Abstract
There are inconsistent findings regarding the rates of nonmedical prescription drug use (NMPDU) among Black Americans. The majority of previous studies used pharmaceutical names of drugs and relied on national data that excludes incarcerated populations, in which Black men are overrepresented. Therefore, the current study aimed to describe pre-incarceration rates of NMPDU among Black men in prison using culturally relevant alternative drug names. We recruited 208 incarcerated (adult age 18 or older) Black men nearing community reentry to urban counties from four state prisons in Kentucky. Results indicated the majority of participants engaged in lifetime NMPDU. The most commonly endorsed class of prescription drug was, “Other Sedatives, Hypnotics, and Tranquilizers” and the most commonly endorsed specific prescription drugs were “Syrup,” Lortab/Hydrocodone, and Xanax. There were significant age differences in the number of days that drugs were used in the year prior to incarceration. The current study contributes to the dearth of literature on NMPDU among Black Americans. These findings have implications for disease transmission, overdose risk, and culturally relevant data collection methods and interventions aimed at reducing NMPDU among Black men.
Keywords: Nonmedical, Prescription drugs, African American, Black, Men
Introduction
In the USA, prescription drugs are misused more often than any other illicit drug, with the exception of marijuana [1]. Generally, the media has depicted prescription drug misuse, particularly opioids, as a predominantly rural and suburban or “White” problem [2, 3]. However, recent data suggest Black Americans have similar rates of prescription drug misuse as Whites [4]. Recent data from the National Survey on Drug Use and Health (NSDUH) showed that 14.6% of Blacks reported lifetime NMPDU [5]. However, national surveys exclude incarcerated samples and Black men in particular are disproportionately incarcerated [6]. This indicates that many potential Black male nonmedical prescription drug users are not being accounted for in the rates produced by national surveys. The current study describes pre-incarceration rates of NMPDU among incarcerated Black men. This study contributes to the literature by establishing usage rates by age cohort among a segment of the Black community that is not well represented in previous research on NMPDU.
NMPDU among Black Americans
The extant literature on NMPDU focuses on racial comparisons. Although many studies examining usage rates of NMPDU have established that Whites misuse prescription drugs at higher rates than other races [7–16], there is evidence to suggest that there may be similar rates of misuse of certain classes of prescription drugs, such as opioids [4]. For example, Blacks and Whites may not significantly differ in nonmedical use of opioids across multiple geographical settings and age groups [17–20]. Further, there is evidence to suggest that Black users may even take prescription opioids nonmedically more often than Whites [21]. There is also inconsistent evidence on whether racial differences in NMPDU exist for stimulants, tranquilizers, and sedatives [22–24].
A common drug misused by Black men and women is codeine cough syrup. A series of studies by Peters and colleagues demonstrated frequent usage of “lean,” a concoction containing codeine cough syrup, among Blacks in Houston, Texas [25–27]. However, a later study found that codeine usage among college students was lower among Black students compared to students of other races [28]. One factor that may contribute to the inconsistent reports of Black opioid use is the way questions about use are measured. Studies that do not explicitly ask about codeine use, identify its alternative names (e.g., “lean,” “sizzurp,” “syrup”), or identify it as a prescription drug may not accurately ascertain the rates of misuse. Overall, these findings indicate that Blacks may misuse different classes of prescription drugs at different rates than Whites. The current study focused on incarcerated Black men nearing community reentry contributes to the limited research focused on Black Americans and may aid to clarify some the inconsistencies in reports of NMPDU.
NMPDU and Criminal Justice Involvement
Ex-offenders often return to their communities with poor social support and limited resources, which can be stressors that lead to relapse [29]. As such, recently released offenders with a history of NMPDU have an increased risk for poor post-release outcomes, including overdose [30, 31]. Potential negative post-release outcomes associated with NMPDU indicate Black men in prison with a history of NMPDU are vulnerable upon community reentry. The current study aimed to describe NMPDU in a sample of incarcerated Black men nearing reentry to urban counties. Further, we aimed to highlight the importance of measuring NMPDU in Black men by using common culturally relevant names for prescription drugs in conjunction with pharmaceutical names.
Methods
The data for the current study were derived from a larger study examining mental health and HIV risk among incarcerated Black men who were nearing community reentry. Participants were recruited from four minimum to medium security prisons in Kentucky. Men were eligible to participate in the study based on following criteria: [1] self-identified as African American or Black; [2] at least 18 years old; [3] willing to participate in the study; [4] eligible for community reentry within 120 days of participating in the study; and [5] returning to Jefferson or Fayette County, two urban counties in Kentucky. Participants were recruited through letters in the mail inviting them to participate in a health study and meet face-to-face with study staff.
