Abstract
Background:
Emotional response to infertility is mediated by numerous interrelated psychological variables such as personality, health perceptions, cognitive appraisals, coping, and social support. While men and women respond to infertility differently, illness cognitions are a vital component of their emotional adjustment. The aim of this study is to compare the infertile men and women undergoing fertility treatments on perceived distress, helplessness, acceptance, benefits, anxiety, and depression.
Materials and Methods:
Eighty-one infertile couples, undergoing intrauterine insemination participated in the study. They were assessed on the presence of infertility distress using the fertility problem inventory, for psychiatric morbidity using the Mini International Neuropsychiatric Interview, for affective disturbances using the Hamilton Anxiety and Depression scales, and for illness cognitions using the Illness Cognition Questionnaire.
Statistical Analysis:
Data are analyzed using SPSS version 15. The paired sample t-test is performed for assessing differences on normally distributed data. The Wilcoxon Signed-Rank test is performed for assessing differences in medians obtained on data that was skewed.
Results and Discussion:
Infertile women (wives) were more emotionally distressed, anxious, and depressed than men (husbands). Gender-wise differences were found for perceptions of helplessness and acceptance of infertility. Infertility was perceived to be a nonbeneficial event for both partners investigated.
Conclusion:
Negative cognitions and affective disturbances may contribute to higher treatment burden in couples seeking-assisted conception. The present study suggests that psychosocial intervention for couples plays a central role and should be integrated within the conventional treatments for infertility.
KEYWORDS: Anxiety, appraisal, assisted conception, burden, cognition, couple, depression, Infertility specific stress, men, treatments, women
INTRODUCTION
One of the earliest definitions of “cognition” defines it as a mental process of knowing, by which internal and external sensory input is transformed, reduced, elaborated, stored, recovered, and used.[1] It comprises all activities related to perceiving, thinking, remembering, planning, and making choices in daily lives. “Illness cognitions” are terms used to describe a range of cognitive processes underlying the human behavior in response to the illness-related information. Illness cognitions exist in each person, in the presence of physical illness and even in its absence. The self-regulatory model of illness perceptions proposes that many features of one's medical illness, namely its label, identity, short-term and long-term consequences, temporal course, causes, curability, and controllability affects the way people cope and recover from it.[2] From this analogy, psychological distress due to a medical illness is higher if it is perceived as dangerous, life-changing, threatening, chronic, continuous, and incurable. There also exists a close association between illness cognitions and other health-related behaviors such as treatment-seeking, self-care, lifestyle habits, compliance, and adherence.[3] The complex and reciprocal interplay of personality characteristics, emotions, and cognitions governs the personal representations of health and illness.[4] For instance, if a person with a fairly stable personality believes that an illness is caused by identifiable factors, is curable, has shorter duration, then it has relatively minor psychological consequences for him/her.
Illness perceptions and cognitions are also known to be independent contributors to disease management, morbidity, well-being, functional recovery, and comorbid psychiatric disorders in individuals with acute and chronic disease.[5,6,7,8,9] Numerous studies have highlighted the role of cognitions in coping with acute and chronic medical illnesses.[10]
In the light of these perspectives, it is worth hypothesizing that an individual's cognitive appraisal with regard to “being childless” considerably impacts the magnitude of perceived stress. Review supports that intrusive ideation increases distress in infertility.[11] Furthermore, the emotional struggles of infertile couples often elevate when treatments span over several years, and they endure undesirable treatment outcomes over and over again. This may be the reason that distress gradually elevates after the third year of fertility treatment.[12,13] Research on stress and coping in infertility reveals that core cognitions associated with this condition are unpredictability, negativity, uncontrollability, and ambiguity.[14] Furthermore, studies accentuate the important of cognitions such as personal threat, powerlessness, helplessness, hopelessness, and nonacceptance in infertility.
Cognitions of powerlessness in infertility stem from an unfavorable diagnostic labels such as severe sperm defects,[15] premature ovarian failure,[16] treatment outcomes like limited success rates per cycle, poor or nonresponse,[17] side-effects like ovarian hyperstimulation syndrome,[18] nonfulfilment of social role, stigma, discrimination, exclusion from entitled family roles, and kinships and auspicious rituals.[19,20] Feelings of uncontrollability develop as patients experience a loss of control over several aspects such as one's own body (in controlled ovarian hyperstimulation cycles and otherwise), sexuality, intimate lives, loss of privacy, and an increased sense of being invaded.[21,22] Moreover, feelings of powerlessness and uncontrollability worsen with elevating distress and psychopathology further leading to a poorer psychological adjustment in women during in vitro fertilization (IVF).[23] Men's psychological adjustment also gets affected overtime as it is indirectly related to their spouse's emotional well-being.[24] Research also reports that “perception of heightened threat and uncontrollability” can stem due to three causes.[25] Firstly, if stress keeps on increasing it will naturally cause a decline in one's the psychological endurance over time. Secondly despite best efforts, if the desired results are not attained it leads to frustrations and disappointments. Moreover, finally, uncontrollability arises when random rather than predictable and planned course of events affect the pregnancy outcomes.
