Abstract
When individuals are on probation, they face challenges with securing employment and safe housing due to their criminal records, which may make food access problematic. Food insecurity is a construct used as a marker for food access that considers financial constraints and has been associated with poorer health and substance use. There is limited research on the extent of food insecurity and associated morbidities and substance use among adults on probation. We conducted a cross-sectional study in 2016, surveying 304 probationers in Rhode Island to determine whether food insecurity is associated with obesity, high blood pressure, depression, and substance use. Separate logistic regression models were used to determine the associations between food insecurity and obesity, high blood pressure, depression, and substance use. Food insecurity was experienced by 70% of our study population. The estimated prevalence of high blood pressure was significantly higher in our study sample compared to the general US population. Food insecurity was not associated with obesity, high blood pressure, or current drug use in this study sample. Food insecurity was independently associated with more than three times greater odds of being depressed (AOR 3.33, 95%CI 1.89, 5.86) and a nearly twofold greater odds of self-reporting a lower health status (AOR 1.91, 95%CI 1.18, 3.10) after adjusting for gender, race/ethnicity, age, income categories, and being homeless. Probationers were found to have a higher estimated prevalence of high blood pressure and food insecurity compared to the general population, which highlights the health disparities faced by this population. Our findings have important implications for future research and interventions to decrease the health burden not only on the individuals but their families and communities.
Keywords: Criminal justice, Probation, Food insecurity, Hunger, Social determinants of health, Homeless, Substance use, Alcohol use, Depression, High blood pressure
Introduction
According to the annual Bureau of Justice Statistics Report, at the year end of 2015, 1 in 37 adults (2.7% of the adult population) in the USA was under correctional supervision [1], with 1 in 66 adults (1.5% of the adult population) on probation [2]. Probation is a court-ordered period of community correctional supervision that is generally used as an alternative to prison [2].
Adults in US jails and prisons have higher rates of chronic and infectious diseases compared to the general US population [3]. It is reasonable to expect similar trends of chronic disease in adults on probation because they have limited resources and also may cycle in and out of the correctional system; however, the empirical evidence is lacking. When individuals are on probation, they face challenges in securing employment and safe housing, which may make food access problematic. Food insecurity is a construct used as a marker for food access that considers financial constraints and is defined as uncertain or limited availability of nutritionally adequate or safe food or the inability to acquire personally acceptable foods in socially acceptable ways. Nationally, 12.3% of US households (15.6 million households) were food insecure at some point in 2016 [4].
Figure 1 outlines a framework for the association between food insecurity and morbidities and adverse behaviors. Food insecurity can result in poorer quality of dietary intake which can lead to further health decrements. Based on research conducted in the general US population, food insecurity is associated with increased risk for overweight and obesity [5–8], chronic disease [9–11], and mental health disorders, such as depression and anxiety [12, 13]. Food insecurity has also been associated with high-risk coping strategies such as substance use [14–16], each of which can increase the risk of acquisition and transmission of infections, such as HIV and hepatitis C. The relationships between food insecurity and depression and high-risk coping strategies may be bidirectional, further highlighting the complex web of food insecurity and deleterious health and behavior consequences. It could also be argued that the relationship between food insecurity and chronic diseases is bidirectional in that individuals that may be too sick may not have the ability to be productive in the workforce and would have economic issues with acquiring adequate amounts of food.
Fig. 1.
Conceptual framework for adverse health and behaviors associated with food insecurity. Food insecurity can lead to the development of chronic disease from poor dietary quality and inadequate intake of nutrients, mental health issues such as depression, and high-risk behavioral coping strategies, such as substance use (including alcohol use) and risky sexual practices. These high-risk coping strategies increase the risk for acquisition and transmission of sexually transmitted infections (STI), particularly HIV and hepatitis C. Individuals with mental health issues may also engage in high-risk coping strategies and are therefore also at risk for STI acquisition and transmission. Chronic disease development, mental health issues, and substance use can have a bidirectional relationship with food insecurity, which adds to the complexity of this framework. Food insecurity impacts health directly at the individual and household levels, but these consequences also adversely impact the health of communities
Recent research studies have focused on food insecurity in criminal justice populations. Evidence suggests parental incarceration is associated with an increased risk for food insecurity in households with children [17, 18], particularly for fathers who lived with their children prior to incarceration [19]. Further, household food insecurity has been associated with adolescent male misconduct [20] and children raised in food insecure households, especially with persistent food insecurity, were found to have low self-control and early delinquency [21]. This, in turn, could heighten offsprings’ eventual involvement with the criminal justice system and contribute to intergenerational impact.
Limited research has explored the extent of food insecurity and associated morbidity and high-risk coping strategies among adults on probation. Such information is essential to develop an understanding of how to address health disparities with effective programs and policies to improve the wellbeing of this marginalized population. The primary objectives of this study were to determine whether food insecurity is associated with obesity, high blood pressure, depressive symptoms, and substance use in adults on probation. We hypothesized that adults on probation that are food insecure would experience greater likelihood of obesity, high blood pressure, depression, and substance use compared to those who are food secure. The proposed research is expected to provide some of the first information on food insecurity and associated morbidities and substance using behaviors in individuals on probation.
Methods
Participants
In Rhode Island, 1 out of every 45 adult residents is on probation, which is the second highest rate of community corrections in the nation [2]. For this cross-sectional study, we enrolled English-speaking adults ≥ 18 years of age that were under active probation supervision at one particular probation office in Rhode Island between July and October 2016. Participants were recruited in the waiting room of the probation office or by referral from probation officers. A small number (10%) refused to participate at the time of recruitment because the timing was inconvenient with transportation home or other appointments. Fewer than 5% of the individuals that reported to this office were estimated to be non-English speaking. Participants were given $25 gift cards to compensate for their time for participating in this research project. The study was approved by the Institutional Review Board of The Miriam Hospital and the Medical Research Advisory Committee of the Rhode Island Department of Corrections. Subjects signed a written consent form to participate.
