Abstract
Objective
To explore variation in acute care use of inpatient (IRF) and skilled nursing (SNF) rehabilitation following ischemic and hemorrhagic stroke.
Design
A secondary analysis of Medicare claims data linked to IRF and SNF assessment files (2013–2014).
Results
The sample included 122,084 stroke patients discharged to IRF or SNF from 3,677 acute hospitals. Of the acute hospitals, 3,649 discharged patients with an ischemic stroke (range 1–402 patients/hospital, median=15) compared to 1,832 acute hospitals that discharged patients with hemorrhagic events (range 1–73 patients/hospital, median=4). The intraclass correlation (ICC) examined variation in discharge settings attributed to acute hospitals (Ischemic ICC=0.318, Hemorrhagic ICC=0.176). Patients >85 years and those with greater numbers of comorbid conditions were more likely to discharge to SNF. Comparison of self-care and mobility across stroke type suggests that patients with ischemic stroke have higher functional abilities at admission.
Conclusion
This study suggests demographic and clinical differences among stroke patients admitted for post-acute rehabilitation at IRF and SNF settings. Furthermore, examination of variation in ischemic and hemorrhagic stroke discharges suggests acute facility level differences and indicates a need for careful consideration of patient and facility factors when comparing the effectiveness of IRF and SNF rehabilitation.
Keywords: Stroke, Inpatient Rehabilitation Facilities, Skilled Nursing Facilities, Rehabilitation
Introduction
Stroke is a leading cause of long-term disability in the United States (US), with over 795,000 strokes occurring each year.1 In terms of resources use, stroke costs $34 billion dollars a year in medical costs and loss of productivity.2 While there is a sharp decline in mortality rate following stroke, rate of long-term residual impairments, disabilities and risk for developing high rates of secondary conditions remains high.2 Cumulatively these result in a high need for rehabilitation services within acute and post-acute care (PAC). The two most common inpatient PAC settings for stroke rehabilitation are inpatient rehabilitation facilities (IRF) and skilled nursing facilities (SNF). Accredited IRFs provide 3 or more hours of intensive therapy 5 days a week. SNFs provide extended care and rehabilitation to persons who cannot tolerate 3 hours of intensive therapy per day. The amount of therapy is based on the resident’s SNF Resource Utilization Group and their health status.3
A study using Medicare data to examine community re-entry across PAC settings found that SNF use increased institutionalization, suggesting that patients were better off going to IRF when acute facilities had choice between placements.4 However, it is unclear if there is variation in the use of IRF and SNF rehabilitation across types of stroke. In addition, a national study of hospitals participating in the American Heart Association Get with the Guidelines Stroke Program found considerable hospital variation in functional status at three months for ischemic stroke based on decisions made at discharge, indicating the importance of the acute care decision making processes on long-term outcomes.5 In a study of transitions for patients with ischemic stroke from less to more intensive levels of care, Kind et al. (2010) found variation in PAC use across racial and ethnic groups. They suggest complications in transitions may be attributable to client choice and cultural differences in patient and family approaches to end of life.6 These studies support the need for research examining acute hospital discharges to PAC.
Recent healthcare policy and demonstration projects target the connection between the acute care hospital and PAC and likely influence the decisions about who receives rehabilitation for which type of setting. The Bundled Payment for Care Improvement Initiative (BPCI) connects acute and PAC rehabilitation for an episode of care,7 which has been shown to reduce the use of institutional PAC.8 The Affordable Care Act (ACA) established Accountable Care Organizations (ACO) which connect groups of doctors, hospitals, and PAC.9 ACO’s have resulted in spending decreases mostly due to reductions in acute discharges and PAC lengths of stay.10 These policies are designed to integrate healthcare, including PAC rehabilitation, to improve coordination across the transition of care from acute setting to PAC rehabilitation (IRF and SNF). In a study of PAC, Graham et al. (2017) found greater continuity for hospitals with affiliated rehabilitation units.11 Arguably the presence of these policies impact acute care discharge decisions related to PAC.
