A 62-year-old man with hepatitis C mediated Child’s A cirrhosis and severe chronic obstructive pulmonary disease presented for esophageal variceal screening with upper endoscopy. In addition to small varices, a small 6-mm irregular lesion was found in the gastric fundus (Fig. 1), which underwent biopsy and was found to be a gastric adenocarcinoma with signet ring features. Staging CT of the chest, abdomen, and pelvis did not reveal any distant metastases or other masses, although we did observe marked intra-abdominal vascular collaterals and splenomegaly (Fig. 2). EUS revealed a mucosal mass extending into the level of the submucosa, without adjacent lymphadenopathy. Surgical consultation was obtained, and, given the small size of the lesion and the significant comorbidities associated with an open total gastrectomy, the patient opted for an attempt at endoscopic removal with the full-thickness resection device (FTRD).
Figure 1.

Endoscopic view of adenocarcinoma in the gastric fundus.
Figure 2.

Representative axial CT image showing sequelae of cirrhosis and portal hypertension.
Using an Olympus 1T190 endoscope (Olympus Corp, Tokyo, Japan), we identified the lesion and marked the borders with cautery (Fig. 3). The 1T endoscope was removed, and the Olympus 2T180 endoscope was fitted with the FTRD. Despite the size of the FTRD, there was no difficulty passing it through the oropharynx, through the esophagus, and into the stomach. The lesion was identified again. Using the tissue grasper, we drew the lesion into the cap of the device (Fig. 4), and the clip was deployed rapidly, followed by resection of the tissue by means of snare cautery (VIO 300, Endocut Q1/4/1) (Video 1, available online at www.VideoGIE.org). The lesion was then removed from the stomach and sent en bloc for pathologic evaluation (Fig. 5). The excision site was inspected, no adverse event was noted (Fig. 6), and the patient was discharged home after overnight observation.
Figure 3.

Marking the periphery of the lesion with cautery.
Figure 4.

Pulling the lesion into the cap of the device with the tissue grasper.
Figure 5.

Mucosal surface of resected specimen.
Figure 6.

Endoscopic view of resection site.
Gross examination of the specimen revealed the presence of muscularis propria (Fig. 7), and microscopic evaluation, through the aid of hematoxylin and eosin stain, revealed 3-mm negative margins with the tumor invading into the submucosa without muscularis propria involvement (Figs. 8 and 9). Pathologic staging was determined to be pT1b pNxMx.
Figure 7.
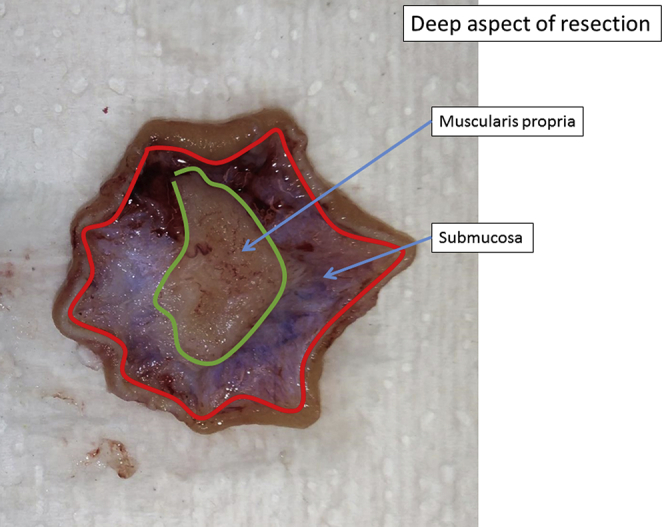
Deep aspect of resected specimen.
Figure 8.

Histologic sample showing negative margin (H&E, orig. mag. ×40).
Figure 9.

Histologic sample showing lesion confined to the submucosa (H&E, orig. mag. ×100).
Endoscopic resection of early gastric adenocarcinoma has been shown to be of similar efficacy compared with gastrectomy in the appropriately selected patient.1 Generally, a candidate for endoscopic resection should have a tumor <20 mm confined to the mucosa, with absence of venous or lymphatic invasion, and of intestinal-type adenocarcinoma.2 On the basis of the presence of signet ring features, this patient did not meet the standard criteria but did fall within the proposed expanded criteria, including larger well-differentiated tumors and the inclusion of undifferentiated-type adenocarcinoma <20 mm, confined to the upper 0.5 mm of the submucosa without lymphovascular invasion.3 The expanded criteria are still considered investigational and are associated with increased, although still low, rates of lymph node metastasis.4 Determining whether a patient will fit within these criteria before endoscopic resection is undertaken remains challenging. EUS has, unfortunately, demonstrated limited ability in adequately delineating T1a and T1b lesions.5
In this surgically unfit patient with likely submucosal involvement based on EUS evaluation, a novel device was used to obtain broader pathologic margins than would have been possible by endoscopic submucosal dissection, and we demonstrated complete resection to the level of the muscularis propria. Of note, this was an off-label use of this device in the United States because it is currently approved only for use in the colon. Although no immediate adverse events occurred and negative margins were achieved, close endoscopic and radiographic follow-up remain of paramount importance because a risk for local or metachronous recurrence persists.6
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Endoscopic resection of a gastric adenocarcinoma by use of a full-thickness resection device.
References
- 1.Choi K.S., Jung H.Y., Choi K.D. EMR versus gastrectomy for intramucosal gastric cancer: comparison of long-term outcomes. Gastrointest Endosc. 2011;73:942–948. doi: 10.1016/j.gie.2010.12.032. [DOI] [PubMed] [Google Scholar]
- 2.Min Y.W., Min B.H., Lee J.H. Endoscopic treatment for early gastric cancer. World J Gastroenterol. 2014;20:4566–4573. doi: 10.3748/wjg.v20.i16.4566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahn J.Y., Jung H.Y., Choi K.D. Endoscopic and oncologic outcomes after endoscopic resection for early gastric cancer: 1370 cases of absolute and extended indications. Gastrointest Endosc. 2011;74:485–493. doi: 10.1016/j.gie.2011.04.038. [DOI] [PubMed] [Google Scholar]
- 4.Lee J.H., Choi M.G., Min B.H. Predictive factors for lymph node metastasis in patients with poorly differentiated early gastric cancer. Br J Surg. 2012;99:1688–1692. doi: 10.1002/bjs.8934. [DOI] [PubMed] [Google Scholar]
- 5.Mocellin S., Pasquali S. Diagnostic accuracy of endoscopic ultrasonography (EUS) for the preoperative locoregional staging of primary gastric cancer. Cochrane Database Syst Rev. 2015 Feb 6:CD009944. doi: 10.1002/14651858.CD009944.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manner H., Rabenstein T., May A. Long-term results of endoscopic resection in early gastric cancer: the Western experience. Am J Gastroenterol. 2009;104:566–573. doi: 10.1038/ajg.2008.151. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic resection of a gastric adenocarcinoma by use of a full-thickness resection device.


