Abstract
Background
Depression is the most prevalent psychiatric disorder among people living with HIV (PLWHIV) and is associated with poor quality of life, additional comorbidities, disability, unemployment, poorer therapeutic outcomes and risky behaviors. The present systematic review and meta-analysis aims to systematically summarize empirical evidence and to formulate recommendations for future research.
Methods
We searched PubMed, EMBASE, SCOPUS, and relevant literature for possible studies to include. A qualitative and quantitative analysis was undertaken for this systematic review. Subgroup and sensitivity analysis were performed. Cochran's Q- and the I2 test were used to assess heterogeneity. The presence of publication bias was evaluated by using Egger's test and visual inspection of the symmetry in funnel plots.
Results
Of 283 titles initially identified, 81 abstracts were eligible for review. Of these, 46 articles qualified for full text review and 19 were retained. In our meta-analysis the pooled prevalence of depression in PLWHIV was 38% (95% CI 29.30-47.54). The pooled prevalence estimates of depression was 49.79% in Ethiopia and 30.88% in Uganda. In addition, the prevalence of depression was 12.40% and 46% as measured by diagnostic and screening instrument respectively. Our qualitative synthesis showed that factors such as having opportunistic infection, perceived stigma, negative life event, WHO clinical staging of disease, hospitalization in the past one month, stressful life events, food insecurity, self-efficacy, missed frequency of clinic visit, frequency of follow-up, older age, low income, urban residence and being government employee were strongly and significantly associated with depression in PLWHIV in east Africa.
Conclusion
The pooled prevalence estimates of prevalence of depression in PLWHIV was 38%. The prevalence estimates of depression in PLWHIV in Ethiopia was significantly higher than Uganda. In addition the prevalence of depression was significantly higher in studies conducted by screening than diagnostic instrument. Routine screening and integrated management of depression into the existing HIV care services is warranted. Validation and use of standard instrument to assess depression in PLWHIV is needed. Moreover, longitudinal and community based studies focusing on incidence and determinates of depression in PLWHIV are recommended.
Electronic supplementary material
The online version of this article (10.1186/s12888-018-1835-3) contains supplementary material, which is available to authorized users.
Keywords: Prevalence, HIV, AIDS, Determinants, Factors, Depression, Systematic review, Meta-analysis, East Africa
Background
Depression is the most prevalent psychiatric disorder among people living with HIV (PLWHIV) and is associated with poorer therapeutic outcomes and risky behaviors. Different epidemiological studies have estimated the prevalence of depression in PLWHIVto be between 2.27% and 76.7% [1–20]. In fact, it is one of the leading causes of morbidity and mortality among PLWHIV [21].
In the past decades, studies have determined the prevalence of depression in PLWHIV. However, the overall prevalence rate of depression in PLWHIV remains unclear in east Africa; previous studies reported prevalence rates between 2.7% and 76.7% [1–20]. Several factors may contribute to this wide range of prevalence rates, including: (i) differences between included PLWHIV with respect to the stages of HIV disease, treatment status and CD4 level (ii) the use of different instruments to assess depression with different psychometric properties; and (iii) the use of different criteria to define depression [22].
Depression is the most commonly experienced psychological conditions experienced by PLWHIV and is associated with poor quality of life [23], additional comorbidities [24], disability, and unemployment [25–27]. In addition, depression in PLWHV leads poor social conditions, poor treatment adherence and, poor therapeutic outcomes, and risky behaviors [28–31].
A number of factors can predispose PLWHIV to depression including, having opportunistic infection [9, 10], perceived stigma [2], negative life event [26], having severe WHO clinical stage diseases [2, 9, 10], stressful life events [26], food insecurity [9], older age [17], low income [3] and advanced HIV disease [22].
Evidence shows that east Africa is the region most affected by HIV in the world next to south Africa [32]. However, the there are no systematic review and meta-analysis studies conducted on the epidemiology of depression in PLWHIV in east Africa. Therefore, the main objective of this systematic review and meta-analysis is to summarize the available empirical evidence in east Africa on: [1] the prevalence of depression in people living with HIV (PLWHIV) and [2] the determinants of depressionin PLWHIV and to formulate recommendations for future clinical practice and research.
Methods/design
We conducted extensive search of literature as indicated in the guideline of reporting systematic review and meta-analysis (PRISMA) [32]. Three databases such as PubMed, Embase, and Scopus were consulted for our literature search. We conducted our search in Pubmed using the following terms and keywords: "Epidemiology OR prevalence OR magnitude OR incidence AND depression OR depressive symptoms OR depressive disorder OR depressive AND HIV OR human immunodeficiency virus OR AIDS AND factor OR risk OR risk factor OR determinant AND Ethiopia OR Eritrea OR Kenya OR Uganda OR Tanzania OR Sudan OR Djibouti OR Somalia OR Rwanda OR east Africa". For the other two databases (Embase and Scopus) we employed specific-subjects headings as advised for each databases. In addition, in order to identify other relevant articles we manually searched the reference lists of eligible articles.
Eligibility criteria
Two reviewers (GA and MA) evaluated the relevant articles using their title and abstracts prior to retrieval of full-text articles. The retrieved full-text articles were further screened according to pre-specified inclusion and exclusion criteria. We resolved disagreements by discussing with a third reviewer (MS).
Inclusion criteria
Design type -Cross sectional and other observational studies
Study subject– people living with HIV
Articles published in English language
Studies which reported magnitude of depression in PLWHIV
Articles that assessed risk factors of depression in PLWHIV
Studies done in east Africa
Exclusion criteria
We excluded commentaries, editorials, letters, reviews, and interventional studies
Duplicate studies were also excluded
Methods for data extraction and quality assessment
We used standardized data extraction form to extract data from identified studies. The following information were extracted for each included study: The name of the first author, publication date, study design, associated factors, sample size study setting, tools used for assessing outcome, confounders adjusted for, risk estimate (OR) and their 95% confidence interval. Data extraction from source documents was done independently by two investigators. Disagreements were resolved by consensus.
The quality of included studies was evaluated by using a modified version of the Newcastle-Ottawa Scale (NOS) [33]. Sample representativeness and size, comparability between participants, ascertainment of depressive symptoms, and statistical quality were the domains NOS scale uses to assess the quality of each studies. Actual agreement and agreement beyond chance (unweighted Kappa) were used to evaluate the agreement between the two reviewers. We considered the values 0 as poor agreement, 0.01–0.20 as slight agreement, 0.21– 0.40 as fair agreement, 0.41–0.60 = moderate agreement, 0.61– 0.80 as substantial agreement, and 0.81–1.00 as almost perfect agreement [34].
Data synthesis and analysis
Comprehensive meta-analysis software version3 was used for meta-analysis and forest plots that showed combined estimates with 95%CI. The overall pooled prevalence was estimated by random effect meta-analysis [35]. Heterogeneity was evaluated using Q statistic and the I2statistics [35]. The magnitude of statistical heterogeneity between studies was assessed using I2 statistic and values of 25, 50 and 75% were considered to represent low, medium and high, respectively [36]. For the data identified as heterogeneous, a random-effects model was used during analysis. When statistical pooling is not possible, non-pooled data was presented in table form. Meta-regression was performed to explore the potential source of heterogeneity.