Lifestyle and Health Questionnaire
Participants completed a lifestyle questionnaire via an audio computer-assisted self-interview (ACASI) to allow for a private interview to elicit more accurate, rather than socially desirable responses, to questions about sensitive risk behaviors compared to face-to-face interviews interviews [22–24]. The Tufts ACASI system (http:\\acasi.tufts.edu) was administered on individual laptops with each participant listening to the survey questions and response options over their own headphones. This format allows for direct data entry of participant responses. Participants responded to each question by pressing a number on the keyboard or using a mouse to click on the response. Each question also had the options to refuse or respond “Don’t Know.” All ACASI surveys were administered in a private room at the probation office without probation officers present to ensure confidentiality of survey responses. The 30-min questionnaire included questions about sociodemographic characteristics, food security, general health status, depression, high blood pressure, illicit drug use, and alcohol use which are described in more detail below.
Primary Exposure: Food Security Status
The primary exposure, food security status, was determined using the USDA 10-Item Adult Food Security Module [25]. This food security survey collects data for ten indicators that focus on conditions that represent the respondents’ perception of uncertain or inadequate food access and availability because of limited financial resources, compromised eating patterns (such as cutting the size of or skipping meals or not eating for a whole day), and physical outcomes, such as hunger and weight loss. Questions ask about prior 30 days. Affirmative responses to questions in the food security survey are summed. Scores range from zero to ten, with higher scores reflecting increased severity of household food insecurity. The food insecurity score is commonly analyzed as a binary variable defined as food secure (score 0 to 2) or food insecure (score 3 to 10) [25].
General Health Status and Depression
To measure perceived health status, participants were asked, “Overall, how would you rate your own health”? Response options included “excellent,” “very good,” “good,” “fair,” and “poor.” Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D). The CES-D questionnaire asks 20 questions about the way an individual may have felt or behaved in the last week. The response options were “rarely or none of the time (less than one day)”, “some or a little of the time (1-2 days)”, “occasionally or a moderate amount of time (3-4 days),” or “all of the time (5-7 days)”. Each question has a scoring range of 0 to 3 points based upon the responses. The cumulative score for the questionnaire can range from 0 to 60, with a higher score indicating more depressive symptoms. A cutoff score of ≥ 16 was used to define depression [26].
High Blood Pressure
Blood pressure was measured once during the study visit following the ACASI using an automated blood pressure cuff (Omron Healthcare, Model HEM-712C). Blood pressure was measured using either an adult or large adult-sized cuff, with the participant in a seated position, with legs uncrossed, feet flat on the floor, and the right arm resting on a table. The blood pressure was taken on the right arm for all measurements. Participants were instructed to relax and not talk during the measurement. High blood pressure was identified according to the American Heart Association (AHA) Guidelines definition of High Blood Pressure Stage 1: systolic reading of ≥ 140 mmHg or diastolic reading of ≥ 90 mmHg [27].
A brief medical history within the ACASI queried about high blood pressure. Participants were asked if they were ever told by a healthcare professional that they had high blood pressure or hypertension. For any affirmative responses, a follow-up question asked participants if they were prescribed medication for high blood pressure and whether they were currently taking the medication.
Obesity
Obesity was determined by body mass index (BMI), calculated as weight (kilograms) divided by height (meters) squared. BMI is a standard marker for adiposity and risk of various metabolic and disease outcomes [28]. After the blood pressure reading, participants were weighed without shoes in light clothing using a calibrated standing scale (Tanita, Model TBF-410). Weight was measured to the nearest 0.1 kg. Height was measured to the nearest 0.1 cm using a portable stadiometer (Seca, Model 213).
Substance Use
Assessment of substance use included alcohol and illicit drug use. Alcohol consumption was measured using the World Health Organization’s Alcohol Use Disorders Identification Test (AUDIT) survey [29]. The AUDIT survey consists of ten questions and each question has a possible score of 0 to 4. The total score for the AUDIT survey ranges from 0 to 40, with higher scores being indicative of hazardous and harmful alcohol use. There are two ways that individuals’ alcohol use/consumption can be classified as “hazardous” based on the AUDIT survey. First, “hazardous alcohol use” is based on the total AUDIT score (≥ 8). Second, “hazardous alcohol consumption” is based on the individual consuming three or more alcoholic drinks on a typical day and/or consuming six or more alcoholic drinks on one occasion. Additional domains measured via the AUDIT survey include alcohol dependence and alcohol harm. Alcohol dependence is any affirmative response to: not being able to stop drinking once started, failing to do what was expected because of drinking, or needing a drink first thing in the morning to get going after a heavy drinking session. Alcohol harm is any affirmative response to: feeling guilt after drinking, not being able to remember what happened the night before because of drinking, injury to oneself or someone else because of drinking, or someone expressing concern about their drinking or suggesting to decrease drinking [29].
Illicit drug use was assessed by determining current drug use (in past 30 days), types of drugs ever and currently used, frequency of current use, and ever injecting drugs. These questions were asked using an analogous series of questions. For this analysis, we combined all types of drugs into two drug use variables: ever and current drug use. We did not include marijuana as illicit drug use but present it separately.