Even with these policy and research efforts, much remains unknown about what influences acute care hospital use of inpatient rehabilitation services. Discharge to PAC rehabilitation is highly variable and depends on a variety of clinical and non-clinical factors.5,12–14 Although clinical characteristics, including condition severity, comorbidities, and functional abilities influence discharge to PAC, other non-clinical factors like distance and geography also contribute to acute care discharge decisions.4,5,14
Medicare requirements and payment policies include the need and tolerance for 3 hours of interdisciplinary rehabilitation in IRF settings.15,16 In a discussion of rehabilitation placement following stroke, Dobkin (2005) presented an algorithm that included the three hour tolerance along with other clinical and environmental factors.17 Additionally, even though the majority of studies comparing IRF and SNF outcomes for stroke suggest that IRF patients experience more functional gains,4,18 other studies suggest that these gains may be attributable to patient factors like age, race, ethnicity, and disability severity.19,20 In the end, decisions are often driven by who is expected to benefit most from which type of PAC setting.4 The success of patients with stroke in PAC depends in part on the decisions made by the acute care team.21
Given the many factors that influence admission to inpatient PAC stroke rehabilitation and the recent healthcare policies and programs that influence current discharge decisions, we sought to examine the discharge patterns from acute care hospitals to inpatient rehabilitation facilities and skilled nursing facilities for those with ischemic and hemorrhagic stroke. The purpose of our study was twofold: (1) to examine variation in the use of IRF and SNF rehabilitation for those with ischemic and hemorrhagic stroke attributed to acute hospitals (number and likelihood of being discharged, amount of variation), and (2) to examine patient and clinical characteristics for patients with ischemic and hemorrhagic stroke admitted for IRF and SNF stroke rehabilitation.
Methods
Study data
We combined four Medicare data files (FY 2013–2014) to construct an analytical study file, including 1) Master Beneficiary Summary File for beneficiary enrollment information, 2) Medicare Provider Analysis and Review (MedPAR) for use of hospital inpatient services, 3) Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF-PAI) for function score in IRF, and 4) Minimum Dataset 3.0 (MDS) for function scores in SNF. Additionally, we merged a ZIP Code Tabulation Area (ZCTA) Distance database (http://www.nber.org/data/zip-code-distance-database.html) with Medicare data files to measure the distance patients traveled from acute hospitals to PAC setting.4 The study was approved by the Institutional Review Board the University of Texas Medical Branch and complies with Centers for Medicare and Medicaid Services (CMS) Data Use Agreement. Consent was not required due to the use of administrative data. This study conforms to all STROBE guidelines and reports the required information accordingly (see Supplementary Checklist).
Sample
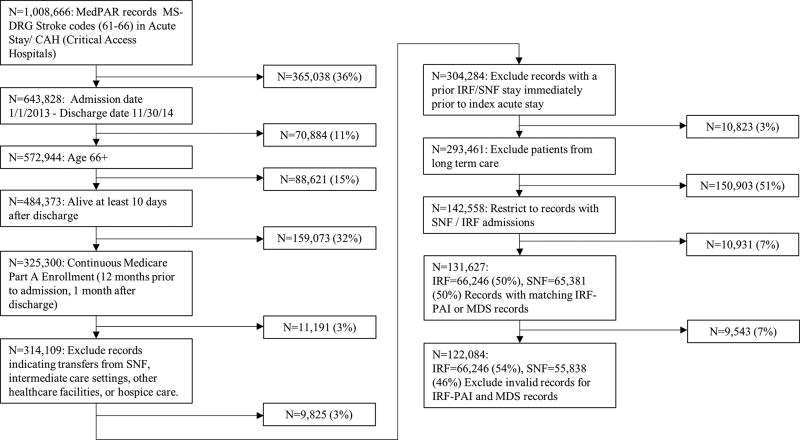
Our sample of interest was Medicare beneficiaries discharged to IRF or SNF following acute hospitalization for stroke. The study sample included patients with the diagnoses of stroke based on Medicare Severity Diagnosis Related Groups (MS-DRG) codes 061–066.22 We stratified the sample into ischemic stroke (MS-DRG 061–063) and hemorrhagic stroke (MS-DRG 064–066) for analysis because hemorrhagic stroke has different outcomes (i.e., low functional scores and longer length of stay) than ischemic stroke.7 Additional inclusion criteria included 1). discharged from IRF or SNF from January 1, 2013 through December 30, 2014, 2). age 66 years or older at admission to the acute hospital, 3). patient must be alive at least 10 days after hospital discharge, 4). continuous enrollment 12 months prior to admission, 10 days after discharge in Medicare Part A, and 5). living in a community setting prior to index acute hospitalization. A total of 122,084 Medicare beneficiaries with a stroke diagnosis discharged from acute hospitals to IRF and SNF between January 2013 and December 2014. Figure 1 depicts the study flow diagram for the sample.
Figure 1.
Study flow diagram for the sample.
