Abstract
Facing competing demands with limited resources following release from prison, people who inject drugs (PWID) may neglect health needs, with grave implications including relapse, overdose, and non-continuous care. We examined the relative importance of health-related tasks after release compared to tasks of everyday life among a total sample of 577 drug users incarcerated in Ukraine, Azerbaijan, and Kyrgyzstan. A proxy measure of whether participants identified a task as applicable (easy or hard) versus not applicable was used to determine the importance of each task. Correlates of the importance of health-related reentry tasks were analyzed using logistic regression, with a parsimonious model being derived using Bayesian lasso method. Despite all participants having substance use disorders and high prevalence of comorbidities, participants in all three countries prioritized finding a source of income, reconnecting with family, and staying out of prison over receiving treatment for substance use disorders, general health conditions, and initiating methadone treatment. Participants with poorer general health were more likely to prioritize treatment for substance use disorders. While prior drug injection and opioid agonist treatment (OAT) correlated with any interest in methadone in all countries, only in Ukraine did a small number of participants prioritize getting methadone as the most important post-release task. While community-based OAT is available in all three countries and prison-based OAT only in Kyrgyzstan, Kyrgyz prisoners were less likely to choose help staying off drugs and getting methadone. Overall, prisoners consider methadone treatment inapplicable to their pre-release planning. Future studies that involve patient decision-making and scale-up of OAT within prison settings are needed to better improve individual and public health.
Keywords: People who inject drugs, Prisoners, Incarceration, Post-release challenges, HIV, Opioid agonist treatment, Methadone, Eastern Europe and Central Asia
Introduction
Eastern Europe and Central Asia (EECA) remains the only region globally where HIV incidence and mortality continue to increase [1]. There are numerous economic, political, programmatic, and social reasons for the ongoing volatile epidemic in the region, including suboptimal HIV prevention and treatment in prisons [2]. Although diverse, EECA countries have commonalities in drug policy and addiction treatment practices rooted in shared post-Soviet value systems that prioritize collective needs over individual autonomy [3]. Harsh policies criminalizing drug use [4] result in the concentration of people with or at high risk for HIV in prisons [2, 5], where high-risk behavior such as drug injection often continues [6, 7]. Nationally representative surveys of prison populations show that HIV prevalence is 12- [8], 51-[9], and 37-times [10] greater in prisons than in the community in Ukraine, Kyrgyzstan, and Azerbaijan, respectively [2]. As drug use continues to remain largely criminalized, implementation and scale-up in prisons of evidence-based strategies for HIV prevention and treatment will be crucial tools for curbing the epidemic [2, 7, 11].
Nearly all prisoners, including those with substance use disorders, return to their communities, mostly in urban settings. Thus, transitioning prisoners contribute greatly to urban health and health service delivery. As incarcerated individuals (including recidivists) contemplate release, many experience a heightened sense of optimism about “renewing” their life, known as penal optimism [12], which extends to feeling optimistic about recovery and community reintegration [13]. Penal optimism is considered a psychological phenomenon of planning fallacy, when individuals have excessive optimism bias towards the future, exaggerating their abilities, underestimating their challenges, and avoiding difficult realities [14, 15]. Similarly, during imprisonment, prisoners often minimize challenges that may impede their plans to make positive changes in their lives after release [16].
Qualitative research in the USA and elsewhere suggests that former prisoners often find themselves “in a world of chaos” characterized by competing demands on their limited resources, with basic needs like food and shelter taking priority [17]. For people who inject drugs (PWID), allowing one’s health needs to fall off this list of key priorities has grave implications for transitional care, particularly for addiction treatment and continued recovery [18, 19]. Discontinuity of care [20–22], relapse to drug use, overdose, and resultant death are common immediately after release [23]. Risk of death from opioid overdose increases more than sevenfold in the first 2 weeks after release [24], and 1 in 200 prisoners with a history of injecting opioids dies from overdose in the month following release [23, 25, 26]. Indeed, the only evidence-based therapy for opioid use disorder in prisoners is to use pharmacological treatment with methadone or buprenorphine within prison and continue it post-release.
Aside from overdose risk, post-incarceration relapse increases exposure to HIV infection [27]. Studies [28] show that rates of engagement in HIV care and receipt of ART decline more than twofold after release [21, 22, 28]. A comprehensive review that included EECA countries reported that ART adherence drops after release, especially for women, due to relapse to substance use, unstable housing and unemployment, reduced access to health care, and inability to access ART in the community [29]. To develop effective transitional programs from prison to community care, there is a need to better prioritize health tasks in prison that may shape planning for continued healthcare after release. Despite evidence that while in prison, individuals underestimate the difficulty of meeting post-release health challenges, there are no data on whether individuals incorporate their health status into how they prioritize their post-release needs, despite the overwhelming evidence that treatment for substance use disorders within prison and continued after release is associated with the best possible health, psychological, legal, and social integration outcomes.
In this study, we examine a cross-sectional survey of prisoners within 6 months of release that met criteria for substance use disorders. Examining three EECA countries, we examine the relative importance of health-related tasks compared to tasks of everyday life, explore the correlates of prioritizing health-related tasks, and consider whether there are meaningful differences in findings by country.
Methods
Study Design
The design for the parent study has been described previously in each of the three countries: Ukraine [8], Kyrgyzstan [9], and Azerbaijan [10]. Briefly, using a random sampling scheme [30], prisoners being released within 6 months were recruited to participate from all prisons, excluding juveniles and hospital prisons. Both first time and recidivist prisoners were included. The target size of the sample was based on estimates of the number of inmates in non-specialized facilities in each country meeting eligibility criteria, proportional to the number of prisoners within 6 months of release in each facility [8–10].
Following informed consent, respondents answered survey questions (~ 45 min) using computer-assisted structured interviews (CASI) that included demographic characteristics; criminal justice history; social circumstances prior to incarceration; pre-incarceration substance use; self-perceived health status; sexual and drug risk behaviors prior to incarceration; validated measures of alcohol use disorder, depression, and social support; and reentry challenges and likelihood of recidivism. All instruments were translated and back-translated into both Russian and Ukrainian, Kyrgyz, and Azerbaijani, respectively [31]. All participants were then tested for HIV (followed by a second confirmatory HIV and CD4 testing), hepatitis C virus (HCV), hepatitis B virus (HBV), and syphilis, counseled, and referred for treatment.
Among the combined sample of 1280 prisoners, 577 (45%) self-reported previous drug use aside from cannabis or alcohol, which was defined as having a substance use disorder, and were included in the current analysis; drug use in EECA is often under-reported unless it is non-recreational and regular. Drug use is the major risk factor for HIV in EECA and also for increased morbidity, mortality, and social harm after release in prisoner populations [27, 32].
Study Settings
Azerbaijan is an upper middle-income country [33] of 9.8 million people with ~ 40,000 prisoners. HIV prevalence is 37-fold higher in prisoners (3.7%) than in the community (0.1%). The predominant religion is Islam and there are estimated to be 71,283 PWID [34] with an HIV prevalence of 19 to 24% [35]. The coverage of OAT using methadone in Azerbaijan was 0.2% or 155 PWID in 2014, falling far below the WHO-recommended coverage of at least 20% [34].
Kyrgyzstan is a lower income country [33] of 6.1 million people with 10,195 prisoners [36]. About half of the population is Muslim. HIV prevalence in prisoners (10.3%) is 51-fold higher than in the community (0.2%) [9] and OAT is provided in prisons. The OAT program in Kyrgyzstan has about 1200 clients [37], with coverage at 18%.
Ukraine is a lower middle-income country [38] that is the most secular among the three included countries. Ukraine has a population of about 42 million and a prisoner population of about 60,000 [39]. HIV prevalence among prisoners (19.4%) is 12 times higher than in the community (1.63%) [8]. It is estimated that there are 340,000 PWID [40], mostly of opioids, with high prevalence of substance use disorders among incarcerated individuals [8].
