SUMMARY
Aim:
This study was undertaken to update the outcome of the treated lesions with electrochemotherapy (ECT) plus intravenous injection of bleomycin in patients with in-transit disease or distant cutaneous metastases in melanoma patients.
Patients & methods:
89 patients with relapsed and refractory cutaneous melanoma metastases or in-transit disease were submitted to 126 treatments of ECT.
Results:
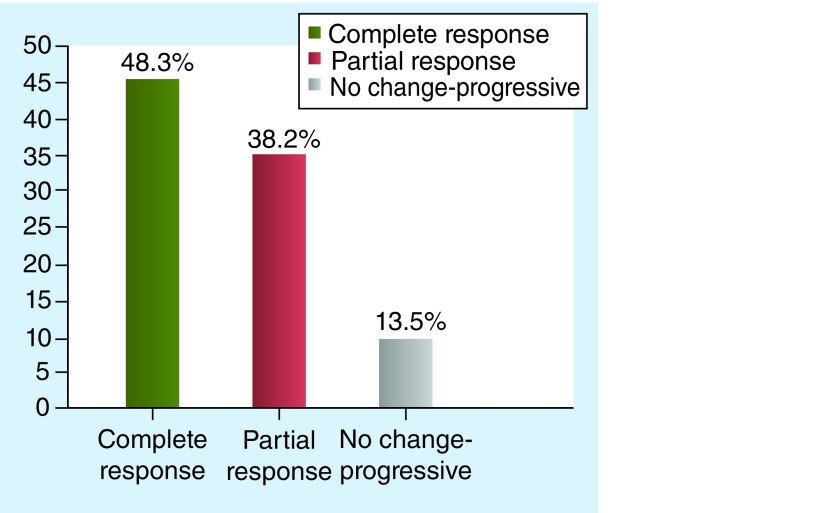
34 patients (38.2%) had a partial response and 43 had a complete response (48.3%). 12 patients (13.5%) had no change or progressive disease. The objective response rate was 67.5%.
Conclusion:
The favorable outcome obtained in the present study demonstrates that ECT is a reliable, easy, fast and effective procedure showing benefits in terms of curative and palliative treatment for unresectable cutaneous lesions respecting the quality of life.
KEYWORDS : cutaneous metastases, electrochemotherapy, in-transit, loco-regional treatments, melanoma
Practice points.
Electrochemotherapy (ECT) is a tumor ablation modality which consists of local application of electric pulses which can transiently increase cell membrane permeability to cytotoxic chemotherapeutic drugs.
ECT has shown to be effective as palliative treatment of cutaneous and subcutaneous metastases in patients with cutaneous melanoma.
ECT has a high response rate and a favorable safety profile showed a long-lasting response in patients with cutaneous or subcutaneous metastases, obtained with an easy, fast and effective procedure that can be repeated.
Overall response rates ranging 55–99% comparable with other locoregional treatments such isolated limb perfusion, which are more complex treatment with higher morbidity.
ECT has been shown to rapidly stop bleeding in patients with bleeding cutaneous lesions, thereby improving quality of life.
Melanoma is the leading cause of skin cancer death, producing an estimated 160,000 cases of melanoma worldwide and 40,8000 deaths in 2012 [1]. However, the fact that melanomas incidence and mortality rate are steadily increasing in many populations of European origin, that cure is probable only if melanoma is diagnosed early and that medical and physical therapy exert dismaying results, make it as an important public health issue. The estimated incidence rate standardized to the age distribution averaged between 9.2 and 5.9 per 100,000 in Europe [2]. Local recurrence, in-transit metastases and satellitosis represent the same lymphatic dissemination, occurring in 2–20% of patients, depending largely on initial tumor thickness, within 3 years. Of those 20–30% are local recurrence alone, 30–60% are regional and 15–40% have distant metastases. The survival is generally poor, being 20–50% at 5 years [3].
The treatment of recurrent cutaneous melanoma is primarily surgical, but quite often lesions are so numerous and widespread to be unresectable. In such cases, the therapeutic challenge is tremendous because cutaneous metastasis is not sensitive to conventional therapies.
