SUMMARY
Basal cell carcinoma (BCC) is the most common skin cancer in Caucasian population. Surgical excision is the gold standard treatment for BCC. Secondary surgical approach in patients presenting surgical scars after multiple surgical excisions or submitted to radiotherapy without obtaining a safe clearance margin, should be avoided. In recent years the use of electrochemotherapy (ECT) in head and neck cancers using intravenous bleomycin was specifically addressed and BCC resulted to be among tumors with the best response to ECT. We report a case of a recurrent nasal BCC treated with ECT with a complete regression of lesions after 8 weeks and a disease free period of 7 months. ECT is a good palliative treatment not affecting survival rate but improving quality of life in patients.
KEYWORDS : basal cell carcinoma, bleomycin, electrochemotherapy, electroporation, ESOPE, skin cancer
Practice points.
Introduction
Basal cell carcinoma is the most common skin cancer in the Caucasian population, mostly located in the head and neck region.
Surgical resection is the gold standard for basal cell carcinoma treatment but it is not indicated to treat recurrent tumors.
Case report
A 63 year old patient with recurrent nasal basal cell carcinoma treated with electrochemotherapy.
Complete regression of lesions after 8 weeks, disease free after 7 months.
Discussion
Electrochemotherapy using bleomycin is an alternative to surgery in the treatment of nonmelanoma head and neck cancer.
European Standard Operating Procedures of Electrochemotherapy study showed a complete response in about 73% patients while an objective response was recorded in 85% of cases.
Conclusion
Electrochemotherapy is usually well accepted because it uses a low chemotherapy dose, it is repeatable, it is safe and well tolerated by patients, without important side effects, with good long term results.
Basal cell carcinoma (BCC) is the most common skin cancer in Caucasian population [1]; its incidence, as well as that of the other nonmelanoma skin cancers, is progressively increasing particularly among individuals with fair skin and is considerably high in the elderly. Three major clinical variables of BCC are identified: nodular, superficial and morpheaform. Four histological subtypes are defined: superficial, nodular, infiltrative and morpheaform [2]. Superficial spreading BCC represents the most common subgroup, occurring in about 15– 25% of patients [1]. This neoplasm appears to be related to acute exposure to sunlight [3] but, together with sun exposure, immunosuppression is another important factor in tumor pathogenesis, whereas lifestyle factors do not appear to have a major role. Most of the tumors are located in the head and neck region as these are the more sun exposed regions of the body but BCC may often occur on other cutaneous areas chronically exposed to sun, like trunk and upper and lower limbs [4,5]. Although most BCCs are indolent, metastases occur in rare cases [6,7]. Surgical resection with an adequate margin of normal tissue remains the gold standard for treatment. As a matter of fact recurrence rates reported are around 10% when a BCC is completely excised as compared with recurrence rates of over 30% when a lesion is incompletely excised. Mohs micrographic surgery is typically utilized for high-risk lesions in critical anatomic areas [8]. Alternative treatment modalities exist in selected cases, including radiotherapy (RT), cryotherapy, photodynamic therapy, topical imiquimod, topical 5-fluorouracil [9]. Recently, the electrochemotherapy (ECT) using bleomycin is being used as a new technique in order to evaluate and confirm its efficacy and safety in the treatment of nonmelanoma head and neck cancers [10]. ECT is an anticancer treatment that combines the use of specific chemotherapy drugs, which have an intracellular target and low membrane permeability, with the application of electric pulses (electroporation) directly into the tumors to increase cells’ drug uptake [11].
Case report
We report the case of a 63 years old male patient with no comorbidities.
Starting from 1998, the patient underwent multiple surgical excisions for recurrent BCC on nasal pyramid and right nasal wing. In 2002, he was treated with RT and phototherapy (PT) which was discontinued after the second session since the patient was not compliant, referring to unsustainable pain during the treatment. Other medical history information was not available.
The patient arrived at our institute in October 2013, 3 months after the last PT session, presenting 3 new skin lesions on nasal pyramid.