While in all three countries opioid agonist therapy (OAT) was introduced as part of HIV prevention and harm reduction efforts [41, 42], the addiction treatment community has been slow to adopt it as evidence-based drug treatment. Azerbaijan has a small pilot OAT program in the community, and Ukraine offers OAT using buprenorphine and methadone only in the community with relatively low coverage, while Kyrgyzstan offers OAT both in the community and in prisons.
Data Analysis
Basic characteristics of study participants include: demographic characteristics; pre-incarceration income; recidivism; history of drug use and OAT; HIV, HCV, HBV, and syphilis test results; medical screening variables; and a set of validated screening instruments for alcohol use disorders using the AUDIT [43], depression using the CES-D 10 [44], health-related quality of life (HRQoL) using the MOS short form 36 (SF-36) [45], and social support [46]. An alcohol use disorder was met if the scores were 8 or higher for males and 4 or higher for females [47] and depression if the CES-D was 10 or greater [48]. The composite social support scale is an integer-valued measure and ranges from 1 (no support) to 5 (high support) [46].
To measure the general health status of the study participants, we constructed a multi-comorbidity index (MCI) as a weighted sum of the following conditions: asthma, skin ulcers, abscesses, arthritis/joint pain, gonorrhea and other STIs (except syphilis), seizures, high blood pressure, liver problems, pneumonia, cancer, heart disease, and tuberculosis. Weights were based on whether the condition is acute (1) or chronic (3) and symptomatic (1) versus asymptomatic (0). For example, an acute asymptomatic condition contributed a value of 1 to the multi-comorbidity index, and a presence of a chronic symptomatic condition added a value of 4 to the total. The total value of the MCI ranged from 0 to 26. HIV, HCV, HBV, and syphilis infections were analyzed separately and are not included in the index. The WHO Tuberculosis (TB) screening questionnaire captures the presence of TB symptoms based on self-report [49]. As recommended by the WHO for high prevalence settings, positive screening was defined as having a cough for at least 2 weeks or the presence of both sputum and unexplained weight loss (in the last 3 months) [49]. Because sensitivity is high for this symptom survey, those screening positive should undergo confirmatory testing to determine the need for treatment. Specificity, however, is low making this symptom survey not a true indicator of TB disease.
The outcomes of our analysis included: (1) assessment of each post-release task individually as very easy/easy/hard/very hard or not applicable and (2) identification of one most important post-release task. For the first outcome, categories “easy” and “very easy” were collapsed into “easy” and “hard” and “very hard” into “hard.” The list of potentially challenging post-release tasks was compiled based on previous research in this area [19, 50] and included a total of 18 items. Of these, health-related tasks included: getting access to HIV care, getting treatment for illnesses other than HIV, getting help staying off drugs, and getting OAT. Since the task of getting access to HIV care only applied to a small sub-sample, our analysis focused on the latter three potential challenges. To provide a comparison of how incarcerated individuals perceived the relative importance of their post-release tasks, we selected three “comparison” tasks of everyday life, namely: finding a job or a stable source of income, reuniting with family and/or friends, and staying out of prison following release.
We used a proxy measure for whether a task was perceived as important. This proxy measure identified a task as applicable (easy or hard) versus not applicable. Correlates of identifying a health-related task as applicable were analyzed using logistic regression, and this analysis was performed separately for the three health-related tasks of interest. A parsimonious model was derived using Bayesian lasso method [51]. This method provides a more conservative way to perform variable selection and estimation of regression coefficients compared to traditional stepwise methods [52].
Statistical analyses were performed in SPSS (version 22.0, Chicago, IL) and R (Foundation for Statistical Computing, Vienna, Austria). Significance of between-country differences was assessed using ANOVA and chi-squared test for continuous and categorical variables respectively. R Package “EBglmnet” [53] was used to implement Bayesian lasso, and we used three-level hierarchical priors with normal/exponential/gamma distributions to perform variable selection and estimation of regression coefficients and their 95% credible intervals.
Ethics Statement
This study was approved by both the Institutional Review Boards at the Yale University School of Medicine and Institutional Review Boards in Ukraine, Azerbaijan, and Kyrgyzstan. Further safety assurances were provided by the Office for Human Research Protections.
Results
Characteristics of the Participant Population
As seen in Table 1, there was substantial diversity between participants in Azerbaijan, Kyrgyzstan, and Ukraine for several characteristics: religion, education, rate of recidivism, history of OAT, physical and mental wellness scores, and results of screening for diseases such as tuberculosis and HIV. In Ukraine, almost 80% of participants completed high school or received higher education in comparison to just over half of participants in Kyrgyzstan and just over a third in Azerbaijan. The rate of recidivism was generally high in our sample but was the highest in Kyrgyzstan (80%), while in Ukraine and Azerbaijan, it was about half of participants. The duration of injection drug use was also high (15 years on average), being the highest in Azerbaijan. While more than half of participants in Ukraine and more than two thirds of participants in Azerbaijan reported moderate (1–14 days) to heavy (15–30 days) drug injection in the month prior to incarceration, about two thirds of participants in Kyrgyzstan stated they had not injected drugs in the month prior to incarceration. Over two thirds of Kyrgyzstan participants reported a history of participation in OAT in contrast to only 1% in Azerbaijan and 7.5% in Ukraine. Health-related quality of life (HRQoL) showed that the study population was sicker than the general population in all three countries. In all three countries, HRQoL for physical health was similar to the general population level, but for mental health, it was markedly lower. HIV prevalence was the highest in Ukraine at 23.8% (with 42% of HIV positive unaware of their status) and the lowest in Azerbaijan at 6.8%. The three countries were similar on other health indicators such as prevalence of depression, hepatitis B and C, and multi-comorbidity index (Table 1).
Table 1.