The instrument used to assess depression and the country where the studies were conducted were used to determine the possible source of heterogeneity between the studies. In addition, we carried out a leave-one-out sensitivity analysis to evaluate the key studies that exert major impact on between-study heterogeneity. Publication bias was assessed by funnel plot and Egger’s regression tests
Results
Identification of studies
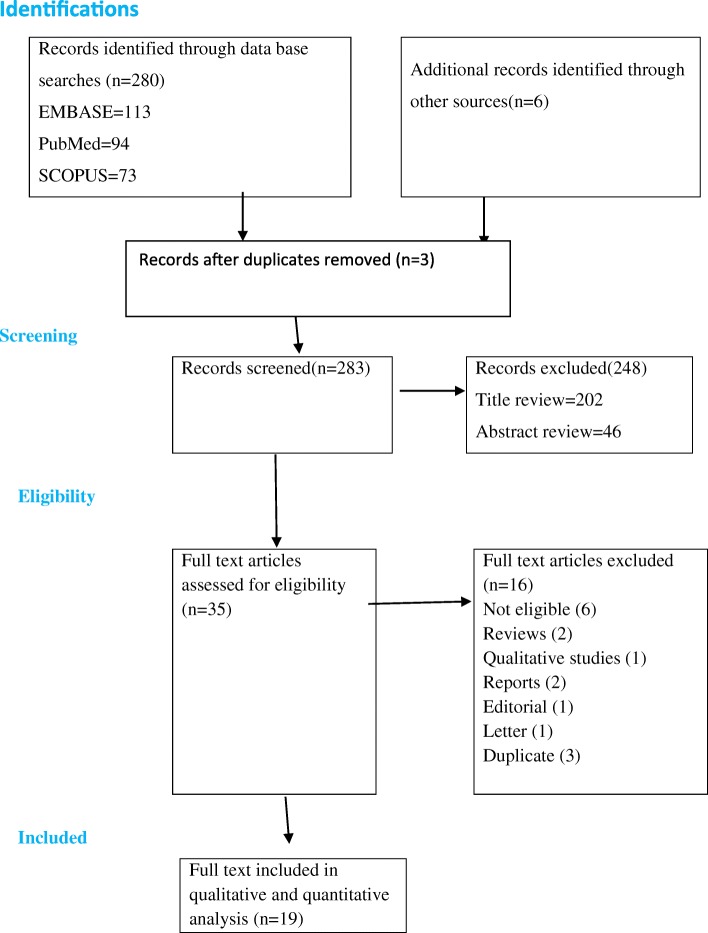
We identified 280 articles in our database search. Our manual search resulted additional six articles. Of these we excluded 205 articles during the review of duplicate and titles as they did not met the inclusion criteria (Fig. 1). In our review of abstracts and keywords we excluded another 46 studies and 19 articles with full-text that met the inclusion criteria were included in our final analysis.
Fig. 1.
PRISMA flowchart of review search
Characteristics of included studies
Among the total of nineteen studies included in our analysis ten of them were done in Uganda [5, 7, 8, 10, 11, 20, 26, 37–39], whereas five of the studies were conducted in Ethiopia [2, 3, 9, 16, 17] and the other studies were conducted in Kenya [18], Tanzania [15], Rwanda [14] and Sudan [40]. The publication year of those studies ranged from 2006 to 2017. All of the included studies used cross-sectional study design. One study used community samples [11] and eighteen studies used samples from institution [2, 3, 5, 7–10, 14–18, 20, 26, 37–40]. Regarding the instrument used, four studies used diagnostic instrument [5, 10, 15, 38], fourteen studies used screening instrument [2, 3, 7–9, 14, 16, 17, 26, 37, 39, 40] and one study used self-report questionnaire to assess depression in PLWHIV [11]. Majority(84.22%) of the studies not reported response rate. Seven studies used random sampling technique, seven used the cohort sample, one study used covenant sampling and four studies not reported the sampling technique (See Table 1).
Table 1.
Distribution of studies on depression in people living with HIV included in qualitative and quantitative analysis based on year, study design, sample size, instrument, country, response rate, study population and prevalence
| Author (year) (reference number) | Study design(setting) | Sample size | Tool | Response rate | Country | Sampling | Study population | Outcome (magnitude of depression) |
|---|---|---|---|---|---|---|---|---|
| Psaros C. et. al. (2014) [37] | Cross sectional study (institution based) | 453 | HSC-D | Not reported | Uganda | Used Cohort population sample | adults | 38%(n=172) |
| Shumba C,et. al. (2013) [11] | Cross sectional study (Community based study) | 732 | Self report | Not reported | Uganda | Random sampling (specific technique not reported) | Adults on HAART | 59%(n=429) |
| Kinyanda E. et. al. (2017) [5] | Cross sectional study (institution based study) | 899 | DSM | Not reported | Uganda | Not reported | adults | 14%(n=126) |
| Yeneabat T.et. al. (2017) [9] | Cross sectional study (institution) | 390 | CES-D | Not reported | Ethiopia | Not reported | adults | 76.7%(n=299) |
| Kinyanda E. et. al. (2011) [38] | Cross sectional study (institution) | 618 | DSM-IV | Not reported | Uganda | Not reported | adults | 8.1%(n=50) |
| Nakasujja N. et. al. (2010) [39] | Cross sectional study (institution setting) | 102 | CES-D | Cohort survey | Uganda | Not reported | Adults | 53.9%(n=55) |
| Akena D. et. al. (2012) [26] | Cross sectional study (institution setting) | 368 | PHQ-9 | Not reported | Uganda | Simple random sampling | Adults | 17.4%(n=64) |
| Hatcher AM. et. al. (2012) [7] | Cross sectional study (institution setting) | 270 | HSC-D | Not reported | Uganda | Used Cohort population sample | Adults | 23.7%(n=64) |
| Cohen MH.et. al. (2009) [14] | Cross sectional study (institution setting) | 658 | CES-D | Not reported | Rwanda | Used Cohort population sample | Adults | 81%(n=533) |
| Musisi S. et. al. (2014) [8] | Cross sectional study (institution setting) | 386 | PHQ-9 | Not reported | Uganda | Used cohort population sample | Adults | 30%(n=116) |
| Tesfaw G.et. al. (2016) [2] | Cross sectional study (institution setting) | 417 | HADS | 100% | Ethiopia | Systematic random sampling | Adults | 41.2%(n=172) |
| Elbadawi A.et. al. (2017) [40] | Cross sectional study (institution setting) | 362 | HADS | Not reported | Sudan | Systematic random sampling | Adults | 61.3%(n=222) |
| Eshetu DA. et. al. (2014) [17] | Cross sectional study (institution setting) | 416 | PHQ-9 | Not reported | Ethiopia | Systematic random sampling | Adults | 38.94%(n=162) |
| Berhe H. et. al. (2013) [3] | Cross sectional study (institution setting) | 269 | HAM-D | Not reported | Ethiopia | Not reported | adults | 43.9%(n=118) |
| Mohammed M. et. al. (2015) [15] | Cross sectional study (institution setting) | 740 | PHQ-9 | 97% | Ethiopia | Systematic random sampling | Adults | 45.8%(n=339) |
| MB.ChB.PW (2011) [18] | Cross sectional study (institution setting) | 400 | BDI | Not reported | Kenya | Systematic random sampling | 47.25%(n=189) | |
| Marwick KF. et. al. (2010) [15] | Cross sectional study (institution setting) | 220 | ICD-10 | 97% | Tanzania | Convenience sampling | Adults | 2.7%(n=6) |
| Kahazura FM. et. al. (2006) [20] | Cross sectional study (institution setting) | 1017 | CES-D | Not reported | Uganda | Used Cohort population sample | Adults | 47%(n=476) |
| Mpungu EN.et. al, 2011 [10] | Cross sectional study (institution setting) | 500 | DSM (MINI) | Not reported | Ugnada | Not clearly indicated | adults | 46.4%(232) |
Key: DSM Diagnostic and Statistical Manual of Mental Disorders, ICD International Classification of Disease, PHQ-9 Patient Health Questionnaire-9, CES-D Center for Epidemiologic Studies Depression Scale Revised, HAM-D Hamilton Depression Rating Scale, BDI Beck's Depression Inventory, HADS Hospital Anxiety and Depression Scale, HSC-D Hopkins Symptom Checklist for Depression
Quality of included studies
We used a modified version of the Newcastle-Ottawa scale (NOS) scale to evaluate the quality of included studies. The methodological quality was good for all nineteen studies. The risk of selection, measurement and non-response bias was low for all studies. The agreement between reviewers regarding the level of bias was moderate or almost perfect for all studies (Kappa statistic range 0.50-1 (Additional file 1: Table S1).