Procedures
Research staff obtained written informed consent from each participant. Interviews were administered using Audio Computer Assisted Self-Interviewing (ACASI) techniques to enhance validity of responses due to the confidential and sensitive nature of the questions [32] and to assist with any potential literacy issues [33]. The interviewers were masters-level clinicians with experience working with prison populations. Participants were compensated $25 to complete the interview. The study was approved by the Kentucky Department of Corrections Research Ethics Committee and the University of Kentucky Institutional Review Board (IRB). The principal investigator obtained a Federal Certificate of Confidentiality to ensure responses remained confidential and could not be requested by a third party.
Measures
Dependent Variables
Lifetime Nonmedical Use of Prescription Drugs
A modified version of the Addiction Severity Index, fifth edition (ASI-V) [34] was administered to assess drug use. Participants were asked, Have you ever used ___ that was not prescribed to you? and responded either 1 = yes or 0 = no. The ASI-V was modified to include culturally relevant names of the drugs underneath each question to allow participants to easily identify classes of prescription medications they had used nonmedically. The culturally relevant names used in this study (Table 1) were chosen based on extensive clinical experience of the study team and were piloted prior to primary data collection.
Table 1.
Culturally relevant alternative drug names
| Drug name | Culturally relevant alternative name |
|---|---|
| Opiates | Subs |
| Hospital Heroin/Dilaudid | |
| Oxy | |
| Percs | |
| Norco | |
| Blue Pills | |
| Barbiturates | Quaalude |
| Ludes | |
| 714s | |
| Yellow Jackets | |
| Red Birds | |
| Goofballs | |
| Amphetamines | Ritalin |
| Adderall | |
| Meth | |
| Speed | |
| Rits | |
| Addies | |
| Truck Drivers | |
| Vitamin R | |
| Uppers | |
| Other sedatives, hypnotics, and tranquilizers | Syrup |
| Xanax | |
| Valium | |
| Klonopin | |
| A minus | |
| Totem Poles | |
| Footballs | |
| Bars | |
| School Buses | |
| Hulk | |
| Codeine | |
| Pancakes and Syrup | |
| Candy Blunt |
Nonmedical Use of Prescription Drugs in the Year Prior to Incarceration
For each of the 15 specific prescription drugs, participants were asked the following question: How many days in the year prior to incarceration did you use___?
Independent Variable
Age Cohort
Participants were divided by age cohort to examine differences in NMPDU by age group. There were three age cohorts that comprised the sample: 19–29, 30–39, and 40 years old and above [35].
Analytical Approach
All analyses were conducted using SPSS 24.0. Chi-square analyses were conducted to determine whether there were significant differences between age cohorts regarding lifetime use of the four classes of prescription drugs and the 15 specific prescription drugs. ANOVAs were conducted to assess whether there were significant differences in the mean number of days of prescription drug use in the year prior to incarceration between the three age cohorts. Data were positively skewed due to notable outliers reporting using nearly every day in the year before incarceration. A log transformation was completed and homogeneity of variance was met for each of the dependent variables.
Results
Sample Characteristics
A total of 208 Black men were recruited from prisons in the state of Kentucky. All demographic information was assessed via self-report and is presented in Table 2.
Table 2.