Statistical Analyses
Differences in sociodemographic characteristics, morbidities, alcohol use, and drug use by food insecurity status were determined using Chi-square or Fisher’s exact tests for categorical variables and Wilcoxon Rank Sum tests for continuous variables (age and BMI were both skewed so a non-parametric test was used). To determine if the estimated prevalence of food insecurity, obesity, and high blood pressure in probationers was different compared to the general US population, a one sample t-test comparing the prevalence estimate was conducted. A proportional odds ordinal logistic regression model was used to determine the association between food insecurity, our primary exposure, and the outcome of general self-reported health, which was collapsed to three categories (“excellent/very good,” “good,” and “fair/poor”) for analysis. We conducted likelihood ratio tests and the Gamma tests to ensure we did not violate the proportional odds assumption. Odds ratios from ordinal logistic regression models can be interpreted as the odds of being in higher levels of an outcome given a particular exposure compared to the odds of being at lower levels of an outcome in the absence of that particular exposure [30, 31]. Separate logistic regression models were used to determine the associations between food insecurity and the following dichotomous “outcomes”: obesity, high blood pressure, depression, and current substance use. For each model, unadjusted and adjusted odds ratios and 95% confidence intervals were computed. In the final multivariate models, we adjusted each regression model for gender, race/ethnicity, age, income categories, and being homeless based upon findings from previous research. To determine whether gender and race/ethnicity modified the associations between food insecurity and the outcomes, we included interaction terms in our models. Stata v13 (StataCorp, College Station, TX) was used for all statistical analyses.
Results
Table 1 displays the main characteristics of the participants by food security status. The study sample included 304 participants, of whom the majority (70%) were food insecure. The median age was 36 years and 72% were male. Participants were predominantly non-Hispanic white (53%), 15% were non-Hispanic black, and 21% were Hispanic/Latino. At the time of their participation in the study, 41% of participants had spent at least 24 months or more on probation. Approximately one-third (33%) had less than a high school education, nearly half (47%) were never married, 25% had a child or children living with them, almost one-quarter (23%) were homeless, almost one half (47%) of participants reported an annual income of $5000 or less, and 41% reported having a full- or part-time job. Compared to food secure participants, food insecure participants were more likely to be homeless (29 versus 10%, p < 0.001) and participate in the Supplemental Nutrition Assistance Program (SNAP, formerly known as food stamps) (77 versus 66%, p = 0.046), and less likely to have a full-time job (16 versus 34%, p = 0.004). More than three-fourths (77%) of participants had government health insurance, but food insecure participants were more likely to have government health insurance compared to food secure participants (80 versus 69%, respectively) while food secure participants were more likely to have private insurance than food insecure participants (16 versus 5%, respectively) (global p value = 0.005). About half of the participants (51%) reported that they had a primary care physician.
Table 1.
Characteristics of a Sample of Probationers in Rhode Island by Food Security Status, 2016. N (%) or Median (IQR)a.
| All (n = 304) | Food insecure (n = 214) | Food secure (n = 90) | p value | |
|---|---|---|---|---|
| Age, years (19–65 years)a | 36 (27, 47) | 36 (27, 46) | 36 (27, 48) | 0.928 |
| Male | 220 (72) | 149 (70) | 71 (79) | 0.094 |
| Race/ethnicity | 0.218 | |||
| Black, non-Hispanic | 45 (15) | 30 (14) | 15 (17) | |
| Hispanic/Latino, any race | 64 (21) | 50 (23) | 14 (16) | |
| White, non-Hispanic | 161 (53) | 107 (50) | 54 (60) | |
| Other | 33 (11) | 26 (12) | 7 (8) | |
| Current time on probation | 0.807 | |||
| < 1 year | 114 (37) | 80 (37) | 34 (38) | |
| 1 year to < 18 months | 39 (13) | 25 (12) | 14 (16) | |
| 18 months to < 2 years | 25 (8) | 18 (8) | 7 (8) | |
| 2 years or more | 126 (41) | 91 (43) | 35 (39) | |
| Education | 0.882 | |||
| Less than high school/no GEDb | 101 (33) | 70 (33) | 31 (34) | |
| High school/GEDb | 129 (42) | 94 (44) | 35 (39) | |
| Trade/technical school | 19 (6) | 13 (6) | 6 (7) | |
| Some college/college degree/graduate school | 54 (18) | 36 (17) | 18 (20) | |
| Relationship Status | 0.900 | |||
| Never Married | 143 (47) | 100 (47) | 43 (48) | |
| Married | 22 (7) | 16 (7) | 6 (7) | |
| Divorced/widowed | 53 (17) | 37 (17) | 16 (18) | |
| Separated | 30 (10) | 22 (10) | 8 (9) | |
| Living with partner | 56 (18) | 39 (18) | 17 (19) | |
| Children living with participant | 75 (25) | 52 (34) | 23 (40) | 0.424 |
| Homeless | 70 (23) | 61 (29) | 9 (10) | <0.001 |
| Income, annual | 0.599 | |||
| ≤ $5000 | 133 (47) | 98 (49) | 35 (42) | |