Characteristics of study participants (N = 577)
| Characteristic | Total N = 577 |
AZ N = 191 |
KYR N = 146 |
UA N = 240 |
p valuea |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 494 (85.6) | 179 (93.7) | 125 (85.6) | 190 (79.2) | < 0.001 |
| Female | 83 (14.4) | 12 (6.3) | 21 (14.4) | 50 (20.8) | |
| Age, years; mean (S.D.) | 34.9 (9.0) | 39.4 (8.1) | 36.5 (9.7) | 30.4 (6.9) | < 0.001 |
| Marital status | |||||
| Single | 360 (62.4) | 76 (39.8) | 95 (65.1) | 189 (78.8) | < 0.001 |
| Has a partner | 217 (37.6) | 115 (60.2) | 51 (34.9) | 51 (21.2) | |
| Religion | |||||
| Christian | 290 (50.3) | 0 (0.0) | 72 (49.3) | 218 (90.8) | < 0.001 |
| Muslim | 258 (44.7) | 186 (97.4) | 72 (49.3) | 0 (0.0) | |
| Other | 29 (5.0) | 5 (2.6) | 2 (1.4) | 22 (9.2) | |
| Education | |||||
| Completed high school | 341 (59.1) | 71 (37.2) | 83 (56.8) | 187 (77.9) | < 0.001 |
| Less than high school | 236 (40.9) | 120 (62.8) | 63 (43.2) | 53 (22.1) | |
| Income pre-incarceration | |||||
| Above poverty line | 279 (48.4) | 85 (44.5) | 92 (63.0) | 102 (42.5) | < 0.001 |
| Below poverty line | 298 (51.6) | 106 (55.5) | 54 (37.0) | 138 (57.5) | |
| Recidivism | |||||
| First time | 245 (42.5) | 97 (50.8) | 29 (19.9) | 119 (49.6) | < 0.001 |
| Previously incarcerated | 332 (57.5) | 94 (49.2) | 117 (80.1) | 121 (50.4) | |
| History of injecting drugs | |||||
| No | 114 (19.8) | 30 (15.7) | 37 (25.3) | 47 (19.6) | 0.088 |
| Yes | 463 (80.2) | 161 (84.3) | 109 (74.7) | 193 (80.4) | |
| Duration of injecting drug use, years (among 463 who reported injecting), mean (S.D.) | 15.4 (8.7) | 19.3 (8.6) | 15.0 (9.7) | 12.4 (7.0) | < 0.001 |
| Recent injecting drug use, 30 days prior to current incarceration | |||||
| None | 244 (42.3) | 55 (28.8) | 93 (63.7) | 96 (40.0) | < 0.001 |
| Moderate (1–14 days) | 186 (32.2) | 98 (51.3) | 26 (17.8) | 62 (25.8) | |
| Heavy (15–30 days) | 147 (25.5) | 38 (19.9) | 27 (18.5) | 82 (34.2) | |
| History of opioid drug use | |||||
| No | 126 (21.9) | 25 (13.1) | 39 (26.9) | 62 (25.8) | 0.003 |
| Yes | 450 (78.1) | 166 (86.9) | 106 (73.1) | 178 (74.2) | |
| History of being prescribed OAT | |||||
| No | 453 (78.5) | 189 (99.0) | 42 (28.8) | 222 (92.5) | < 0.001 |
| Yes | 124 (21.5) | 2 (1.0) | 104 (71.2) | 18 (7.5) | |
| Alcohol use disorderb | |||||
| No | 305 (52.9) | 152 (79.6) | 65 (44.5) | 88 (36.7) | < 0.001 |
| Yes | 272 (47.1) | 39 (20.4) | 81 (55.5) | 152 (63.3) | |
| Moderate to severe depressionc | |||||
| No | 345 (59.8) | 120 (62.8) | 82 (56.2) | 143 (59.6) | 0.464 |
| Yes | 232 (40.2) | 71 (37.2) | 64 (43.8) | 97 (40.4) | |
| Health-related quality of life: Physical Composite Score, mean (S.D.) | 48.0 (5.7) | 47.3 (4.7) | 44.9 (5.8) | 50.5 (5.3) | < 0.001 |
| Health-related quality of life: Mental Composite Score, mean (S.D.) | 41.9 (9.1) | 36.7 (6.5) | 38.3 (8.1) | 48.2 (7.4) | < 0.001 |
| Social Support, mean (S.D.)d | 3.0 (1.1) | 3.1 (1.1) | 2.8 (1.0) | 3.0 (1.1) | 0.009 |
| HIV status | |||||
| Negative | 481 (83.4) | 178 (93.2) | 120 (82.2) | 183 (76.2) | < 0.001 |
| Positive and aware | 58 (10.1) | 11 (5.8) | 14 (9.6) | 33 (13.8) | |
| Positive and unaware | 38 (6.6) | 2 (1.0) | 12 (8.2) | 24 (10.0) | |
| Hepatitis C status | |||||
| Negative | 137 (23.7) | 47 (24.6) | 38 (26.0) | 52 (21.7) | 0.585 |
| Positive | 440 (76.3) | 144 (75.4) | 108 (74.0) | 188 (78.3) | |
| Hepatitis B status | |||||
| Negative | 537 (93.1) | 179 (93.7) | 137 (93.8) | 221 (92.1) | 0.734 |
| Positive | 40 (6.9) | 12 (6.3) | 9 (6.2) | 19 (7.9) | |
| Syphilis | |||||
| Negative | 521 (90.3) | 185 (96.9) | 116 (79.5) | 220 (91.7) | < 0.001 |
| Yes | 56 (9.7) | 6 (3.1) | 30 (20.5) | 20 (8.3) | |
| Multi-comorbidity index; mean (S.D.)e | 5.7 (5.4) | 5.9 (6.1) | 6.2 (5.6) | 5.2 (4.7) | 0.157 |
| Medical screening: weight change over 5% during 1 month | |||||
| No | 480 (83.2) | 190 (99.5) | 76 (52.1) | 214 (89.2) | < 0.001 |
| Yes | 97 (16.8) | 1 (0.5) | 70 (47.9) | 26 (10.8) | |
| Medical screening: hospitalization (last 30 days) | |||||
| No | 558 (96.7) | 187 (97.9) | 131 (89.7) | 240 (100) | < 0.001 |
| Yes | 19 (3.3) | 4 (2.1) | 15 (10.3) | 0 (0.0) | |
| Symptoms indicative of tuberculosis (WHO Tuberculosis screening)f | |||||
| Not indicative of TB | 457 (79.2) | 182 (95.3) | 70 (47.9) | 205 (85.4) | < 0.001 |
| Indicative of TB | 120 (20.8) | 9 (4.7) | 76 (52.1) | 35 (14.6) | |
For categorical variables, data is presented in the form N (%) and for continuous variables mean (S.D.). Values may not sum up to totals due to missing values, and percentages may not sum up to 100 due to rounding
AZ Azerbaijan, KYR Kyrgyzstan, UA Ukraine, OAT opioid agonist therapy, WHO World Health Organization, S.D. standard deviation
ap value for the ANOVA for continuous variables and chi-squared test for categorical variables
bScreening positivity threshold for AUDIT is 8 or higher for males and 4 or higher for females
cScreening positivity threshold for CES-D 10 scale is 10 or higher
dInteger-valued scale that ranges from 1 (no support) to 5 (high support)
eMulti-comorbidity index is a weighted sum of the following comorbid conditions: asthma, skin ulcers, abscesses, arthritis/joint pain, gonorrhea, and other STIs (except syphilis), seizures, high blood pressure, liver problems, pneumonia, cancer, heart disease, and tuberculosis. Weights are based on whether the condition is acute (1) or chronic (3) and symptomatic (1) versus asymptomatic (0). Minimum and maximum index value is 0 and 26, respectively. HIV, hepatitis C, hepatitis B, and syphilis are analyzed separately and not included into the multi-comorbidity index
fScreening is indicative of tuberculosis if an individual had cough for at least 2 weeks or both production of sputum and unexplained weight loss in the last 3 months
Participants’ Perceptions of Reentry Challenges
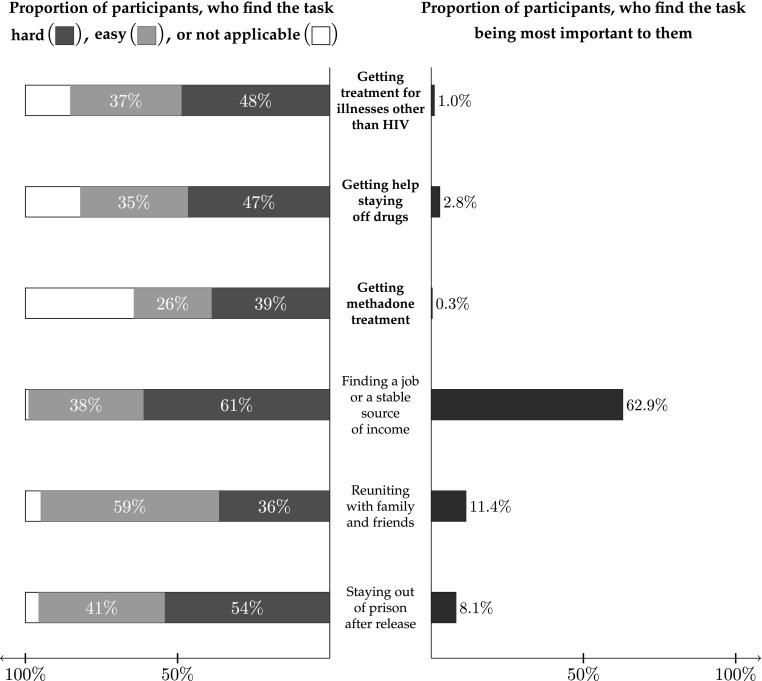
Figure 1 illustrates participants’ perceptions of reentry challenges. In terms of health-related challenges, about half of participants considered that getting treatment for illnesses other than HIV and getting help staying off drugs is hard, and about two fifths of participants considered that getting methadone treatment is hard. Yet, a sizeable proportion of participants—between one fifth to over one third—considered that health-related challenges (especially initiating methadone treatment) were not applicable to them at all. This is particularly striking because all participants in our sample had a substance use disorder with 80% having an opioid use disorder. In terms of competing everyday life challenges, 61% of participants reported they thought finding a job and 54% indicated staying out of prison would be hard. Interestingly, while many participants considered health-related tasks as not applicable, very few (< 5%) participants considered everyday life challenges as irrelevant (Fig. 1).