Data from the latest investigation reflects that “hope” is a mental state that protects women from getting depressed.[26] Furthermore, women who receive social support and patient-centric professional support from infertility staff are emotionally stronger even in times of high stress.[27] Hopelessness develops overtime in women and is governed by two factors, namely chronic treatment failures and increasing duration of infertility.[26] It is also documented that feelings of helplessness coupled with hopelessness are highest around events such as poor treatment response, abandoned cycles, failed fertilization, miscarriages, repeated pregnancy loss, and other complications.[28,29] In addition, during the pretreatment phases, helplessness serves as a vulnerability factor whereas acceptance and hope serve as protective factors against psychological distress in infertile women undergoing cycles of IVF/intracytoplasmic sperm injection.[30,31] Hopelessness is found to be more prevalent in infertile women with low educational achievement, uneducated spouse, and unemployment and is not related to factors such as the age of patients, length of marital duration, and cause of infertility.[27,32,33]
Theoretically speaking, “learnt helplessness” is another related psychological phenomenon that may explain why distressed patients prematurely drop out from fertility treatments. Learned helplessness[34] is “a mental state in which an organism who is forced to bear aversive or unpleasant stimuli, becomes unable or unwilling to avoid subsequent encounters with those stimuli, even if they are “escapable,” presumably because he has learned that it cannot control the situation.”[35]
Acceptance of infertility as a medical and social condition is a complex process rather than a stage-specific event. It evolves gradually, over several years and course of events faced by childless couples.[36] Acceptance in those who face less (<two cycles of IVFs per year) or high amounts of treatment failure (>seven cycles of failed IVFs per year) is usually stable. It fluctuates in those who face moderate amount of IVF failure (four cycles of conventional and aggressive treatment failures per year) since their mind set dwindles between periods of optimism and despair.[37] The later researcher also highlights that acceptance and adjustment is not associated with age of women and the duration of infertility or treatments.
In addition to these facts, it is believed that health beliefs and illness cognitions serve as important predictors of “coping with infertility.” Evidences support that positive mental states such as acknowledging fertility struggles, realistic optimism, emotion-focused efforts, active problem-solving, grief resolution, mindful compassion, empathetic partner communication, and acceptance are associated with constructive coping, healthy, and speedy recovery from infertility crisis.[38,39,40,41,42] On the other hand, responses such as denial, blaming, and active or passive avoidance are associated with negative psychological health.[18,19,20,21,22]
Despite these evidences on the importance of “cognitive beliefs and appraisals in infertility,” limited Indian studies have ventured into this area. The emotional trauma and grief of treatment repeaters, particularly in “pronatalic Indian setups,” are often neglected.[15,16,20] Accordingly, as cited in Western literature one cannot rule out the possibility that even in our kind of setups “psychological factors” elevate overall dropouts from fertility treatments.[43] Research also supports that critical events (such as repeated IVF failures) is known to be associated with adverse beliefs such as “infertility is chronic, has adverse consequences, and is uncontrollable,” and this lowers patient's confidence in its treatment efficacy.[44]
Moreover, the physical and emotional burden are reported to be among the top three causes of treatment discontinuation from medically assisted reproductive treatments, even in those having a favorable diagnosis.[44,45,46]
With these considerations, the present research was planned to explore the role of illness cognitions in distressed couples with infertility as there have been limited studies highlighting the importance of such an exploration. In addition, the rationale of this study was to compare men and women on their illness perceptions as these can serve as vital agents for planning psychological interventions for them. The aim of this study was to compare the infertile men and women undergoing fertility treatments on levels of experienced helplessness, acceptance, perceived benefits, anxiety, and depression.
MATERIALS AND METHODS
Study participants
This study is conducted during July 2013–August 2014 and is a part of a larger project which on the effectiveness of psychotherapy for distressed couples with infertility. The principal investigator screened 181 couples for inclusion in the larger project of which a pool of 81 couples was enrolled in this particular investigation using purposive sampling. The participants were screened using fertility problem inventory (FPI)[47] and Mini International Neuropsychiatric Interview (MINI Version 5.00).[48]
Inclusion criteria for this study
Both husband and wife being highly distressed due to infertility (raw score of 167 or above on FPI as assessed in females and of 147 or above on FPI as assessed in males[47]). None of them met any criteria for major psychiatric illness (as assessed by MINI).
Excluded participants
Couples who were nondistressed or moderately distressed (44 in number) or nonwilling to participate (50 in number) were excluded from the study. Further, six of 181 couples originally screened were excluded from research as they were found to be suffering from a major psychiatric illness, and thus referred to Department of Psychiatry for careful clinical management.
Ethical statement
This study was conducted after its review and clearance by the Institutional Ethics Committee. An informed written consent was taken by the participants before the conduct of this work and the rights of information, confidentiality, and withdrawal from the study was reserved. All ethical guidelines (in accordance with the Declaration of Helsinki) were followed while the conduct of this work.
Data collection
The study participants were administered the Kuppuswamy's revised socioeconomic scale for collecting sociodemographic information.[49] Clinical details were collected using a structured interview schedule devised by the investigator. Finally, the psychological questionnaires were administered to them. These included the Hamilton anxiety and depression scales,[50,51] and the “Illness Cognition Questionnaire (ICQ)”[52] administered by men and women.