Electrochemotherapy (ECT) is a nonthermal tumor ablation modality, whereby the application of electric fields on cancer tissue renders the cell membrane permeable to non- or low-permeant antineoplastic drugs, thus potentiating their cytotoxic effect directly on cellular DNA. This temporary increased permeability of the cell membrane caused by the electric pulses facilitates a potent localized effect and magnifies the drug cytotoxicity by orders of magnitude. ECT is characterized by the absence of toxicity and high effectiveness in the control of superficial skin metastases [4,5].
The present analysis is an update to a previous analysis of the experience with ECT in an increased data set of patients with in-transit or cutaneous disease focusing on the locoregional control rate [6]. The paper has its scientific impact for clinicians validating a procedure in the management of metastatic melanoma. The higher number of cases and a longer follow-up confirmed the results already reported and the role of ECT in the treatment of cutaneous melanoma metastases.
Patients & methods
Between 2010 January and 2014 September, 89 patients with relapsed and refractory cutaneous melanoma metastases or in-transit disease underwent one to five courses of ECT using the Cliniporator™ (IGEA Ltd, Modena, Italy) pulse generator with intravenous injection of bleomycin according to the European Standard Operating Procedures of Electrochemotherapy (ESOPE) guidelines [7].
All treatments were performed using the Cliniporator™ device (IGEA Ltd) with two different types of electrodes: type II, with parallel needles, for treatment of lesions in the head and neck area and type III, with hexagonal needles, for all other sites. Electric pulses were delivered from 8 until 28 min after intravenous injection of bleomycin according to the ESOPE standardized criteria. Electrical parameters were for type II electrodes eight electric pulses of 1000 V/cm amplitude over distant ratio and 100 μs duration, delivered at either 1 5000 Hz repetition frequency; for type III electrodes 96 electric pulses of 1000V/cm amplitude over distant ratio and 100 μs duration, delivered at 1 or 5000 Hz repetition frequency. The required dose of bleomycin was 1,5000 IU/m2. ECT was performed under general or locoregional anesthesia, dependent on the area being treated. All patients gave written informed consent before each treatment. The rate of electrode application is the number of applications for a patient in a single course of ECT.
Response to treatment was evaluated 3 months after ECT in accordance with WHO guidelines and defined as progressive disease (PD) for lesions increased in tumor size (larger diameter of metastases) >25%, no change (NC) for lesions increased in tumor size <25% or decreased <50%, partial response (PR) for lesions decreased in tumor size >50% and complete response (CR) for lesions that had disappeared. Patients were assessed every 4 weeks for 6 months and thereafter every 3 months. In the course of follow-up, the appearance of lesions in untreated areas was considered to be new disease rather than a relapse of the previously treated lesion. A further ECT session was proposed at least 6–8 weeks after the previous treatment in all patients with PR. The 3 months evaluation was clinical despite of the number of ECTs. The objective was not to analyze how many treatments are necessary to obtain response, but to verify the overall efficacy of the treatment adopted. The treatment was approved by Ethical Committee.
Results
Clinical and pathological characteristics of patients are summarized in Table 1. All patients had recurrent cutaneous disease after one or more previous radical surgical treatments. 28 patients had cutaneous or in-transit disease of the trunk, 60 had in-transit disease of an inferior limb and six patients had cutaneous disease in the head and neck area. No patient with limb disease had previously received isolated limb perfusion.
Table 1. . Patient and tumor characteristics.
| Characteristic | Value |
|---|---|
| Age, median (range); years | 62 (27–89) |
| Male/female (n) | 49/40 |
| Breslow thickness, median (range) | 5.0 (0.8–20.0) |
| Site of metastases (n): | |
| – Trunk | 28 |
| – Limbs | 55 |
| – Head and neck | 6 |
| Type of metastases (n): | |
| – In-transit | 60 |
| – Local recurrence | 5 |
| – Distant cutaneous | 24 |
| Size of metastases, median (range); mm | 12 (2–35) |
A total of 126 courses of ECT were performed in the 89 patients; 39 patients had a single ECT session and 50 patients underwent ≥2 sessions of ECT, including one patient who had five sessions and one patient who had six ECTs. The mean rate of electrode application per patient was 73 and ranged from 8 to 187. The median duration of follow-up was 27.5 months (range: 6–67 months). Nine (10.1%) patients had the dose reduced to 10,000 IU/m2 because of decreased renal function or cardiac disease, but this is not related with local response rate. Treatment was well tolerated with the most frequent side effects being nonsignificant, mild local pain in 33 patients (37.0%) resolved within the 48 h and locoregional myalgia in 12 patients (13.5%) that requested medical treatment and persisting for no longer than 2 weeks. No systemic side effects were observed. Necrosis of the treated lesions occurred in 26 patients (29.2%), all of whom had received multiple sessions of ECT. Tattoo of needle electrodes remained visible in the treated areas for about 3 months. There were not correlations with the size of treated lesions and the electrodes used.