Fig. 1.
Perceptions of reentry challenges (N = 577)
Table 2 illustrates country differences in participants’ perceptions of health-related reentry challenges. In Kyrgyzstan, where over two thirds of participants reported a history of OAT involvement, almost half of participants reported that getting help staying off drugs was not applicable to them and over two thirds of participants considered getting methadone treatment after release as non-applicable to them (Table 2).
Table 2.
Perceptions of importance and difficulty of reentry tasks: country differences (N = 577)
| Reentry task | Total N = 577 |
AZ N = 191 |
KYR N = 146 |
UA N = 240 |
p valuea |
|---|---|---|---|---|---|
| Health-related tasks | |||||
| Getting treatment for illnesses other than HIV | |||||
| Easy | 211 (36.6) | 86 (45.0) | 43 (29.5) | 82 (34.2) | < 0.001 |
| Hard | 281 (48.7) | 91 (47.6) | 67 (45.9) | 123 (51.2) | |
| Not applicable | 85 (14.7) | 14 (7.3) | 36 (24.7) | 35 (14.6) | |
| Getting help staying off drugs | |||||
| Easy | 204 (35.4) | 61 (31.9) | 36 (24.7) | 107 (44.6) | < 0.001 |
| Hard | 269 (46.6) | 120 (62.8) | 44 (30.1) | 105 (43.8) | |
| Not applicable | 104 (18.0) | 10 (5.2) | 66 (45.2) | 28 (11.7) | |
| Getting methadone treatment | |||||
| Easy | 148 (25.6) | 61 (31.9) | 28 (19.2) | 59 (24.6) | < 0.001 |
| Hard | 224 (38.8) | 111 (58.1) | 14 (9.6) | 99 (41.2) | |
| Not applicable | 205 (35.5) | 19 (9.9) | 104 (71.2) | 82 (34.2) | |
| Everyday life tasks | |||||
| Finding a job or a stable source of income | |||||
| Easy | 218 (37.8) | 44 (23.0) | 66 (45.2) | 108 (45.0) | < 0.001 |
| Hard | 353 (61.2) | 146 (76.4) | 75 (51.4) | 132 (55.0) | |
| Not applicable | 6 (1.0) | 1 (0.5) | 5 (3.4) | 0 (0.0) | |
| Reuniting with family or friends | |||||
| Easy | 338 (58.6) | 93 (48.7) | 80 (54.8) | 165 (68.8) | < 0.001 |
| Hard | 210 (36.4) | 92 (48.2) | 45 (30.8) | 73 (30.4) | |
| Not applicable | 29 (5.0) | 6 (3.1) | 21 (14.4) | 2 (0.8) | |
| Staying out of prison following release | |||||
| Easy | 239 (41.4) | 74 (38.7) | 54 (37.0) | 111 (46.2) | < 0.001 |
| Hard | 313 (54.2) | 116 (60.7) | 76 (52.1) | 121 (50.4) | |
| Not applicable | 25 (4.3) | 1 (0.5) | 16 (11.0) | 8 (3.3) | |
| The most important task | |||||
| Getting treatment for illnesses other than HIV | 6 (1.0) | 0 (0.0) | 0 (0.0) | 6 (2.5) | < 0.001 |
| Getting help staying off drugs | 16 (2.8) | 0 (0.0) | 4 (2.9) | 12 (5.0) | |
| Getting methadone treatment | 2 (0.3) | 0 (0.0) | 0 (0.0) | 2 (0.8) | |
| Finding a job or a stable source of income | 363 (62.9) | 131 (70.4) | 100 (72.5) | 132 (55.2) | |
| Reuniting with family or friends | 66 (11.4) | 40 (21.5) | 8 (5.8) | 18 (7.5) | |
| Staying out of prison following release | 47 (8.1) | 1 (0.5) | 12 (8.7) | 34 (14.2) | |
Data is presented in the form N (%). Values may not sum up to totals due to missing values, and percentages may not sum up to 100 due to rounding
AZ Azerbaijan, KYR Kyrgyzstan, UA Ukraine
ap value for chi-square test or Fisher’s exact test
Participants’ Perceptions of Importance of Reentry Challenges
Figure 1 illustrates participants’ perceptions regarding what in their view was the most important task upon reentry. Overall, about two thirds of participants identified that finding a job or a stable source of income was the most important task, while only 0.3% of participants thought that the most important task was getting methadone treatment.
The overwhelming majority of participants (all of whom had a history of drug use, mostly of opioids, and most of whom had injected drugs often just prior to incarceration) did not consider health-related tasks associated with their addiction treatment to be most important post-release. Furthermore, many participants did not consider getting help staying off drugs and getting methadone treatment as applicable to them at all. Thus, instead of determining the correlates of stated reentry challenges, “easy” versus “hard” in our regression analyses, we assessed the correlates of stated reentry challenges as “applicable” (which could be either easy or hard) versus “not applicable.”
Correlates of Considering Reentry Challenges as Applicable
Regression analyses (Table 3) demonstrated that participants in Kyrgyzstan were least likely to consider any of the health-related post-release tasks to be applicable. Participants in Ukraine were less likely than those in Azerbaijan to consider methadone treatment as applicable, but the adjusted odds ratio (AOR) for Ukraine was not nearly as extreme as that for Kyrgyzstan (0.24 versus 0.03, respectively).
Table 3.
Correlates of considering a reentry task being applicable (N = 577)
| Covariate | AOR (95% CI) | ||
|---|---|---|---|
| Treatment for illnesses other than HIV | Getting help staying off drugs | Getting methadone treatment | |
| Country | |||
| Azerbaijan | Referent | Referent | Referent |
| Kyrgyzstan | 0.39 (0.24–0.62) | 0.09 (0.05–0.16) | 0.03 (0.01–0.06) |
| Ukraine | 0.24 (0.14–0.41) | ||
| Education | |||
| Less than high school | Referent | ||
| Completed high school | 0.45 (0.26–0.75) | ||
| History of injecting drugs | |||
| No | Referent | Referent | |
| Yes | 4.54 (2.43–8.48) | 1.87 (1.13–3.09) | |
| Recent injecting drug use, 30 days prior to current incarceration | |||
| None | Referent | Referent | |
| Moderate (1–14 days) | 2.36 (1.17–4.74) | 1.56 (1.02–2.38) | |
| Heavy (15–30 days) | 3.68 (1.64–8.22) | ||
| History of being prescribed OAT | |||
| No | Referent | ||
| Yes | 2.13 (1.03–4.40) | ||
| Moderate to severe depression | |||
| No | Referent | ||
| Yes | 1.36 (0.95–1.93) | ||
| HIV status | |||
| Negative | Referent | ||
| Positive and aware | 2.54 (0.99–6.48) | ||
| Positive and unaware | |||
| Multi-comorbidity index | 1.12 (1.06–1.18) | 1.09 (1.03–1.14) | 1.04 (1.00–1.08) |
Covariates not associated with considering any of the health-related challenges being applicable include: gender, age, marital status, income pre-incarceration, recidivism, having alcohol use problems, health-related quality of life, social support, being HIV-positive and unaware, having hepatitis C and B, having syphilis, substantial recent weight change, and positive TB screening based on symptoms
AOR adjusted odds ratio, CI credible interval, OAT opioid agonist therapy
Those with more education (completed high school) were less likely to consider getting help staying off drugs applicable. Conversely, those with a history of injecting drug use were more likely to consider getting help staying off drugs and getting methadone treatment applicable. Likewise, participants who reported moderate and especially heavy injection habits in the 30 days prior to incarceration were also more likely to consider getting help staying off drugs and getting methadone treatment relevant.