Description of the psychological measures
The Hamilton scales are clinician-rated gold standard scales for assessing psychic anxiety and depressive features, respectively. For the Hamilton anxiety scale, the preestablished cutoff score is 17 which indicate mild severity. The internal consistency reliability ranges from 0.77 to 0.81 and test-retest reliability is 0.96. This scale also shows good construct validity and factorial validity and showing statistically significant relationships with self-report measures of anxiety variables for adults. The internal consistency reliability of different versions of Hamilton depression scale ranges from 0.48 to 0.92, and inter-rater reliability is 0.60 for the 21-item scale. The validity of Hamilton depression scale is reported to be ranging from 0.65 to 0.90 with Montgomery–Asberg depression scale. For the Hamilton depression scale, the preestablished cutoff score is eight. The ICQ[52] assesses cognitions such as helplessness, acceptance, and benefits perceived by patients with chronic medical diseases. The original version of this questionnaire was administered in this study. The principal investigator assisted the participants in understanding and answering the questionnaire within the context of infertility. This measure has a preestablished cutoff for helplessness as 14. Cronbach's alpha of this scale ranges from 0.84 to 0.91, and test-retest reliability is 0.67. Evidence has also been found for its good concurrent and predictive validity.
Statistical analysis
Data are entered and analyzed using SPSS (version 15, September 2007, SPSS Inc., Chicago, IL, USA). The descriptive data analysis is performed using means, medians, quartiles, frequencies, and percentages. The paired sample t-test is performed for assessing the significance of the difference between men (husbands) and women (wives) on infertility specific stress, anxiety, depression, cognitions of helplessness, and cognitions of acceptance. The Wilcoxon signed-rank test is carried out for assessing the significance of the difference in medians obtained in men and women on perceived benefits since this variable was found to be skewed. The value of P < 0.05 is considered as statistically significant.
RESULTS
Table 1 presents the results of descriptive data analysis. The table shows that the study participants were middle-aged couples, most of which were educated up to high school. The medians for the duration of infertility were 4 years. The median for the duration of fertility treatment is 3 years, within which 43% had a history of undergoing 6–8 cycles of ovulation induction (OI) treatments and 58% had histories of unsuccessful intrauterine inseminations (IUIs). 28% of the participants were diagnosed with combined factor infertility.
Table 1.
Descriptive data
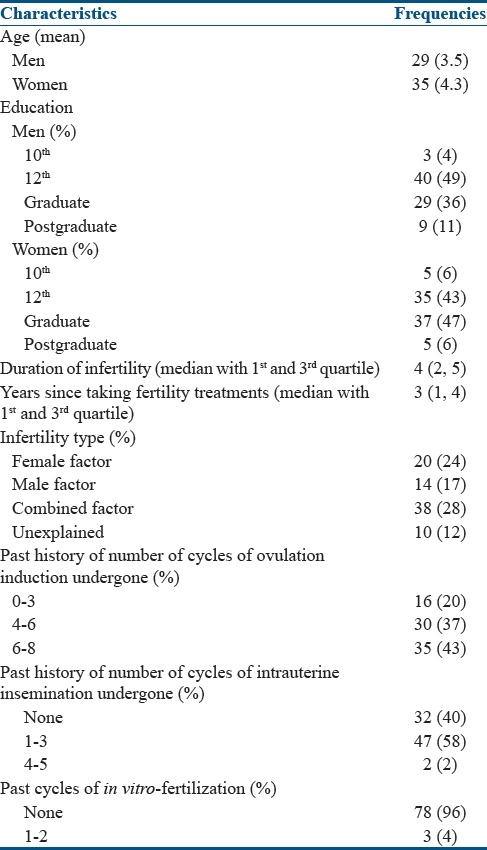
Table 2 presents the results for paired sample t-test carried out for assessing the significance of the difference between men and women on infertility specific stress. Data reveals that women report greater stress, anxiety, and depressive features in comparison to the men. Furthermore, helplessness is higher in women than in men. In comparison to men, the women report lower acceptance of their fertility struggles and the status of “being infertile as a couple.”
Table 2.
Paired sample t-test for the significance of difference between male and female partners on infertility specific stress
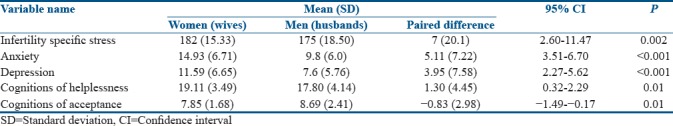
Table 3 presents the results for the difference in medians obtained in men and women on perceived benefits. Table 3 shows no differences in scores obtained among men and women, and thus data on this variable were not subjected to any further statistical analysis. Furthermore, low scores on this measure reflect that neither men nor the women perceived that being infertile has benefitted them in any manner.
Table 3.