Demographics
| M | SD | Range | n | Percent | |
|---|---|---|---|---|---|
| Race/ethnicity | |||||
| Black/African American | 187 | ||||
| Black and bi-racial | 19 | ||||
| Black and Moorish American | 1 | ||||
| Black and Cuban | 1 | ||||
| Black and Puerto Rican | 1 | ||||
| Age (years) | 35.92 | 10.56 | 19.00–69.00 | ||
| 19–29 | 32.2 | ||||
| 30–39 | 38.0 | ||||
| 40 and above | 29.8 | ||||
| Education (years) | 12.00a | 2.53 | 6.00–16.00 | ||
| Partner status (1 = yes; 0 = no) | 18 | ||||
| Months of lifetime incarceration | 72.00a | 84.00 | 1.00–420.00 | ||
aMedian years of education and months of lifetime incarceration
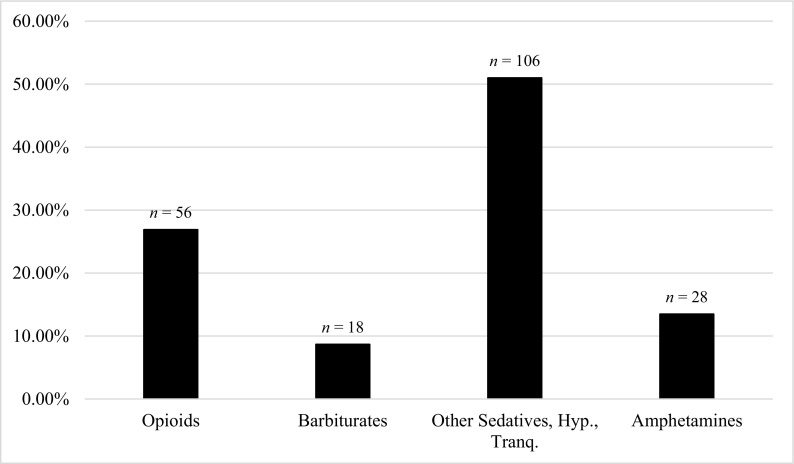
Lifetime Nonmedical Use of Prescription Drugs
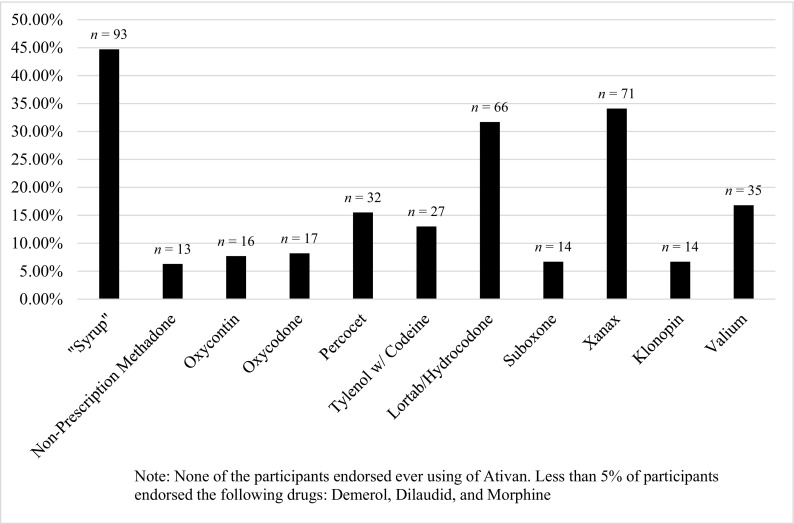
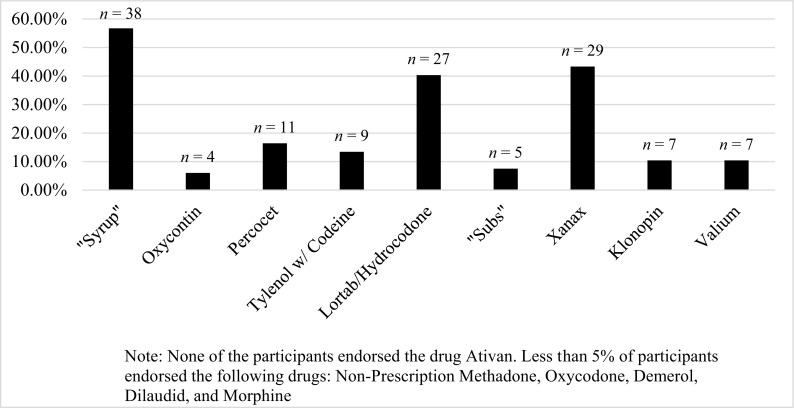
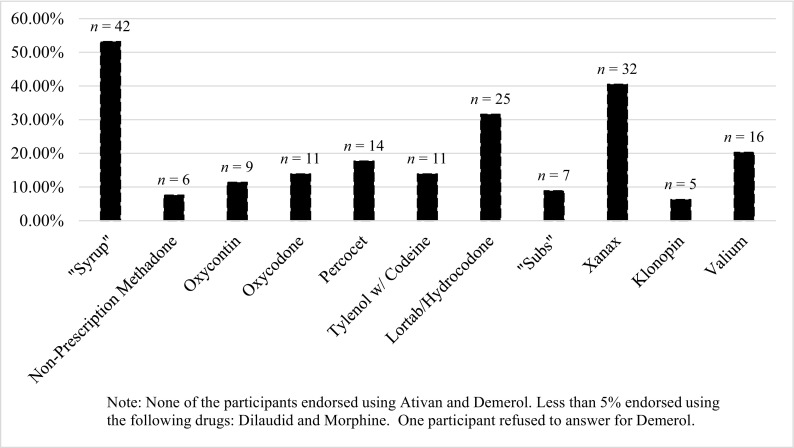
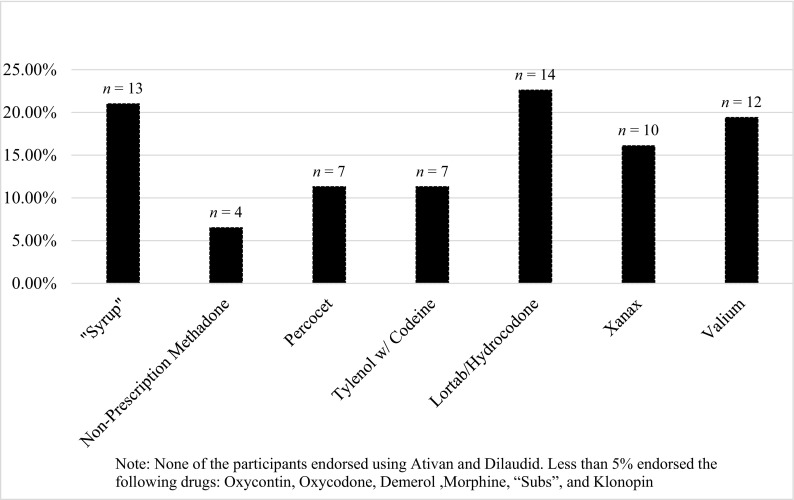
Among all participants, 58.2% reported ever using prescription drugs that had not been prescribed to them. Rates of lifetime NMPDU among each age cohort were as follows: 64.2% of 19 to 29 year olds, 67.1% of 30 to 39 year olds, and 41% of participants aged 40 years and above. The most commonly used substance among the entire study sample was “Syrup,” or cough syrup with codeine, with approximately 45% of the sample reporting lifetime use (n = 93). Xanax (n = 71) and Lortab/Hydrocodone (n = 66) were the next most commonly endorsed drugs (Fig. 1). Rates of lifetime use of the 15 prescription drugs for each age cohort are presented in Figs. 2, 3, and 4. The 40-years-old and above cohort’s (n = 