| $5001 to $10,000 | 59 (21) | 43 (22) | 16 (19) | |
| $10,001 to $20,000 | 38 (13) | 26 (13) | 12 (14) | |
| > $20,000 | 53 (19) | 33 (17) | 20 (24) | |
| Refused/don’t know | 21 (7) | 14 (7) | 7 (8) | |
| Employment | 0.004 | |||
| Full-time job (yes/no) | 66 (22) | 35 (16) | 31 (34) | |
| Part-time job (yes/no) | 58 (19) | 47 (22) | 11 (12) | |
| SNAP | 223 (73) | 164 (77) | 59 (66) | 0.046 |
| Current smoker | 0.240 | |||
| Everyday | 142 (72) | 110 (74) | 32 (65) | |
| Some days | 39 (20) | 29 (19) | 10 (20) | |
| Not at all | 17 (8) | 10 (7) | 7 (14) | |
| Type of health insurance | 0.005 | |||
| Government | 234 (77) | 172 (80) | 62 (69) | |
| Private | 24 (8) | 10 (5) | 14 (16) | |
| None | 29 (10) | 23 (11) | 6 (7) | |
| Other | 17 (5) | 9 (5) | 8 (9) | |
| Has a primary care physician | 156 (51) | 104 (49) | 52 (58) | 0.144 |
aIQR interquartile range (25th%ile, 75th%ile)
bGED general education development (high school equivalency diploma)
Participants’ overall health status and select health conditions are shown in Table 2. Almost one third (34%) of participants reported their overall health rating as “Fair/Poor.” Participants that were food insecure were more likely to rate their overall health as “Fair/Poor” compared to food secure participants (39 versus 22%, respectively) and food secure participants were more likely to rate their overall health as “Excellent/Very Good” compared to food insecure participants (36 versus 28%, respectively) (global p value = 0.017). More than half of participants (56%) were depressed, but food insecure participants were significantly more likely to be depressed compared to food secure participants (81 versus 19%, p < 0.001). The median BMI for participants was in the overweight range (27.7 kg/m2) and there were no significant differences in BMI category based upon food security status (p = 0.808). More than one third of participants (37%) had high blood pressure measured during the study visit and more than one-quarter (27%) were told by a healthcare professional that they had high blood pressure or hypertension. The occurrence of high blood pressure, either measured during the study visit or by self-report, did not differ significantly by food security status. We were not able to measure blood pressure for two participants because their arm circumference exceeded the cuff size, but both reported being told by a healthcare professional that they had high blood pressure.
Table 2.
Health status and morbidities in a sample of probationers in Rhode Island by food security status, 2016. N (%) or median (IQR)
| All (n = 304) | Food insecure (n = 214) | Food secure (n = 90) | p value | |
|---|---|---|---|---|
| Self-reported healthb | 0.017 | |||
| Excellent | 25 (8) | 12 (6) | 13 (14) | |
| Very good | 68 (22) | 48 (22) | 20 (22) | |
| Good | 108 (36) | 71 (33) | 37 (41) | |
| Fair | 80 (26) | 64 (30) | 16 (18) | |
| Poor | 23 (8) | 19 (9) | 4 (4) | |
| Depressed | 69 (56) | 137 (81) | 32 (19) | <0.001 |
| Body mass index (kg/m2)a | 27.7 (24.0, 32.7) | 28.2 (24.3, 32.7) | 26.7 (23.5, 31.9) | 0.346 |
| BMIc Categories | 0.808 | |||
| Obese | 111 (37) | 81 (38) | 30 (33) | |
| Overweight | 89 (29) | 61 (29) | 28 (31) | |
| Normal Weight | 99 (33) | 69 (32) | 30 (33) | |
| Underweight | 5 (2) | 3 (1) | 2 (2) | |
| High blood pressure (measured) | 112 (37) | 77 (36) | 35 (39) | 0.602 |
| Ever diagnosed with HBPd (self-report) | 83 (27) | 55 (26) | 28 (31) | 0.334 |
aIQR interquartile range (25th%ile, 75th%ile)
bIn response to the question, “Overall, how would you rate your own health?”
cBMI body mass index
dHBP high blood pressure
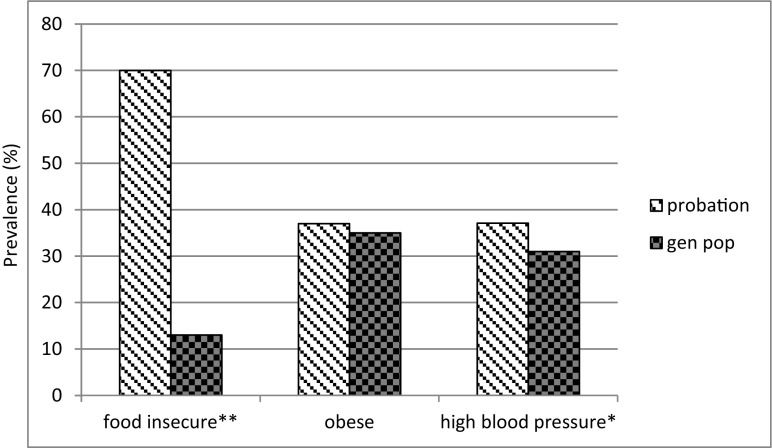
Figure 2 shows the differences between our study sample of probationers and the general US adult population with regard to estimated prevalence of food insecurity, obesity, and high blood pressure [32, 33]. Compared to the general US population, there was a large and statistically significant difference in prevalence of food insecurity (13 versus 70%, respectively, p < 0.001). The difference in prevalence of obesity in our study sample compared to the general population was not statistically significant (37 versus 35% [33], p = 0.580). High blood pressure (31 [32] versus 37%, respectively, p = 0.022) was also significantly different in our study sample compared to the general population. Based upon the results from our brief medical history questions, about two thirds (62%) of the participants with a high blood pressure measurement during the study reported that they had never been told by a healthcare professional that they had high blood pressure. Of the individuals that reported they had been told by a healthcare professional that they had high blood pressure (n = 83), 43 (52%) had a high blood pressure measurement and 38 (46%) had a controlled blood pressure measurement during the study visit. Fifty (60%) of the participants that reported a diagnosis of high blood pressure were prescribed high blood pressure medications and 35 (42%) were taking prescribed medications at the time of the study. More than half (57%) of the participants taking high blood pressure medication had high blood pressure measured during the study visit.