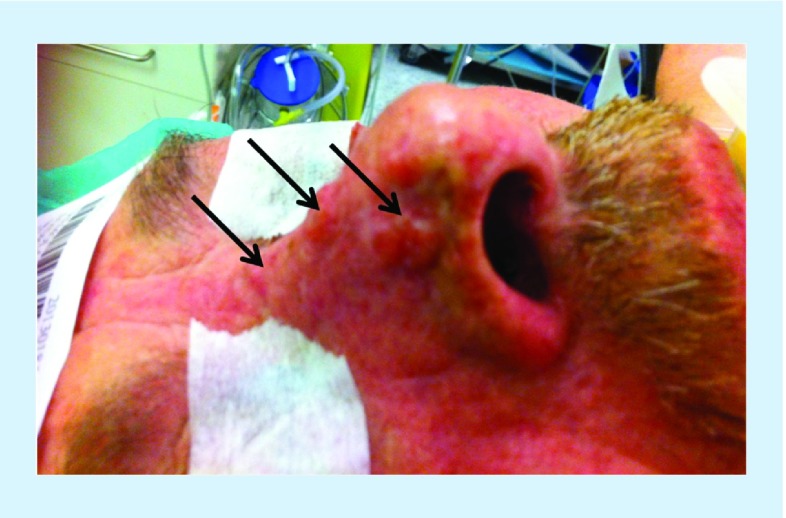
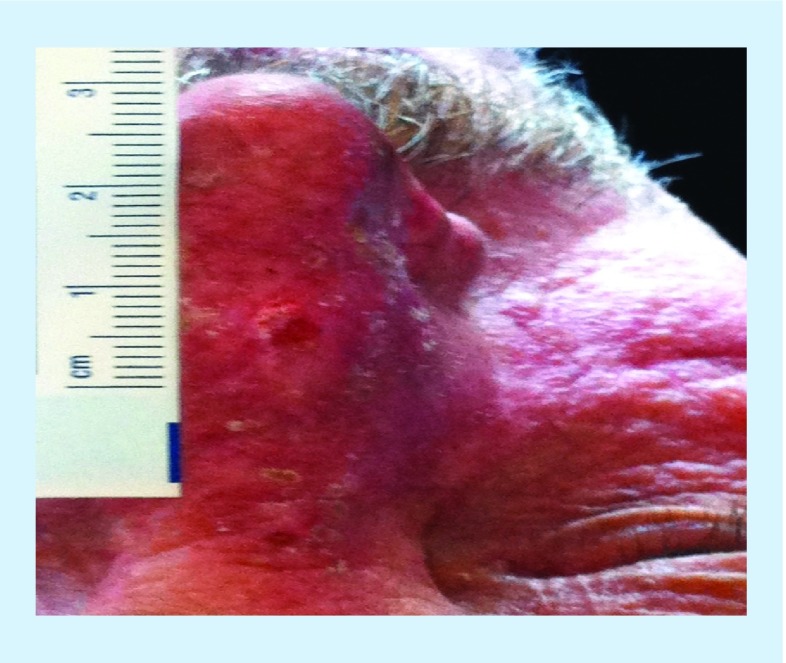
Physical examination showed multiple surgical scars and two nodules on the nasal pyramid cranially and caudally (with a diameter of 4 and 8 mm, respectively) and a third nodule (diameter 7 mm) on the right nasal wing (Figures 1 & 2).
Figure 1. . Pretreatment situation: note the three nodules in the nasal area (arrows).
Figure 2. . Pretreatment situation: note the 8 mm nodule on the nasal pyramid and the patient's skin after multiple surgical excisions, radiotherapy and phototherapy.
After a multidisciplinary evaluation with plastic surgeons, we considered a conventional surgical excision with skin graft as a procedure associated with a high risk of unsuccessful results, since the patient has been already treated with surgery followed by RT and PT on the tissues of the nasal area.