62) highest reports of lifetime use were in “Syrup” (21.0%), Lortab/Hydrocodone (22.6%), and Valium (19.4%). This group was the only one to have high usage rates of Valium compared to other substances and to not use “Syrup” most frequently (Fig. 4).
Fig. 1.
Lifetime nonmedical use of 15 specific prescription drugs
Fig. 2.
Lifetime nonmedical use of specific prescription drugs: 19–29 year olds (n = 67)
Fig. 3.
Lifetime nonmedical use of specific prescription drugs: 30–39 year olds (n = 79)
Fig. 4.
Lifetime nonmedical use of specific prescription drugs: 40 years old and above (n = 62)
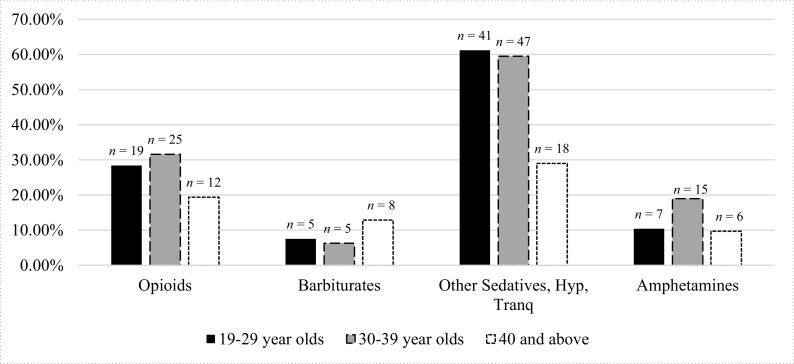
The most commonly endorsed category of drug use was other sedatives, hypnotics, and tranquilizers (n = 106). Opioids were the second most commonly used drug class (n = 56), followed by amphetamines, and barbiturates (Fig. 5). Among users of other sedatives, tranquilizers, and hypnotics, there was a significant association between age group and lifetime use, χ2(2, N = 208) = 17.433, p < 0.001. Specifically, participants aged 40 years and above had lower rates of lifetime use of other sedatives, tranquilizers, and hypnotics than the other age cohorts (Fig. 6). Results regarding specific drugs indicated for “Syrup,” there was a significant difference between age cohort and lifetime use of the drug with a medium effect size, χ2(2, N = 208) = 20.329, p < 0.001, Cramer’s V = 0.313. There was also a significant difference among age cohorts with regard to lifetime use of Xanax with a medium effect size, χ2(2, N = 208) = 12.861, p = 0.002, Cramer’s V = 0.249.