3 months after the ECT treatments, 34 patients (38.2%) had a PR and 43 had a CR (48.3%). 12 patients (13.5%) had NC or PD. The objective response rate of all treated lesions was 67.5% (Figure 1).
Figure 1. . Treatment response.
Discussion
Cutaneous melanoma is the seventh most common type of cancer and the most common form of malignancy in young adults. Local recurrence, in-transit metastases and satellitosis represent a challenge because of their unresectability and relative insensitivity to conventional systemic therapies. This peculiar metastatic disease is a psychological burden for the patient, whose quality of life may be adversely affected by pain, ulceration, malodorous discharge and bleeding associated with lesions.
The reported 5-year survival for patients with in-transit melanoma metastasis is poor, ranging from 12 to 37% [4].
ECT is a tumor ablation modality which consists of the local application of short duration (˜5 KHz for 100 μs) but high-voltage (several hundred V cm-1) pulses which can transiently increase cell membrane permeability to cytotoxic chemotherapeutic drugs [8–12]. Several cytotoxic drugs have been tested and the best candidate for this type of therapy resulted to be bleomycin. Electroporation (EP) or the drugs on their own do not influence the growth of tumors, but the combination of the EP and bleomycin has potent antitumor effects. In previous reports, ECT has shown to be effective as palliative treatment of cutaneous and subcutaneous metastases in patients with cutaneous melanoma [13–28].
Clinical evidence for ECT for local control of metastatic melanoma with superficial lesions is evolving, but its potential advantages for patients are now recognized. ECT has a high response rate and a favorable safety profile. The limited damage to surrounding tissue coupled with the simplicity of administration and short patient recovery time make it a useful tool for any oncologist [18,19]. A particular benefit of ECT is that it can facilitate the treatment of tumor nodules that occur in the proximity of important, and often vulnerable, structures, such as blood vessels and nerves where surgery is not possible [29,30].
In a previous analysis we have shown that 21.7% of patients experienced a long-lasting response in melanoma treated with ECT, obtained with an easy, fast and effective procedure which can be repeated [6]. In the present series, that represents an update to the experience already published, new cases treated and a longer follow-up confirmed that the ECT approach is effective in about 50% of cases in which a CR was obtained with one or two courses, with a very efficient local tumor control and may improve patient quality of life. Data for tumor size were not analyzed as predictor of local responses because of the homogeneity of the treated cases in which lesion does not exceeded 3 cm. It is possible that the number and the location (cutaneous or subcutaneous) make a difference, but these aspect will be the object of future evaluation. Mali et al. in a systematic review showed that ECT has an antitumor effectiveness in different tumors with better results compared with chemotherapy alone by more than 50%. The objective responses were significantly higher for nonmelanoma than melanoma tumors (86.4 and 80.6%, respectively) [31].
Studies investigating the effectiveness of ECT in patients with advanced melanoma have recently been reported and suggest overall response rates ranging 55 to 99% comparable with other locoregional treatments such isolated limb perfusion [32–34]. Quaglino et al. reported a response rate of 93% (13/14) after the first ECT, with a complete regression in seven patients (50%) [35]. Kis et al. reported their experience with the use of ECT with bleomycin in 158 cutaneous and subcutaneous metastases from nine patients with cutaneous melanoma, in which an objective response rate of 62% was achieved. Repeating the ECT procedure increased the response rate in the retreated lesions (72%) with a local tumor control rate of 74.5% at 2 years [36].
ECT has also been shown to rapidly stop bleeding in patients with bleeding cutaneous lesions, thereby improving quality of life [32–40].
In a recent meta-analyses of 47 prospective studies, Spratt concluded that skin-directed therapies showed heterogeneous but high response rate, with low recurrence rates and minimal toxicity and improvements in quality of life [19].
