Abstract
Background:
Prior to spine surgery (SS), we ask whether and when to stop low-dose aspirin (LD-ASA), particularly in patients with significant cardiovascular disease (CAD). Although platelets typically regenerate in 10 days, it can take longer in older patients.
Methods:
Here we reviewed several studies regarding the perioperative risks/complications [e.g. hemorrhagic complications, estimated blood loss (EBL), continued postoperative drainage] for continuing vs. stopping LD-ASA at various intervals prior to lumbar SS.
Results:
Multiple studies confirmed the increased perioperative risks for continuing LD-ASA throughout SS, or when stopping it for just 3–7 preoperative days; however, there were no increased risks if stopped between 7 to 10 days postoperatively. Other studies documented no increased perioperative risk for continuing LD-ASA throughout SS, although some indicated increased morbidity (e.g., one patient developed a postoperative hematoma resulting in irreversible paralysis).
Conclusions:
Several studies demonstrated more hemorrhagic complications if LD-ASA was continued throughout or stopped just 3 to up to 7 days prior to SS. However, there were no adverse bleeding events if stopped from 7–10 days preoperatively. As a spine surgeon who wishes to avoid a postoperative epidural hematoma/paralysis, I would recommend stopping LD-ASA 10 days or longer prior to SS. Nevertheless, each spine surgeon must determine what is in the “best interest” of their individual patient. Certainly, we need future randomized controlled trials to better answer: when and if to stop LD-ASA before spine surgery.
Keywords: Bleeding complications, cardiac risk, hemorrhagic sequelae, low-dose aspirin, perioperative spine surgery, postoperative drainage, prophylaxis
INTRODUCTION
For patients on low-dose aspirin (LD-ASA) (e.g., 81–100 mg) prophylaxis for cardiovascular disease (CAD) (e.g., stents, bypasses, other), spine surgeons frequently confront whether or when to stop therapy prior to spine surgery (SS). Platelets typically regenerate in 10 days, although it may take longer for older patients. In this editorial and focused review of the literature, we briefly compared the perioperative risks/complications [e.g., hemorrhagic complications, estimated blood loss (EBL), continued postoperative drainage] for continuing vs. discontinuing (e.g. stopping LD-ASA from 3-<7 and from 7-10 days) LD-ASA at different intervals prior to lumbar SS.
Part 1: Increased perioperative bleeding risks using low-dose aspirin (LD-ASA) for spine surgery [Table 1]
Table 1.
Increased risks for continuing low-dose aspirin for spine surgery
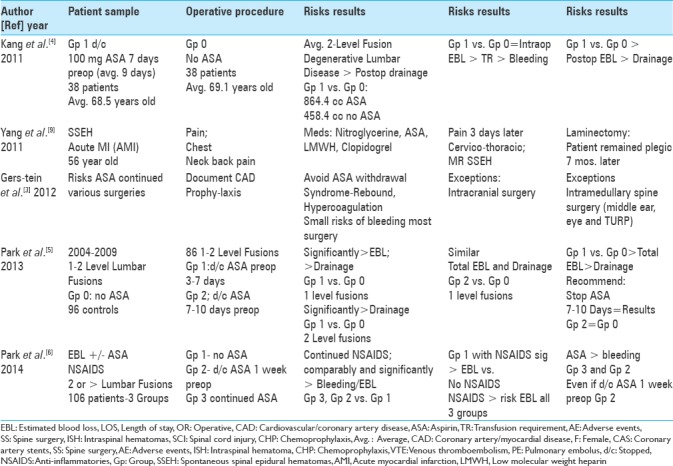
Increased perioperative bleeding risks when low-dose aspirin was continued or not stopped long enough prior to lumbar spine surgery
Several series documented the increased perioperative risks/complications (e.g., hemorrhagic complications, EBL, continued postoperative drainage) when LD-ASA was continued and/or stopped for just 3 up to 7 days preoperatively vs. finding no such risks for LD-ASA stopped for 7–10 (average 9) preoperative days.[4,5] For patients undergoing 1-level lumbar fusions in Kang et al. (2011), Group 0 were on no LD-ASA, whereas Group 1 patients stopped LD-ASA (100 mg) at least 7 days (average 9 days) preoperatively. Although both groups demonstrated comparable intraoperative bleeding, Group 1 patients showed more postoperative bleeding, greater estimated postoperative blood loss, more drainage, and higher transfusion requirements [Table 1].[4] Park et al. (2013) evaluated the hemorrhagic complications for patients undergoing 1–2 level lumbar fusions on no ASA (Group 0) vs. LD-ASA stopped 3–7 days (Group 1) vs. LD-ASA stopped 7–10 days (Group 2) preoperatively [Table 1].[5] Cessation of LD-ASA 7–10 days preoperatively in Group 2 patients resulted in no significant increased bleeding risks when compared with those on no LD-ASA (Group 0). However, more bleeding risks/complications were observed for Group 1 patients where LD-ASA was just stopped 3–7 days prior to surgery.