Thus we decided to propose the patient for a palliative ECT treatment on the three nasal nodules. The procedure was performed according to the European Standard Operating Procedures of Electrochemotherapy (ESOPE) [12]. Intravenous bleomycin infusion of 15.000 IU/m2 was administered 8 min before delivery of electric pulses under general anesthesia by means of a hexagonal electrode (length 25 mm) connected to an electric pulses generator (Cliniporator™) [13]. The lesions were treated by multiple direct insertions of the electrode completed within 28 min of bleomycin infusion. A full coverage of the lesions was obtained and the margins were treated up to 0.5 cm from the lesions.
Procedure was well tolerated and patient was discharged on postoperative day (POD) 1 with no postoperative complication and a satisfying pain control (Numeric Rate Scale [NRS] <3 not requiring pain killer administration). Local application of antibiotic cream was prescribed for the following 2 weeks to achieve a complete skin healing.
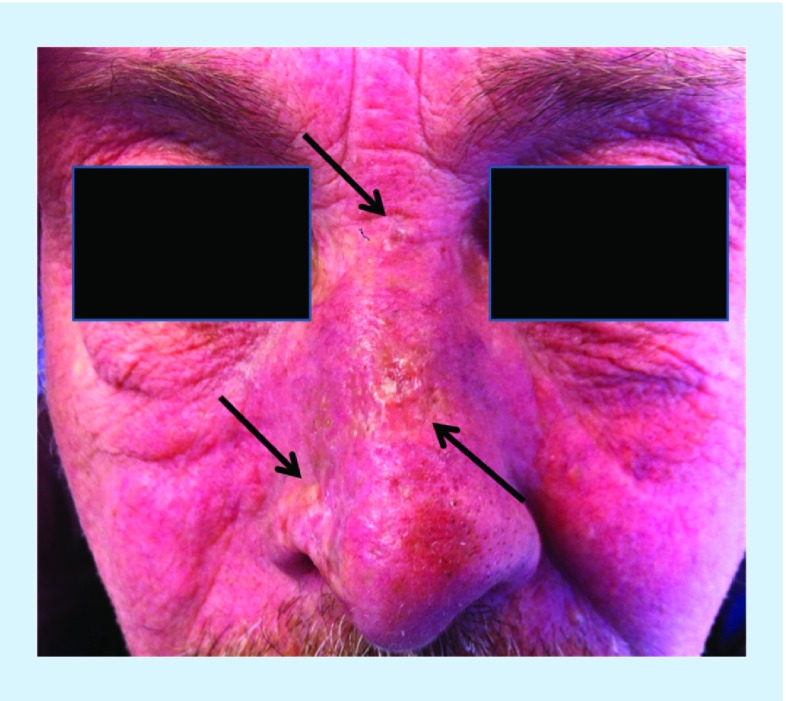
First re-evaluation was performed on POD 15 with initial good result: initial reduction of skin lesion diameter, no skin ulcers, redness or swelling (Figure 3).
Figure 3. . Evaluation on POD 15: initial regression of the lesions.
Second re-evaluation was performed 8 weeks after procedure with patient presenting a complete BCC regression (Figure 4). Up to date (after 7 months follow-up) the patient is disease-free.
Figure 4. . Evaluation after 8 weeks: complete basal cell carcinoma regression.
Discussion
Surgical excision is the most common treatment for BCC. The 5-year cure rates obtained with this procedure exceed 95% and approach 99% when resection margins are clean to histological examination [14]. Since surgery has a curative intent, it is very important to achieve negative clearance margins. Thus when planning a surgical excision of a BCC, the site of primary tumor, the size, the clinical type, as well as the anatomic development of local recurrences should be carefully taken into consideration. Excision margins of 5 mm are recommended, although small lesions may be managed with closer margin excision and still have a 95% cure rate, while large lesions may require wider margins because positivity of resection margin and recurrence rates increase with the increasing of tumor size [14]. If surgery is considered the BCC treatment gold standard, secondary surgical approach in patients presenting surgical scars after multiple surgical excisions for BCC local relapses or submitted to RT without obtaining a safe clearance margin, should be possibly avoided.