Campana et al. analyzed the predictors for the best response to ECT in 85 cases with superficial disseminated melanoma and concluded that ECT proved to be highly active against metastases that were refractory to previous chemotherapy and leads to long-term stabilization of widespread superficial melanoma. Patients with 20 or fewer skin metastases, smaller than 3 cm in diameter, have a high local response rate, with disease control and favorable survival [14].
Conclusion
ECT is easy to perform and provides a good quality of life and economic benefits without the potentially undesirable side effects of systemic chemotherapy. The favorable outcome obtained in the present study confirmed that ECT is a reliable, easy, fast and effective procedure that provides benefits in terms of curative and palliative treatment for unresectable cutaneous lesions without adversely impacting on the quality of life of patients.
Future perspective
As ECT-based technology evolves, it will be interesting to see the impact this has on future treatment regimens in oncology [10–12]. This technology may eventually provide multiple clinical applications. Continuous technological development and clinical investigation of EP-based treatments will only serve to further increase its clinical relevance [41].
Footnotes
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.GLOBOCAN 2012. Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. http://globocan.iarc.fr/Default.aspx
- 2.Robinson JK, Baker MK, Hillhouse JJ. New approaches to melanoma prevention. Dermatol. Clin. 2012;30:405–412. doi: 10.1016/j.det.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kretschmer L, Beckmann I, Thoms KM, Mitteldorf C, Bertsch HP, Neumann C. Factors predicting the risk of in-transit recurrence after sentinel lymphonodectomy in patients with cutaneous malignant melanoma. Ann. Surg. Oncol. 2006;13:1105–1112. doi: 10.1245/ASO.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 4.Gehl J. Electrochemotherapy: theory and methods, perspectives for drug delivery gene therapy and research. Acta Physiol. Scand. 2003;177(4):437–447. doi: 10.1046/j.1365-201X.2003.01093.x. [DOI] [PubMed] [Google Scholar]
- 5.Sersa G, Miklavčič D, Cemazar M, Rudolf Z, Pucihar G, Snoj M. Electrochemotherapy in treatment of tumors. Eur. J. Surg. Oncol. 2007;34:232–240. doi: 10.1016/j.ejso.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 6.Caracò C, Mozzillo N, Marone U, et al. Long-lasting response to electrochemotherapy in melanoma patients with cutaneous metastasis. BMC Cancer. 2013;13:564. doi: 10.1186/1471-2407-13-564. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Reported for the first time a long-lasting response to electrochemotherapy.
- 7.Marty M, Sersa G, Garbay JR, et al. Electrochemotherapy – an easy, highly effective and safe treatment of cutaneous and subcutaneous metastases: results of ESOPE (European Standard Operating Procedures of Electrochemotherapy) study. EJC Supplements. 2006;4:3–13. [Google Scholar]; •• Reported the standard operative procedures of electrochemotherapy.
- 8.Mir LM. Bases and rationale of the electrochemotherapy. Eur. J. Cancer. 2006;4(11):38–44. [Google Scholar]
- 9.Larkin JO, Collins CG, Aarons S, et al. Electrochemotherapy: aspects of preclinical development and early clinical experience. Ann. Surg. 2007;245:469–479. doi: 10.1097/01.sla.0000250419.36053.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miklavčič D, Mali B, Kos B, Heller R, Serša G. Electrochemotherapy: from the drawing board into medical practice. Biomed. Eng. Online. 2014;13:29. doi: 10.1186/1475-925X-13-29. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Discussion about implementation of electrochemotherapy into standard of care for treatment of skin tumors.
- 11.Yarmush ML, Golberg A, Serša G, Kotnik T, Miklavčič D. Electroporation-based technologies for medicine: principles, applications, and challenges. Ann. Rev. Biomed. Eng. 2014;16:295–320. doi: 10.1146/annurev-bioeng-071813-104622. [DOI] [PubMed] [Google Scholar]
- 12.Cadossi R, Ronchetti M, Cadossi M. Locally enhanced chemotherapy by electroporation: clinical experience and perspective of use of electrochemotherapy. Future Oncol. 2014;10:877–890. doi: 10.2217/fon.13.235. [DOI] [PubMed] [Google Scholar]; •• Analyzed future applications of electrochemotherapy.