The results of pooled meta-analysis
Prevalence of depression in people living with HIV (PLWHIV)
Nineteen of the studies provided information regarding the prevalence of depression in PLWHIV in east Africa [1–19] (Table 1). These nineteen studies could be combined to provide the pooled estimates. Based on the results of random-effects method, the pooled prevalence of depression in PLWHIV was 38.00% (95% CI 29.30-47.54) and the heterogeneity was considerable (I2=98.59%; Q=11276.10, df=18, variance= 0.08, p <0.0001). The forest plots of the prevalence of depression in people living with HIV were shown in Fig. 2.
Fig. 2.
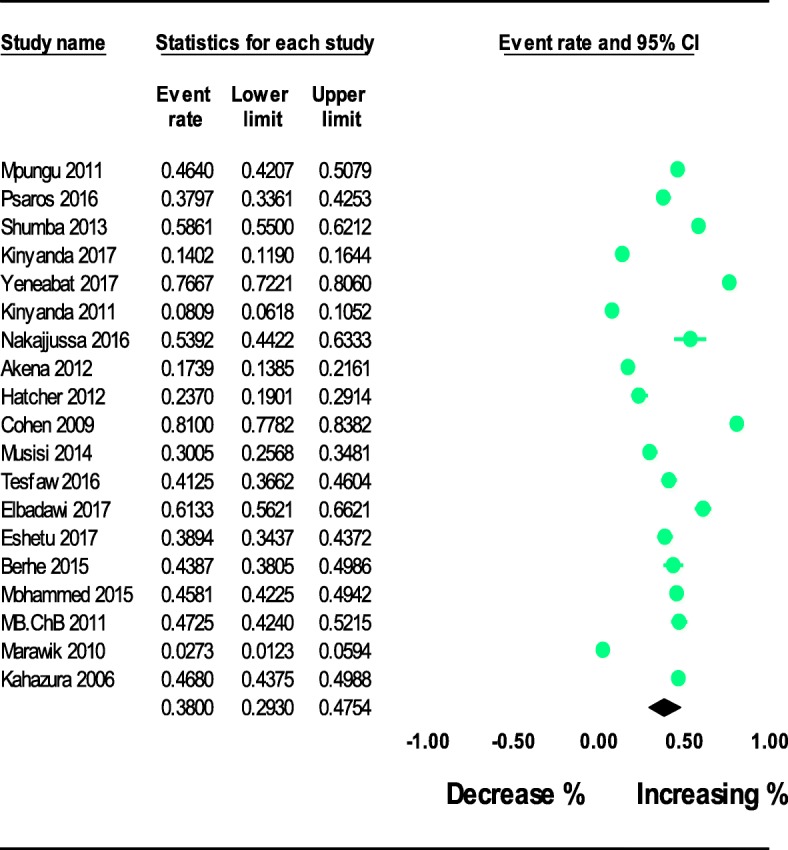
The prevalence of depression in people living with HIV in East Africa: meta-analysis
Subgroup analyses of the prevalence of depression in people living with HIV (PLWHIV)
Subgroup analysis were performed by type of instrument used to assess depression and the country where the studies were conducted as possible source of heterogeneity between the studies as well as to explore the prevalence in each country. For our subgroup analysis based on the country where the studies were conducted, we identified representative data only for Uganda and Ethiopia. For the rest of east African countries (Kenya, Tanzania, Rwanda and Sudan), there is limited data for subgroup analysis.
Of the included studies, ten reported the prevalence of depression in PLWHIV in Uganda [1–4, 6–9, 11, 19, 20]. The pooled prevalence estimates of depression in PLWHIV in Ugandawas30.88% (95% CI 20.84-43.13) (See Table 2).
Table 2.
Prevalence of depression in people with HIV in east Africa: Subgroup meta-analysis and heterogeneity analysis
| Characteristics | Observation (N) | Prevalence (%) | 95% CI | I2 | Q | df | P value |
|---|---|---|---|---|---|---|---|
| Geographic location or country | |||||||
| Uganda | 10 | 30.88 | 20.84-43.13 | 98.57% | 636.65 | 9 | P<0.0001 |
| Ethiopia | 5 | 49.79 | 37.22-62.38 | 97.08 | 136.79 | 4 | P<0.0001 |
| Instrument used or tool used | |||||||
| Diagnostic | 4 | 12.40 | 4.0-32.80 | 98.94% | 281.77 | 3 | P<0.0001 |
| Screening | 14 | 46.00 | 36.90-55.38 | 97.96% | 638.36 | 13 | P<0.0001 |
| Study Setting | |||||||
| Institution based | 18 | 36.86 | 27.87-46.86 | 98.59% | 1207.91 | 17 | P<0.0001 |
| Sample size | |||||||
| <400 | 8 | 34.20 | 19.84-52.18 | 98.32% | 416.89 | 7 | P<0.0001 |
| >400 | 11 | 40.46 | 29.39-52.60 | 98.84% | 858.66 | 10 | P<0.0001 |
| Reference to diagnostic criteria | |||||||
| DSM/ICD | 4 | 12.40 | 4.0-32.80 | 98.94% | 281.77 | 3 | P<0.0001 |
| PHQ-9 | 4 | 32.15 | 21.58-44.92 | 96.61% | 88.57 | P<0.0001 | |
| HADS | 2 | 51.30 | 32.20-70.10 | 96.75% | 30.82 | 1 | P<0.0001 |
| CES-D | 4 | 66.14 | 44.34-82.73 | 98.67% | 226.22 | 3 | P<0.0001 |
| HSC-D | 2 | 30.50 | 18.50-46.10 | 93.51% | 14.41 | 1 | P<0.0001 |
| Year of publication | |||||||
| 2006-2010 | 3 | 33.90 | 10.17-69.93 | 99.25% | 267.34 | 2 | P<0.0001 |
| 2011-2013 | 7 | 32.03 | 19.49-47.84 | 98.52% | 406.32 | 6 | P<0.0001 |
| 2014-2017 | 9 | 43.50 | 31.23-56.69 | 98.37% | 98.37% 489.63 | 8 | P<0.0001 |
Five studies reported the prevalence of depression in PLWHIV in Ethiopia [5, 12, 14–16]. The pooled prevalence of depression in PLWHIV in Ethiopia was 49.79% (95% CI37.22-62.38). (See Table 2). In our analysis the prevalence of depression in PLWHIV in Ethiopia is significantly higher than the prevalent in Uganda (P<.00001). For the rest of east African countries, there is limited data for subgroup analysis. We found only one study conducted in each of the other four east African countries such as Kenya [18], Tanzania [15], Rwanda [14] and Sudan [40].