Fig. 2.
Estimated prevalence of food insecurity, obesity, and high blood pressure in a sample of probationers in Rhode Island compared to the general adult US population [32], 2016 (%). Obesity and high blood pressure for probationers were measured during the study visit. Source for prevalence for obesity and high blood pressure in the general population is the CDC [32]. Source for the prevalence of food insecurity in the general population is the USDA [4]. *The difference in proportions between the sample of probationers and the general adult US population for high blood pressure is statistically significant (p = 0.022). **The difference in proportions between the sample of probationers and the general adult US population for food insecurity is statistically significant (p < 0.001)
Substance use by food security status is depicted in Table 3. Approximately one quarter of participants (24%) were defined as experiencing hazardous alcohol use while 43% were defined as experiencing hazardous alcohol consumption. Approximately one-fifth (22%) were categorized as alcohol dependent, and 41% experienced harm from their alcohol use. More than one third of participants (39%) reported using marijuana in the last month, 19% reported current illicit drug use, 62% reported ever using illicit drugs, and 18% reported ever injecting drugs. The recreational drugs participants reported currently using were prescription drugs that had not been prescribed directly to them (28%), sedatives (including tranquilizers and barbiturates) (21%), prescription opioids (7%), cocaine (7%), crack (6%), heroin (5%) and methamphetamines (1%). Compared to food secure participants, food insecure participants were almost twice as likely to experience hazardous alcohol dependence (26 versus 14%, p = 0.032), and more likely to report ever use of illicit drugs (66 versus 53%, p = 0.039), and report ever injecting drugs (21 versus 11%, p = 0.049).
Table 3.
Substance use in a sample of probationers in Rhode Island by Food Security Status, 2016
| All (n = 304) | Food insecure (n = 214), n (%) | Food secure (n = 90), n (%) | p value | |
|---|---|---|---|---|
| Hazardous alcohol use | 74 (24) | 57 (27) | 17 (19) | 0.151 |
| Hazardous alcohol consumption | 132 (43) | 98 (46) | 34 (38) | 0.198 |
| Alcohol dependence | 68 (22) | 55 (26) | 13 (14) | 0.032 |
| Alcohol harm | 124 (41) | 93 (43) | 31 (34) | 0.144 |
| Current marijuana use (last 30 days) | 119 (39) | 89 (42) | 30 (33) | 0.372 |
| Current illicit drug use (last 30 days) | 58 (19) | 42 (20) | 16 (18) | 0.708 |
| Ever drug use | 189 (62) | 141 (66) | 48 (53) | 0.039 |
| IDUa ever | 54 (18) | 44 (21) | 10 (11) | 0.049 |
aIDU injection drug use
The results from the crude and adjusted logistic regression models are presented in Table 4. In the adjusted model, being food insecure was associated with an almost twofold greater odds of reporting a lower health status category (AOR 1.91, 95%CI 1.18, 3.10). Food insecurity was not associated with high blood pressure or obesity in our study sample. In the final adjusted model, compared to those individuals who were food secure, individuals who were food insecure had more than three times greater odds of being depressed (AOR 3.33, 95%CI: 1.89, 5.86). Food insecurity was not associated with current drug use in our study. With respect to alcohol use, food insecurity was not associated with hazardous alcohol use, hazardous alcohol consumption, or experiencing alcohol harm. Being food insecure was associated with a greater odds of alcohol dependence in the unadjusted model (OR 2.05, 95% CI 1.06, 3.98). In the adjusted model, the relationship between food insecurity and alcohol dependence was attenuated, and no longer statistically significant. Gender and race/ethnicity did not emerge as effect modifiers in the relationship between food insecurity and the outcomes considered (data not shown).
Table 4.
Association between food insecurity and morbidity and substance use in adults on probation in Rhode Island, 2016 (n = 304).
| Unadjusted | Adjusteda | |
|---|---|---|
| OR (95%CI) | AOR (95%CI) | |
| Perception of healthb | 1.77 (1.13, 2.79) | 1.91 (1.18, 3.10) |
| High blood pressure | 0.87 (0.53, 1.45) | 0.92 (0.53, 1.60) |
| Obesity | 1.22 (0.73, 2.04) | 1.25 (0.72, 2.17) |
| Depressed | 3.22 (1.93, 5.39) | 3.33 (1.89, 5.86) |
| Current drug use | 1.13 (0.60, 2.14) | 1.20 (0.61, 2.36) |
| Alcohol use | ||
| Hazardous alcohol use | 1.56 (0.85, 2.87) | 1.53 (0.80, 2.92) |
| Hazardous alcohol consumption | 1.39 (0.84, 2.30) | 1.36 (0.80, 2.33) |
| Alcohol dependence | 2.05 (1.06, 3.98) | 1.97 (0.97, 4.01) |
| Alcohol Harm | 1.46 (0.88, 2.44) | 1.62 (0.94, 2.79) |
OR odds ratios, AOR adjusted odds ratios, CI confidence intervals
aAll models were adjusted for gender, race/ethnicity, age, income categories (> $20,000 as referent group), and being homeless
bOdds ratios estimated from proportional odds ordinal logistic regression models (see “Methods”)
Discussion
Our study is among the first to examine morbidities and substance use associated with food insecurity among probationers. We found staggering differences with regard to health disadvantages in our study population compared to the general population. Almost three fourths of our study population was food insecure, suggesting that accessing food on a regular basis is a common problem for individuals on probation. The level of food insecurity in our study sample (70.4%) was substantially higher than the general population (12.3%). Being food insecure was associated with a greater odds of reporting poorer health in our study sample. The probationers in our study had a significantly higher prevalence of high blood pressure compared to the general population. Also, participants that were food insecure had a greater odds of being depressed compared to food secure participants. These findings highlight the health disparities in this population and put these individuals at increased risk for poorer health outcomes, especially given their limited income and resources.
