Abstract
Returning to the community after incarceration is a particularly vulnerable time with significantly increased risk of death in the first 2 weeks. The elevated risk of death persists as long as 2 years, with cardiovascular disease (CVD) among the leading causes. African-Americans, especially African-American men, have higher rates of incarceration and community supervision (e.g., probation and parole) and an earlier onset of hypertension compared to Whites. Few studies have objectively assessed the cardiovascular health profile of criminal justice involved individuals. This study is designed to determine the cardiovascular health profile among men in community corrections and/or transitional housing, identify the prevalence of key CVD risk factors, and assess if risk varies by race/ethnicity. We recruited 100 adult men (mean age = 42.7, SD = 11.35, 60% White, 40% non-Hispanic White) with a history of incarceration in jail or prison of ≥ 6 months during their most recent incarceration and enrolled in a community corrections program. Using the American Heart Association’s Life’s Simple 7™ (LS-7), measures of each of the LS-7 components (body mass index, blood pressure, lipids, blood glucose, smoking, diet, and physical activity) were obtained, and LS-7 scores were generated for each measure using AHA-defined categories of poor (1 point), intermediate (2 points), and ideal (3 points) and summed to yield a total score ranging from poor for all (7 points) to ideal for all (21 points). Mann-Whitney U tests were performed to assess differences in LS-7 scores (poor, intermediate, ideal) by race/ethnicity. Additionally, an independent samples t test was conducted for race/ethnicity and LS-7 total score. Mann-Whitney U tests for LS-7 categories and race/ethnicity indicated a greater number of non-Whites had poor blood pressure (p < .01) and diet (p < .05) as compared to Whites. The independent samples t test demonstrated significantly lower LS-7 scores for non-Whites compared to Whites. To our knowledge, this is the first study to evaluate cardiovascular health among individuals with a history of incarceration using the LS-7 metric, which included objective measures for four of the seven LS-7 metrics. Non-Whites, which included African-Americans, Hispanics, and American Indians, were more likely than Whites to fall into the poor category for both diet and blood pressure and had significantly lower total LS-7 scores than Whites, indicating they have worse scores across all seven of the LS-7 measures. Similar to what is found among non-incarcerated samples, non-Whites with incarceration histories are at elevated risk for cardiovascular events relative to their White peers.
Keywords: Community corrections, Incarceration, Cardiovascular risk, Cardiovascular health, Life’s Simple 7 (TM)
Introduction
The USA has the highest incarceration rate of any other country in the world. Currently, 6.7 million people are under US correctional supervision. Of this 6.7 million, 4.6 million are under community supervision, and 2.1 million are incarcerated [1]. The Urban Institute projects that over 95% of prisoners will return to the community [2], and most will return with a multitude of health issues, with cardiovascular disease (CVD) being among the most prevalent [3]. Returning to the community is a particularly vulnerable time with an approximately 12-fold increased risk of death in the first 2 weeks after release and 3.5-fold increased risk across almost 2 years, with cardiovascular disease (CVD) among the leading causes [4]. Increasing evidence suggests that incarceration is associated with a higher burden of CVD risk factors such as low socioeconomic status (SES), hypertension, and poor post-release health behaviors such as eating fast food and smoking [3, 5–9]. Public health and criminal justice experts have called for further study of the association of criminal justice system involvement with health disparities since both disproportionately affect minorities, particularly those of low income and/or educational status [10–15].
Community corrections include non-confined forms of supervision for persons facing conviction or who have already been convicted. Parole and probation are the most well-known forms of community corrections which also include, but is not limited to home confinement, electronic monitoring, work release, and diversion programs such as Drug Court. Community-based transitional housing programs are key partners to community corrections programs, as they frequently provide supportive housing, education programs, job training and placement, and social support to help foster self-sufficiency. The structure for regular access to services and accountability in community corrections and transitional housing programs allows for easy integration of additional services and monitoring of outcomes. In contrast to incarcerated persons, individuals in community corrections and transitional housing programs are living in the community and aside from any court-ordered programs (e.g., drug treatment), they may have increased autonomy to engage in health behaviors daily activities (e.g., diet, exercise, medication adherence) to manage and control chronic disease [16]. Care for chronic diseases such as hypertension during incarceration is fraught with challenges due to heterogeneity of quality and quantity of care provided in correctional facilities, and the majority of this population experiences significant barriers to establishing care when reentering the community [6, 15]. Therefore, community correction programs and/or community-based transitional housing programs offer a novel opportunity for CVD risk reduction interventions for a population at high risk for poor health outcomes [11, 13, 15, 17–19].