We also performed subgroup analysis based on the instrument used to assess depression. Four studies used diagnostic instrument (DSM or ICD) and [1, 4, 6, 18, 20] and fourteen studies used screening instrument (PHQ-9, HADS, BDI, CES-D, or HSC-D) to assess depression in people living with HIV in east Africa [1, 5, 7–17, 19]. The pooled prevalence of depression in people living with HIV was 12.40% (95% CI 4.0-32.80) and 46% (95% CI 36.90-55.38) for the studies conducted using diagnostic and screening instrument respectively (see Table 2).
Furthermore, we conducted subgroup analysis based on each instrument used to assess depression. The pooled prevalence estimates of depression for the studies conducted using CES-D 66.14% (44.34-82.73) and HADS 51.30% (32.20-70.10) were significantly higher than results of studies conducted using DSM or ICD12.40% (95% CI 4.0-32.80), PHQ-9 32.15% (21.58-44.92), and HSC-D 30.50% (18.50-46.10) (see Table 2).
Finally, we performed subgroup analysis based on the setting where the studies were conducted. The pooled prevalence of depression in people living with HIV in east Africa for institution based studies was 36.86% (95% CI 27.87-46.86) (see Table 2).
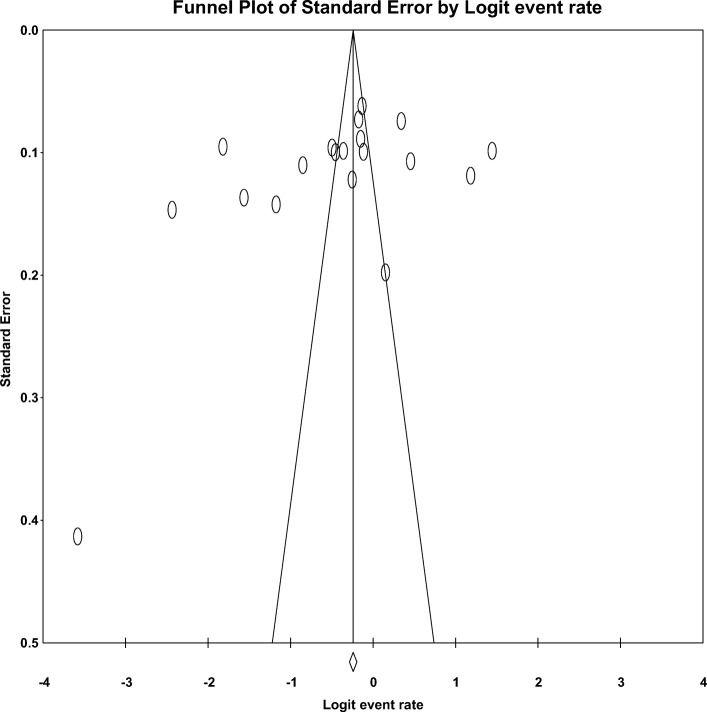
Publication bias
The funnel plot and Egger’s regression tests (B=-9.17, SE=6.16, P=0.155) provided no evidence of substantial publication bias for the prevalence of depression in PLWHIV in east Africa (Fig. 3).
Fig 3.
Funnel plot of risk of publication bias for the prevalence of depression in PLWHIV in east Africa
Sensitivity analysis
For the purpose of further investigating potential source of heterogeneity in the analysis of the prevalence of depression in PLWHIV, we performed leave-one-out sensitivity analysis. Our sensitivity analysis showed that our findings were strong and not dependent on a single study. Our pooled estimated prevalence varied between 35.86(27.53-44.25) and 41.39(32.33-51.07) after deletion of a single study (see Table 3).
Table 3.
Sensitivity analysis of prevalence for each study being removed at a time: prevalence and 95% confidence interval of depression in people living with HIV in east Africa
| Study excluded | Prevalence | 95%CI |
|---|---|---|
| Mpungu 2011 | 37.49 | 28.32–47.66 |
| Psaros 2016 | 37.96 | 28.79–48.08 |
| Shumba 2013 | 36.86 | 27.87–46.86 |
| Kinyanda 2017 | 39.90 | 31.51–48.94 |
| Yeneabat 2017 | 35.86 | 27.53–45.14 |
| Kinyanda 2011 | 40.67 | 32.13–49.82 |
| Nakajjussa 2016 | 37.17 | 28.31–46.99 |
| Akena 2012 | 39.44 | 30.52–49.11 |
| Hatcher 2012 | 38.89 | 29.88–48.74 |
| Cohen 2009 | 35.59 | 27.78–44.25 |
| Musisi 2014 | 38.45 | 29.67–48.42 |
| Tesfaw 2016 | 37.78 | 28.63–47.89 |
| Elbadawi 2017 | 36.74 | 27.90–46.56 |
| Eshetu 2017 | 37.91 | 28.76–48.01 |
| Berhe 2015 | 37.65 | 28.60–47.65 |
| Mohammed 2015 | 37.50 | 28.19–47.84 |
| MB.ChB 2011 | 37.46 | 28.36–47.54 |
| Marawik 2010 | 41.39 | 32.33–51.07 |
| Kahazura 2006 | 37.43 | 27.98–47.95 |
Key. The analysis is based on random effect model
Determinants of depression in people living with HIV
Of 19 included studies, 11 studies that reported factors associated with depression in peoples living with HIV in east Africa were included in the qualitative analysis [2, 3, 5, 7, 9, 10, 16, 17, 20, 26, 38] (See Table 4). Association between WHO clinical staging of disease and depression was observed in three studies [2, 10, 17].
Table 4.