According to the 2011–2012 National Inmate Survey, prisoners and jail inmates have a significantly higher prevalence of ever having hypertension compared to the general population [3]. Our findings suggest similar elevations in the probation setting and it is likely that many are underdiagnosed. Along the high blood pressure continuum of care, many individuals who were prescribed medications were either not taking them or potentially not experiencing adequate blood pressure control from the medications as evidenced by their high blood pressure measurement during the study visit. The majority of participants reported having some type of health insurance, but only one-half reported having a primary care physician, which could reflect underinsurance or the fact that healthcare is a lower priority compared to other needs, such as employment, safe housing, and adequate access to food. We characterized the priorities of probationers in a qualitative study of 22 participants under correctional supervision at the same probation office [34]. In this study, participants ranked their top priorities (from highest to lowest) as substance use recovery, employment, housing, and food intake. Healthcare was ranked last out of seven priorities [34].
Despite the very high rates of food insecurity and obesity identified in our study population, we did not detect the hypothesized association between food insecurity and obesity. The relationship between food insecurity and weight status is complicated, and study findings vary across populations. Some of these inconsistencies might relate to the degree of food insecurity observed in the populations, where populations with a majority of participants being food insecure, there is no statistically significant association between food insecurity and obesity. The hypothesized association is thought to reflect the overconsumption of cheap, high calorie foods among those who are food insecure, which can result in insulin resistance and increased risk of obesity. Obesity has been associated with food insecurity in HIV-infected and HIV-at risk women in the Bronx [35], Hispanic men and women in California who were ≤ 200% of the federal poverty level [7], adults living in a community setting in Connecticut [6], and in adults from 12 states across the USA [5]. A study of homeless adults in Rhode Island found no association between food insecurity and obesity, perhaps because the study population was homogenous with 94% of the study participants defined as food insecure [36]. Another study of low-income African-American families in Baltimore also reported high rates of obesity and food insecurity but did not see an association between food insecurity and obesity [37]. To make comparisons between our study and previous studies about the relationship between food insecurity and obesity, all but one of the studies described here used the same USDA Adult Food Security Module that was used in our study. The one exception identified food insecurity based on an affirmative response to one question about being worried about having enough money to buy nutritious food [5]. Also, our failure to identify an association between food insecurity and obesity may reflect our largely male sample; the relationship between food insecurity and obesity has been stronger in females [38].
Depression was significantly associated with food insecurity in our study sample. Prior studies, both domestic and international, have found associations between depression and food insecurity [12, 13]. These investigations were all cross-sectional, so temporality is unclear. Mental health problems are prevalent in the criminal justice population [39]; however, the intersection of depression and food insecurity in this population has not been previously explored. Because of the high prevalence of food insecurity in our study sample and the high prevalence of depression in individuals that were food insecure compared to food secure, this relationship between food insecurity and depression warrants further investigation.
In our study, the association between food insecurity and alcohol dependence was trending towards statistical significance. According to the 2012 National Survey on Drug Use and Health, the prevalence of alcohol or illicit drug use disorder in the past year in male probationers was 40.3% [40]. A study by Lurigio et al. of 627 adult probationers in Illinois found that alcohol and illicit drugs were used at higher rates in the probation population compared to the non-institutionalized population in Illinois [41]. Alcohol use disorder combines hazardous alcohol use and alcohol dependence into a single disorder. Almost one quarter of participants in our current study (24%) reported hazardous alcohol use and 22% were alcohol dependent. While we do not have information about illicit drug use disorder in our study sample, 19% reported currently using drugs.
To intervene upon alcohol use disorder in probationers, it is important to understand why alcohol is used in this population. Plugge et al. conducted a qualitative study in the UK that included a total of 41 focus group participants on probation, where probationers described why alcohol use was common [42]. One theme highlighted by probationers was that alcohol was of particular concern because its consumption was viewed as socially acceptable and was easily accessible [42]. Participants in Plugge’s study also disclosed that alcohol was used as a way to cope with the stress from being on probation. They also identified the lack of inadequate services available to address substance use [42]. It is plausible that our study sample uses alcohol to cope with being food insecure. Or, if people are dependent on alcohol, they may choose to spend money on alcohol instead of food. Because of the cross-sectional nature of our study, we cannot discern the directionality of this relationship.
Our findings should be considered in the context of several study limitations. First, as indicated above, our cross-sectional study design precludes establishing the temporal sequence of the relationships we observed, and thus precludes claims of causality. Second, because food insecurity and substance use were self-reported, social desirability or recall bias may have influenced responses. Use of the ACASI is believed to help elicit more candid responses, but current drug use may have been underreported given that the study was conducted at the probation office. Third, we measured blood pressure only once during the study visit, which may falsely elevate the estimated prevalence of high blood pressure in the study sample. However, participants were seated at rest completing the survey an average of 30 min before their blood pressure was measured. Finally, since the study was restricted to one probation office in Rhode Island, our results may not be generalizable to other probation settings across the country.
Our study has several noteworthy strengths. To our knowledge, ours is the first study to examine the relationship of food insecurity with morbidities and substance use in probationers. Our data collection methods were designed to elicit high quality self-reported information and clinical measurements. Our study provides some of the first estimates of prevalence of obesity and high blood pressure in a sample of probationers, a group for which data on physical health status are limited.