The American Heart Association (AHA) has developed the Life’s Simple 7™ (LS-7) as a cardiovascular health profile comprised of measures of CVD risk factors including blood pressure, cholesterol, glucose, body mass index, smoking, physical activity, and diet [20]. The LS-7 metric characterizes health based on the presence of favorable health behaviors (i.e., abstinence from smoking within the last year, ideal body mass index (BMI), meeting recommended levels of physical activity, and favorable dietary patterns), favorable health factors (i.e., untreated total cholesterol under 200 mg/dL, abstinence of diabetes mellitus, and untreated blood pressure < 120/< 80 mmHg), and the absence of any CVD history (stroke, heart attack, and etc.). LS-7 showed a graded relationship with CVD incidence and all-cause mortality and has been shown to be associated with improvement in longevity by preventing many other chronic illnesses [20–22].
African-Americans, especially African-American men, have higher rates of incarceration, probation, and parole compared to Whites [23]. African-Americans also have less favorable LS-7 profiles which contributes to racial/ethnic disparities in CV outcomes [24, 25]. Because most national studies of correctional populations have relied primarily on inmate self-report, limited data are available on LS-7 components measured objectively by clinical exam among correctional populations in the USA [26, 27]. Our study is designed to determine the cardiovascular health profile, as defined by AHA’s LS-7, among formerly incarcerated men in community corrections and/or transitional housing, in order to establish and/or confirm the prevalence of key CVD risk factors amenable to behavioral interventions and compare risk factor prevalence by race/ethnicity.
Methods
Participants
We recruited 100 adult men (aged 19 or older as state law defined age of consent as 19 or older) with a history of incarceration ≥ 6 months during their most recent incarceration and enrolled in the UAB Community Corrections/Treatment Alternatives for Safer Communities (TASC) community corrections program and/or housed at The Foundry Ministries, a community-based organization that provides a transitional housing program to individuals returning to the community upon release from prison. Both programs are located in Jefferson County, Alabama. Informed consent was obtained from all participants, and the protocol was approved by the University of Alabama at Birmingham’s Institutional Review Board.
Protocol and Measures
Measures of each of the LS-7 components, including height, weight, blood pressure, lipids, and blood glucose as well as assessments of smoking, diet, and physical activity via short survey were obtained using standardized and quality controlled approaches at either TASC or The Foundry Ministries. Lipid and non-fasting glucose measures were obtained utilizing CLIA-waived point-of-care testing systems (lipids and random glucose: Cardiochek Plus Analyzer, PTS Diagnostics; Hemoglobin A1c: DCA Vantage Analyzer, Siemens). BMI was calculated based on height and weight measured by a digital scale (Seca 813) and stadiometer (Seca 213). Blood pressure was obtained using the clinically validated Omron BP785 DIGITAL 10 Series Blood Pressure monitor.
LS-7 scores were generated for each measure (BMI, blood pressure, total cholesterol, glycemic control, smoking status, diet, physical activity) using AHA-defined categories of poor (1 point), intermediate (2 points), and ideal (3 points), and summed to yield a total score ranging from poor for all (7 points) to ideal for all (21 points) (Table 1). We used glucose, but when missing (n = 58), we substituted A1C measurement (ideal < 5.7%, intermediate 5.7 to 6.4%, poor ≥ 6.5%) to have a measure of glycemic control.
Table 1.