Increased blood loss with low-dose aspirin and/or anti-inflammatories (NSAIDS) for patients undergoing spinal surgery
Increased hemorrhagic risks were observed in Park et al. (2014) where patients were divided into three groups based on LD-ASA use, and additionally given NSAIDS prior to 2 or more level lumbar fusions [Table 1].[6] Group I patients were on no LD-ASA, Group 2 patients stopped LD-ASA 1 week preoperatively, whereas Group 3 patients continued LD-ASA throuhgout surgery. LD-ASA significantly increased bleeding for Group 3 and Group 2 patients (stopped 7 days preoperatively). Interestingly, additional utilization of NSAIDS in all three groups comparably increased intraoperative, postoperative, and total blood loss. Furthermore, Group 1 patients (on no LD-ASA) but on NSAIDS had significantly greater EBL vs. Group 1 patients on no NSAIDS.
Surgical risk for bleeding on low-dose aspirin increased in cranial/selective spinal surgery
Gerstein et al. (2012) determined that continuing LD-ASA to avoid perioperative rebound/hypercoagulation syndrome resulted in only a small increased risk of bleeding for most operations, notably excluding cranial surgery, intramedullary spine surgery, middle ear surgery, eye surgery, and transurethral prostatectomy [Table 1].[3] Given the results from previously quoted studies, these exclusion criteria should probably include other spinal procedures as well.
Case: Acute spontaneous spinal epidural hematoma due to antiplatelet and anticoagulation therapy for acute myocardial infarction
In Yang et al. (2010), a 56-year-old male presented with an acute myocardial infarction (AMI) for which he was placed on nitroglycerine, aspirin, low-molecular-weight heparin prophylaxis, and Clopidogrel [Table 1].[9] Three days after the AMI, he developed acute cervicothoracic pain and quadriplegia. When the MR documented a spontaneous cervicothoracic spinal epidural hematoma (SSEH), he underwent emergent surgical decompression. Unfortunately, at 7 postoperative months, he failed to recover. Spontaneous bleeding risks attributed to the simultaneous administration of multiple antiplatelet and anticoagulation therapies should be carefully considered particularly in patients who suddenly develop the new onset of pain complaints and/or new neurological deficits.
Part II: No increased risks for continuing low-dose aspirin (LD-ASA) for spine surgery [Table 2]
Table 2.
No increased risks for continuing aspirin with spine surgery
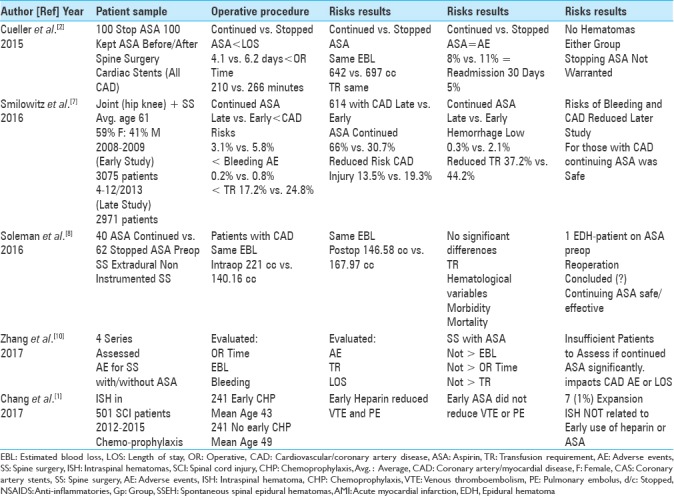
Studies support continuation of low-dose aspirin for spine surgery but with instances of acute epidural hematoma/permanent paraplegia
Although several studies supported continuing LD-ASA throughout spine surgery, some series cited significant perioperative morbidity (e.g., permanent paraplegia).[2,7,10] In 2015, Cueller et al. studied patients with cardiac disease (CAD) undergoing spine surgery who either continued LD-ASA (100 mg/day) or discontinued LD-ASA (100 mg/day) prior to the surgery [Table 2].[2] Those continuing LD-ASA demonstrated a decreased length of stay and operative time, while showing comparable postoperative EBL, complications, and readmission rates (30 postoperative days). In 2016, Smilowitz et al. analyzed patients kept on LD-ASA throughout joint or spine surgery; here, they divided them into early (2008–2009; 3075 patients) and late groups (2013: 2971 patients) [Table 2].[7] The late group showed a reduced risk of perioperative CAD complications, fewer bleeding-related adverse events/significant hemorrhages, and reduced transfusion requirements. When Zhang et al. (2017) evaluated 4 SS series performed with/without perioperative LD-ASA, they found continuing LD-ASA did not increase EBL, surgical time, or transfusion requirements [Table 2].[10] However, they found their data were insufficient to determine whether continuing LD-ASA significantly impacted the frequency of perioperative cardiac events, bleeding complications, or LOS.