Significance of median differences between men and women on perceived benefits
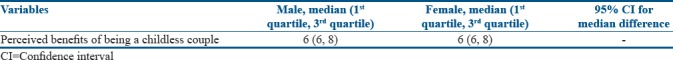
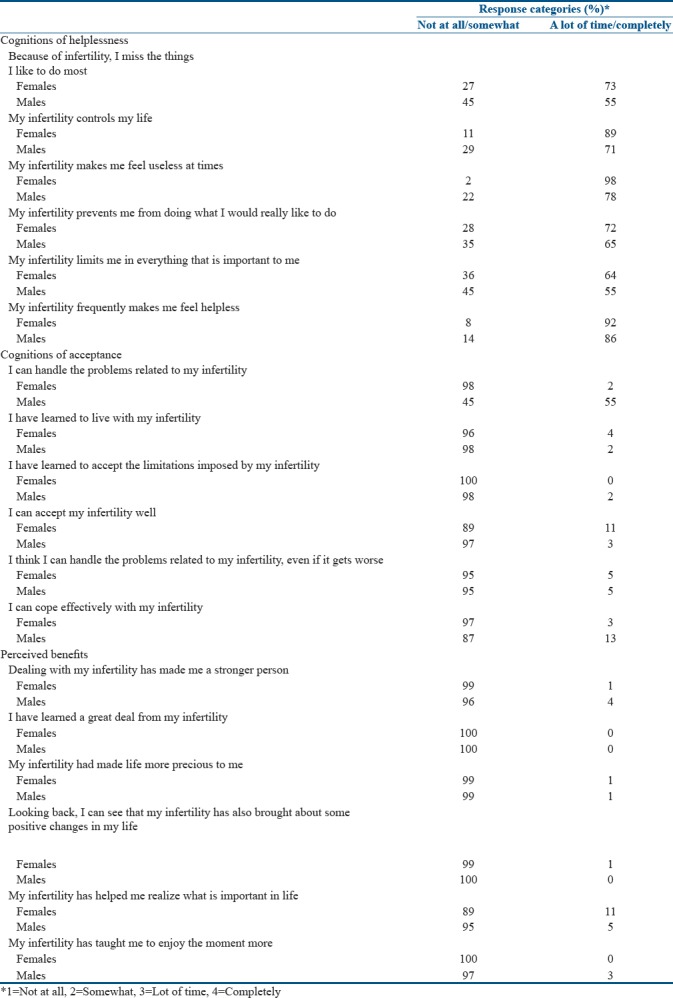
Table 4 presents item-wise frequency counts given by the participants on various questions of the ICQ.
Table 4.
Item-wise frequency counts on various questions of the illness cognition questionnaire answered by infertile females and males
DISCUSSION
This study aims to investigate the presence of illness cognitions in distressed couples undergoing fertility treatments and compare the men (husbands) and women (wives) on domains of anxiety, depression, helplessness, acceptance, and perceived benefits.
The results of the present investigation depict that infertile women report more distress while taking fertility treatments than the infertile men. Within the couple as a dyad, husband and wife differ clinically and statistically on levels of stress, anxiety, and depression. Furthermore, women have subclinical levels of anxiety and mild depressive features. Whereas, the men report subclinical levels of both anxiety and depression. These facts clearly suggest that the emotional strain is more on the women in comparison to their husbands, and that the men are indirectly affected by treatment-related stressors. Men suffer more in the context of their wife's distress in context of their wife's suffering.[24] These findings are in coherence with other studies.[53,54,55,56]
A comparison of the profile of cognitions associated with infertility depicts that women report helplessness more often than the men. Fifty-two percentage of the female participants in this study said that infertility makes them feel helpless, whereas 43% of men reported the same. Data of this exploration also shows that one in every two women and one in every three men undergoing IUI feel that infertility regimens have taken over their normal daily routines. Furthermore, both men and women equally felt a sense of personal inadequacy. In the verbatim interviews with patient's helplessness is reported within the context of “failed attempts at conceptions in nature cycles,” “uncertainties related to success of treatments,” their outcomes (endless attempts, physical side-effects, and normality of the child conceived), and “the frustrated wish for a child.” Patients report that “trying hard is not enough; one needs good fortune, money, and patience too.” Similar outcomes have also been reported by other investigations.[28,30,57]
Acceptance is another key cognition that is closely related to coping patterns, and was thus explored in this study. Acceptance refers to the acknowledgment and assent to a negative situation that helps individuals appraise stressors in a realistic and effective manner. Acceptance of the diagnosis and of involuntary childlessness on the whole is found to be lower in women than men. This finding was in conjunction with other studies,[36,37] which urge that patients with a history of moderate treatment failure in OI and IUI (<4 cycles per year) tend to hope for the success of pregnancy either spontaneously or with more aggressive treatments. Patients go on to explain that “they have not given up on their faith in God.” Most of them adhere to the belief that “as of now they may be childless, but one day they shall be blessed with a baby.”
In addition, 67% of the women, whereas 43% of men reported that they cannot handle the consequences of infertility. These include the decisions of how much treatment is needed, high financial cost of repeated cycles, distressing investigations (Trans-vaginal USG and Semen tests), interpersonal conflicts due to demeaning remarks and intrusive questioning of family members, in-laws, peers, and the sociocultural bias held against them. About 10% of the participants have made attempts to adjust to a child-free lifestyle and accept limitations associated with subfertility by moving on to their career goals. These patients report that “they have tried as much as they could and find it too much to tolerate. For the time being, they have decided to try one last time and then take a break from treatments by focusing on other things in life.”
The present study reveals that one in every eight women and one in every five men report of having coping problems. A small number and barely 5% of study participants, irrespective of gender report that they would be able to deal and handle their issues even if their conception difficulties worsened. Coping issues were predominantly related to “maintaining emotional stability, composure, tackling the identity crisis, sexual interest, and pleasure; marital well-being, handling unsolicited questioning by others, difficulty in guarding their private matters, protecting oneself from social politicization of reproductive loss and sexual inadequacy; and guarding oneself from magic-religious social beliefs and cures, stigma, social alienation, and exclusion.”
