Abstract
Objective: Native fistula creation for hemodialysis in patients who have exhausted all their superficial veins presents a challenge to vascular practice. We review our experience in transposed basilic vein fistula (BVT) creation and its usage for hemodialysis.
Materials and Methods: We analyzed the hospital operative registry from January 2009 till June 2012 to identify the total number of BVT created in our center. Medical records of all patients were traced, and patients were interviewed using a standard proforma. In our center, BVT is performed as a two-stage procedure. All patients were routinely assessed with duplex scan preoperatively and postoperatively.
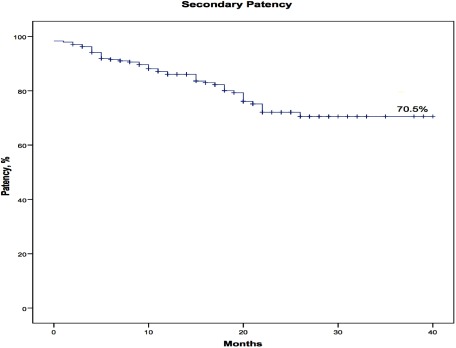
Results: Two hundred thirty-nine patients were recruited in the study. Of these patients, 50.6% were male and 49.4% were female. Mean age was 53.4 years. Of these patients, 81.2% had history of other previous fistula creation. Risk factors profile includes diabetes mellitus in 59.8%, hypertension in 86.2%, and smoking in 13.0%. Of these patients, 84.5% had no operative complication. Commonest complication was wound infection, 6.3%, followed by hemorrhage or hemotoma required surgical intervention, 5.9%, and pseudoaneurysm, 1.3%. Primary and secondary patencies were at 84.2% and 86.1% at 1 year and 67.7% and 70.5% at 3 years, respectively.
Conclusion: BVT is a credible option for challenging patients with absence of superficial veins for native fistula creation with good patency and low operative complication rate. Preoperative ultrasound assessment improves patient selection and outcome of BVT.
Keywords: transposed basilic vein, brachio-basilic fistula (BBF)
Introduction
End-stage renal failure (ESRF) is a common disease with significant disease burden, and the incidence is on the rise globally.1) In 2010, the reported prevalence of end-stage renal disease was 1,870 per million in the United States with Taiwan reaching 2,584. More than half of newly diagnosed ESRF patients have diabetes mellitus reported in a number of countries including Singapore, Malaysia, New Zealand, and Mexico.2)
ESRF is commonly associated with other comorbidities. Besides, there is also increasing incidence of more elderly population needing dialysis. Thus, it is a common encounter in current practice where patients who have exhausted their superficial veins present to surgeons requiring creation of permanent vascular access. Unfortunately, remaining vascular access options for this group of patients are generally confined to transposed arteriovenous fistula (AVF) and arteriovenous graft (AVG). Despite the earlier cannulation advantage of AVG, transposed AVF remains superior to AVG in terms of patency and complications profile. In line with the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF KDOQI) recommendation, native fistula takes preference over AVG.3)
We performed a retrospective review of the outcome of basilic vein transposition (BVT) carried out in our center, Kuala Lumpur Hospital.
Materials and Methods
The hospital surgical registry was revisited to identify the number of BVTs performed from January 2009 till June 2012. The medical records of all patients were traced, and relevant data were collected. Further information was obtained through telephone interviews with the patients and their respective dialysis center. Data collected include patients’ sex; age; risk factors such as diabetes mellitus, smoking, and hypertension; history of previous vascular access; complications of surgery; and patency. Statistical analysis was performed with Statistical Package for the Social Sciences (SPSS) Version 15. Association between categorical variables was tested with chi-squared test. Patency of BVTs was estimated with Kaplan–Meier estimate. Primary patency (intervention-free access survival) was defined as the interval from time of access placement to any intervention designed to maintain or reestablish patency or to access thrombosis or the time of measurement of patency. Secondary patency (access survival until abandonment) was defined as the interval from time of access placement to access abandonment or time of measurement of patency, including intervening manipulations (surgical or endovascular interventions) designed to reestablish the functionality of thrombosed access.4)