As a matter of fact it must be considered that ionizing radiation either directly damages the genome or injures the DNA through the production of free radicals. The end point of chronic radiation damage is a no healing ulcer; therefore few surgical procedures are performed on patients with acutely radiated tissues. The greater concern lies with patients with chronic radiation damage, who show a relevant rate of postoperative infection in previously irradiated sites [15]. Thus, surgery for patients previously submitted to RT should be approached cautiously.
In recent years the evaluation of the clinical activity of ECT in head and neck cancers using intravenous bleomycin was specifically addressed [12]. This technique is based on the concept that electroporation, obtained by the application of electric fields, temporarily increases the permeability of the cell membrane and allows the diffusion of different drugs in the tumor cells. ECT standardization was developed through a multicenter study (ESOPE) [12]. In this study the treatment response was tested according to the tumor type, the drug used, the route of its administration and the type of electrodes used. A complete response was obtained in about 73% of patients, while an objective response was recorded in 85% of cases, irrespectively from the tumor histology, the type of drug and the route of administration. The best local tumor control rate for ECT (88%) was achieved with bleomycin given intravenously [11,12,14–20]. The BCCs resulted to be among tumors with the best response to ECT in literature [13,19–22].
The use of ECT found indications for primary or relapsing tumors of the skin or subcutaneous tissue and the sizes of the treated lesions varied from few millimeters to several centimeters [12].
Conclusion
In the reported case, we obtained a high local response on recurrent BCC small lesions on the nose, confirming that lesion size represents a relevant predictive parameter for ECT response. This procedure is usually well accepted because it represents a simple and repeatable treatment based on the use of low chemotherapy doses, safe and well tolerated by patients, without important side effects [13]. Our results show that ECT could represent an effective alternative treatment to surgery, RT and PT to achieve local tumor control in cases of BCC, with a good tolerance for patients.
Future perspective
Electrochemotherapy is a safe and effective treatment for skin cancer and cutaneous and subcutaneous metastases [13,19–22]. The use of ECT does not change the natural history of the disease and does not modify the extent of survival, but provides a palliative and provisional effect and it is able to improve quality of life in patients. This technique seems to be particularly suitable for some kind of skin tumors like BCC that usually has only a local malignancy.
Footnotes
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of non melanoma skin cancer. Br. J. Dermatol. 2012;166(5):1069–1080. doi: 10.1111/j.1365-2133.2012.10830.x. [DOI] [PubMed] [Google Scholar]
- 2.Trakatelli M, Morton C, Nagore E, et al. Update of the European guidelines for basal cell carcinoma management. Eur. J. Dermatol. 2014 doi: 10.1684/ejd.2014.2271. Epub ahead of print. [DOI] [PubMed] [Google Scholar]; • Practical guidelines on basal cell carcinoma management.
- 3.Lovatt TJ, Lear JT, Bastrilles J, et al. Associations between ultraviolet radiation, basal cell carcinoma site and histology, host characteristics, and rate of development of further tumors. J. Am. Acad. Dermatol. 2005;52:468–473. doi: 10.1016/j.jaad.2004.08.060. [DOI] [PubMed] [Google Scholar]
- 4.Reinau D, Surber C, Jick SS, Meier CR. Epidemiology of basal cell carcinoma in the United Kingdom: incidence, lifestyle factors, and comorbidities. Br. J. Cancer. 2014 doi: 10.1038/bjc.2014.265. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richmond-Sinclair NM, Pandeya N, Ware RS, et al. Incidence of basal cell carcinoma multiplicity and detailed anatomic distribution: longitudinal study of an Australian population. J. Invest. Dermatol. 2009;129(2):323. doi: 10.1038/jid.2008.234. [DOI] [PubMed] [Google Scholar]
- 6.Rubin AI, Chen EH, Ratner D. Basal cell carcinoma. N. Engl. J. Med. 2005;353:2262–2269. doi: 10.1056/NEJMra044151. [DOI] [PubMed] [Google Scholar]
- 7.McCusker M, Basset-Seguin N, Dummer R, et al. Metastatic basal cell carcinoma: prognosis dependent on anatomic site and spread of disease. Eur. J. Cancer. 2014;50(4):774–783. doi: 10.1016/j.ejca.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Schell AE, Russell MA, Park SS. Suggested excisional margins for cutaneous malignant lesions based on Mohs micrographic surgery. JAMA Facial Plast. Surg. 2013;15(5):337–343. doi: 10.1001/jamafacial.2013.1011. [DOI] [PubMed] [Google Scholar]; • The importance of clear margins in surgical resection for cutaneous malignant lesions.
