar]
- 18.Grattan LM, Roberts S, Mahan WT, Jr, et al. The Early Psychological Impacts of the Deepwater Horizon Oil Spill on Florida and Alabama Communities. Environmental Health Perspectives. 2011;119 doi: 10.1289/ehp.1002915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buttke D, Vagi S, Bayleyegn T, et al. Mental health needs assessment after the Gulf Coast oil spill-Alabama and Mississippi, 2010. Prehosp Disaster Med. 2012;27:401–8. doi: 10.1017/S1049023X12001100. [DOI] [PubMed] [Google Scholar]
- 20.Fan AZ, Prescott MR, Zhao G, et al. Individual and Community-Level Determinants of Mental and Physical Health After the Deepwater Horizon Oil Spill: Findings from the Gulf States Population Survey. Journal of Behavioral Health Services & Research. 2015;42:23–41. doi: 10.1007/s11414-014-9418-7. [DOI] [PubMed] [Google Scholar]
- 21.Rung AL, Oral E, Fontham E, et al. Mental health impact of the Deepwater Horizon Oil Spill among wives of clean-up workers. Epidemiol. 2015;26:e44–e6. doi: 10.1097/EDE.0000000000000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shenesey JW, Langhinrichsen-Rohling J. Perceived Resilience: Examining Impacts of the Deepwater Horizon Oil Spill One-Year Post-Spill. Psychological Trauma: Theory, Research, Practice, and Policy. 2015;7 doi: 10.1037/a0035182. [DOI] [PubMed] [Google Scholar]
- 23.Rung AL, Gaston S, Oral E, et al. Depression, Mental Distress and Domestic Conflict among Louisiana Women Exposed to the Deepwater Horizon Oil Spill in the Women and Their Children’s Health Study. Environmental Health Perspectives. 2016;124:1429–35. doi: 10.1289/EHP167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drescher CF, Schulenberg SE, Smith CV. The Deepwater Horizon Oil Spill and the Mississippi Gulf Coast: Mental health in the context of a technological disaster. Am J Orthopsychiatry. 2014;84:142–51. doi: 10.1037/h0099382. [DOI] [PubMed] [Google Scholar]
- 25.Cherry KE, Sampson L, Nezat PF, et al. Long-term psychological outcomes in older adults after disaster: relationships to religiosity and social support. Aging Ment Health. 2015:1–14. doi: 10.1080/13607863.2014.941325. [DOI] [PubMed] [Google Scholar]
- 26.Norris FH, Friedman MJ, Watson PJ, et al. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65:207–39. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- 27.Aguilera F, Méndez J, Pásaro E, et al. Review on the effects of exposure to spilled oils on human health. Journal of Applied Toxicology. 2010;30:291–301. doi: 10.1002/jat.1521. [DOI] [PubMed] [Google Scholar]
- 28.Gill DA, Picou JS. Technological disaster and chronic community stress. Society & Natural Resources. 1998;11:795–815. [Google Scholar]
- 29.Laffon B, Pasaro E, Valdigesias V. Effects of exposure to oil spills on human health: Updated review. Journal of Toxicology and Environmental Health, Part B. 2016;19:105–28. doi: 10.1080/10937404.2016.1168730. [DOI] [PubMed] [Google Scholar]
- 30.Buttke D, Vagi S, Schnall A, et al. Community Assessment for Public Health Emergency Response (CASPER) One Year Following the Gulf Coast Oil Spill: Alabama and Mississippi, 2011. Prehospital and Disaster Medicine. 2012;27:496–502. doi: 10.1017/S1049023X12001380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morris JG, Jr, Grattan LM, Mayer BM, et al. Psychological responses and resilience of people and communities impacted by the Deepwater Horizon Oil Spill. Transactions of the American Clinical and Climatological Association. 2013;124:191–201. [PMC free article] [PubMed] [Google Scholar]
- 32.Peters ES, Rung AL, Bronson MH, et al. The Women and Their Children’s Health (WaTCH) Study: Methods and Design of a Prospective Cohort Study in Louisiana to Examine the Health Effects from the BP Oil Spill. BMJ Open. 2017;7:e012887. doi: 10.1136/bmjopen-2016-014887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peres LC, Trapido E, Rung AL, et al. The Deepwater Horizon Oil Spill and Physical Health among Adult Women in Southern Louisiana: The Women and Their Children’s Health (WaTCH) Study. Environmental Health Perspectives. 2016;124:1208–13. doi: 10.1289/ehp.1510348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Radloff LS, Teri L. Use of the Center for Epidemiological Studies-Depression Scale with Older Adults. Clinical Gerontologist. 1986;5:119–36. [Google Scholar]
- 36.Kessler RC, Galea S, Jones RT, et al. Mental illness and suicidality after hurricane Katrina. Bulletin of the World Health Organization. 2006;2006:930–9. doi: 10.2471/blt.06.033019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.9.4 SAS. Cary, NC: SAS Institute; 2012. [Google Scholar]
- 38.Hansel CT, Osofsky JH, Osofsky DJ, et al. Longer-Term Mental and Behavioral Health Effects of the Deepwater Horizon Gulf Oil Spill. Journal of Marine Science and Engineering. 2015;3 [Google Scholar]
- 39.Palinkas LA. A Conceptual Framework for Understanding the Mental Health Impacts of Oil Spills: Lessons from the Exxon Valdez Oil Spill. Psychiatry. 2012;75:203–22. doi: 10.1521/psyc.2012.75.3.203. [DOI] [PubMed] [Google Scholar]
- 40.Rung AL, Gaston S, Robinson WT, et al. Untangling the disaster-depression knot: The role of social ties after Deepwater Horizon. Social Science & Medicine. 2017;177:19–26. doi: 10.1016/j.socscimed.2017.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boe HJ, Holgersen KH, Holen A. Mental Health Outcomes and Predictors of Chronic Disorders After the North Sea Oil Rig Disaster: 27-Year Longitudinal Follow-Up Study. J Nerv Ment Dis. 2011;199:49–54. doi: 10.1097/NMD.0b013e31820446a8. [DOI] [PubMed] [Google Scholar]
- 42.Rhodes J, Chan C, Paxson C, et al. The impact of hurricane Katrina on the mental and physical health of low-income parents in New Orleans. Am J Orthopsychiatry. 2010;80:237–47. doi: 10.1111/j.1939-0025.2010.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paxson C, Fussell E, Rhodes J, et al. Five years later: Recovery from post traumatic stress and psychological distress among low-income mothers affected by Hurricane Katrina. Social Science & Medicine. 2012;74:150–7. doi: 10.1016/j.socscimed.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rose G. Sick Individuals and Sick Populations. International Journal of Epidemiology. 1985;14:32–8. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 45.Marshall BK, Picou JS, Schlichtmann J. Technological Disasters, Litigation Stress and the Use of Alternative Dispute Resolution Mechanisms. Law & Policy. 2004 [Google Scholar]
- 46.Gregorio D. REFILE-TIMELINE-BP oil spill, litigation at a glance. Reuters. 2015 [Google Scholar]