In our center, BVT is performed as a two-stage procedure for patients with the presence of suitable arm basilic vein and with no other suitable superficial veins. The clinical assessment and operative procedure are performed in a standard manner with minor variations between surgeons. All patients presented to our center will be assessed by duplex scan to assess both venous and arterial suitability for fistula creation, which consist of arm basilic vein of least 2.5 mm in diameter with no proximal stenosis and artery with no overt calcifications with good distal perfusion. In the first stage of BVT, brachio-basilic fistula (BBF) is created under local anesthesia. Patient will normally be discharged home on the same day of surgery and reviewed as outpatient to assess the maturity of the fistula both clinically and radiologically with duplex scan. Complications after the initial surgery, such as development of arm swelling secondary to central vein occlusion and infection, are addressed prior to the second-stage surgery. The second-stage surgery will usually be performed after around 6 to 8 weeks when the fistula has matured. This is performed under either general or regional anesthesia. The basilic vein is dissected from around 1 to 2 cm from the fistula anastomosis till the axilla with ligation and division of tributaries and preservation of medical cutaneous nerve of the forearm (Fig. 1). The basilic vein is then marked with sterile marking pen for orientation. Vascular control is obtained with vascular clamps near the initial anastomosis and at the axilla before the vein is divided near the anastomosis. The vein is flushed with heparinized saline and tunneled at a more superficial, anterior, and lateral position at the arm. The divided ends are then anastomosed using 7 ‘O’ polyprophylene sutures (Fig. 2). Any acute angulation, which may occur at both proximal and distal swing tunneled segments, is corrected by releasing the surrounding soft tissue. Depending on the surgeon’s discretion, a vacuum drain may be placed before closure of wound with absorbable suture (Fig. 3). Patient is normally discharged home at postoperative days 1 to 3 after the drain is taken down and satisfactory wound inspection. Patient is then reviewed around 2–3 weeks later, again, with clinical and duplex scan assessment for venous diameter, flow volume, and possible complication. A satisfactory assessment will lead on to patient to be referred to our nephrology colleague for cannulation when indicated.
Fig. 1 Basilic vein dissected in its length till the axilla (1) with the preservation of the medial cutaneous nerve of the forearm (2).
Fig. 2 Both ends of the divided basilic vein being anastomosed after tunneling.
Fig. 3 At the end of the procedure with the transposed course of basilic vein (arrow) at a more superficial, anterior, and lateral position.
Results
In total, 239 BVTs were performed in January 2009 till June 2012 in our center. This also represented 9.5% of total native fistula created in the study period, which was 2,513 cases. Gender distribution was almost equal with 50.6% male and 49.4% female. Mean age was 53.4 (17–81) years with age group of 50 to 59 years as the commonest group at 34.7%. Risk factors profile of patients includes diabetes mellitus in 59.8%, hypertension in 86.2%, and smoking in 13.0%.
Not surprisingly, 81.2% of patients had history of previous fistula creation with superficial veins, namely, radio-cephalic fistula (RCF) and brachio-cephalic fistula (BCF). Mean size of basilic vein was 7.5 (5–15) mm with mean flow rate of 1,034.1 mL/min before second-stage transposition. Of the BVTs, 53.7% were created at the left arm. There was no reported perioperative mortality, but there were primary failures in four patients (1.7%). Postoperatively, 84.5% of patients were free of operative complication. Commonest complication was wound infection, 6.3%, followed by hemorrhage or hematoma required surgical intervention, 5.9%, and pseudoaneurysm, 1.3%. All patients complicated with wound infection had superficial infection. They were diabetics and were treated satisfactorily with antibiotics with no associated primary failure. Surgical intervention for hemorrhage and pseudoaneurysm contributed to all the primary failures in the study. Beyond the perioperative period, secondary procedures were performed in 6.3% of patients for fistula salvage. Secondary procedures performed include thrombectomy with fistuloplasty of existing fistula stenosis in 12 patients and fistuloplasty alone in the remaining 3 patients. Primary and secondary patencies were at 84.2% and 86.1% at 1 year and 67.7% and 70.5% at 3 years, respectively (Figs. 4 and 5). We could not identify any statistically significant factors associated with fistula thrombosis in this study. In total, 19.7% of patients died within the period of this study.
Fig. 4 Kaplan–Meier curve for primary patency.
Fig. 5 Kaplan–Meier curve for secondary patency.
Discussion
The basilic vein is situated deep at the medial aspect of the arm. This natural position renders the basilic vein relatively free from cannulation and trauma. Coupled with its decent diameter and straight course, basilic vein appears to be a good option for AVF construction. However, the basilic vein is often deeply located within the deep fascia with close proximity to the brachial artery and medial cutaneous nerve of the forearm. As such, cannulation of this vein without transposition or superficialization is often dangerous. Hence, the creation of a functioning of BVT is more tedious and time-consuming as compared with RCF, BCF, and AVG.