Conclusion
Our findings highlight the health disparities of this vulnerable probation population and have important implications for future research and interventions. Our findings demonstrate that criminal justice involvement, even at the community corrections level, places probationers at high risk for poorer health outcomes due to limited resources and constant life stressors that put them at risk for recidivism or extended probation sentences. Probationers were found to have a higher estimated prevalence of high blood pressure and food insecurity compared to the general population, which highlights the health disparities faced by this population. The impoverished circumstances resulting from being on probation may predispose probationers to food insecurity which may be strongly associated with depression and moderately with alcohol dependence. Food insecurity is a modifiable risk factor for health outcomes; addressing the root causes of food insecurity will help to decrease the health burden not only on the individuals but their families and communities. In addition, probation represents the highest number of individuals in the correctional supervision system so determining mechanisms to address food insecurity and health consequences will help to begin to address health disparities in this population. Utilizing the probation setting as a mechanism to intervene and provide resources for food insecurity, linkage to healthcare, and treatment for depression and alcohol dependence warrant further exploration. Community corrections offers a window of opportunity for public health interventions because probationers are required to have regular visits at the probation office.
Acknowledgments
The authors would like to thank the study participants. We also thank Marc Moody from the Rhode Island Department of Corrections, Tasia Liu, and the probation officers for their invaluable contributions to the implementation of this study.
Funding Information
Funding was provided by National Institute on Drug Abuse (NIDA) Grant #R25DA037190, The Lifespan/Brown Criminal Justice Research Program on Substance Use, HIV, and Comorbidities; The Providence/Boston Center for AIDS Research Grant #P30AI042853; and The Boston Obesity Research Center Grant #P30DK046200.
References
- 1.Kaeble D, Glaze LE. Correctional Populations in the United States, 2015. US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. December 2016;NCJ 250374.
- 2.Kaeble D, Bonczar TP. Probation and Parole in the United States, 2015. US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. December 2016;NCJ 250230.
- 3.Maruschak LM, Berzofsky M, Unangst J. Medical problems of state and federal prisoners and jail inmates, 2011-12. U.S. Department of Justice, Bureau of Justice Statistics Special Report. 2015;NCJ 248491:1–22.
- 4.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2016, ERR-237. US Department of Agriculture, Economic Research Service. September 2017.
- 5.Pan L, Sherry B, Njai R, Blanck HM. Food insecurity is associated with obesity among US adults in 12 states. J Acad Nutr Diet. 2012;112(9):1403–1409. doi: 10.1016/j.jand.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin KS, Ferris AM. Food insecurity and gender are risk factors for obesity. J Nutr Educ Behav. 2007;39(1):31–36. doi: 10.1016/j.jneb.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 7.Leung CW, Williams DR, Villamor E. Very low food security predicts obesity predominantly in California Hispanic men and women. Public Health Nutr. 2012;15(12):2228–2236. doi: 10.1017/S1368980012000857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP. Food insecurity is positively related to overweight in women. J Nutr. 2001;131(6):1738–1745. doi: 10.1093/jn/131.6.1738. [DOI] [PubMed] [Google Scholar]
- 9.Perez-Escamilla R, Villalpando S, Shamah-Levy T, Mendez-Gomez Humaran I. Household food insecurity, diabetes and hypertension among Mexican adults: results from Ensanut 2012. Salud Publica Mex. 2014;56(Suppl 1):s62–s70. doi: 10.21149/spm.v56s1.5167. [DOI] [PubMed] [Google Scholar]
- 10.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–310. doi: 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Irving SM, Njai RS, Siegel PZ. Food insecurity and self-reported hypertension among Hispanic, black, and white adults in 12 states, behavioral risk factor surveillance system, 2009. Prev Chronic Dis. 2014;11:E161. doi: 10.5888/pcd11.140190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stuff JE, Casey PH, Szeto KL, Gossett JM, Robbins JM, Simpson PM, et al. Household food insecurity is associated with adult health status. J Nutr. 2004;134(9):2330–2335. doi: 10.1093/jn/134.9.2330. [DOI] [PubMed] [Google Scholar]
- 13.Weaver LJ, Hadley C. Moving beyond hunger and nutrition: a systematic review of the evidence linking food insecurity and mental health in developing countries. Ecol Food Nutr. 2009;48(4):263–284. doi: 10.1080/03670240903001167. [DOI] [PubMed] [Google Scholar]
- 14.Strike C, Rudzinski K, Patterson J, Millson M. Frequent food insecurity among injection drug users: correlates and concerns. BMC Public Health. 2012;12:1058. doi: 10.1186/1471-2458-12-1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(supp):1729S–1739S. doi: 10.3945/ajcn.111.012070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whittle HJ, Palar K, Napoles T, Hufstedler LL, Ching I, Hecht FM, et al. Experiences with food insecurity and risky sex among low-income people living with HIV/AIDS in a resource-rich setting. J Int AIDS Soc. 2015;18:20293. doi: 10.7448/IAS.18.1.20293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cox R, Wallace S. The Impact of Incarceration on Food Insecurity Among Households with Children. Andrew Young School of Policy Studies Research Paper Series 2013;13–05: https://ssrn.com/abstract=2212909. Accessed May 17, 2017.