A comparison of the profile on the measure of perceived benefits reveals no differences in men and women. A large number of participants report coping problems in this study. Nearly, all men and women (90% of them) felt that they did not emerge as a stronger person after facing and coping with infertility crisis. In addition to this, 99%, i. e., 80 couples who participated in the research reported that infertility did not bring about any positive change in their life. These results are supported by previous investigations conducted in India, that brings forth the relevance of psychosocial counseling for not only the distressed women but also for the men in Indian setups.[15,16,20]
This study highlights certain glaring psychological issues faced by infertile couples coming for treatments. The present study purports that high distress coupled with helplessness and low acceptance in infertile women makes them exceedingly vulnerable. This may places the women (wives) more at risk of deteriorating mental illness than their better halves. Theoretically, low acceptance also makes the women more likely to experience unresolved grief.[34]
Powerlessness over the infertility situation may also be attributed to an inability to embrace events the way “as they are” and recreate life around other meaningful life goals. The constant struggle for “being someone else or having some other kind of life” increases the dissatisfaction from present living and sense of self.[58] Studies reveal that in extreme cases of infertility distress, the person moves toward an unhealthy wish for a child wherein he/she experiences massive pressures for conception, demands a child at any cost, feels that having a child is the only success in their lives, and insists for repeated invasive high-risk treatments.[59] Whereas, in the same situation, a healthy wish for a child reflects true psychological acceptance which can be transformative. A “healthy wish for a child” is when couples perceive moderate pressures for conception, express hesitancy for invasive treatments, and in the case of renunciation of the wish, these couples experience distress but at the same time they tend to readjust toward a power-balanced doctor–patient relationship.[59] When true acceptance permeates through one's mind, it makes radical changes in the way patients perceive and cope with their problems.[60,61] This does not denote that one has to “swallow the hard truth or the worst possible outcome.” Rather, it means that the patients can deal with the low-control situations by developing an ability to “take reality for what it is,” having a realistic hope, regulate emotions, find workable solutions toward solvable aspects, and develop resilience toward unsolvable issues related to their infertility experience.[60,61] Often this has been referred to as “radical acceptance,” and this has been known to set individuals free from any trauma, be it physical or psychological.[61] Research suggests that such approach-oriented ways of coping (including a balance between problem-solving, emotional processing, and expression) are related to psychological well-being.[14,24,58,62,63,64,65] This relates to a coping pattern in which one becomes mindfully aware of life, tries to slow down, and resonate with enjoyable moments of life, rather than rush from one thing to the next. The idea is to apply tenets of positive psychology by replacing learnt helplessness with learnt optimism even in times of high distress since negative appraisals are inversely related to psychosocial well-being.[31,34,65,66] Thus, psychosocial management of infertile patients should focus on effective stress management and cognitive behavioral coping as these predict infertility distress at all levels of fertility treatments.[67] In this light, literature also supports that cognitive behavior therapy approaches can be applied as these effectively focus on positive reappraisals, reduce helplessness, and depression in infertility.[68,69,70,71,72]
Psychologists postulate that “that chronicity of a disease effects personal distress, coping, and depression rather than the mere diagnosis of it.”[10] Comparative research on the psychological impact of infertility and other medical conditions reveals that infertility specific distress has serious consequences. It is comparable to the distress experienced in chronic medical conditions such as cancer, hypertension, and cardiac diseases but it is less severe to that experienced in chronic pain and HIV.[73] It is also believed that “internal, stable, and controllable cognitive attributions” to one's medical condition is associated with positive psychological adjustment and coping. Psychological avoidance and resistance are correlated with uncertainty, thus impeding the functional impairment in chronic medical conditions.[74] Accordingly, further studies may expand the scope of the present work by investigating the differences in illness cognitions and psychological morbidity in infertility versus other chronic medical conditions using a multiple comparison-group design.
The limitations of this research are that it was an uncontrolled trial and captured selective information and specific cognitive variables related to distress in infertile couples. Moreover, cultural-specific elements of illness beliefs may have been missed in our cross-sectional research as the English version of original ICQ was used. The future studies can plan to implement a qualitative investigation to understand the “disease identity” of infertile patients in the Indian scenario. Yet, the restricted findings of this study are valuable as it became a foreground for developing psychotherapy module for managing distress in couples with infertility at the study site.
CONCLUSION
Human minds are active and effective problem solvers. The psychological model of coping suggests that illness cognitions predict emotional well-being and health behaviors. Thus, coping with infertility is crucially important during treatment times, particularly when the conception related stressors begin to elude one's health.
The findings from this study suggest that when examining intracouple dynamics, the women (wives) report greater distress, anxiety, and depressive symptoms than the men (husbands). In men, subclinical depressive and anxiety features are more common. Coping problems are found in both partners of the couple. Helplessness and poor acceptance are more in women than men. Within Indian setups, neither men nor women believe that infertility benefits them in any way. All of these psychological factors may contribute to higher treatment burden in patients seeking assisted conception. Thus, psychosocial care for couples plays a centrally important role and should be integrated within the conventional treatment pathway.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would also like to convey our gratitude to Dr. BS Patel for help with proof-reading this article.