Having had previous experience with OAT was a statistically significant correlate of higher likelihood of considering getting methadone treatment. Meeting screening criteria for moderate to severe depression also positively correlated with higher likelihood of considering methadone treatment; however, 95% credible interval for this covariate includes the null.
Having higher levels of comorbidity was significantly correlated with choosing health-related reentry tasks as applicable. Participants, who were HIV positive and aware of their status, were more likely to consider treatment of illnesses other than HIV as applicable. While having a positive HIV status and being aware of it did not correlate with a higher likelihood to consider addiction-related reentry tasks as applicable, scoring higher on the multi-comorbidity index was associated with higher likelihood of considering all three health-related reentry tasks applicable.
A number of candidate covariates were not found to be associated with considering any of the health-related post-release tasks applicable. Of those, the most notable are: age, recidivism, HRQoL, hepatitis C and B status, and positive symptomatic screening for TB (Table 3).
Discussion
Most prisoners with substance use disorders return to urban settings that are often unequipped to deal with the myriad of health and social needs of individuals who have spent considerable time outside the fabric of these communities. Results from this study of soon-to-be-released prisoners with substance use disorders point to three main findings. First, overwhelmingly, prisoners prioritize basic needs over all else, including health, as central to the transitional process. To improve support and preparation for release and reintegration for transitioning prisoners, a clear understanding of why prisoners prioritize everyday life challenges over health needs is essential, especially since good health is crucial to overcoming everyday life challenges. Maslow’s hierarchy of needs provides a useful framework for understanding these challenges [54], which posits that individuals prioritize basic needs (e.g., food, housing, safety) over secondary needs (e.g., healthcare and health safety). The findings here are similar to those reported elsewhere in prisoners in other settings where basic needs are prioritized over addiction treatment [18, 19, 21]. Unlike treatment for other conditions, addiction treatment with OAT results in improvements for most basic and secondary needs like improved family reintegration, employment, criminal activity, health-related quality of life, and other health benefits [2, 55, 56]. The challenges of soon-to-be released prisoners’ social reintegration [57], rather than indifference to health, may explain why, despite the high prevalence of morbidity (including HCV, HBV, TB, syphilis, and various acute and chronic conditions included into the comorbidity index) and a universal history of drug use in our sample, in all three countries, study participants prioritized finding a source of income, reconnecting with family, and staying out of prison as most important. An alternate interpretation of this finding may be that tasks related to finding a job, reuniting with family, and staying out of prison are viewed by soon-to-be released prisoners as more essential to immediate survival than those related to health [58]. Rather than focusing on health issues, transitioning prisoners may prioritize those things that are more meaningful to them, like work that is socially affirming and reintegrating with family as activities essential to the fulfillment of social roles and obligations. Qualitative research on people in EECA countries suggests that social and relational connectedness is central to a sense of purpose in life, and conversely, feeling unneeded by others who do not value what one has to give, may lead to worsening mental and physical health and even suicide [59]. While such socially affirming activities appear to be important to transitioning prisoners, what is concerning is how these individuals do not understand the positive role of addiction treatment (especially OAT) in family reintegration, employment, reduced criminal activity, and health-related quality of life, which is often required to meet these socially affirming activities. Interventions that connect the role of OAT and dispel myths related to its use will be crucial to realistically meet the expectation of transitioning prisoners with substance use disorders.
It is concerning that over a third of participants considered starting methadone as “Not Applicable” despite most of them injecting nearly daily before incarceration. One possible explanation why these participants considered these challenges as irrelevant could be that they did not consider their drug use a chronic, relapsing disease (or methadone treatment initiated in prison and continued after release as the only evidence-based addiction treatment). Despite data from multiple clinical trials in communities [60] and in prisoners documenting its efficacy and the high relapse rate after release from prison in its absence [61–63], data from two Eastern European countries suggest that methadone is not perceived an effective treatment [55, 56, 64–66], including in prisons [13, 67, 68]. Russia retains a strong influence in the EECA region with its staunch ban on all OAT for treatment of opioid use disorder. Alternatively, prisoners might inaccurately believe in their willpower to remain off drugs or have future plans on using heroin as a more natural and healthy substance than methadone [69]. Either way, informed decision-making aids that provide culturally accurate information [70–72] should be considered to help prisoners with substance use disorders plan for their transition to the community.
Second, for those prisoners with higher levels of medical comorbidity, this subset of participants was more willing to prioritize their health during transition to the community. While having HIV did not change the odds of seeking help for addiction problems, participants with poorer general health considered getting help to stay off drugs more frequently. This could indicate that individuals in poorer health may recognize the need to accomplish health-related tasks like staying off drugs. Alternatively, it could indicate these individuals perceived fewer available resources to pursue street drugs after release [73].
Third, in Kyrgyzstan where OAT coverage is highest, a significantly smaller portion of prisoners prioritized methadone treatment compared to the other two settings where OAT coverage is lower and unavailable in prisons. One explanation for this finding is that OAT was introduced in select EECA countries in the mid-2000s not as a treatment for addiction but for HIV prevention [74]. Thus, policy makers, providers, and even patients might perceive methadone as means to control and reduce the HIV epidemic rather than as an evidence-based addiction treatment. In some contexts, this approach might have shaped patients’ attitudes towards the treatment. Research in other global settings revealed that individuals underprivileged by judicial and social regimes may experience OAT more as a tool wielded by those who wish to control them as the harm and less as a treatment meant to improve their health and wellness [75]. Another possible explanation may be that informal control of the prisons in post-Soviet settings by the prisoners themselves plays a strong role in shaping meanings of methadone in this context. Qualitative research is urgently needed to explore how the meanings of harm reduction and OAT intersect in daily experiences of PWID and prisoners in EECA countries.
Besides these three main findings, we want to highlight several other interesting observations from our analyses. It was striking that recidivists did not prioritize post-release tasks any differently than participants incarcerated for the first time. This could signify the persistence of planning fallacy [14, 15] during subsequent re-incarcerations or misalign the impact of relapse to drug use as a contributor to re-incarceration on recidivism [76]. Further, understanding the impact of OAT on reducing recidivism may need emphasis in assisting prisoners with opioid use disorder in setting their priorities [76]. Interestingly, more educated participants were less likely to consider getting help staying off drugs. Our qualitative research in Ukraine showed that PWID perceive OAT engagement as a sign of deteriorating health [56]. Thus, higher education may indicate participants’ higher socioeconomic status underlying more resourcefulness, but also higher drug use stigma, with methadone perceived as the last resort of those who are “really sick.”
We noted several interesting country differences. None of the study participants in Azerbaijan identified any of the three health-related tasks as the most important. A few (2.9%) study participants in Kyrgyzstan said that getting help staying off drugs was the most important reentry task, but despite the availability of methadone, no one identified such treatment as a priority. Only in Ukraine a small number of participants chose getting methadone treatment and getting treatment for general health conditions as the main post-release task, although the severity of health problems was comparable in all three countries. It is possible that the perceived criminalization of drugs is more severe in Ukraine than in Kyrgyzstan and Azerbaijan.