- 18.Jackson DB, Vaughn MG. Parental history of disruptive life events and household food insecurity. J Nutr Educ Behav. 2017;49(7):554–560.e551. doi: 10.1016/j.jneb.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 19.Turney K. Paternal incarceration and Children’s food insecurity: a consideration of variation and mechanisms. Soc Serv Rev. 2015;89(2):335–367. doi: 10.1086/681704. [DOI] [Google Scholar]
- 20.Jackson DB, Vaughn MG. Household food insecurity during childhood and adolescent misconduct. Prev Med. 2017;96:113–117. doi: 10.1016/j.ypmed.2016.12.042. [DOI] [PubMed] [Google Scholar]
- 21.Jackson DB, Newsome J, Vaughn MG, Johnson KR. Considering the role of food insecurity in low self-control and early delinquency. J Crim Just. 2017
- 22.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 23.Hewett PC, Mensch BS, Erulkar AS. Consistency in the reporting of sexual behaviour by adolescent girls in Kenya: a comparison of interviewing methods. Sex Transm Infect. 2004;80(Suppl 2):ii43–ii48. doi: 10.1136/sti.2004.013250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simões AA, Bastos FI, Moreira RI, Lynch KG, Metzger DS. Acceptability of audio computer-assisted self-interview (ACASI) among substance abusers seeking treatment in Rio de Janeiro, Brazil. Drug Alcohol Depend. 2006;82:S103–S107. doi: 10.1016/S0376-8716(06)80016-5. [DOI] [PubMed] [Google Scholar]
- 25.United States Department of Agriculture Economic Research Service. USDA Adult Food Security Survey Module. 2015; http://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools.aspx#adult. Accessed 15 Jan 2016.
- 26.Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 27.American Heart Association. Understanding Blood Press Readings December 18, 2015; http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/AboutHighBloodPressure/Understanding-Blood-Pressure-Readings_UCM_301764_Article.jsp#.VseVcuZcjgk. Accessed 2/19/16.
- 28.Centers for Disease Control and Prevention. Division of nutrition, physical activity, and obesity: defining adult overweight and obesity. April 27, 2012; http://www.cdc.gov/obesity/adult/defining.html. Accessed 22 Feb 2016.
- 29.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG, World Health Organization, Department of Mental Health and Substance Dependence. AUDIT: the alcohol use disorders identification test: guidelines for use in primary care. Babor TF et al. (2nd ed). Geneva: World Health Organization; 2001. http://www.who.int/iris/handle/10665/67205. Accessed 12 Jan 2017.
- 30.Armstrong BG, Sloan M. Ordinal regression models for epidemiologic data. Am J Epidemiol. 1989;129:191–204. doi: 10.1093/oxfordjournals.aje.a115109. [DOI] [PubMed] [Google Scholar]
- 31.Ananth CV, Kleinbaum DG. Regression models for ordinal responses: a review of methods and applications. Int J Epidemiol. 1997;26(6):1323–1333. doi: 10.1093/ije/26.6.1323. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention Vital signs: prevalence, treatment, and control of hypertension. United States, 1999-2002 and 2005-2008. MMWR. 2011;60(4):103–108. [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion: adult obesity facts. September 21, 2015; http://www.cdc.gov/obesity/data/adult.html. Accessed 20 Feb 2016.
- 34.Dong KR, Must A, Tang AM, Beckwith CG, Stopka TJ. Competing priorities that rival health in adults on probation in Rhode Island: substance use recovery, employment, housing, and food intake. BMC Public Health. 2018;18(1):289. doi: 10.1186/s12889-018-5201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sirotin N, Hoover DR, Shi Q, Anastos K, Weiser SD. Food insecurity with hunger is associated with obesity among HIV-infected and at risk women in Bronx, NY. PLoS One. 2014;9(8):e105957. doi: 10.1371/journal.pone.0105957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martins DC, Gorman KS, Miller RJ, Murphy L, Sor S, Martins JC, et al. Assessment of food intake, obesity, and health risk among the homeless in Rhode Island. Public Health Nurs. 2015;32(5):453–461. doi: 10.1111/phn.12180. [DOI] [PubMed] [Google Scholar]
- 37.Vedovato GM, Surkan PJ, Jones-Smith J, et al. Food insecurity, overweight and obesity among low-income African-American families in Baltimore City: associations with food-related perceptions. Public Health Nutr. 2015:1–12. [DOI] [PMC free article] [PubMed]
- 38.Ivers LC, Cullen KA. Food insecurity: special considerations for women. Am J Clin Nutr. 2011;94(6):1740s–1744s. doi: 10.3945/ajcn.111.012617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The Sentencing Project. Mentally Ill Offenders in the Criminal Justice System: An Analysis and Prescription. 2002; http://www.sentencingproject.org/wp-content/uploads/2016/01/Mentally-Ill-Offenders-in-the-Criminal-Justice-System.pdf. Accessed 1 Apr 2017.
- 40.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The NSDUH Report: Trends in Substance Use Disorders among Males Aged 18 to 49 on Probation and Parole. March 6, 2014; http://www.samhsa.gov/data/sites/default/files/sr084-males-probation-parole/sr084-males-probation-parole/sr084-males-probation-parole.htm. Accessed 5 Oct 2015. [PubMed]
- 41.Lurigio AJ, Cho YI, Swartz JA, Johnson TP, Graf I, Pickup L. Standardized assessment of substance-related, other psychiatric, and comorbid disorders among probationers. Int J Offender Ther Comp Criminol. 2003;47(6):630–652. doi: 10.1177/0306624X03257710. [DOI] [PubMed] [Google Scholar]
- 42.Plugge E, Ahmed Abdul Pari A, Maxwell J, Holland S. When prison is "easier": probationers' perceptions of health and wellbeing. Int J Prison Health. 2014;10(1):38–46. doi: 10.1108/IJPH-01-2013-0001. [DOI] [PubMed] [Google Scholar]