Variables
Patient characteristics included age at admission to IRFs or SNFs (categories: 65–69, 70–74, 75–79, 80–84, ≥85 years), sex (male, female), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other), length of stay in acute care (categories: 0–3, 4–7, 8–11, 12–25, ≥26 days), Medicaid eligibility (yes, no) which was a proxy for socioeconomic status,23 and stays in intensive care unit/coronary care unit (yes, no) which was a measure of stroke severity.24 We used CMS Hierarchical Condition Categories (HCC) for comorbidities. While the primary purpose of HCC is for adjusting risk in the Medicare Advantage payment plans, it can also be used to risk adjust patient-level health conditions.25 Among the 79 categories, we used the 30 most frequent HCC codes (yes, no) among the sample in the analysis.
In order to better capture stroke severity, we used functional status contained in CMS assessment files for IRF and SNF: IRF-PAI, and the MDS 3.0 respectively. We used Mallinson and colleagues (2012) crosswalk for IRF-PAI and MDS assessments to construct comparable admission functional scores between these two PAC settings.26 The co-calibrated crosswalk contains the domains of mobility and self-care and was developed using a Rasch common-person equating method.26,27 This measurement method has demonstrated efficacy for equating different ADL instruments.26,27 To meet requirements for this assumption, we subsequently excluded 9,543 SNF patients (14.5%) whose MDS records were inconsistent. For example if a record classified the individual transfer capacity as “independent” (MDS 3.0 G0110, Transfer: Self Performance = 0) while at the same time denoting the amount of support given for transfers (MDS 3.0, Transfer Support = 3) classified as “More than two persons physical assistance.” In our study we reported the co-calibrated admission functional status for self-care and mobility domains for both IRF and SNF on a 0–100 point scale using the crosswalk, where higher scores indicate greater functional status.
Statistical analysis
We conducted univariate analyses to determine the top 30 comorbidities to examine differences between the patients admitted to IRFs and SNFs. We investigated the amount of variation in discharges to IRF versus SNF attributed to the acute hospitals by stroke type (all stroke, ischemic, hemorrhagic) with intraclass correlation coefficients (ICC) estimated from hierarchical generalized linear mixed (HGLM) model. ICC is estimated by a ratio of group-level error variance over the total error variance which indicates the proportion of explained variance attributable to the grouping structure (e.g., acute hospital) in a hierarchical model.28 The HGLM models were further used to predict the likelihood (odds ratio and 95% confidence intervals) of IRF versus SNF discharge (dependent variable) adjusting for the random effect of acute hospitals.29 We used two multilevel models to examine the effect of patient and facility level characteristics (independent variables), including age, sex, race, top 30 HCCs, length of stay in acute care, Medicaid eligibility, function scores, distance from acute hospital to PAC setting, and the number of stroke discharges from the acute hospital. All analyses and data management were performed with SAS statistical software version 9.4.a
Results
Table 1 presents the demographic characteristics of the study sample across post-acute facilities and stroke type. Across the sample, 88.6% (n=108,128) of patients had an ischemic stroke. Of those 54.6% (n=59,027) were discharged to IRFs. For those with a hemorrhagic event (n=13,956) 51.7% were discharged to IRF. Patients with hemorrhagic stroke stayed in the intensive care unit (ICU) longer than those with ischemic stroke (Hemorrhagic: mean=6.7 days; Ischemic: mean=5.1 days). Likewise patients discharged to SNF had longer acute care lengths of stay for ischemic stroke (5.9 days) and hemorrhagic stroke (7.6 days) than those who discharged to IRF (4.5 and 5.9 days). Patients with ischemic stroke had a higher percentage of Medicaid eligibility than those with hemorrhagic stroke regardless of PAC settings (IRF: 17.4% vs. 14.6%, SNF: 24.4% vs. 23.0%, respectively). In contrast, patients with hemorrhagic stroke received more care in an intensive care unit during their acute care stay. Regardless of stroke type, patients discharged to SNF had lower self-care (IRF: 44.6, SNF: 41.6) and mobility (IRF: 44.2, SNF: 40.6) functional scores at the time of admission and shorter distances to acute hospitals (IRF: 20.2 miles, SNF: 18.2 miles). Table 2 presents the most frequent comorbid conditions (HCC) across stroke type and post-acute rehabilitation facilities. The patients with stroke who discharged to SNF had a higher percentage of conditions compared to those discharged to IRF.
Table 1.