- 9.Clark CM, Furniss M, Mackay-Wiggan JM. Basal cell carcinoma: an evidence-based treatment update. Am. J. Clin. Dermatol. 2014;15(3):197–216. doi: 10.1007/s40257-014-0070-z. [DOI] [PubMed] [Google Scholar]
- 10.Gargiulo M, Papa A, Capasso P, Moio M, Cubicciotti E, Parascandolo S. Electrochemotherapy for non-melanoma head and neck cancers: clinical outcomes in 25 patients. Ann. Surg. 2012;255(6):1158–1164. doi: 10.1097/SLA.0b013e31824f68b2. [DOI] [PubMed] [Google Scholar]; •• A small but significant example of electrochemotherapy use on nonmelanoma skin cancer of head and neck.
- 11.Mir LM, Gehl G, Sersa G, et al. Standard operating procedures of the electrochemotherapy: instructions for the use of bleomyicin or cisplatin administered either systemically or locally and electric pulses delivered by the Cliniporator™ by means of invasive or noninvasive electrodes. EJC Supplements. 2006;(4):14–25. [Google Scholar]
- 12.Marty M, Sersa G, Garbay JR, et al. Electrochemotherapy: an easy, highly effective and safe treatment of cutaneous and subcutaneous metastases: results of ESOPE (European Standard Operating Procedures of Electrochemotherapy) study. Eur. J. Cancer. 2006;4(Suppl.):3–13. [Google Scholar]; •• Results from the ESOPE study: indication and outcome on electrochemotherapy for cutaneous and subcutaneous metastases.
- 13.IGEA clinical biophysics. www.igea.it
- 14.Goldberg DP. Assessment and surgical treatment of basal cell skin cancer. Clin. Plast. Surg. 1997;24:673. [PubMed] [Google Scholar]
- 15.Drake DB, Oishi SN. Wound healing considerations in chemotherapy and radiation therapy. Clin. Plast. Surg. 1995;22:31. [PubMed] [Google Scholar]
- 16.Silverman MK, Kopf AW, Bart RS, et al. Recurrence rates of treated basal cell carcinomas. Part 3: surgical excision. J. Dermatol. Surg. Oncol. 1992;18:471–476. doi: 10.1111/j.1524-4725.1992.tb03307.x. [DOI] [PubMed] [Google Scholar]
- 17.Campana LG, Valpione S, Mocellin S, et al. Electrochemotherapy for disseminated superficial metastases from malignant melanoma. Br. J. Surg. 2012;99(6):821–830. doi: 10.1002/bjs.8749. [DOI] [PubMed] [Google Scholar]
- 18.Salwa SP, Bourke MG, Forde PF, et al. Electrochemotherapy for the treatment of ocular basal cell carcinoma; a novel adjunct in the disease management. J. Plast. Reconstr. Aesthet. Surg. 2014;67(3):403–406. doi: 10.1016/j.bjps.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 19.Mevio N, Bertino G, Occhini A, et al. Electrochemotherapy for the treatment of recurrent head and neck cancers: preliminary results. Tumori. 2012;98(3):308–313. doi: 10.1177/030089161209800305. [DOI] [PubMed] [Google Scholar]
- 20.http://clinicaltrials.gov/show/NCT00198276 Study using the MedPulser electroporation system with bleomycin to treat cutaneous and subcutaneous cancer.
- 21.www.electroporation.net Electrochemotherapy for primary basal cell carcinoma and primary squamous cell carcinoma.
- 22.www.nice.org.uk Interventional procedure overview of electrochemotherapy for primary basal cell carcinoma and primary squamous cell carcinoma.