Characteristics of factors associated with depression in people living with HIV east Africa by their odds ratio, confidence interval strength of association, author and year
| Factors | Odds ratio (AOR) | 95% Confidence interval | Strength of association | Adjusted for | Author, year |
|---|---|---|---|---|---|
| Past history of mania | 2.73 | 1.16–6.40 | Moderate, negative | Gender, age, educational status, income, social support, self-efficacy, cognitive impairment, current alcohol use, current alcohol use disorder, duration of ART, CD4 count, WHO clinical staging of HIV disease, tuberculosis | Mpungu, 2011 |
| Mean self efficacy score > 89% | 0.61 | 0.41–0.90 | Strong, negative | Gender, age, educational status, income, social support, mania, cognitive impairment, current alcohol use, current alcohol use disorder, duration of ART, CD4 count, WHO clinical staging of HIV disease, tuberculosis | Mpungu, 2011 |
| WHO clinical staging of HIV disease | 1.88 | 1.24–2.44 | Moderate, positive | Gender, age, educational status, income, social support, mania, self-efficacy, cognitive impairment, current alcohol use, current alcohol use disorder, duration of ART, CD4 count, mania, tuberculosis | Mpungu, 2011 |
| Tuberculosis | 2.37 | 1.20–4.66 | Moderate, positive | Gender, age, educational status, income, social support, mania, self-efficacy, cognitive impairment, current alcohol use, current alcohol use disorder, duration of ART, CD4 count, mania, WHO clinical staging of HIV disease | Mpungu, 2011 |
| Age group 40–49 | 0.95 | 0.92–0.98 | Strong, negative | AIDS stigma, CD4 counts, sex | Akena, 2012 |
| AIDS stigma | 1.65 | 1.20–1.26 | Moderate, positive | Age, CD4 counts, sex | Akena, 2012 |
| CD4 count | 0.43 | 0.20–0.91 | Moderate, negative | Age, AIDS stigma, sex | Akena, 2012 |
| Not have enough food security | 2.89 | 1.40–5.98 | Moderate, positive | Distance from HIV clinic, When knew HIV status, On ART, social support, negative life events, stress score index | Kinyanda. 2011 |
| Negative life event score 6–10 | 4.89 | 1.83–10.06 | Strong, positive | Distance from HIV clinic, When knew HIV status, On ART, social support, food security, stress score index | Kinyanda. 2011 |
| Negative life event score 6–11+ | 16.67 | 7.01–39.66 | Strong, positive | Distance from HIV clinic, When knew HIV status, On ART, social support, food security, stress score index | Kinyanda. 2011 |
| Stress score index> 10 | 7.18 | 2.65–19.47 | Strong, positive | Distance from HIV clinic, When knew HIV status, On ART, social support, food security, negative life event | Kinyanda. 2011 |
| Food insecurity | 3.83 | 1.58–9.32 | Strong, positive | Sex, age educational status, marital status, occupation, residence, number of dependent children, access to food aids, practice of agriculture, ownership of livestock, CD4 level, OIs | Yeneabat, 2017 |
| Presence of OIs | 5.20 | 1.34–20.16 | Strong, negative | Sex, age educational status, marital status, occupation, residence, number of dependent children, access to food aids, practice of agriculture, ownership of livestock, CD4 level, food insecurity | Yeneabat, 2017 |
| HIV stage three | 2.80 | 1.50–5.21 | Moderate, positive | Age, educational status, marital status, residence, CD4 level, perceived stigma, medication adherence, social support | Tesfaw, 2016 |
| Perceived stigma | 3.60 | 2.23–5.80 | Strong, positive | Age, educational status, marital status, residence, CD4 level, HIV stage, medication adherence, socia; support | Tesfaw, 2016 |
| Medication adherence | 1.61 | 1.02–2.55 | Moderate, positive | Age, educational status, marital status, residence, CD4 level, HIV stage, social support | Tesfaw, 2016 |
| Social support | 2.02 | 1.25–3.27 | Moderate, positive | Age, educational status, marital status, residence, CD4 level, HIV stage, medication adherence | Tesfaw, 2016 |
| Married | 0.01 | 0.01–0.07 | Weak, positive | Sexual relationship power scale, age, educational status, heavy drinking, tobacco use, WHO HIV stage, CD4 count, previously treated with ART | Hatcher, 2012 |
| Resilience score | 1.28 | 1.12–1.45 | Weak, positive | Study site, age, sex, stigma score, childhood trauma score, negative coping score, negative life event experience | Kinyanda, 2017 |
| Stigma score | 1.37 | 1.08–1.73 | Weak, positive | Study site, age, sex, resilience childhood trauma score, negative coping score, negative life event experience | Kinyanda, 2017 |
| Childhood trauma score | 1.25 | 1.02–1.55 | Weak, positive | Study site, age, sex, resilience stigma score, negative coping score, negative life event experience | Kinyanda, 2017 |
| Negative scoping score | 1.50 | 1.17–1.92 | Moderate, positive | Study site, age, sex, resilience stigma score, childhood trauma, negative life event experience | Kinyanda, 2017 |
| Negative life experience score | 1.81 | 1.46–2.25 | Moderate, positive | Study site, age, sex, resilience stigma score, childhood trauma, negative scoring score | Kinyanda, 2017 |
| Male sex | 1.633 | 1.138–2.342 | Moderate, positive | Marital status,income, verbal stigma, missed frequency of clinic visit, frequency of clinic visit/month | Mohammed, 2016 |
| Monthly income<500eth.birr | 1.924 | 1.159,3.195 | Moderate, positive | Marital status, sex,, verbal stigma, missed frequency of clinic visit, frequency of clinic visit/month | Mohammed, 2016 |
| Had verbal stigma | 2.705 | 1.445,5.063 | Moderate, positive | Marital status, sex,, verbal stigma, missed frequency of clinic visit, frequency of clinic visit/month | Mohammed, 2016 |
| Missed frequency of clinic visit past one,two and three weeks | 4.35 4.56 and 3.75 respectively | 2.20–8.59, 2.42–8.58 and 1.39–9.93 respectively | Strong, positive | Marital status, sex,, verbal stigma, frequency of clinic visit/month | Mohammed, 2016 |
| Once, twice and three times frequency of clinic visit/month | 19.033, 13.784 and 22.729 | 2.095–172.878, 1.430–132.871, and 2.450–210.873 respectively | Strong, positive | Marital status, sex,, verbal stigma, verbal stigma, missed frequency of clinic visit | Mohammed, 2016 |
| Female sex | 2.071 | 1.077–3.985 | Moderate, positive | Age, income, HIV stage, hospitalization in past one month, felt stigmatized | Eshetu 2015 |
| Age 30–39 | 2.761 | 1.165–6.540 | Moderate, positive | Sex, Income, HIV stage, hospitalization in past one month, felt stigmatized | Eshetu 2015 |
| Age 50–59 | 2.596 | 1.49–9.94 | Moderate, positive | Sex, Income, HIV stage, hospitalization in past one month, felt stigmatized | Eshetu 2015 |
| Age 60–69 | 19.645 | 4.02–95.99 | Strong, positive | Sex, Income, HIV stage, hospitalization in past one month, felt stigmatized | Eshetu 2015 |
| Income < 200 Birr | 3.917 | 1.559, 9.845 | Strong, positive | Age,Sex, HIV stage, hospitalization in past one month, felt stigmatized | Eshetu 2015 |
| Income201–400 Birr | 2.796 | 1.139–6.865 | Moderate, positive | Age, Sex, HIV stage, hospitalization in past one month, felt stigmatized | Eshetu 2015 |
| Income 401–700 Birr | 2.590 | 1.058–6.340 | Moderate, positive | Age, Sex, HIV stage, hospitalization in past one month, felt stigmatized | Eshetu 2015 |
| HIVStage III | 2.317 | 1.108–4.85 | Moderate, positive | Age, Sex, income hospitalization in past one month, felt stigmatized | Eshetu 2015 |
| HIV Stage Iv | 8.769 | 1.93–39.87 | Strong, positive | Age, Sex, income hospitalization in past one month, felt stigmatized | Eshetu 2015 |
| Hospitalized in the past one Month | 15.26 | 1.463–159.22 | Strong, positive | Age, Sex, income month, felt stigmatized, HIVStage | Eshetu 2015 |
| Felt stigmatized | 3.597 | 1.86–6.95 | Strong, positive | Age, Sex, income month,, HIVStage, hospitalized in the past one Month | Eshetu 2015 |