Ideal, Intermediate, and poor levels of Life’s Simple 7 components
| Component | Ideal (2 points) | Intermediate (1 point) | Poor (0 point) |
|---|---|---|---|
| Smoking | Never or former > 1 year | Former ≤ 1 year | Current |
| Healthy diet score* | 4 to 5 points | 2 to 3 points | 0 to 1 point |
| Physical activity+ | ≥ 150 min/week moderate intensity or ≥ 75 min/week vigorous intensity |
1 to 149 min/week moderate intensity or 1 to 74 min/week vigorous intensity or 1 to 149 min/week moderate + vigorous intensity |
None |
| Body mass index | < 25 kg/m2 | 25 to 29.9 kg/m2 | ≥ 30 kg/m2 |
| Blood pressure | SBP < 120 mmHg AND DBP < 80 mmHg untreated |
SBP 120–139 mmHg or DBP 80–89 mmHg or treated to ideal level |
SBP ≥ 140 mmHg or DBP ≥ 90 mmHg |
| Total cholesterol | < 200 mg/dL untreated | 200 to 239 mg/dL or treated to ideal level |
≥ 240 mg/dL |
| Glucoseǂ | |||
| Fasting | < 100 mg/dL untreated | 100 to 125 mg/dL or treated to ideal level |
≥ 126 mg/dL |
| Random | 100–125 mg/dL untreated | 140 to 199 mg/dL | ≥ 200 mg/dL |
| A1c | < 5.7% | 5.7 to 6.4% | ≥ 6.5% |
DBP indicates diastolic blood pressure; SBP, systolic blood pressure
*Based on American Heart Association definitions of 5 healthy diet components, each worth 1 point:
1) fruits and vegetables: ≥ 4.5 cups per day
2) fish: ≥ two 3.5-oz servings per week (preferably oily fish)
3) fiber-rich whole grains (≥ 1.1 g of fiber per 10 g of carbohydrate): ≥three 1-oz-equivalent servings per day;
4) sodium: < 1500 mg per day
5) sugar-sweetened beverages: ≤ 450 kcal (36 oz) per week
+American Heart Association definition
ǂ Categories based on the American Diabetes Association (ADA) criteria for the diagnosis of diabetes and prediabetes (Ref: Diabetes Care 2011; 34:S11)
Statistical Analysis
Descriptive statistics were generated for the individual components and total score of the LS-7. Because of the low representation of Native American/American Indian and Hispanic/Latino participants (n = 4), race/ethnicity was divided into two groups: non-Hispanic White (N = 36) and non-White (African-American, Native American/American Indian, and Hispanic/Latino, N = 64), and Mann-Whitney U tests were performed to assess differences in LS-7 scores (poor, intermediate, ideal) by race/ethnicity. Additionally, an independent samples t test was conducted for race/ethnicity and LS-7 total score. We conducted sensitivity analyses by repeating these analyses and excluding the Native American/American Indian and Hispanic/Latino participants (n = 4) and including only the non-Hispanic White and non-Hispanic Black participants.
Results
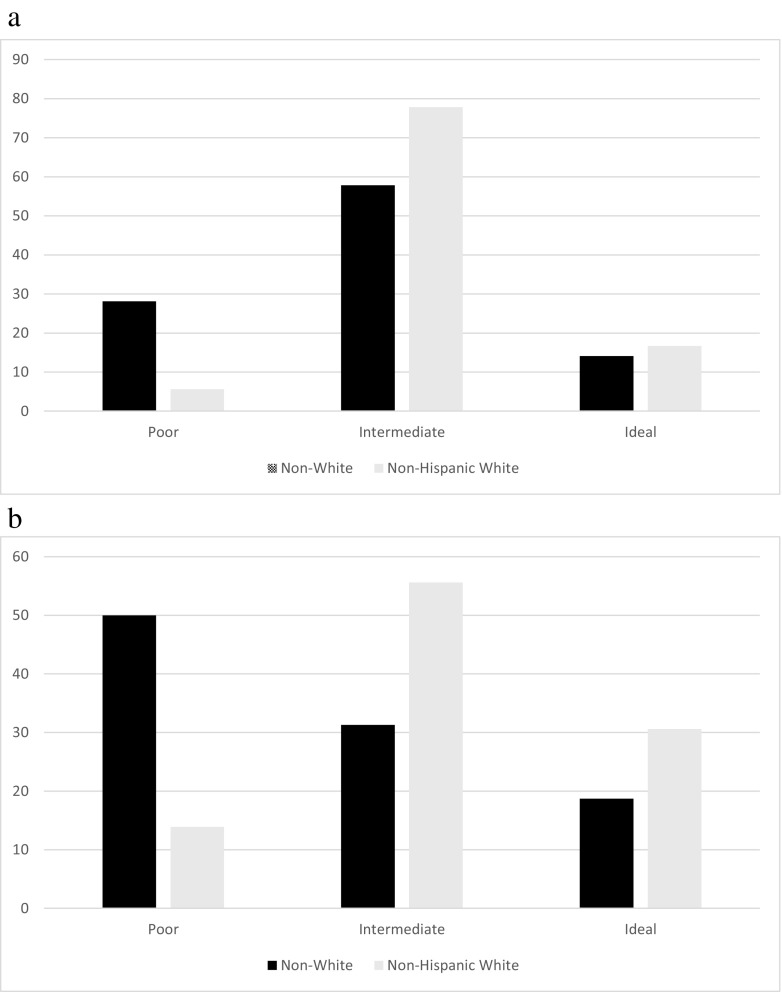
We recruited 100 participants who were 60% African-American, 36% White, 2% Native American, and 2% Hispanic. Although 40% of the sample did not graduate high school, the majority completed high school with 40% having obtained their GED or high school diploma and 20% with at least some education after high school. The majorities of the participants were unemployed (51%) or disabled (16%), with only 27% working full-time and 4% working part-time, and 16% were disabled. Most the participants reported little or no annual income, with 48% of