REFERENCES
- 1.Neisser U. Cognitive Psychology. Englewood Cliffs. NJ: Prentice-Hall; 1967. [Google Scholar]
- 2.Leventhal H, Meyer D, Nerenz D. The Common-Sense Representation of Illness Danger. In: Rachman S, editor. Contributions to Medical Psychology. Vol. 2. New York: Pergamon Press; 1980. pp. 7–30. [Google Scholar]
- 3.Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health, and behavior: A perceptual-cognitive approach. Psychol Health. 1998;13:717–33. [Google Scholar]
- 4.Leventhal H, Diefenbach M, Leventhal EA. Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cogn Ther Res. 1992;16:143–63. [Google Scholar]
- 5.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 6.Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychol Health. 2003;18:141–84. [Google Scholar]
- 7.Weinman J, Petrie KJ, Moss-Morris R, Horne R. The illness perception questionnaire: A new method for assessing illness perceptions. Psychol Health. 1996;11:431–46. [Google Scholar]
- 8.Kaptein AA, Scharloo M, Fischer MJ, Snoei L, Cameron LD, Sont JK, et al. Illness perceptions and COPD: An emerging field for COPD patient management. J Asthma. 2008;45:625–9. doi: 10.1080/02770900802127048. [DOI] [PubMed] [Google Scholar]
- 9.Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: The role of message framing. Psychol Bull. 1997;121:3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- 10.Turner J, Kelly B. Emotional dimensions of chronic disease. West J Med. 2000;172:124–8. doi: 10.1136/ewjm.172.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mabasa LF. Sociocultural aspects of infertility in a Black South African community. [Last accessed on 2017 Aug 17];Psychol Afr. 2002 12:65–79. Available from: http://www.search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2002-15798-005&site=ehost-live . [Google Scholar]
- 12.Berg BJ, Wilson JF. Psychological functioning across stages of treatment for infertility. J Behav Med. 1991;14:11–26. doi: 10.1007/BF00844765. [DOI] [PubMed] [Google Scholar]
- 13.Greil AL. Infertility and psychological distress: A critical review of the literature. Soc Sci Med. 1997;45:1679–704. doi: 10.1016/s0277-9536(97)00102-0. [DOI] [PubMed] [Google Scholar]
- 14.Stanton AL, Dunkel-Schetter C, editors. Plenum Publishing Cooperation. New York: Springer Science & Business Media; 2013. Infertility: Perspectives from Stress and Coping Research. [Google Scholar]
- 15.Patel A, Sharma PS, Narayan P, Nair BV, Narayanakurup D, Pai PJ, et al. Distress in infertile males in Manipal-India: A clinic based study. J Reprod Infertil. 2016;17:213–20. [PMC free article] [PubMed] [Google Scholar]
- 16.Patel A, Sharma PS, Narayan P, Binu VS, Dinesh N, Pai PJ, et al. Prevalence and predictors of infertility-specific stress in women diagnosed with primary infertility: A clinic-based study. J Hum Reprod Sci. 2016;9:28–34. doi: 10.4103/0974-1208.178630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benyamini Y, Gozlan M, Kokia E. On the self-regulation of a health threat: Cognitions, coping, and emotions among women undergoing treatment for infertility. Cogn Ther Res. 2004;28:577–92. [Google Scholar]
- 18.Chang SN, Mu PF. Infertile couples' experience of family stress while women are hospitalized for ovarian hyperstimulation syndrome during infertility treatment. J Clin Nurs. 2008;17:531–8. doi: 10.1111/j.1365-2702.2006.01801.x. [DOI] [PubMed] [Google Scholar]
- 19.Gonzalez LO. Infertility as a transformational process: A framework for psychotherapeutic support of infertile women. Issues Ment Health Nurs. 2000;21:619–33. doi: 10.1080/01612840050110317. [DOI] [PubMed] [Google Scholar]
- 20.Widge A. Seeking conception: Experiences of urban Indian women with in vitro fertilisation. Patient Educ Couns. 2005;59:226–33. doi: 10.1016/j.pec.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 21.Phipps SA. A phenomenological study of couples' infertility: Gender influence. Holist Nurs Pract. 1993;7:44–56. doi: 10.1097/00004650-199301000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Pook M, Krause W, Röhrle B. Coping with infertility: Distress and changes in sperm quality. Hum Reprod. 1999;14:1487–92. doi: 10.1093/humrep/14.6.1487. [DOI] [PubMed] [Google Scholar]
- 23.Dunkel-Schetter C, Stanton AL. Infertility. US: Springer; 1991. Psychological adjustment to infertility; pp. 197–222. [Google Scholar]
- 24.Stanton AL, Tennen H, Affleck G, Mendola R. Coping and adjustment to infertility. J Soc Clin Psychol. 1992;11:1–3. doi: 10.1300/J013v17n03_01. [DOI] [PubMed] [Google Scholar]
- 25.Thompson SC. Will it hurt less if i can control it? A complex answer to a simple question. Psychol Bull. 1981;90:89–101. [PubMed] [Google Scholar]
- 26.Cwikel J, Gidron Y, Sheiner E. Psychological interactions with infertility among women. Eur J Obstet Gynecol Reprod Biol. 2004;117:126–31. doi: 10.1016/j.ejogrb.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 27.Yaǧmur Y, Oltuluoǧlu H. Social support and hopelessness in women undergoing infertility treatment in Eastern Turkey. Public Health Nurs. 2012;29:99–104. doi: 10.1111/j.1525-1446.2011.00976.x. [DOI] [PubMed] [Google Scholar]