Fig. 5.
Lifetime nonmedical use of prescription drug use (N = 208)
Fig. 6.
Percentages of each age group reporting lifetime use of each drug class
Nonmedical Use of Prescription Drugs in the Year Prior to Incarceration
The mean number of days participants used “Syrup” in the year prior to incarceration was 42.1 days and participants reported using Xanax 46.5 days. Usage rates leading up to incarceration were highest for Lortab/Hydrocodone, with an average of 70.9 days. ANOVA analyses examining differences between the age cohorts in the mean number of days of use in the year leading up to incarceration showed there was no significant difference between the three age groups and the log of the mean days of use of “Syrup,” F(2, 88) = 2.403, p = 0.096, and Lortab/Hydrocodone, F(2, 62) = 1.670, p = 0.197. However, there was a significant difference between age groups and the log of the mean days of use of Xanax in the year leading up to incarceration, F(2, 68) = 3.360, p = 0.041. Post hoc analyses using Tukey’s test showed 19 to 29 years old used Xanax significantly more frequently in the year prior to incarceration than men in the 40 years and above cohort. The 30- to 39-year-old cohort did not significantly differ from either of the other age groups with regard to NMPDU in the year prior to incarceration (see Table 3).
Table 3.
One-way ANOVA: difference between age cohorts of mean number of days of drug use in year prior to incarceration
| Drug | n | Source of variation | df | Sums of squares | Mean square | F | p |
|---|---|---|---|---|---|---|---|
| “Syrup” | 91 | Between | 2 | 2.736 | 1.368 | 2.403 | 0.096 |
| Within | 88 | 50.099 | .569 | – | – | ||
| Lortab/Hydrocodone | 65 | Between | 2 | 1.865 | .993 | 1.670 | 0.197 |
| Within | 62 | 34.628 | .559 | – | – | ||
| Xanax | 71 | Between | 2 | 3.955 | 1.978 | 3.360 | 0.041 |
| Within | 68 | 40.021 | .589 | – | – |
Discussion
The current study contributes to the literature by highlighting the frequency of lifetime and past year nonmedical use of prescription drugs among incarcerated Black men. Over half of the men in our sample reported lifetime NMPDU, compared to 14.6% of Blacks surveyed by NSDUH [5]. Our finding that the most commonly used prescription drug was “Syrup,” or codeine cough syrup, is critical because codeine may not be recognized as an opioid analgesic in national survey studies and therefore, may not be accurately assessed in Black populations [36]. In addition, results suggest that there are age-related differences in the types of prescription drugs most commonly misused. Specifically, the oldest cohort was more likely to report Valium use than Xanax, which are both benzodiazepines. Xanax replaced Valium as a popular benzodiazepine in recent decades because of its decreased half-life and reduced side effects [37]. Therefore, it is possible that participants aged 40 years and above had greater access to Valium in their lifetime than participants in their 20s. However, it is important to note the oldest cohort still used Xanax at a substantial rate, with 16.1% reporting lifetime use.
A key factor that could be impacting current understanding of rates of prescription drug use among Black Americans is the way that drug use is measured. The current study was one of the only studies to use culturally relevant common alternative names of prescription drugs when asking about NMPDU. Golub and colleagues noted that is important to investigate the extent to which youth recognize “sizzurp” (“Syrup”), or codeine cough syrup, as a prescription drug and can accurately report use in surveys [36]. Black users may be more likely to misuse prescription drugs they obtained from other means rather than from their own prescription [22, 38]. Therefore, it is likely that they may be more readily able to identify these drugs by the names that are used by dealers, names used in their communities, or names used in culturally relevant media outlets rather than by their formal pharmaceutical names.
The high rates of NMPDU prior to incarceration in this sample have significant community-level health implications because approximately 95% of incarcerated persons are released [39]. Notably, nonmedical prescription drug users are more likely to report multiple sex partners, having sex after drinking or using drugs, engaging in more unprotected sex acts, and trading sex for money [26, 40]. NMPDU also often precedes the initiation of injection drug use [41]. These behaviors all pose an increased risk for HIV and HCV infection in Black communities with staggering heath disparities [42, 43].