participants reporting no yearly income (Table 2). LS-7 scores overall and by race are summarized in Table 3. Mann-Whitney U tests for LS-7 categories and race/ethnicity yielded significant results for two measures (Table 3): diet (U = 843.0, p < 0.05, r = 0.21; Fig. 1a) and blood pressure (U = 683.0, p < 0.01, r = 0.33; Fig. 1b). A greater number of non-Whites had poor blood pressure and diet as compared to Whites. The independent samples t test assessing differences in LS-7 scores by race/ethnicity was significant (t = − 2.45, p < 0.05), demonstrating significantly lower LS-7 scores for non-Whites compared to Whites. When we compared African-Americans to non-Whites and excluded other racial groups (N = 4), a similar pattern of results was seen, so the other racial groups were combined with African-Americans.
Table 2.
Demographic information
| M (SD) | |
| Age | 42.7 (11.4) |
| BMI | 28.1 (8.0) |
| HDL | 43.8 (15.1) |
| LDL | 68.1 (32.2) |
| Glucose | 119.1 (68.9) |
| % | |
| Race | |
| African-American | 60.0 |
| Non-Hispanic White | 36.0 |
| Native American | 2.0 |
| Hispanic/Latino | 2.0 |
| Highest education achieved | |
| Less than high school | 40.0 |
| High school or GED | 40.0 |
| More than high school | 20.0 |
| Employment status | |
| Full-time | 27.0 |
| Part-time | 4.0 |
| Unemployed | 51.0 |
| Disabled | 16.0 |
| Non-White | 2.0 |
| Yearly household income | |
| None | 48.0 |
| Less than $10,000 | 9.2 |
| $10,000–$19,999 | 15.3 |
| $20,000–$39,000 | 20.4 |
| $40,000 or more | 7.1 |
Table 3.
Life’s Simple 7 scores overall and Mann-Whitney U tests for individual LS7 scores by race, df = 2, LS7 total mean = 8.3, SD = 1.9
| LS7 measure | Race | LS7 rating n (%) | U | p value | r | ||
|---|---|---|---|---|---|---|---|
| Poor | Intermediate | Ideal | |||||
| Diet | Overall | 20 (20.0) | 65 (65.0) | 15 (15.0) | 843.0 | 0.036 | 0.21 |
| Non-White | 18 (30.0) | 33 (55.0) | 9 (15.0) | ||||
| Non-Hispanic White | 2 (5.6) | 28 (77.8) | 6 (16.7) | ||||
| Blood pressure | Overall | 37 (37.0) | 40 (40.0) | 23 (23.0) | 683.0 | 0.001 | 0.33 |
| Non-White | 31 (51.7) | 18 (30.0) | 11 (18.3) | ||||
| Non-Hispanic White | 5 (13.9) | 20 (55.6) | 11 (30.5) | ||||
| Smoking | Overall | 78 (78.0) | 6 (6.0) | 16 (16.0) | 1052.0 | 0.77 | 0.03 |
| Non-White | 48 (80.0) | 4 (6.7) | 8 (13.3) | ||||
| Non-Hispanic White | 28 (77.8) | 2 (5.6) | 6 (16.7) | ||||
| BMI | Overall | 29 (31.2) | 31 (33.3) | 33 (35.5) | 787.5 | 0.11 | 0.17 |
| Non-White | 22 (40.7) | 15 (27.8) | 17 (31.5) | ||||
| Non-Hispanic White | 7 (19.4) | 15 (41.7) | 14 (38.9) | ||||
| Exercise | Overall | 6 (6.0) | 7 (7.0) | 87 (87.0) | 1032.5 | 0.55 | 0.14 |
| Non-White | 5 (8.3) | 4 (6.7) | 51 (85.0) | ||||
| Non-Hispanic White | 1 (2.8) | 3 (8.3) | 32 (88.9) | ||||
| Glucose/A1C | Overall | 11 (11.2) | 21 (21.4) | 66 (67.3) | 888.5 | 0.17 | 0.14 |
| Non-White | 7 (11.9) | 15 (25.4) | 37 (62.7) | ||||
| Non-Hispanic White | 3 (8.6) | 5 (14.3) | 27 (77.1) | ||||
| Total cholesterol | Overall | 1 (1.3) | 1 (1.3) | 76 (97.4) | 572.0 | 0.36 | 0.10 |
| Non-White | 1 (1.9) | 1 (1.9) | 52 (96.2) | ||||
| Non-Hispanic White | 0 (0) | 0 (0) | 22 (100) | ||||
Italics denote significant values
Fig. 1.