- 13.Campana LG, Testori A, Mozzillo N, Rossi CR. Treatment of metastatic melanoma with electrochemotherapy. J. Surg. Oncol. 2014;109:301–307. doi: 10.1002/jso.23512. [DOI] [PubMed] [Google Scholar]
- 14.Queirolo P, Marincola F, Spagnolo F. Electrochemotherapy for the management of melanoma skin metastasis: a review of the literature and possible combinations with immunotherapy. Arch. Dermatol. Res. 2014;306:521–526. doi: 10.1007/s00403-014-1462-x. [DOI] [PubMed] [Google Scholar]; • Analyzed the possible associations of electrochemotherapy with new immunotherapeutic drugs.
- 15.Solari N, Spagnolo F, Ponte E, et al. Electrochemotherapy for the management of cutaneous and subcutaneous metastasis: a series of 39 patients treated with palliative intent. J. Surg. Oncol. 2014;109:270–274. doi: 10.1002/jso.23481. [DOI] [PubMed] [Google Scholar]
- 16.Rastrelli M1, Alaibac M, Stramare R, et al. Melanoma m (zero): diagnosis and therapy. ISRN Dermatol. 2013;11:616–617. doi: 10.1155/2013/616170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Testori A, Soteldo J, Powell B, et al. Surgical management of melanoma: an EORTC Melanoma Group survey. Ecancermedicalscience. 2013;7:294. doi: 10.3332/ecancer.2013.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campana LG, Valpione S, Mocellin S, et al. Electrochemotherapy for disseminated superficial metastases from malignant melanoma. Br. J. Surg. 2012;99(6):821–830. doi: 10.1002/bjs.8749. [DOI] [PubMed] [Google Scholar]
- 19.Spratt DE, Gordon Spratt EA, Wu S, et al. Efficacy of skin-directed therapy for cutaneous metastases from advanced cancer: a meta-analysis. J. Clin. Oncol. 2014;32(28):3144–3155. doi: 10.1200/JCO.2014.55.4634. [DOI] [PMC free article] [PubMed] [Google Scholar]; • A meta-analyses about the application of electrochemotherapy in cutaneous metastases.
- 20.Mir-Bonafé JM, Vilalta A, Alarcón I, et al. Electrochemotherapy in the treatment of melanoma skin metastases: a report on 31 cases. Actas. Dermosifiliogr. 2014;12:S0001–S7310. doi: 10.1016/j.ad.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 21.Ricotti F, Giuliodori K, Cataldi I, et al. Electrochemotherapy: an effective local treatment of cutaneous and subcutaneous melanoma metastases. Dermatol. Ther. 2014;27(3):148–152. doi: 10.1111/dth.12098. [DOI] [PubMed] [Google Scholar]
- 22.Kähler KC, Egberts F, Gutzmer R. Palliative treatment of skin metastases in dermato-oncology. J. Dtsch. Dermatol. Ges. 2013;11(11):1041–1045. doi: 10.1111/ddg.12197. [DOI] [PubMed] [Google Scholar]
- 23.Matthiessen LW, Chalmers RL, Sainsbury DC, et al. Management of cutaneous metastases using electrochemotherapy. Acta Oncol. 2011;50(5):621–629. doi: 10.3109/0284186X.2011.573626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muñoz Madero, V1, Ortega Pérez G. Electrochemotherapy for treatment of skin and soft tissue tumours. Update and definition of its role in multimodal therapy. Clin. Transl. Oncol. 2011;13:18–24. doi: 10.1007/s12094-011-0612-2. [DOI] [PubMed] [Google Scholar]
- 25.Reinhold U. Electrochemotherapy for primary skin cancer and skin metastasis related to other malignancies. Anticancer Drugs. 2011;22(8):711–718. doi: 10.1097/CAD.0b013e32834618da. [DOI] [PubMed] [Google Scholar]
- 26.Skarlatos I, et al. Electrochemotherapy in cancer patients: first clinical trial in Greece. In Vivo. 2011;25:265–274. [PubMed] [Google Scholar]
- 27.Cavalcanti A, Souadka A, Mateus C, Mir L, Robert C. Clinical experience with electrochemotherapy (ECT) in the skin melanoma metastases. Eur. J. Surg. Oncol. 2010;36:9. [Google Scholar]