- 28.Hasanpoor-Azghdy SB, Simbar M, Vedadhir A. The emotional-psychological consequences of infertility among infertile women seeking treatment: Results of a qualitative study. Iran J Reprod Med. 2014;12:131–8. [PMC free article] [PubMed] [Google Scholar]
- 29.Baram D, Tourtelot E, Muechler E, Huang KE. Psychosocial adjustment following unsuccessful in vitro fertilization. J Psychosom Obstet Gynaecol. 1988;9:181–90. [Google Scholar]
- 30.Verhaak CM, Smeenk JM, Evers AW, van Minnen A, Kremer JA, Kraaimaat FW, et al. Predicting emotional response to unsuccessful fertility treatment: A prospective study. J Behav Med. 2005;28:181–90. doi: 10.1007/s10865-005-3667-0. [DOI] [PubMed] [Google Scholar]
- 31.Rockliff HE, Lightman SL, Rhidian E, Buchanan H, Gordon U, Vedhara K, et al. A systematic review of psychosocial factors associated with emotional adjustment in in vitro fertilization patients. Hum Reprod Update. 2014;20:594–613. doi: 10.1093/humupd/dmu010. [DOI] [PubMed] [Google Scholar]
- 32.Boivin J, Sanders K, Schmidt L. Age and social position moderate the effect of stress on fertility. Evol Human Behav. 2006;27:345–56. [Google Scholar]
- 33.van Rooij FB, Van Balen F, Hermanns JM. Emotional distress and infertility: Turkish migrant couples compared to Dutch couples and couples in Western Turkey. J Psychosom Obstet Gynaecol. 2007;28:87–95. doi: 10.1080/01674820701410015. [DOI] [PubMed] [Google Scholar]
- 34.Seligman ME. A series of books in psychology. New York, NY: WH Freeman/Times Books/Henry Holt & Co; 1975. Helplessness: On depression, development, and death. [Google Scholar]
- 35.Nolen-Hoeksema S, Girgus JS, Seligman ME. Learned helplessness in children: A longitudinal study of depression, achievement, and explanatory style. J Pers Soc Psychol. 1986;51:435–42. doi: 10.1037//0022-3514.51.2.435. [DOI] [PubMed] [Google Scholar]
- 36.Boivin J, Takefman JE, Tulandi T, Brender W. Reactions to infertility based on extent of treatment failure. Fertil Steril. 1995;63:801–7. [PubMed] [Google Scholar]
- 37.Peddie VL, van Teijlingen E, Bhattacharya S. A qualitative study of women's decision-making at the end of IVF treatment. Hum Reprod. 2005;20:1944–51. doi: 10.1093/humrep/deh857. [DOI] [PubMed] [Google Scholar]
- 38.Berger GS, Goldstein M, Fuerst M. The Couple's Guide to Fertility: Entirely Revised and Updated with the Newest Scientific Techniques to Help You Have a Baby. New York: Broadway Books; 2001. [Google Scholar]
- 39.Abbey A, Andrews FM, Halman LJ. Gender's role in responses to infertility. Psychol Women Q. 1991;15:295–316. [Google Scholar]
- 40.Austenfeld JL, Stanton AL. Coping through emotional approach: A new look at emotion, coping, and health-related outcomes. J Pers. 2004;72:1335–63. doi: 10.1111/j.1467-6494.2004.00299.x. [DOI] [PubMed] [Google Scholar]
- 41.Schmidt L, Holstein BE, Christensen U, Boivin J. Communication and coping as predictors of fertility problem stress: Cohort study of 816 participants who did not achieve a delivery after 12 months of fertility treatment. Hum Reprod. 2005;20:3248–56. doi: 10.1093/humrep/dei193. [DOI] [PubMed] [Google Scholar]
- 42.Jordan C, Revenson TA. Gender differences in coping with infertility: A meta-analysis. J Behav Med. 1999;22:341–58. doi: 10.1023/a:1018774019232. [DOI] [PubMed] [Google Scholar]
- 43.Domar AD. Impact of psychological factors on dropout rates in insured infertility patients. Fertil Steril. 2004;81:271–3. doi: 10.1016/j.fertnstert.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 44.Gameiro S, Boivin J, Peronace L, Verhaak CM. Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Hum Reprod Update. 2012;18:652–69. doi: 10.1093/humupd/dms031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Campagne DM. Should fertilization treatment start with reducing stress? Hum Reprod. 2006;21:1651–8. doi: 10.1093/humrep/del078. [DOI] [PubMed] [Google Scholar]
- 46.Brandes M, van der Steen JO, Bokdam SB, Hamilton CJ, de Bruin JP, Nelen WL, et al. When and why do subfertile couples discontinue their fertility care? A longitudinal cohort study in a secondary care subfertility population. Hum Reprod. 2009;24:3127–35. doi: 10.1093/humrep/dep340. [DOI] [PubMed] [Google Scholar]
- 47.Newton CR, Sherrard W, Glavac I. The fertility problem inventory: Measuring perceived infertility-related stress. Fertil Steril. 1999;72:54–62. doi: 10.1016/s0015-0282(99)00164-8. [DOI] [PubMed] [Google Scholar]
- 48.Sheehan DV, Lecrubier Y, Sheehan KH, Janavs J, Weiller E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12:232–41. [Google Scholar]
- 49.Kumar BR, Dudala SR, Rao AR. Kuppuswamy's socio-economic status scale – A revision of economic parameter for 2012. Int J Res Dev Health. 2013;1:2–4. [Google Scholar]