People who misuse prescription drugs prior to incarceration are also at a greater risk for death from prescription drug overdose [30, 31]. Our study indicated that over half of incarcerated Black men had a substantial history of NMPDU prior to incarceration, increasing their vulnerability at reentry. Intervention efforts aimed at reducing NMPDU among Black men prior to release, such as medication-assisted therapy (MAT), could help mediate these overdose risks and have been effective in reducing NMPDU among incarcerated populations [44, 45]. However, culturally relevant factors and barriers to treatment, such as lacking insurance [44], should be addressed when implementing MAT among this population.
Limitations and Future Research
Although the findings of the current study make a significant contribution to the literature on NMPDU, there are some limitations. First, data for this study came from incarcerated Black men nearing community reentry into two urban counties in Kentucky; therefore, it is possible that these results are not generalizable to other regions in the USA. In addition, our findings are likely not generalizable to Black women and Black Americans without a history of criminal justice involvement. Secondly, we primarily aimed to examine prevalence rates of NMPDU in an understudied group; thus, the descriptive and cross-sectional nature of this study does not allow us to imply causational relationships involving NMPDU among Black males. Third, the list of drugs examined is far from exhaustive; there are likely other prescription drugs with abuse potential that were not examined here. Further, the study collected no data on how participants obtained the prescriptions. Lastly, the current study was unable to control for length of current incarceration when assessing prescription drug misuse in the time leading up to incarceration. Therefore, recall bias is possible, and was likely greater for participants who had been incarcerated longer than others.
The results of this study provide further evidence that nonmedical use of prescription drugs is not solely a “White” phenomenon [2, 3] and indicates that measurement of drug use and intervention efforts should incorporate culturally relevant approaches. Specifically, future research should use culturally relevant names of prescription drugs in conjunction with pharmaceutical names in order to more accurately assess use among Black populations. The results also highlight the need for more within-group examination of drug use among Blacks rather than operationalizing race as a covariate in NMPDU studies or using Whites as a reference group to establish usage rates among other racial groups. Lastly, future studies should also examine rates of NMPDU among Black incarcerated women using culturally relevant common alternative names of prescription drugs. Undoubtedly, NMPDU among Black Americans is an area ripe for study.
Acknowledgements
The authors gratefully acknowledge research support from the National Institute on Drug Abuse with the National Institutes of Health under award number K08DA032296. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.SAMHSA. Key Substance Use and Mental Health Indicators in the United States: results from the 2016 National Survey on Drug Use and Health. NSDUH Series H-52 2017; https://www.samhsa.gov/data/. Published September 2017. Accessed November 12, 2017.
- 2.Netherland J, Hansen HB. The war on drugs that wasn’t: wasted whiteness, “Dirty Doctors,” and race in media coverage of prescription opioid misuse. Cult Med Psychiatry. 2016;40(4):664–686. doi: 10.1007/s11013-016-9496-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Netherland J, Hansen H. White opioids: pharmaceutical race and the war on drugs that wasn't. BioSocieties. 2017;12(2):217–238. doi: 10.1057/biosoc.2015.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hughes A, Williams MR, Lipari RN, Bose J, Copello EAP, Kroutil LA. Prescription Drug Use and Misuse in the United States: results from the 2015 National Survey on Drug Use and Health. Rockville, MD:SAMHSA; 2016.
- 5.SAMHSA. Results from the 2013 National Survey on Drug Use and Health: detailed tables. NSDUH series H-48, HHS publication no. (SMA) 14–4863. Rockville, MD: Substance Abuse and Mental Health Services Administration. Published 2014. Accessed March 1, 2018.