- 28.Edhemović I, Brecelj E, Gašljević G, et al. Intraoperative electrochemotherapy of colorectal liver metastases. J. Surg. Oncol. 2014;110:320–327. doi: 10.1002/jso.23625. [DOI] [PubMed] [Google Scholar]
- 29.Tauceri F, Mura G, Roseano M, Framarini M, Ridolfi L, Verdecchia GM. Surgery and adjuvant therapies in the treatment of stage IV melanoma: our experience in 84 patients. Langenbecks Arch. Surg. 2009;394(6):1079–1084. doi: 10.1007/s00423-008-0312-8. [DOI] [PubMed] [Google Scholar]
- 30.Edhemović I, Gadžijev EM, Brecelj E, et al. Electrochemotherapy: a new technological approach in treatment of metastases in the liver. Technol. Cancer Res. Treat. 2011;10:475–485. doi: 10.7785/tcrt.2012.500224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mali B, Jarm T, Snoj M, Serša G, Miklavčič D. Antitumor effectiveness of electrochemo-therapy: a systematic review and meta-analysis. Eur. J. Surg. Oncol. 2013;39:4–16. doi: 10.1016/j.ejso.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 32.Campana LG, Mocellin S, Basso M, et al. Bleomycin-based electrochemotherapy: clinical outcome from a single institution's experience with 52 patients. Ann. Surg. Oncol. 2009;16:191–199. doi: 10.1245/s10434-008-0204-8. [DOI] [PubMed] [Google Scholar]
- 33.Sanki A, Kam PC, Thompson JF. Long-term results of hyperthermic, isolated limb perfusion for melanoma: a reflection of tumor biology. Ann. Surg. 2007;245:591–596. doi: 10.1097/01.sla.0000251746.02764.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Möller MG, Salwa S, Soden DM, O'Sullivan GC. Electrochemotherapy as an adjunct or alternative to other treatments for unresectable or in-transit melanoma. Expert Rev. Anticancer Ther. 2009;9(11):1611–1630. doi: 10.1586/era.09.129. [DOI] [PubMed] [Google Scholar]
- 35.Quaglino P, Mortera C, Osella-Abate S, et al. Electrochemotherapy with intravenous bleomycin in the local treatment of skin melanoma metastases. Ann. Surg. Oncol. 2008;15:2215–2222. doi: 10.1245/s10434-008-9976-0. [DOI] [PubMed] [Google Scholar]
- 36.Kis E, Olah J, Ocsai H, et al. Electrochemotherapy of cutaneous metastases of melanoma. A case series study and systematic reviewe of the evidence. Dermatol. Surg. 2011;37:816–824. doi: 10.1111/j.1524-4725.2011.01951..x. [DOI] [PubMed] [Google Scholar]
- 37.Snoj M, Cemazar M, Srnovrsnik T, Kosir SP, Sersa G. Limb sparing treatment of bleeding melanoma recurrence by electrochemotherapy. Tumori. 2009;95:398–402. doi: 10.1177/030089160909500324. [DOI] [PubMed] [Google Scholar]
- 38.Gehl J, Geertsen PF. Efficient palliation of haemorrhaging malignant melanoma skin metastases by electrochemotherapy. Melanoma Res. 2000;10:585–589. doi: 10.1097/00008390-200012000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Jarm T, Cemazar M, Miklavčič D, Sersa G. Antivascular effects of electrochemotherapy: implications in treatment of bleeding metastases. Expert Rev. Anticancer Ther. 2010;10(5):729–746. doi: 10.1586/era.10.43. [DOI] [PubMed] [Google Scholar]
- 40.Kaehler KC, Egberts F, Hauschild A. Electrochemotherapy in symptomatic melanoma skin metastases: intraindividual comparison with conventional surgery. Dermatol. Surg. 2010;6(7):1200–1202. doi: 10.1111/j.1524-4725.2010.01608.x. [DOI] [PubMed] [Google Scholar]
- 41.Miklavčič D, Serša G, Brecelj E, et al. Electrochemotherapy: technological advancements for efficient electroporation-based treatment of internal tumors. Med. Biol. Eng. Comput. 2012;50(12):1213–1225. doi: 10.1007/s11517-012-0991-8. [DOI] [PMC free article] [PubMed] [Google Scholar]