| Age > 50 years | 1.93 | 1.09–3.42 | Moderate, positive | Religion, education, marital status, sex, source of income, CD4 level, HIVStage, number of living children | Kaharuza, 2006 |
| Pensions as source of income | 1.81 | 1.24–2.66 | Moderate, positive | Religion, education, marital status, sex, CD4 level, HIVStage, number of living children, age | Kaharuza, 2006 |
| Primary education | 1.69 | 1.12–2.52 | Moderate, positive | Religion, marital status, sex, CD4 level, HIVStage, number of living children, age, source of income | Kaharuza, 2006 |
| CD4 count 50–99 | 2.02 | 1.22–3.36 | Moderate, positive | Religion, marital status, sex, education, HIVStage, number of living children, age, source of income | Kaharuza, 2006 |
| CD4 count < 50 | 2.34 | 1.39–3.93 | Moderate, positive | Religion, education, marital status, sex, HIVStage, number of living children, age, source of income | Kaharuza, 2006 |
| Urban residence | 3.19 | 1.50–6.65 | Strong, positive | Sex, marital status, income, educational status, occupation, CD4 level | Berhe, 2013 |
| Income < 200 ETB | 4.43 | 1.35–14.58 | Strong, positive | Sex, residence, marital status,, educational status, occupation, CD4 level | Berhe, 2013 |
| Unemployed | 2.74 | 1.34–5.57 | Moderate, positive | Sex, residence, marital status, educational status, CD4 level | Berhe, 2013 |
| Government employee | 3.56 | 1.73–7.30 | Strong, positive | Sex, residence, marital status, educational status, CD4 level | Berhe, 2013 |
In the current review presence of opportunistic infection [9], perceived stigma [2, 20], negative life event [38], WHO clinical staging of disease [17], hospitalization in the past one month [17], stressful life events [38], food insecurity [9], mean self-efficacy (>80%) [41], missed frequency of clinic visit one to three weeks [16], frequency of follow-up [16], older age (age 60-69) [17], income less than 200 Ethiopian birr [3, 17], urban residence [3] and government employee [3] were strongly and significantly associated with depression in people living with HIV in east Africa (See Table 4).
Discussion
To our knowledge, this is the first systematic review and meta-analysis of depression and determinants in PLWHIV in east Africa. The main aim of the study was identification of epidemiological information on the overall prevalence and common determinants of depression in PLWHIV in the area. It is also believed that the results of this review provide greater precision than the results of the studies individually considered. Nineteen studies that analyzed the prevalence of depression and associated factors in PLWHIV in east Africa were included.
The pooled prevalence estimate of depression in this meta-analysis was found a to be 38% in PLWHIV. The magnitude of depression in PLWHIV differed by the setting and the country where the studies were conducted as well as the type of instrument used to measure depression. When measured by DSM or ICD the estimated pooled prevalence of major depressive disorder appeared to be 12.40 % , but the pooled prevalence of depression was 46% as measured by screening instruments. The magnitude of major depressive disorder in PLWHIV in our meta-analysis is much higher compared with the 4% found in the general population [42].
Our estimated pooled prevalence of depression (38%) was higher than the results of systematic review and meta-analysis studies in sub-Saharan Africa which reported the pooled prevalence estimates of depression was 19% in people living HIV with sub-Saharan Africa [22]. These difference might be due to the socioeconomic and cultural differences of the countries.
In our study the pooled prevalence estimates of depression in PLWHIV in Ethiopia (49.79%) was significantly higher than the pooled prevalence estimates of depression in Uganda(30.88%). The difference might be due to all studies done in Ethiopia used screening instrument to determine depression and based on the pooled prevalence estimate, the prevalence of depression measured by screening instrument(46%) was higher than the prevalence of depression measured by diagnostic instrument (12.40%).
As expected, the magnitude of depression showed a considerable variations depending on the measurement used to determine depression in PLWHIV. The pooled prevalence of depression in PLWHIV was apparently higher in studies conducted using screening instrument than diagnostic instrument. The estimated pooled prevalence of depression in PLWHIV was found to be 66.14% , 51.30%, 12.40%, 32.15% and 30.50% as measured by CES-D, HADS, DSM or ICD, PHQ-9, and HSC-D respectively. The fact that diagnostic instrument give more weights towards the high specificity as compared to screening instrument which gives more emphasis towards high sensitivity might be the main reason for the observed difference. The other possible explanation might be diagnostic instrument uses strict criteria as compared to screening instrument as screening instrument aimed to identify potential indicators for disease or potential disease rather than establishing the presence or absence of disease which is the main purpose of diagnostic instrument. Finally, the possible interpretation for the variation in magnitude of depression among the different screening instrument may be due to difference in the sensitivity and specificity the tools used to screen depression in PLWHIV. The findings support the view that validation and use of standard instrument for screening as well as diagnosis of depression in PLWHIV.
Moreover, in our subgroup analysis of prevalence in PLWHIV by study setting show the pooled prevalence of depression in PLWHIV for the studies conducted institution-based setting was 36.86%. This results are lower than unpooled results of depression in community setting which reported magnitude of depression 59%. (see Tables 1 and 2). The fact that the community based study included in this review used self report of depression and all institution based studies used standard diagnostic or screening instrument to assess depression might be the possible reason for the observed difference in magnitude of depression in clinical and community based settings. In addition, the community based study is only one study so the observed result might be highly biased as it is self-report. The study suggest replication of studies in community samples to strengthen our finding as well as understanding of the precise estimates of depression in PLWHIV.
Concerning associated factors, Our qualitative synthesis showed that factors such as having opportunistic infection, perceived stigma, negative life event, WHO clinical staging of disease, hospitalization in the past one month, stressful life events, food insecurity, self-efficacy, missed frequency of clinic visit, frequency of follow-up, older age, low income, urban residence and being government employee were strongly and significantly associated with depression in people living with HIV in east Africa.
Difference between studies
The variation between the studies included in our systematic review and meta-analysis led to high level of heterogeneity in our analysis. The possible contributing factors for the variance in prevalence rates of depression in PLWHIV in east Africa includes the instrument used to measure depression, the study setting and populations. We conducted leave-one-out sensitivity analysis for the purpose of further investigating potential source of heterogeneity in the analysis of the prevalence of depression in PLWHIV. Our sensitivity analysis showed that our findings were strong and not dependent on a single study.