- 6.Pettit . Invisible men: mass incarceration and the myth of Black progress. The Russel Sage Foundation: New York, NY; 2012. [Google Scholar]
- 7.Striley CW, Kelso-Chichetto NE, Cottler LB. Nonmedical prescription stimulant use among girls 10–18 years of age: associations with other risky behavior. J Adolesc Health. 2017;60(3):328–332. doi: 10.1016/j.jadohealth.2016.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCabe SE. Correlates of nonmedical use of prescription benzodiazepine anxiolytics: results from a national survey of U.S. college students. Drug Alcohol Depend. 2005;79(1):53–62. doi: 10.1016/j.drugalcdep.2004.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miech R, Bohnert A, Heard K, Boardman J. Increasing use of nonmedical analgesics among young cohorts in the United States: a birth cohort effect. J Adolesc Health. 2013;52(1):35–41. doi: 10.1016/j.jadohealth.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cranford JA, McCabe SE, Boyd CJ. Adolescents’ nonmedical use and excessive medical use of prescription medications and the identification of substance use subgroups. Addict Behav. 2013;38(11):2768–2771. doi: 10.1016/j.addbeh.2013.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conn BM, Marks AK. Ethnic/racial differences in peer and parent influence on adolescent prescription drug misuse. J Dev Behav Pediatr. 2014;35(4):257–265. doi: 10.1097/DBP.0000000000000058. [DOI] [PubMed] [Google Scholar]
- 12.Monnat SM, Rigg KK. Examining rural/urban differences in prescription opioid misuse among US adolescents. J Rural Health. 2015;32:204–218. doi: 10.1111/jrh.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khosla N, Juon HS, Kirk GD, Astemborski J, Mehta SH. Correlates of non-medical prescription drug use among a cohort of injection drug users in Baltimore City. Addict Behav. 2011;36(12):1282–1287. doi: 10.1016/j.addbeh.2011.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pletcher MJ, Kertesz SG, Sidney S, Kiefe CI, Hulley SB. Incidence and antecedents of nonmedical prescription opioid use in four US communities: the Coronary Artery Risk Development in Young Adults (CARDIA) prospective cohort study. Drug Alcohol Depend. 2006;85(2):171–176. doi: 10.1016/j.drugalcdep.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21–31. doi: 10.1097/chi.0b013e31815a56f1. [DOI] [PubMed] [Google Scholar]
- 16.Kelly BC, Wells BE, LeClair A, Tracy D, Parsons JT, Golub SA. Prevalence and correlates of prescription drug misuse among socially active young adults. Int J Drug Policy. 2013;24(4):297–303. doi: 10.1016/j.drugpo.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang KH, Becker WC, Fiellin DA. Prevalence and correlates for nonmedical use of prescription opioids among urban and rural residents. Drug Alcohol Depend. 2013;127(1–3):156–162. doi: 10.1016/j.drugalcdep.2012.06.027. [DOI] [PubMed] [Google Scholar]
- 18.Ford JA, Rigg KK. Racial/ethnic differences in factors that place adolescents at risk for prescription opioid misuse. Prev Sci. 2015;16(5):633–641. doi: 10.1007/s11121-014-0514-y. [DOI] [PubMed] [Google Scholar]
- 19.McCabe SE, West BT, Boyd CJ. Medical use, medical misuse, and nonmedical use of prescription opioids: results from a longitudinal study. Pain. 2013;154(5):708–713. doi: 10.1016/j.pain.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salas J, Scherrer JF, Lustman PJ, Schneider FD. Racial differences in the association between nonmedical prescription opioid use, abuse/dependence, and major depression. Subst Abuse. 2016;37(1):25–30. doi: 10.1080/08897077.2015.1129523. [DOI] [PubMed] [Google Scholar]
- 21.Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA. 2015;314(14):1468–1478. doi: 10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- 22.Herman-Stahl MA, Krebs CP, Kroutil LA, Heller DC. Risk and protective factors for nonmedical use of prescription stimulants and methamphetamine among adolescents. J Adolesc Health. 2006;39(3):374–380. doi: 10.1016/j.jadohealth.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Oluwoye O, Merianos AL, Nabors LA. Nonmedical use of prescription drugs and peer norms among adolescents by race/ethnicity. J Subst Use. 2017;22(2):199–205. doi: 10.1080/14659891.2016.1177615. [DOI] [Google Scholar]
- 24.McCabe SE, West BT, Wechsler H. Trends and college-level characteristics associated with the non-medical use of prescription drugs among US college students from 1993 to 2001. Addiction. 2007;102(3):455–465. doi: 10.1111/j.1360-0443.2006.01733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peters R, Yacoubian GS, Rhodes W, Forsythe KJ, Bowers KS, Eulian VM, Mangum CA, O'Neal JD, Martin Q, Essien EJ. Beliefs and social norms about codeine and promethazine hydrochloride cough syrup (CPHCS) use and addiction among multi-ethnic college students. J Psychoactive Drugs. 2007;39(3):277–282. doi: 10.1080/02791072.2007.10400614. [DOI] [PubMed] [Google Scholar]