Postoperative epidural hematoma in patient continuing perioperative ASA
Soleman et al. (2016) compared two patient groups undergoing extradural noninstrumented spinal surgery; in 40 patients, LD-ASA was continued, whereas in 62 patients, LD-ASA was stopped prior to the surgery [Table 2].[8] They claimed intraoperative and postoperative blood loss were similar for both groups; however, data for the former were quite disparate, e.g. averaging 221 cc (for the continued LD-ASA group) vs. 140.16 cc for the latter group (stopped LD-ASA). Notably, they concluded there were no significant differences in hematological variables, morbidity, and mortality. Nevertheless, 1 patient remaining on LD-ASA developed an epidural hematoma resulting in irreversible paralysis. How could they, therefore, conclude continuing perioperative LD-ASA for SS was safe and effective?
Mini-heparin and low-dose chemoprophylaxis do not increase size of intraspinal hematoma following spinal cord injury
Following spinal cord injury (SCI), Chang et al. (2017) compared the frequency of intraspinal hemorrhage for 241 patients on early chemoprophylaxis vs. 241 patients not placed on early prophylaxis (e.g., mini-heparin, LD-ASA) for deep venous thrombosis ([DVT]/pulmonary embolism [PE]). [Table 2].[1] Although mini-heparin reduced the incidence of DVT/PE, LD-ASA did not. Of interest, neither mini-heparin or LD-ASA contributed to clot expansion in 7% of the patients who originally presented with SCI-related intraspinal hematomas.
CONCLUSIONS
Multiple studies demonstrated the relative increased hemorrhagic risks/complications of performing spinal surgery while continuing LD-ASA or just stopping LD-ASA for 3–7 days prior to SS; notably, several other studies also indicated no such risks if LD-ASA was stopped for >7–10 days [Tables 1 and 2].[1,2,3,4,5,6,7,8,9,10] As a spine surgeon who wants to avoid an intraspinal hematoma and irreversible neurological injury, my bias would be to stop ASA at least 7–10 days prior to SS (e.g., more toward day 10). Notably, these studies were of variable quality (e.g., no adequate randomized controlled trials), and came to different conclusions. Finally, each spine surgeon must determine on a case-by-case basis what is in the “best interest” of their patient.
Footnotes
REFERENCES
- 1.Chang R, Scerbo MH, Schmitt KM, Adams SD, Choi TJ, Wade CE, et al. Early chemoprophylaxis is associated with decreased venous thromboembolism risk without concomitant increase in intraspinal hematoma expansion after traumatic spinal cord injury. J Trauma Acute Care Surg. 2017;83:1088–94. doi: 10.1097/TA.0000000000001675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cuellar JM, Petrizzo A, Vaswani R, Goldstein JA, Bendo JA. Does aspirin administration increase perioperative morbidity in patients with cardiac stents undergoing spinal surgery? Spine (Phila Pa 1976) 2015;40:629–35. doi: 10.1097/BRS.0000000000000695. [DOI] [PubMed] [Google Scholar]
- 3.Gerstein NS, Schulman PM, Gerstein WH, Petersen TR, Tawil I. Should more patients continue aspirin therapy perioperatively.: Clinical impact of aspirin withdrawal syndrome? Ann Surg. 2012;255:811–9. doi: 10.1097/SLA.0b013e318250504e. [DOI] [PubMed] [Google Scholar]
- 4.Kang SB, Cho KJ, Moon KH, Jung JH, Jung SJ. Does low-dose aspirin increase blood loss after spinal fusion surgery? Spine J. 2011;11:303–7. doi: 10.1016/j.spinee.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Park JH, Ahn Y, Choi BS, Choi KT, Lee K, Kim SH, et al. Antithrombotic effects of aspirin on 1- or 2-level lumbar spinal fusion surgery: A comparison between 2 groups discontinuing aspirin use before and after 7 days prior to surgery. Spine (Phila Pa 1976) 2013;38:1561–5. doi: 10.1097/BRS.0b013e31829a84d2. [DOI] [PubMed] [Google Scholar]
- 6.Park HJ, Kwon KY, Woo JH. Comparison of blood loss according to use of aspirin in lumbar fusion patients. Eur Spine J. 2014;23:1777–82. doi: 10.1007/s00586-014-3294-y. [DOI] [PubMed] [Google Scholar]
- 7.Smilowitz NR, Oberweis BS, Nukala S, Rosenberg A, Stuchin S, Iorio R, et al. Perioperative antiplatelet therapy and cardiovascular outcomes in patients undergoing joint and spine surgery. J Clin Anesth. 2016;35:163–9. doi: 10.1016/j.jclinane.2016.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soleman J, Baumgarten P, Perrig WN, Fandino J, Fathi AR. Non-instrumented extradural lumbar spine surgery under low-dose acetylsalicylic acid: A comparative risk analysis study. Eur Spine J. 2016;25:732–9. doi: 10.1007/s00586-015-3864-7. [DOI] [PubMed] [Google Scholar]
- 9.Yang SM, Kang SH, Kim KT, Park SW, Lee WS. Spontaneous spinal epidural hematomas associated with acute myocardial infarction treatment. Korean Circ J. 2011;41:759–62. doi: 10.4070/kcj.2011.41.12.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang C, Wang G, Liu X, Li Y, Sun J. Safety of continuing aspirin therapy during spinal surgery: A systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e8603. doi: 10.1097/MD.0000000000008603. [DOI] [PMC free article] [PubMed] [Google Scholar]