Strength and limitations
The strength of the study includes the use of predefined search strategy in order to reduce reviewers bias as well as performing data extraction and quality assessment by two independent reviewers to minimize the possible reviewer bias. The other strength is performing sensitivity and subgroup analysis based on study setting, instrument used, and country of study to identify the small study effect and the risk of heterogeneity. Finally, evaluating the quality of the studies included in analysis and based on the results from the assessment of the study quality the methodological quality was generally good. Nevertheless, the study has some limitations: first, small number of studies were included in our subgroup analysis which reduce the precision of the estimate; second, apparent heterogeneity was identified among the studies; due to inconsistent adjustment and inclusion of factors determining depression in PLWHIV we done only qualitative analysis for associated factors of depression.
Conclusion
Our study found that the pooled prevalence estimate of depression in PLWHIV was 38% (95% CI 29.30-47.54). In our study the pooled prevalence estimates of depression in PLWHIV in Ethiopia was significantly higher than the pooled prevalence estimates of depression in Uganda. In addition the prevalence of depression was significantly higher in studies conducted by using screening as compared to diagnostic instrument. The study also resulted in a significant variation in prevalence of depression based on the instrument used. These findings have several implications for clinical practice and research. Based on this finding routine screening and integrated management of mental health condition into the existing HIV care services is warranted in east Africa. Validation and use of standard instrument to assess depression in PLWHIV is needed. In addition longitudinal and community based studies focusing on incidence and determinates of depression in PLWHIV are recommended. Attention need to be given for those people who have opportunistic infection, older age, advanced HIV stage, experienced stressful life events,who have perceived stigma and those who are on ART to prevent risk of non-adherence and treatment resistance and further to improve the quality PLWHIV.
Additional files
Table S1. Summary of agreed level of bias and level of agreement on the methodological qualities of included studies in meta-analysis based on sampling, outcome, response rate and method of analysis. (DOCX 15 kb)
Acknowledgments
Availability of data and materials
All data generated or analyzed during this study are included in this article.
Abbreviations
- BDI
Beck's Depression Inventory
- CES-D
Center for Epidemiologic Studies Depression Scale Revised
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- HADS
Hospital Anxiety and Depression Scale
- HAM-D
Hamilton Depression Rating Scale
- HIV
Human Immunodeficiency Virus
- HSC-D
Hopkins Symptom Checklist for Depression
- ICD
International Classification of Disease
- PHQ-9
Patient Health Questionnaire-9,
- PLWHIV
people living with Human Immunodeficiency Virus
Authors’ contributions
The author (GA) performed the search, data extraction, analyses and draft and approval of final manuscript. MA performed data extraction, quality assessment and approved final manuscript. MS participated in discussion and consensus and approved the final manuscript.
Ethics approval and consent to participate
N/A.
Consent for publication
N/A.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Getinet Ayano, Email: babiget2015@gmail.com.
Melat Solomon, Email: mimisolomon2010@gmail.com.
Mebratu Abraha, Email: mebratuabraha21@gmail.com.
References
- 1.Feuillet P, Lert F, Tron L, Aubriere C, Spire B, Dray-Spira R. Prevalence of and factors associated with depression among people living with HIV in France. Hiv Medicine. 2017;18(6):383–394. doi: 10.1111/hiv.12438. [DOI] [PubMed] [Google Scholar]
- 2.Tesfaw G, Ayano G, Awoke T, Assefa D, Birhanu Z, Miheretie G, et al. Prevalence and correlates of depression and anxiety among patients with HIV on-follow up at Alert Hospital, Addis Ababa. Ethiopia. BMC psychiatry. 2016;16(1):368. doi: 10.1186/s12888-016-1037-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berhe H, Bayray A. Prevalence of depression and associated factors among people living with HIV/AIDS in tigray, North Ethiopia: A cross sectional hospital based study. International Journal of Pharmaceutical Sciences and Research. 2013;4(2):761–771. [Google Scholar]
- 4.Kinyanda E, Kuteesa M, Scholten F, Mugisha J, Baisley K, Seeley J. Risk of major depressive disorder among older persons living in HIV-endemic central and southwestern Uganda. AIDS care. 2016;28(12):1516–1521. doi: 10.1080/09540121.2016.1191601. [DOI] [PubMed] [Google Scholar]
- 5.Kinyanda E, Nakasujja N, Levin J, Birabwa H, Mpango R, Grosskurth H, et al. Major depressive disorder and suicidality in early HIV infection and its association with risk factors and negative outcomes as seen in semi-urban and rural Uganda. Journal of affective disorders. 2017;212:117–127. doi: 10.1016/j.jad.2017.01.033. [DOI] [PubMed] [Google Scholar]
- 6.Peterson K, Togun T, Klis S, Menten J, Colebunders R. Depression and posttraumatic stress disorder among HIV-infected Gambians on antiretroviral therapy. AIDS Patient Care STDs. 2012;26(10):589–96. [DOI] [PubMed]
- 7.Hatcher AM, Tsai AC, Kumbakumba E, Dworkin SL, Hunt PW, Martin JN, et al. Sexual relationship power and depression among HIV-infected women in Rural Uganda. PloS one. 2012;7(12):e49821. doi: 10.1371/journal.pone.0049821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Musisi S, Wagner GJ, Ghosh-Dastidar B, Nakasujja N, Dickens A, Okello E. Depression and sexual risk behaviour among clients about to start HIV antiretroviral therapy in Uganda. International journal of STD & AIDS. 2014;25(2):130–137. doi: 10.1177/0956462413495186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeneabat T, Bedaso A, Amare T. Factors associated with depressive symptoms in people living with HIV attending antiretroviral clinic at Fitche Zonal Hospital, Central Ethiopia: Cross-sectional study conducted in 2012. Neuropsychiatric Disease and Treatment. 2017;13:2125–2131. doi: 10.2147/NDT.S131722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nanni MG, Caruso R, Mitchell AJ, Meggiolaro E, Grassi L. Depression in HIV infected patients: a review. Curr Psychiatry Rep. 2015;17(1):530. [DOI] [PubMed]
- 11.Shumba C, Atukunda R, Imakit R, Memiah P. Prevalence of depressive symptoms amongst highly active antiretroviral therapy (HAART) patients in AIDSrelief Uganda. Journal of Public Health in Africa. 2013;4(2):84–87. doi: 10.4081/jphia.2013.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Niu L, Luo D, Liu Y, Silenzio VMB, Xiao S. The Mental Health of People Living with HIV in China, 1998–2014: A Systematic Review. PLOS ONE. 2016;11(4):e0153489. [DOI] [PMC free article] [PubMed]
- 13.Wang T, Fu H, Kaminga AC, Li Z, Guo G, Chen L, et al. Prevalence of depression or depressive symptoms among people living with HIV/AIDS in China: a systematic review and meta-analysis. BMC Psychiatry. 2018;18(1):160. [DOI] [PMC free article] [PubMed]
- 14.Cohen MH, Fabri M, Cai X, Shi Q, Hoover DR, Binagwaho A, et al. Prevalence and predictors of posttraumatic stress disorder and depression in HIV-infected and at-risk Rwandan women. Journal of women's health (2002) 2009;18(11):1783–1791. doi: 10.1089/jwh.2009.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marwick KF, Kaaya SF. Prevalence of depression and anxiety disorders in HIV-positive outpatients in rural Tanzania. AIDS care. 2010;22(4):415–419. doi: 10.1080/09540120903253981. [DOI] [PubMed] [Google Scholar]
- 16.Mohammed M, Mengistie B, Dessie Y, Godana W. Prevalence of depression and associated factors among HIV patients seeking treatments in ART clinics at Harar Town. Eastern Ethiopia. J AIDS Clin Res. 2015;6(474):2. [Google Scholar]
- 17.Eshetu DA, Meseret S, Kebede MA, Techane GN, Gizachew KD, Tegegne MT, et al. Prevalence of depression and associated factors among HIV/AIDS Patients attending ART Clinic at Debrebirhan referral hospital, North Showa, Amhara Region, Ethiopia. Clin Psychiatry. 2015;1(1):1–7.