One limitation of our study was cross-sectional design as we only measured expectations for post-release challenges and not actual post-release behavior. During incarceration, participants could try to resolve cognitive dissonance [76, 77] regarding competing post-release challenges by defining challenges over which they felt least control, such as drug use, as not applicable. Previous research showed that PWID perceive more HIV and drug-related stigma post-release than within prison, and intentions to make changes in drug use are stronger in prison than after release [13]. Also, participants in prison may have overvalued their own self-efficacy and thus not felt that “help” getting off drugs was necessary, as they believed they would be able to do so on their own [69]. Consequently, after release, our participants’ little interest in health-related challenges may decrease further. Longitudinal research must examine how PWID’s attitudes and behavior concerning addiction treatment change during post-prison transition. It would also be desirable for future surveys after release to ask participants to choose and rank their top three reentry challenges in order to expand analysis options.
Our findings have implications for policy and practice. Concerning is the high exposure to methadone in Kyrgyzstan, yet the relatively low interest in this treatment. Multiple factors may have contributed to this finding including the perceived ineffectiveness of this treatment. In a setting where methadone coverage is more prevalent, feelings toward methadone by other prisoners are extraordinarily negative leading to bullying and ostracism, such as reported in Moldova [68]. In this context, prisoners in the EECA region would benefit from potentially multiple types of interventions, including those delivered by professionals and peers or through use of informed or shared decision aids. Such strategies would focus on how abstaining from illegal drugs and initiating OAT may help released prisoners reclaim jobs, reunite with family, avoid overdose and re-incarceration. As the prison environment also shapes participants’ values and norms, custodial and clinical prison staff may benefit from similar interventions to enhance their understandings of prisoners’ treatment goals [13, 78]. The key implication is that, despite the availability of OAT, prisoners may forego treatment. Future studies should explore effective methods to overcome barriers by using informed decision-making aids or delivery of effective motivational sessions using professionals or peers. Implementation science studies that overcome scale-up barriers are urgently needed to address patient-level factors. It is crucial to balance the evidence with prisoners’ own priorities and design OAT programs in a way that would integrate support in addressing other social needs, like employment support or job training.
Conclusions
Prisoners in Ukraine, Kyrgyzstan, and Azerbaijan prioritized post-release everyday challenges like finding a source of income and reconnecting with family over health-related tasks, despite their history of drug use and multiple comorbidities. Methadone was not viewed as an effective strategy for staying off drugs. Understanding and addressing the disconnect between the evidence and the belief that devalues that addiction is a disease that can be effectively treated like other chronic diseases will be crucial for scale-up. In designing programs for released prisoners, national and international organizations in EECA must consider educating prisoners and prison staff in how prioritizing addiction treatment helps accomplish other community transition goals.
Funding
This work was supported by grants R01 DA029910 (Altice), R01 DA033679 (Altice), and R36 DA042643 (Morozova) from NIDA.
References
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS), Global AIDS update 2016. 2016: Geneva, Switzerland. p. Accessed on May 28, 2016 at: http://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf.
- 2.Altice FL, Azbel L, Stone J, Brooks-Pollock E, Smyrnov P, Dvoriak S, Taxman FS, el-Bassel N, Martin NK, Booth R, Stöver H, Dolan K, Vickerman P. The perfect storm: incarceration and the high-risk environment perpetuating transmission of HIV, hepatitis C virus, and tuberculosis in Eastern Europe and Central Asia. Lancet. 2016;388(10050):1228–1248. doi: 10.1016/S0140-6736(16)30856-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inglehart R, Welzel C. Modernization, cultural change, and democracy: the human development sequence. New York, NY: Cambridge University Press; 2005. x, 333 p
- 4.Csete J, Kamarulzaman A, Kazatchkine M, Altice F, Balicki M, Buxton J, Cepeda J, Comfort M, Goosby E, Goulão J, Hart C, Kerr T, Lajous AM, Lewis S, Martin N, Mejía D, Camacho A, Mathieson D, Obot I, Ogunrombi A, Sherman S, Stone J, Vallath N, Vickerman P, Zábranský T, Beyrer C. Public health and international drug policy. Lancet. 2016;387(10026):1427–1480. doi: 10.1016/S0140-6736(16)00619-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dolan K, Wirtz AL, Moazen B, Ndeffo-mbah M, Galvani A, Kinner SA, Courtney R, McKee M, Amon JJ, Maher L, Hellard M, Beyrer C, Altice FL. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet. 2016;388(10049):1089–1102. doi: 10.1016/S0140-6736(16)30466-4. [DOI] [PubMed] [Google Scholar]
- 6.Izenberg JM, Bachireddy C, Wickersham JA, Soule M, Kiriazova T, Dvoriak S, Altice FL. Within-prison drug injection among HIV-infected Ukrainian prisoners: prevalence and correlates of an extremely high-risk behaviour. Int J Drug Policy. 2014;25(5):845–852. doi: 10.1016/j.drugpo.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamarulzaman A, Reid SE, Schwitters A, Wiessing L, el-Bassel N, Dolan K, Moazen B, Wirtz AL, Verster A, Altice FL. Prevention of transmission of HIV, hepatitis B virus, hepatitis C virus, and tuberculosis in prisoners. Lancet. 2016;388(10049):1115–1126. doi: 10.1016/S0140-6736(16)30769-3. [DOI] [PubMed] [Google Scholar]
- 8.Azbel L, Wickersham JA, Grishaev Y, Dvoryak S, Altice FL. Burden of infectious diseases, substance use disorders, and mental illness among Ukrainian prisoners transitioning to the community. PLoS One. 2013;8(3):e59643. doi: 10.1371/journal.pone.0059643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azbel L, Polonsky M, Wegman M, Shumskaya N, Kurmanalieva A, Asanov A, Wickersham JA, Dvoriak S, Altice FL. Intersecting epidemics of HIV, HCV, and syphilis among soon-to-be released prisoners in Kyrgyzstan: implications for prevention and treatment. Int J Drug Policy. 2016;37:9–20. doi: 10.1016/j.drugpo.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Azbel L, Wickersham JA, Wegman MP, Polonsky M, Suleymanov M, Ismayilov R, Dvoryak S, Rotberga S, Altice FL. Burden of substance use disorders, mental illness, and correlates of infectious diseases among soon-to-be released prisoners in Azerbaijan. Drug Alcohol Depend. 2015;151:68–75. doi: 10.1016/j.drugalcdep.2015.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sander G, Scandurra A, Kamenska A, MacNamara C, Kalpaki C, Bessa CF, Laso GN, Parisi G, Varley L, Wolny M, Moudatsou M, Pontes NH, Mannix-McNamara P, Libianchi S, Antypas T. Overview of harm reduction in prisons in seven European countries. Harm Reduct J. 2016;13(1):28. doi: 10.1186/s12954-016-0118-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Green DA. Penal optimism and second chances: the legacies of American Protestantism and the prospects for penal reform. Punishment Soc Int J Penol. 2013;15(2):123–146. doi: 10.1177/1462474513477789. [DOI] [Google Scholar]
- 13.Polonsky M, Rozanova J, Azbel L, Bachireddy C, Izenberg J, Kiriazova T, Dvoryak S, Altice FL. Attitudes toward addiction, methadone treatment, and recovery among HIV-infected Ukrainian prisoners who inject drugs: incarceration effects and exploration of mediators. AIDS Behav. 2016;20:2950–2960. doi: 10.1007/s10461-016-1375-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kahneman D, Slovic P, Tversky A. Judgment under uncertainty: heuristics and biases. Cambridge; New York: Cambridge University Press; 1982. [DOI] [PubMed] [Google Scholar]
- 15.Buehler R, Griffin D, Ross M. Exploring the planning fallacy—why people underestimate their task completion times. J Pers Soc Psychol. 1994;67(3):366–381. doi: 10.1037/0022-3514.67.3.366. [DOI] [Google Scholar]
- 16.Reitz KR. American exceptionalism in crime and punishment. New York: Oxford University Press; 2017. [Google Scholar]