BVT was first described by Dagher et al. in 1976.5) Different variations of basilic vein surgery for vascular access have been described in the literature that include single- or two-stage anterolateral transposition with tunneling, transposition with creation of subcutaneous flap without tunneling, and simple elevation of basilic vein.6,7) As the later two techniques do not involve basilic vein division and re-anastomosis, a major branch of the medical cutaneous nerve of the forearm may be divided, which may result in paresthesia. Hossny, interestingly, reported dialysis nurses were more satisfied handling BVTs compared with elevated fistulae (100% vs. 53.3%) (p<0.01) with problems that include difficult cannulation, frequent needle displacement, and patient complaints.8)
BVT, whether best performed as a single- or two-stage surgery, still remains controversial. In our center, we favor the two-stage approach. Arterialized basilic vein has thicker wall and often elongates, which eases dissection and tunneling to place the vein at a more superficial, anterior, and lateral position. Besides, a two-stage approach will prevent unnecessary more major transposition surgery for patients with primary failure of BBF. We will consider performing single-stage BVT in patients with previous functioning RCF or BCF in which the basilic vein is arterialized. The obvious disadvantage of the two-stage procedure is the need for two separate procedures and prolonged presence of indwelling catheter for patients already on hemodialysis support. However, timely referral for fistula creation before initiation of hemodialysis will prevent the need of vascular catheterization and its complications. In the literature, El Mallah reported the only prospective randomized study on single-stage vs. two-stage BVT. He reported 4 weeks postoperative patency of 60% in single-stage procedure as compared with 90% in two-stage procedure. Furthermore, at the end of the study with follow-up period of 6 to 24 months, overall patency was 50% in the single-stage group and 80% in the two-stage group with statistical significance.9) However, Bashar et al., in a systemic review and meta-analysis, did not find significant statistical difference between single- and two-stage BVT despite more studies in the review favor a two-stage approach.10)
Autologous AVF has remained the preference of NKF KDOQI guidelines.3) This recommendation is also applicable when comparing BVT and AVG. There are numerous studies reported comparing BVT and AVG with some conflicting results. Coburn and Carney reported BVT with superior primary and secondary patency when compared with AVG at 2 years, 86% vs. 49% and 70% vs. 64%, respectively. Complications, which include infection and arterial steal, occurred two and a half times more frequently in AVG than in BVT (p<0.05).11) Echoing this finding, Morosetti et al., in their review, reported 2 year primary patency of 60% in BVT as compared with 21% in AVG. Two year secondary patency was 66% vs. 34%. AVG group also demonstrated more long-term adverse events. However, the mean interval between first needling and intervention was, as expectedly, longer in the BVT group (47+/− 3 and 27+/− 3 days, respectively).12) Weale et al. in their retrospective comparison of BVT and AVG reported 2 year primary patency of 40% and 43.2%, respectively, and there was no significant difference in secondary patency. However, infective complications necessitating an operation were significantly higher in the AVG group (6.2% vs. 0%; p=0.031).13) In our series, 6.3% of patients had superficial infection that resolved with antimicrobial treatment without affecting primary patency. The higher rate of infection could be secondary to higher incidence of diabetes mellitus, which is 59.8%. Davoudi et al., in a recent smaller study, reported the mean primary patency time in the BVT and AVG groups at 244.13±103.65 and 264.97±149.28, respectively with no statistically significant difference between the two groups (p=0.533). Complications profile was reported to be similar between these groups.14) In general, most studies reported BVT to be superior in patency and has a better complications profile as compared with AVG. Most authors suggested BVT to be the preferred option for vascular access in patients with no suitable veins for superficial fistula creation.
In our center, we routinely perform duplex scan assessment preoperatively and postoperatively for all vascular access cases. Duplex scan is even more important for preoperative assessment of BBF as the basilic vein is located deep at the medial side of the arm and, thus, not well visualized on clinical examination. Besides, in patients whose medial cubital vein is fibrosed or small at cubital fossa, the more proximal segment of the vein or the basilic vein, which is deeper at the medial aspect of the arm, can be assessed more accurately by duplex scan. Both Mihmanli et al. and Zhang et al. reported superiority of routine duplex scan to clinical examination.15,16) In Mihmanli et al. series, immediate postoperative patency of fistula were 95% vs. 75% in duplex scan group and clinical examination group, respectively. Meanwhile, Zhang et al. reported 6 months patency of 90% in those assessed by preoperative duplex scan as compared with 80% by clinical examination alone.