- 18.Ng’ang’a PW, Mathai M, Obondo A. Prevalence of anxiety and depression among hiv/aids patients attending the comprehensive care centre (ccc), Kenyatta national hospital (knh). Grey literature. 2011. [Google Scholar]
- 19.Belete A, Andaregie G, Tareke M, Birhan T, Azale T. Prevalence of anxiety and associated factors among people living HIV/AIDS at debretabor general hospital anti retro viral clinic Debretabor, Amhara, Ethiopia, 2014. American Journal of Psychiatry and Neuroscience. 2014;2(6):109–114. doi: 10.11648/j.ajpn.20140206.15. [DOI] [Google Scholar]
- 20.Kaharuza FM, Bunnell R, Moss S, Purcell DW, Bikaako-Kajura W, Wamai N, et al. Depression and CD4 cell count among persons with HIV infection in Uganda. AIDS and behavior. 2006;10(4 Suppl):S105–S111. doi: 10.1007/s10461-006-9142-2. [DOI] [PubMed] [Google Scholar]
- 21.Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545-602. [DOI] [PMC free article] [PubMed]
- 22.Bernard C, Dabis F, de Rekeneire N. Prevalence and factors associated with depression in people living with HIV in sub-Saharan Africa: A systematic review and meta-analysis. PloS one. 2017;12(8):e0181960. doi: 10.1371/journal.pone.0181960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adewuya AO, Afolabi MO, Ola BA, Ogundele OA, Ajibare AO, Oladipo BF, et al. Relationship between depression and quality of life in persons with HIV infection in Nigeria. The International Journal of Psychiatry in Medicine. 2008;38(1):43–51. doi: 10.2190/PM.38.1.d. [DOI] [PubMed] [Google Scholar]
- 24.Nakimuli-Mpungu E, Musisi S, Katabira E, Nachega J, Bass J. Prevalence and factors associated with depressive disorders in an HIV+ rural patient population in southern Uganda. Journal of affective disorders. 2011;135(1):160–167. doi: 10.1016/j.jad.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 25.Olley BO, Seedat S, Stein DJ. Persistence of psychiatric disorders in a cohort of HIV/AIDS patients in South Africa: a 6-month follow-up study. Journal of psychosomatic research. 2006;61(4):479–484. doi: 10.1016/j.jpsychores.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 26.Akena D, Musisi S, Joska J, Stein DJ. The association between aids related stigma and major depressive disorder among HIV-positive individuals in Uganda. PloS one. 2012;7(11):e48671. doi: 10.1371/journal.pone.0048671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olley B, Seedat S, Nei D, Stein D. Predictors of major depression in recently diagnosed patients with HIV/AIDS in South Africa. AIDS patient care and STDs. 2004;18(8):481–487. doi: 10.1089/1087291041703700. [DOI] [PubMed] [Google Scholar]
- 28.Sin NL, DiMatteo MR. Depression treatment enhances adherence to antiretroviral therapy: a meta-analysis. Annals of Behavioral Medicine. 2014;47(3):259–269. doi: 10.1007/s12160-013-9559-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: a review and meta-analysis. Journal of acquired immune deficiency syndromes (1999) 2011;58(2):181–187. doi: 10.1097/QAI.0B013E31822D490A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hartzell JD, Janke IE, Weintrob AC. Impact of depression on HIV outcomes in the HAART era. Journal of Antimicrobial Chemotherapy. 2008;62(2):246–255. doi: 10.1093/jac/dkn193. [DOI] [PubMed] [Google Scholar]
- 31.Asangbeh SL, Sobngwi JL, Ekali GL, Eyoum C, Msellati P. Predictors of depression among patients on art in a rural health district in North West Cameroon. AIDS care. 2016;28(2):205–208. doi: 10.1080/09540121.2015.1074654. [DOI] [PubMed] [Google Scholar]
- 32.Reviews UoYCf, Dissemination . Systematic reviews: CRD's guidance for undertaking reviews in health care. University of York: Centre for Reviews & Dissemination; 2009. [Google Scholar]
- 33.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European journal of epidemiology. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 34.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 35.Borenstein M, Hedges LV, Higgins J, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Research synthesis methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 36.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ: British Medical Journal. 2003;327(7414):557. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Psaros C, Haberer JE, Boum Y, II, Tsai AC, Martin JN, Hunt PW, et al. The Factor Structure and Presentation of Depression Among HIV-Positive Adults in Uganda. AIDS and behavior. 2014;19(1):27–33. doi: 10.1007/s10461-014-0796-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kinyanda E, Hoskins S, Nakku J, Nawaz S, Patel V. Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district. Uganda. BMC psychiatry. 2011;11:205. doi: 10.1186/1471-244X-11-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakasujja N, Skolasky RL, Musisi S, Allebeck P, Robertson K, Ronald A, et al. Depression symptoms and cognitive function among individuals with advanced HIV infection initiating HAART in Uganda. BMC psychiatry. 2010;10:44. doi: 10.1186/1471-244X-10-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elbadawi A, Mirghani H. Depression among HIV/AIDS Sudanese patients: a cross-sectional analytic study. The Pan African medical journal. 2017;26:43. doi: 10.11604/pamj.2017.26.43.10919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nakimuli-Mpungu E, Mojtabai R, Alexandre PK, Musisi S, Katabira E, Nachega JB, et al. Lifetime depressive disorders and adherence to anti-retroviral therapy in HIV-infected Ugandan adults: A case-control study. Journal of affective disorders. 2013;145(2):221–226. doi: 10.1016/j.jad.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 42.Waraich P, Goldner EM, Somers JM, Hsu L. Prevalence and incidence studies of mood disorders: a systematic review of the literature. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2004;49(2):124–138. doi: 10.1177/070674370404900208. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Summary of agreed level of bias and level of agreement on the methodological qualities of included studies in meta-analysis based on sampling, outcome, response rate and method of analysis. (DOCX 15 kb)
Data Availability Statement
All data generated or analyzed during this study are included in this article.