- 17.Dennis AC, et al. You're in a world of chaos: experiences accessing HIV care and adhering to medications after incarceration. Janac-J Assoc Nurses Aids Care. 2015;26(5):542–555. doi: 10.1016/j.jana.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morozova O, Azbel L, Grishaev Y, Dvoryak S, Wickersham JA, Altice FL. Ukrainian prisoners and community reentry challenges: implications for transitional care. Int J Prison Health. 2013;9(1):5–19. doi: 10.1108/17449201311310760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi P, Kavasery R, Desai MM, Govindasamy S, Kamarulzaman A, Altice FL. Prevalence and correlates of community re-entry challenges faced by HIV-infected male prisoners in Malaysia. Int J STD AIDS. 2010;21(6):416–423. doi: 10.1258/ijsa.2009.009180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Loeliger KB, Altice FL, Desai MM, Ciarleglio MM, Gallagher C, Meyer JP. Predictors of linkage to HIV care and viral suppression after release from jails and prisons: a retrospective cohort study. Lancet HIV. 2018;5(2):e96–e106. 10.1016/S2352-3018(17)30209-6. [DOI] [PMC free article] [PubMed]
- 21.Bhushan A, Brown SE, Marcus R, Altice FL. Explaining poor health-seeking among HIV-infected released prisoners. Int J Prison Health. 2015;11(4):209–224. doi: 10.1108/IJPH-11-2014-0047. [DOI] [PubMed] [Google Scholar]
- 22.Althoff AL, Zelenev A, Meyer JP, Fu J, Brown SE, Vagenas P, et al. Correlates of retention in HIV care after release from jail: results from a multi-site study. AIDS Behav. 2013;17(Suppl 2):S156–70. 10.1007/s10461-012-0372-1. [DOI] [PMC free article] [PubMed]
- 23.Merrall EL, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105(9):1545–1554. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andrews JY, Kinner SA. Understanding drug-related mortality in released prisoners: a review of national coronial records. BMC Public Health. 2012;12:270. doi: 10.1186/1471-2458-12-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strang J, Bird SM, Parmar MK. Take-home emergency naloxone to prevent heroin overdose deaths after prison release: rationale and practicalities for the N-ALIVE randomized trial. J Urban Health. 2013;90(5):983–996. doi: 10.1007/s11524-013-9803-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adams J, Nowels C, Corsi K, Long J, Steiner JF, Binswanger IA. HIV risk after release from prison: a qualitative study of former inmates. J Acquir Immune Defic Syndr. 2011;57(5):429–434. doi: 10.1097/QAI.0b013e31821e9f41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iroh PA, Mayo H, Nijhawan AE. The HIV care cascade before, during, and after incarceration: a systematic review and data synthesis. Am J Public Health. 2015;105(7):e5–16. doi: 10.2105/AJPH.2015.302635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rich JD, Beckwith CG, Macmadu A, Marshall BDL, Brinkley-Rubinstein L, Amon JJ, Milloy MJ, King MRF, Sanchez J, Atwoli L, Altice FL. Clinical care of incarcerated people with HIV, viral hepatitis, or tuberculosis. Lancet. 2016;388(10049):1103–1114. doi: 10.1016/S0140-6736(16)30379-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hunt, N., & Tyrell, S., Stratified sampling. 2001, Coventry University: UK.
- 31.Brislin RW. Back-translation for cross-cultural research. J Cross-Cultural Psych. 1970;1:185–216. doi: 10.1177/135910457000100301. [DOI] [Google Scholar]
- 32.Jurgens R, Ball A, Verster A. Interventions to reduce HIV transmission related to injecting drug use in prison. Lancet Infect Dis. 2009;9(1):57–66. doi: 10.1016/S1473-3099(08)70305-0. [DOI] [PubMed] [Google Scholar]
- 33.The World Bank. Prevalence of HIV. https://data.worldbank.org/indicator/SH.DYN.AIDS.ZS. Accessed 15 Feb 2018.
- 34.World health organization: Review of HIV program in Azerbaijan. Prepared by: Dave Burrows, Azizbek Boltaev and Mirza Musa, APM Global Health, Sydney, Australia; and Magnús Gottfreðsson, Landspitali University Hospital, Reykjavik, Iceland; and Javahir Suleymanova, WHO CO Azerbaijan. 2014. http://www.euro.who.int/__data/assets/pdf_file/0011/308000/Review-HIV-Programme-Azerbaijan-missionreport.pdf?ua=1. Accessed on 3 Nov 2017.
- 35.Cook C, Kanaef N. The global state of harm reduction 2008: mapping the response to drugrelated HIV and hepatitis C epidemics © 2008 international harm reduction association. International Harm Reduction Association, London. 2008. http://www.antoniocasella.eu/archila/HARM_reduction_2008.pdf. Accessed on 3 Nov 2017.
- 36.Institute for Criminal Policy Research . World Prison Brief Report, Kyrgyzstan. London, UK: Birkbek University of London; 2017. [Google Scholar]
- 37.Subata E, Moller L. Evaluation of opioid substitution therapy in Kyrgyzstan. Geneva: World Health Organization; 2016. [Google Scholar]
- 38.List of low, lower-middle, and upper-middle income economies according to the world bank 38th annual conference of the international society for clinical biostatistics. Vigo, Spain. 2017. http://www.iscb2017.info/uploadedFiles/ISCB2017.y23bw/fileManager/CFDC%20World%20Bank%20List.pdf. Accessed on 3 Nov 2017.
- 39.Institute for Criminal Policy Research . World prison brief Ukraine. London, UK: Birkbek, University of London; 2017. [Google Scholar]
- 40.European monitoring center for drugs and drug addiction: Ukraine country overview. 2016. http://www.emcdda.europa.eu/countries/ukraine_en. Accessed on 3 Nov 2017.
- 41.Latypov AB. The Soviet doctor and the treatment of drug addiction: "a difficult and most ungracious task". Harm Reduction Journal. 2011;8:32. doi: 10.1186/1477-7517-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sarang A, Stuikyte R, Bykov R. Implementation of harm reduction in Central and Eastern Europe and Central Asia. Int J Drug Policy. 2007;18(2):129–135. doi: 10.1016/j.drugpo.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 43.Saunders JB, et al. Development of the Alcohol-Use Disorders Identification Test (Audit): WHO collaborative project on early detection of persons with harmful alcohol-consumption—2. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 44.Weissman MM, et al. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106(3):203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 45.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 46.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-B. [DOI] [PubMed] [Google Scholar]
- 47.Reinert DF, Allen JP. The alcohol use disorders identification test: an update of research findings. Alcoholism-Clinical and Experimental Research. 2007;31(2):185–199. doi: 10.1111/j.1530-0277.2006.00295.x. [DOI] [PubMed] [Google Scholar]
- 48.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. doi: 10.1016/S0749-3797(18)30622-6. [DOI] [PubMed] [Google Scholar]
- 49.World Health Organization. Systematic screening for active tuberculosis. 2013 October 12 2017]; Available from: http://www.who.int/tb/publications/Final_TB_Screening_guidelines.pdf. [PubMed]
- 50.Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications for adequate transitional care for HIV-infected prisoners: five essential components. Clin Infect Dis. 2011;53(5):469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Park T, Casella G. The Bayesian lasso. J Am Stat Assoc. 2008;103(482):681–686. doi: 10.1198/016214508000000337. [DOI] [Google Scholar]
- 52.Morozova O, Levina O, Uusküla A, Heimer R. Comparison of subset selection methods in linear regression in the context of health-related quality of life and substance abuse in Russia. BMC Med Res Methodol. 2015;15:71. doi: 10.1186/s12874-015-0066-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Huang A, Liu D. EBglmnet: a comprehensive R package for sparse generalized linear regression models. Bioinformatics. 2016;1–3. 10.1093/bioinformatics/btw143 [DOI] [PubMed]
- 54.Maslow AH. A theory of human motivation. Psychol Rev. 1943;50:370–396. doi: 10.1037/h0054346. [DOI] [Google Scholar]
- 55.Madden L, Bojko MJ, Farnum S, Mazhnaya A, Fomenko T, Marcus R, et al. Using nominal group technique among clinical providers to identify barriers and prioritize solutions to scaling up opioid agonist therapies in Ukraine. Int J Drug Policy. 2017;49:48–53. 10.1016/j.drugpo.2017.07.025. [DOI] [PMC free article] [PubMed]
- 56.Rozanova J, Marcus R, Taxman FS, Bojko MJ, Madden L, Farnum S, et al. Why people who inject drugs voluntarily transition off methadone in Ukraine. Qual Health Res. 2017;27(13):2057–70. 10.1177/1049732317732307. [DOI] [PubMed]
- 57.Maruna, S. and R. Immarigeon, After crime and punishment: pathways to offender reintegration. 2004, Cullompton; Portland, Or.: Willan. xviii, 302 p.