The results in our study with 3 years primary and secondary patency at 66.2% and 70.5% are modest figures and are favorably compared with other previously reported studies. Our center represents the major vascular referral center in Malaysia and, thus, caters for vascular service of a wide geographical area. This renders routine long-term follow-up and timely referrals for problematic fistulae difficult. This may explain the low secondary intervention rate and the relatively small difference between the primary and secondary patency rates.
Conclusion
We believe BVT is a credible option for challenging patients with absence of superficial veins for native fistula creation with good patency and low operative complication rate. Besides, preoperative ultrasound assessment improves patient selection and outcome of BVT.
Disclosure Statement
All authors have no conflict of interest.
Additional Remarks
The abstract of this article was published in ASVS 2014abstract book.
Author Contributions
Study conception: BL, AZ
Data collection: BL
Analysis: BL
Investigation: all authors
Writing: all authors
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
References
- 1).Hamer RA, El Nahas AM. The burden of chronic kidney disease is rising rapidly worldwide. BMJ 2006; 332: 563-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).2012 United States Renal Data System Annual Data Report. 2012; 2: 341-52. [Google Scholar]
- 3).Vascular Access 2006 Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis 2006; 48 Suppl 1: S176-247. [DOI] [PubMed] [Google Scholar]
- 4).Sidawy AN, Gray R, Besarab A, et al. Recommended standards for reports dealing with arteriovenous hemodialysis accesses. J Vasc Surg 2002; 35: 603-10. [DOI] [PubMed] [Google Scholar]
- 5).Dagher FJ, Gelber RL, Ramos EJ, et al. Basilic vein to brachial artery fistula: a new access for chronic hemodialysis. South Med J 1976; 69: 1438-40. [DOI] [PubMed] [Google Scholar]
- 6).Dukkipati R, de Virgilio C, Reynolds T, et al. Outcomes of brachial artery-basilic vein fistula. Semin Dial 2011; 24: 220-30. [DOI] [PubMed] [Google Scholar]
- 7).Francis DM, Lu Y, Robertson AJ, et al. Two-stage brachiobasilic arteriovenous fistula for chronic haemodialysis access. ANZ J Surg 2007; 77: 150-5. [DOI] [PubMed] [Google Scholar]
- 8).Hossny A. Brachiobasilic arteriovenous fistula: different surgical techniques and their effects on fistula patency and dialysis-related complications. J Vasc Surg 2003; 37: 821-6. [DOI] [PubMed] [Google Scholar]
- 9).El Mallah S. Staged basilic vein transposition for dialysis angioaccess. Int Angiol 1998; 17: 65-8. [PubMed] [Google Scholar]
- 10).Bashar K, Healy DA, Elsheikh S, et al. One stage vs. two-stage brachio-basilic arteriovenous fistula for dialysis access: a systemic review and meta-analysis. PLoS ONE 2015; 10: e0120154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Coburn MC, Carney WI Jr. Comparison of basilic vein and polytetrafluoroethylene for brachial arteriovenous fistula. J Vasc Surg 1994; 20: 896-902; discussion, 903-4. [DOI] [PubMed] [Google Scholar]
- 12).Morosetti M, Cipriani S, Dominijanni S, et al. Basilic vein transposition versus biosynthetic prosthesis as vascular access for hemodialysis. J Vasc Surg 2011; 54: 1713-9. [DOI] [PubMed] [Google Scholar]
- 13).Weale AR, Bevis P, Neary WD, et al. A comparison between transposed brachiobasilic arteriovenous fistulas and prosthetic brachioaxillary access grafts for vascular access for hemodialysis. J Vasc Surg 2007; 46: 997-1004. [DOI] [PubMed] [Google Scholar]
- 14).Davoudi M, Tayebi P, Beheshtian A. Primary patency time of basilic vein transposition versus prosthetic brachioaxillary access grafts in hemodialysis patients. J Vasc Access 2013; 14: 111-5. [DOI] [PubMed] [Google Scholar]
- 15).Mihmanli I, Besirli K, Kurugoglu S, et al. Cephalic vein and hemodialysis fistula: surgeon’s observation versus color Doppler ultrasonographic findings. J Ultrasound Med 2001; 20: 217-22. [DOI] [PubMed] [Google Scholar]
- 16).Zhang Z, Wang XM, Zhang ZW, et al. Hemodynamic evaluation of native arteriovenous fistulas for chronic hemodialysis with color Doppler ultrasound. Chin J Med Imaging Technol 2006; 22: 718-21. [Google Scholar]