a Percentage of participants in each LS7 diet category by race/ethnicity. b Percentage of participants in each LS7 blood pressure category by race/ethnicity
Discussion
Results showed variability among LS-7 measures. Surprisingly, most participants had ideal levels for cholesterol, glucose, and exercise. However, since exercise was self-reported, exercise could have been over-reported. Consistent with previous literature [7], 78% of our participants were current smokers and thus were in the poor category for smoking. BMI categories were somewhat evenly distributed, and most participants reported dietary patterns in the intermediate category. The majority of people had poor or intermediate levels for blood pressure. This data suggests that smoking, BMI, diet, and blood pressure could be significant factors to target for prevention of CVD among men with a history of incarceration in supervised community settings.
Non-Whites were more likely than Whites to fall into the poor category for both diet and blood pressure. This is consistent with research that has found African-American men are less likely to engage in primary medical care, receive preventive health services, or meet goal levels for evidence-based lifestyle modifications (e.g., the Dietary Approaches to Stop Hypertension (DASH) diet, sodium reduction, and physical activity) compared to Whites [28–33]. This also supports data from the Jackson Heart Study which demonstrated that most community dwelling African-American men without hypertension or cardiovascular disease did not have an ideal diet or ideal blood pressure as measured by LS-7 measures. However, this study did not assess the incarceration history of these participants [34]. Additionally, non-White participants in our sample were found to have significantly lower total LS-7 scores than Whites, indicating they have worse scores across all seven or a few of the LS-7 measures. This indicates that they may be at greater risk for CVD than White men with a history of incarceration.
To our knowledge, this is the first study to evaluate cardiovascular health among individuals with a history of incarceration using the LS-7 metric, which included objective measures for four of the seven LS-7 metrics (blood pressure, lipids, glucose, and BMI). Our results provide a foundation for future preventive interventions for this underserved population. Specifically, smoking, BMI, diet, and blood pressure emerged as significant factors to target for CVD prevention among previously incarcerated men. Additionally, minorities had a higher prevalence of poor diet and high blood pressure, suggesting the importance of targeting these factors in this population to address disparities in cardiovascular health. Future research should assess the impact of preventive measures and treatments for CVD among men with incarceration history in community corrections and transitional housing programs.
Our study has a few limitations. The LS-7 measure has demonstrated a relationship with CVD and mortality, but like other national surveys widely used in public health research, relies on self-report data for diet, exercise, and smoking, which limits the accuracy of these data and the conclusions drawn by the investigators [21, 22]. Our sample only included two Hispanics and two Native Americans. Therefore, the results may not generalize to these races/ethnicities. We did not include women for this study because one of our recruitment sites only provided transitional housing to male clients, thereby limiting our ability to recruit an adequate number of women for gender stratified analyses and due to known gender differences in CVD risk. However, women represent an increasing proportion of incarcerated individuals and CVD is a prominent cause of morbidity and mortality; thus, future research should explore the potential for reducing CVD risk among women with incarceration history. Lastly, we did not collect data on demographically matched (e.g., age, race/ethnicity, and/or socioeconomic status) men without incarceration history. Thus, it remains unclear how much incarceration history may be a mediator or moderator of cardiovascular health and CVD disparities.
Nonetheless, community corrections and transitional housing settings have a significant concentration of individuals, particularly minorities and low-income individuals who have disproportionate rates of incarceration and CVD risk factors. Therefore, these may be unique settings for deploying evidence-based CVD risk reduction interventions. This is consistent with recent recommendations to understand how transition from the criminal justice system to the community may impact CVD risk and cardiovascular health disparities and evaluate the effect of community-based CVD prevention and reduction strategies for recently released populations [15].