- 58.van Veen V, Krug MK, Schooler JW, Carter CS. Neural activity predicts attitude change in cognitive dissonance. Nat Neurosci. 2009;12(11):1469–1474. doi: 10.1038/nn.2413. [DOI] [PubMed] [Google Scholar]
- 59.Parsons MA. Dying unneeded: the cultural context of the Russian mortality crisis. Nashville: Vanderbilt University Press. xii; 2014. [Google Scholar]
- 60.Timko C, Schultz NR, Cucciare MA, Vittorio L, Garrison-Diehn C. Retention in medication-assisted treatment for opiate dependence: a systematic review. J Addict Dis. 2016;35(1):22–35. doi: 10.1080/10550887.2016.1100960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wegman MP, Altice FL, Kaur S, Rajandaran V, Osornprasop S, Wilson D, Wilson DP, Kamarulzaman A. Relapse to opioid use in opioid-dependent individuals released from compulsory drug detention centres compared with those from voluntary methadone treatment centres in Malaysia: a two-arm, prospective observational study. Lancet Global Health. 2017;5(2):E198–E207. doi: 10.1016/S2214-109X(16)30303-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT, O'Grady KE. A randomized clinical trial of methadone maintenance for prisoners: results at 12 months postrelease. J Subst Abus Treat. 2009;37(3):277–285. doi: 10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rich JD, McKenzie M, Larney S, Wong JB, Tran L, Clarke J, Noska A, Reddy M, Zaller N. Methadone continuation versus forced withdrawal on incarceration in a combined US prison and jail: a randomised, open-label trial. Lancet. 2015;386(9991):350–359. doi: 10.1016/S0140-6736(14)62338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Makarenko I, Mazhnaya A, Polonsky M, Marcus R, Bojko MJ, Filippovych S, Springer S, Dvoriak S, Altice FL. Determinants of willingness to enroll in opioid agonist treatment among opioid dependent people who inject drugs in Ukraine. Drug Alcohol Depend. 2016;165:213–220. doi: 10.1016/j.drugalcdep.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bojko MJ, Mazhnaya A, Marcus R, Makarenko I, Islam Z, Filippovych S, Dvoriak S, Altice FL. The future of opioid agonist therapies in Ukraine: a qualitative assessment of multilevel barriers and ways forward to promote retention in treatment. J Subst Abus Treat. 2016;66:37–47. doi: 10.1016/j.jsat.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mazhnaya A, et al. In their own voices: breaking the vicious cycle of addiction, treatment and criminal justice among people who inject drugs in Ukraine. Drugs: Education, Prevention and Policy. 2016;23(2):163–175. doi: 10.3109/09687637.2015.1127327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Polonsky M, Azbel L, Wickersham JA, Taxman FS, Grishaev E, Dvoryak S, et al. Challenges to implementing opioid substitution therapy in Ukrainian prisons: personnel attitudes toward addiction, treatment, and people with HIV/AIDS. Drug Alcohol Depend. 2015;148:47–55. 10.1016/j.drugalcdep.2014.12.008. [DOI] [PMC free article] [PubMed]
- 68.Polonsky M, Azbel L, Wickersham JA, Marcus R, Doltu S, Grishaev E, Dvoryak S, Altice FL. Accessing methadone within Moldovan prisons: prejudice and myths amplified by peers. Int J Drug Policy. 2016;29:91–95. doi: 10.1016/j.drugpo.2015.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Azbel L, Rozanova J, Michels I, Altice FL, Stöver H. A qualitative assessment of an abstinence-oriented therapeutic community for prisoners with substance use disorders in Kyrgyzstan. Harm Reduction Journal. 2017;14:43. doi: 10.1186/s12954-017-0168-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Elwyn G, Dannenberg M, Blaine A, Poddar U, Durand MA. Trustworthy patient decision aids: a qualitative analysis addressing the risk of competing interests. BMJ Open. 2016;6(9):e012562. doi: 10.1136/bmjopen-2016-012562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Durand MA, Witt J, Joseph-Williams N, Newcombe RG, Politi MC, Sivell S, Elwyn G. Minimum standards for the certification of patient decision support interventions: feasibility and application. Patient Educ Couns. 2015;98(4):462–468. doi: 10.1016/j.pec.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 72.Elwyn G, Lloyd A, Joseph-Williams N, Cording E, Thomson R, Durand MA, Edwards A. Option grids: shared decision making made easier. Patient Educ Couns. 2013;90(2):207–212. doi: 10.1016/j.pec.2012.06.036. [DOI] [PubMed] [Google Scholar]
- 73.Rozanova J, Brown SE, Bhushan A, Marcus R, Altice FL. Effect of social relationships on antiretroviral medication adherence for people living with HIV and substance use disorders and transitioning from prison. Health Justice. 2015;3:18. doi: 10.1186/s40352-015-0030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jolley E, Rhodes T, Platt L, Hope V, Latypov A, Donoghoe M, Wilson D. HIV among people who inject drugs in Central and Eastern Europe and Central Asia: a systematic review with implications for policy. BMJ Open. 2012;2(5):e001465. doi: 10.1136/bmjopen-2012-001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Smye V, Browne AJ, Varcoe C, Josewski V. Harm reduction, methadone maintenance treatment and the root causes of health and social inequities: an intersectional lens in the Canadian context. Harm Reduct J. 2011;8:17. doi: 10.1186/1477-7517-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mazhnaya A, Bojko MJ, Marcus R, Filippovych S, Islam Z, Dvoriak S, Altice FL. In their own voices: breaking the vicious cycle of addiction, treatment and criminal justice among people who inject drugs in Ukraine. Drugs (Abingdon Engl) 2016;23(2):163–175. doi: 10.3109/09687637.2015.1127327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Egan LC, Santos LR, Bloom P. The origins of cognitive dissonance: evidence from children and monkeys. Psychol Sci. 2007;18(11):978–983. doi: 10.1111/j.1467-9280.2007.02012.x. [DOI] [PubMed] [Google Scholar]
- 78.Polonsky M, Azbel L, Wickersham JA, Taxman FS, Grishaev E, Dvoryak S, Altice FL. Challenges to implementing opioid substitution therapy in Ukrainian prisons: personnel attitudes toward addiction, treatment, and people with HIV/AIDS. Drug Alcohol Depend. 2015;148:47–55. doi: 10.1016/j.drugalcdep.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]