- 26.Peters RJ, Williams M, Ross MW, Atkinson J, Yacoubian GS. Codeine cough syrup use among African-American crack cocaine users. J Psychoactive Drugs. 2007;39(1):97–102. doi: 10.1080/02791072.2007.10399868. [DOI] [PubMed] [Google Scholar]
- 27.Peters RJ, Jr, Amos C, Jr, Meshack A, et al. Codeine cough syrup use among sexually active, African-American high school youths: why southern males are down to have sex. Am J Addict. 2007;16(2):144–145. doi: 10.1080/10550490601186246. [DOI] [PubMed] [Google Scholar]
- 28.Agnich LE, Stogner JM, Miller BL, Marcum CD. Purple drank prevalence and characteristics of misusers of codeine cough syrup mixtures. Addict Behav. 2013;38(9):2445–2449. doi: 10.1016/j.addbeh.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 29.Binswanger IA, Nowels C, Corsi KF, Glanz J, Long J, Booth RE, Steiner JF. Return to drug use and overdose after release from prison: a qualitative study of risk and protective factors. Addict Sci Clinical Pract. 2012;7:3. doi: 10.1186/1940-0640-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592–600. doi: 10.7326/0003-4819-159-9-201311050-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Binswanger IA, Stern MF, Yamashita TE, Mueller SR, Baggett TP, Blatchford PJ. Clinical risk factors for death after release from prison in Washington State: a nested case-control study. Addiction. 2016;111(3):499–510. doi: 10.1111/add.13200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Djawe K, Brown EE, Gaul Z, Sutton M. Community-based electronic data collections for HIV prevention research with black/African-American men in the rural, southern USA. AIDS Care. 2014;26(10):1309–1317. doi: 10.1080/09540121.2014.911812. [DOI] [PubMed] [Google Scholar]
- 33.Schneider SJ, Edwards B. Developing usability guidelines for AudioCasi respondents with limited literacy skills. J Offl Stat. 2000;16(3):255. [Google Scholar]
- 34.McLellan AT, Kushner H, Metzger D, et al. The fifth edition of the addiction severity index. J Subst Abus Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-S. [DOI] [PubMed] [Google Scholar]
- 35.Grant JD, Vergés A, Jackson KM, Trull TJ, Sher KJ, Bucholz KK. Age and ethnic differences in the onset, persistence and recurrence of alcohol use disorder. Addiction. 2012;107(4):756–765. doi: 10.1111/j.1360-0443.2011.03721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Golub A, Elliott L, Brownstein HH. The opiate pain reliever epidemic among US arrestees 2000–2010: regional and demographic variations. J Ethn Subst Abus. 2013;12:1):1–1)29. doi: 10.1080/15332640.2013.759498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller L. Listening to Xanax: how America learned to stop worrying about worrying and pop its pills instead. NY Mag. https://www.nymag.com/news/features/xanax-2012-3/index2.html. Published 2012. Accessed November 12, 2017.
- 38.Kelley-Baker T, Waehrer G, Pollini A. Prevalence of self-reported prescription drug use in a national sample of U.S. drivers. J Stud Alcohol Drugs. 2017;78(1):30–38. doi: 10.15288/jsad.2017.78.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hughes T, Wilson D. Reentry trends in the United States. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics;2004.
- 40.Benotsch EG, Koester S, Luckman D, Martin AM, Cejka A. Non-medical use of prescription drugs and sexual risk behavior in young adults. Addict Behav. 2011;36(1–2):152–155. doi: 10.1016/j.addbeh.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 41.SAMHSA. Racial and ethnic minority populations. https://www.samhsa.gov/specific-populations/racial-ethnic-minority. Updated January 17, 2018. Accessed November 12, 2017.
- 42.Centers for Disease Control and Prevention. HIV among African Americans.https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/cdc-hiv-aa-508.pdf. Published February 2017. Accessed November 14, 2017.
- 43.Centers for Disease Control and Prevention. Hepititis C disproportionately affects the African American community. https://www.cdc.gov/hepatitis/blackhistmnth-hepc.htm. Updated February 1, 2017. Accessed November 14, 2017.
- 44.Lee JD, Grossman E, Truncali A, Rotrosen J, Rosenblum A, Magura S, Gourevitch MN. Buprenorphine-naloxone maintenance following release from jail. Subst Abuse. 2012;33(1):40–47. doi: 10.1080/08897077.2011.620475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Magura S, Lee JD, Hershberger J, Joseph H, Marsch L, Shropshire C, Rosenblum A. Buprenorphine and methadone maintenance in jail and post-release: a randomized clinical trial. Drug Alcohol Depend. 2009;99(1–3):222–230. doi: 10.1016/j.drugalcdep.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]