Acknowledgements
We are grateful for the support of the staff at TASC (Sharron Rowser, Program Administrator; John Dantzler, Ph.D.; and the counseling staff) and The Foundry (Micah Andrews, Chief Executive Officer; Brandon Lackey, Chief Program Officer; Mike Farrell, Reentry Director), and the research administration support of Jessica Oliver, M.Ed.
Funding
Funding for this study was provided by the University of Alabama at Birmingham School of Public Health 2015 Community Health Scholars pilot grant program.
Compliance with Ethical Standards
Disclosures
Dr. Redmond is a board member of the nonprofit organization Physicians for Criminal Justice Reform, from which she receives no financial support; she initiated this study as an employee of the University of Alabama at Birmingham; and contributed to this article as an employee of the National Heart Lung and Blood Institute (NHLBI). Any opinions, findings, and conclusions or recommendations expressed in this paper are those of the authors and do not necessarily reflect the views of the NHLBI, National Institutes of Health (NIH), or Department of Health and Human Services (DHHS). The remaining authors report no other disclosures.
References
- 1.Kaeble D, Bonczar TP. Probation and parole in the United States. Bur Justice Stat Spec Rep. 2015;2016:1–26. [Google Scholar]
- 2.Travis J, Solomon AL, Waul M. From prison to home: the dimensions and consequences of prisoner reentry. 2001.
- 3.Porter LC. Incarceration and post-release health behavior. J Health Soc Behav. 2014;55(2):234–249. doi: 10.1177/0022146514531438. [DOI] [PubMed] [Google Scholar]
- 4.Binswanger I, Stern M, Deyo R, et al. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cropsey K, Eldridge GD, Ladner T. Smoking among female prisoners: an ignored public health epidemic. Addict Behav. 2004;29(2):425–431. doi: 10.1016/j.addbeh.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Wang E, Pletcher M, Vittinghoff E, Kertesz S, Kiefe C, Bibbins-Domingo K. Incarceration, incident hypertension, and access to healthcare: findings from the coronary artery risk development in young adults (CARDIA) study. Arch Intern Med. 2009;169(7):687–693. doi: 10.1001/archinternmed.2009.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cropsey KL, Jones-Whaley S, Jackson DO, Hale GJ. Smoking characteristics of community corrections clients. Nicotine Tob Res. 2010;12(1):53–58. doi: 10.1093/ntr/ntp172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donahue J. Coronary artery disease in offender populations: incarceration as a risk factor and a point of intervention. J Correct Health Care. 2014;20(4):302–312. doi: 10.1177/1078345814541534. [DOI] [PubMed] [Google Scholar]
- 9.Cropsey KL, Clark CB, Zhang, Hendricks PS, Jardin BF, Lahti AC. Race and medication adherence moderate cessation outcomes in criminal justice smokers. Am J Prev Med. 2015;49(3):335–344. doi: 10.1016/j.amepre.2015.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conklin T, Lincoln T, Flanigan T. A public health model to connect correctional health care with communities. Am J Public Health. 1998;88(8):1249–1250. [PubMed] [Google Scholar]
- 11.Golembeski C, Fullilove R. Criminal (in)justice in the city and its associated health consequences. Am J Public Health. 2005;95(10):1701–1706. doi: 10.2105/AJPH.2005.063768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iguchi MY, Bell J, Ramchand RN, Fain T. How criminal system racial disparities may translate into health disparities. J Health Care Poor Underserved. 2005;16(4 Suppl B):48–56. doi: 10.1353/hpu.2005.0081. [DOI] [PubMed] [Google Scholar]
- 13.Freudenberg N, Moseley J, Labriola M, Daniels J, Murrill C. Comparison of health and social characteristics of people leaving New York City jails by age, gender, and race/ethnicity: implications for public health interventions. Public Health Rep. 2007;122(6):733–743. doi: 10.1177/003335490712200605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang EA, Wildeman C. Studying health disparities by including incarcerated and formerly incarcerated individuals. JAMA. 2011;305(16):1708–1709. doi: 10.1001/jama.2011.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang EA, Redmond N, Dennison Himmelfarb CR, Pettit B, Stern M, Chen J, Shero S, Iturriaga E, Sorlie P, Diez Roux AV. Cardiovascular disease in incarcerated populations. J Am Coll Cardiol. 2017;69(24):2967–2976. doi: 10.1016/j.jacc.2017.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Connor T. MegaLinks in criminal justice. Rocky Mount: North Carolina Wesleyan College; 1999.