Demographics across stroke type, inpatient rehabilitation facilities (IRFs) and skilled nursing facilities (SNFs)
| All Stroke | Ischemic Stroke | Hemorrhagic Stoke | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| (N=122,084) | N=108,128 (88.6%) | N=13,956 (11.4%) | ||||
|
| ||||||
| Variable | IRF (N=66246) | SNF (N=55838) | IRF (N=59027) | SNF (N=49101) | IRF (N=7219) | SNF (N=6737) |
| Age | ||||||
| 65–69 | 7982 (12.05%) | 3258 (5.83%) | 7136 (12.09%) | 2894 (5.89%) | 846 (11.72%) | 364 (5.40%) |
| 70–74 | 12028 (18.16%) | 5793 (10.37%) | 10669 (18.07%) | 5071 (10.33%) | 1359 (18.83%) | 722 (10.72%) |
| 75–79 | 13461 (20.32%) | 8463 (15.16%) | 11829 (20.04%) | 7310 (14.89%) | 1632 (22.61%) | 1153 (17.11%) |
| 80–84 | 13962 (21.08%) | 11722 (20.99%) | 12369 (20.95%) | 10178 (20.73%) | 1593 (22.07%) | 1544 (22.92%) |
| 85+ | 18813 (28.40%) | 26608 (47.64%) | 17024 (28.84%) | 23648 (48.16%) | 1789 (24.78%) | 2954 (43.85%) |
| Sex | ||||||
| Male | 29690 (44.82%) | 20020 (35.85%) | 26132 (44.27%) | 17371 (35.38%) | 3558 (49.29%) | 2649 (39.32%) |
| Female | 36556 (55.18%) | 35818 (64.15%) | 32895 (55.73%) | 31730 (64.62%) | 3661 (50.71%) | 4088 (60.68%) |
| Race | ||||||
| Non-Hispanic White | 54632 (82.47%) | 46474 (83.23%) | 48607 (82.35%) | 40914 (83.33%) | 6025 (83.46%) | 5560 (82.53%) |
| Non-Hispanic Black | 7763 (11.72%) | 6400 (11.46%) | 7093 (12.02%) | 5737 (11.68%) | 670 (9.28%) | 663 (9.84%) |
| Hispanic | 1031(1.56%) | 868 (1.55%) | 903 (1.53%) | 723 (1.47%) | 128 (1.77%) | 145 (2.15%) |
| Other race | 2820 (4.26%) | 2096 (3.75%) | 2424 (4.11%) | 1727 (3.52%) | 396 (5.49%) | 369 (5.48%) |
| Length of Stay in Acute Care | ||||||
| 0–3 | 28123 (42.45%) | 16069 (28.78%) | 26402 (44.73%) | 14953 (30.45%) | 1721 (23.84%) | 1116 (16.57%) |
| 4–7 | 30074 (45.40%) | 27009 (48.37%) | 26217 (44.42%) | 23833 (48.54%) | 3857 (53.43%) | 3176 (47.14%) |
| 8–11 | 5859 (8.84%) | 7682 (13.76%) | 4724 (8.00%) | 6314 (12.86%) | 1135 (15.72%) | 1368 (20.31%) |
| 12–25 | 2099 (3.12%) | 4650 (8.33%) | 1622 (2.75%) | 3672 (7.48%) | 477 (6.61%) | 978 (14.52%) |
| 26+ | 91 (0.14%) | 428 (0.77%) | 62 (0.11%) | 329 (0.67%) | 29 (0.40%) | 99 (1.47%) |
| Mean (SD) | 4.6 (3.0) | 6.1 (4.6) | 4.5 (2.9) | 5.9 (4.5) | 5.9 (3.7) | 7.6 (5.4) |
| Medicaid Eligibility (Yes vs No) | 11355 (17.14%) | 13545 (24.26%) | 10297 (17.44%) | 11990 (24.42%) | 1058 (14.66%) | 1555 (23.08) |
| Stay in ICU/CCU (Yes vs No) | 32082 (48.43%) | 23366 (41.85%) | 26150 (44.30%) | 18553 (37.79%) | 5932 (82.17%) | 4813 (71.44%) |
| Number of Stroke Discharges from Acute Hospitals, Mean (SD) | 98.8 (69.2) | 83.6 (69.5) | 96.2 (68.8) | 80.7 (68.6) | 119.7 (68.9) | 105.0 (72.6) |
| Distance from Acute Hospital to PAC setting (Miles), Mean (SD)† | 20.2 (44.3) | 18.2 (42.2) | 19.5 (43.7) | 17.4 (41.7) | 26.2 (48.8) | 24.2 (45.6) |
| Admission Function Score | ||||||
| a Self-Care, Mean (SD) | 44.6 (11.3) | 41.6 (12.2) | 44.8 (11.3) | 41.9 (12.2) | 43.1 (12.1) | 39.8 (12.3) |
| b Mobility, Mean (SD) | 44.2 (7.4) | 40.6 (9.7) | 44.3 (7.4) | 40.9 (9.7) | 43.3 (7.7) | 39.4 (9.6) |
Note.
Admission function scores for Self-Care and Mobility were scaled on 0–100 point scales.
, FIM = Eating + Grooming + Bathing + Dressing_Upper + