Intraductal papillary neoplasm of the biliary tract (IPNB) is a rare clinical entity that may present with mucobilia and has a high risk of malignant transformation to cholangiocarcinoma. These papillary neoplasms are characterized by superficial spread, dilated bile ducts, and multifocal distribution. Surgery is the treatment of choice. Endoscopic therapy may offer palliation.
An 86-year-old woman presented to the emergency department with obstructive jaundice and sepsis due to ascending cholangitis. Her initial MRCP revealed dilated bile ducts without any mass or stone in the ductal system (Fig. 1A). ERCP revealed soft filling defects in the common bile duct consistent with mucobilia (Fig. 1B). The adult gastroscope was introduced into the common bile duct via fluoroscopic guidance (Fig. 1C) and into the common hepatic duct (Fig. 1D). No mass lesions were seen following duct clearance. Unfortunately, she was not a surgical candidate because of her multiple medical comorbidities. Despite endoscopic therapy, the patient experienced multiple episodes of recurrent ascending cholangitis resulting from mucus impaction. On follow-up endoscopic evaluation, per-oral cholangioscopy (POC) with a GIF 180 adult gastroscope (Olympus, Center Valley, Pa, USA) demonstrated mucobilia, dilatated bile ducts, and nodularities in the cystic duct (Fig. 1E). Analysis of biopsy specimens revealed an intraductal papillary neoplasm with low-grade dysplasia from the nodularities of the cystic duct (Fig. 1F). Endoscopic treatment modalities were discussed with the patient to prevent recurrent mucobilia and cholangitis. Argon plasma coagulation (APC) was chosen (Video 1, available online at www.VideoGIE.org).
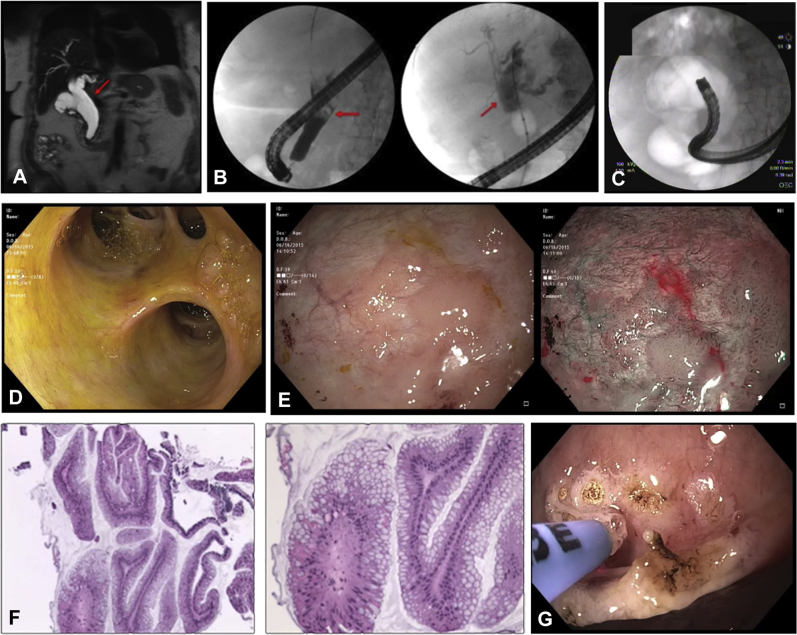
Figure 1.
A, MRCP view showing dilated common bile and hepatic ducts. B, ERCP view showing mucobilia as a filling defect that was aggressively cleared (left). No mass lesion was seen on occlusion cholangiogram following clearance (right). C, Fluoroscopic image of adult gastroscope in the common bile duct. D, Endoscopic view showing the common hepatic duct and bifurcations. E, Endoscopic view showing nodularities of the cystic duct (left) with narrow-band imaging (right). F, Staining of biopsy specimen showing intraductal papillary neoplasm of the bile duct, gastric type. Mucinous epithelium-forming papillary structures also seen here (left, H&E, orig. mag. ×10; right, H&E, orig. mag. ×20). G, Post-argon plasma coagulation treatment of nodularities.
An APC probe was set at 15 to 25 watts, in forced mode, with effect 1, and 0.8 to 1.2 L/min. Visible cystic duct nodularities received treatment with APC (Fig. 1G). Pulses were followed by suction to reduce argon gas distention. At a 14-week follow-up visit, ERCP and POC showed significant reduction in mucobilia, and a scar was seen at the sites of previous treatment. The remaining areas of nodularity were treated with APC. The patient has done well after therapy without recurrent symptoms.
IPNB is a rare disease entity with a high risk of malignant transformation, and, as such, surgical resection is the treatment of choice. However, nonsurgical candidates may benefit from minimally invasive endoscopic therapies. Nonsurgical management of biliary neoplasms with the use of APC is a well-tolerated and safe procedure. Endoscopic therapeutic strategies may improve morbidity and patient survival associated with IPNB.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Argon plasma coagulation treatment of intraductal papillary neoplasm of biliary tract.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Argon plasma coagulation treatment of intraductal papillary neoplasm of biliary tract.