- 17.Freudenberg N. Jails, prisons, and the health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78(2):214–235. doi: 10.1093/jurban/78.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health. 2005;95(10):1725–1736. doi: 10.2105/AJPH.2004.056325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lincoln T, Kennedy S, Tuthill R, Roberts C, Conklin TJ, Hammett TM. Facilitators and barriers to continuing healthcare after jail: a community-integrated program. J Ambul Care Manag. 2006;29(1):2–16. doi: 10.1097/00004479-200601000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD, on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee Defining and setting national goals for cardiovascular health promotion and disease reduction. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 21.Cushman M, Judd SE, Howard VJ, et al. Abstract MP35: the American Heart Association’s Life’s Simple 7 and Mortality by Race and Sex in the U.S.: the REasons for Geographic And Racial Differences in Stroke (REGARDS) Cohort. Circulation. 2014;129(Suppl 1):AMP35. [Google Scholar]
- 22.Kulshreshtha A, Vaccarino V, Judd SE, Howard VJ, McClellan WM, Muntner P, Hong Y, Safford MM, Goyal A, Cushman M. Life’s simple 7 and risk of incident stroke. Stroke. 2013;44(7):1909–1914. doi: 10.1161/STROKEAHA.111.000352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hartney C, Vuong L. Created equal: racial and ethnic disparities in the US criminal justice system. Oakland: National Council on Crime and Delinquency; 2009.
- 24.Polonsky TS, Ning H, Daviglus ML, et al. Association of cardiovascular health with subclinical disease and incident events: the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2017;6(3). [DOI] [PMC free article] [PubMed]
- 25.Dong C, Rundek T, Wright CB, Anwar Z, Elkind MSV, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics. Circulation. 2012;125(24):2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilper AP, Woolhandler S, Boyd JW, Lasser KE, McCormick D, Bor DH, Himmelstein DU. The health and health care of US prisoners: results of a nationwide survey. Am J Public Health. 2009;99:666–672. doi: 10.2105/AJPH.2008.144279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maruschak LM, Glaze L, Carson EA, Noonan M. BJS's efforts to measure health and health care in corrections. Fifth Annual Academic and Health Policy Conference in on Correctional Health. Atlanta, Georgia; 2012.
- 28.Rich JA. Primary care for young African American men. J Am Coll Heal. 2001;49(4):183–186. doi: 10.1080/07448480109596301. [DOI] [PubMed] [Google Scholar]
- 29.Ravenell JE, Whitaker EE, Johnson WE., Jr According to him: barriers to healthcare among African-American men. J Natl Med Assoc. 2008;100(10):1153–1160. doi: 10.1016/S0027-9684(15)31479-6. [DOI] [PubMed] [Google Scholar]
- 30.Satcher D. Overlooked and underserved: improving the health of men of color. Am J Public Health. 2008;98(9 Suppl):S139–S141. doi: 10.2105/AJPH.98.Supplement_1.S139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gao SK, Fitzpatrick AL, Psaty B, Jiang R, Post W, Cutler J, Maciejewski ML. Suboptimal nutritional intake for hypertension control in 4 ethnic groups. Arch Intern Med. 2009;169(7):702–707. doi: 10.1001/archinternmed.2009.17. [DOI] [PubMed] [Google Scholar]
- 32.Scisney-Matlock M, Bosworth HB, Giger JN, Strickland OL, Harrison RV, Coverson D, Shah NR, Dennison CR, Dunbar-Jacob JM, Jones L, Ogedegbe G, Batts-Turner ML, Jamerson KA. Strategies for implementing and sustaining therapeutic lifestyle changes as part of hypertension management in African Americans. Postgrad Med. 2009;121(3):147–159. doi: 10.3810/pgm.2009.05.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hammond WP, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, medical \mistrust, and preventive health services delays among community-dwelling African-American men. J Gen Intern Med. 2010;25(12):1300–1308. doi: 10.1007/s11606-010-1481-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Booth JN, 3rd, Abdalla M, Tanner RM, et al. Cardiovascular health and incident hypertension in blacks: JHS (the Jackson heart study) Hypertension. 2017;70(2):285–292. doi: 10.1161/HYPERTENSIONAHA.117.09278. [DOI] [PMC free article] [PubMed] [Google Scholar]