- 50.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 51.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Evers AW, Kraaimaat FW, van Lankveld W, Jongen PJ, Jacobs JW, Bijlsma JW, et al. Beyond unfavorable thinking: The illness cognition questionnaire for chronic diseases. J Consult Clin Psychol. 2001;69:1026–36. [PubMed] [Google Scholar]
- 53.Thara R, Ramachandran V, Hassan PP. Psychological aspects of infertility. Indian J Psychiatry. 1986;28:329–34. [PMC free article] [PubMed] [Google Scholar]
- 54.Guerra D, Llobera A, Veiga A, Barri PN. Psychiatric morbidity in couples attending a fertility service. Hum Reprod. 1998;13:1733–6. doi: 10.1093/humrep/13.6.1733. [DOI] [PubMed] [Google Scholar]
- 55.Joshi HL, Singh R, Bindu M. Psychological distress, coping and subjective wellbeing among infertile women. J Indian Acad Appl Psychol. 2009;35:329–36. [Google Scholar]
- 56.Pottinger AM, McKenzie C, Fredericks J, DaCosta V, Wynter S, Everett D, et al. Gender differences in coping with infertility among couples undergoing counselling for in vitro fertilization treatment. West Indian Med J. 2006;55:237–42. doi: 10.1590/s0043-31442006000400007. [DOI] [PubMed] [Google Scholar]
- 57.Jin X, Wang G, Liu S, Zhang J, Zeng F, Qiu Y, et al. Survey of the situation of infertile women seeking in vitro fertilization treatment in china. Biomed Res Int 2013. 2013:179098. doi: 10.1155/2013/179098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hynes GJ, Callan VJ, Terry DJ, Gallois C. The psychological well-being of infertile women after a failed IVF attempt: The effects of coping. Psychol Psychother. 1992;65:269–78. doi: 10.1111/j.2044-8341.1992.tb01707.x. [DOI] [PubMed] [Google Scholar]
- 59.Insler V, Lunenfeld B, editors. Infertility: Male and Female. New York: Churchill Livingstone; 1993. [Google Scholar]
- 60.Strosahl KD, Robinson PJ, Gustavsson T. Brief Interventions for Radical Change: Principles and Practice of Focused Acceptance and Commitment Therapy. Oakland, CA: New Harbinger Publications; 2012. [Google Scholar]
- 61.Brach T. Bantam. New York, NY: Bantam; 2003. Radical Acceptance: Embracing your Life with the Heart of a Buddha. [Google Scholar]
- 62.Litt MD, Tennen H, Affleck G, Klock S. Coping and cognitive factors in adaptation to in vitro fertilization failure. J Behav Med. 1992;15:171–87. doi: 10.1007/BF00848324. [DOI] [PubMed] [Google Scholar]
- 63.Verhaak CM. Emotional Impact of Unsuccessful Fertility Treatment in Women. 2003. [Last assessed on 2017 Jul 07]. Available from: http://repository.ubn.ru.nl/bitstream/handle/2066/19378/19378%20_emotimofu.pdf?sequence=1 .
- 64.Berghuis JP, Stanton AL. Adjustment to a dyadic stressor: A longitudinal study of coping and depressive symptoms in infertile couples over an insemination attempt. J Consult Clin Psychol. 2002;70:433–8. doi: 10.1037//0022-006x.70.2.433. [DOI] [PubMed] [Google Scholar]
- 65.van den Akker OB. Coping, quality of life and psychological symptoms in three groups of sub-fertile women. Patient Educ Couns. 2005;57:183–9. doi: 10.1016/j.pec.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 66.Seligmann ME. Learned optimism: How to change your mind and your life. New York, NY: Knopf; 1991. [Google Scholar]
- 67.Gameiro S, Boivin J, Dancet E, de Klerk C, Emery M, Lewis-Jones C, et al. ESHRE guideline: Routine psychosocial care in infertility and medically assisted reproduction-a guide for fertility staff. Hum Reprod. 2015;30:2476–85. doi: 10.1093/humrep/dev177. [DOI] [PubMed] [Google Scholar]
- 68.Tuschen-Caffier B, Florin I, Krause W, Pook M. Cognitive-behavioral therapy for idiopathic infertile couples. Psychother Psychosom. 1999;68:15–21. doi: 10.1159/000012305. [DOI] [PubMed] [Google Scholar]
- 69.Hunt J, Monach JH. Beyond the bereavement model: The significance of depression for infertility counselling. Human reproduction (Oxford, England) 1997;12(11 Suppl):188–94. [PubMed] [Google Scholar]
- 70.Miles LM, Keitel M, Jackson M, Harris A, Licciardi F. Predictors of distress in women being treated for infertility. J Reprod Infant Psychol. 2009;27:238–57. [Google Scholar]
- 71.Stanton AL, Tennen H, Affleck G, Mendola R. Cognitive appraisal and adjustment to infertility. Women Health. 1991;17:1–5. doi: 10.1300/J013v17n03_01. [DOI] [PubMed] [Google Scholar]
- 72.Patel A, Dinesh N, Sharma PS, Kumar P, Binu VS. Outcomes of structured psychotherapy for emotional adjustment in a childless couple diagnosed with recurrent pregnancy loss: A unique investigation. J Hum Reprod Sci. 2018;11:202–7. doi: 10.4103/jhrs.JHRS_127_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Domar AD, Zuttermeister PC, Friedman R. The psychological impact of infertility: A comparison with patients with other medical conditions. J Psychosom Obstet Gynaecol. 1993;14(Suppl 14):45–52. [PubMed] [Google Scholar]
- 74.Roesch SC, Weiner B. A meta-analytic review of coping with illness: Do causal attributions matter? J Psychosom Res. 2001;50:205–19. doi: 10.1016/s0022-3999(01)00188-x. [DOI] [PubMed] [Google Scholar]


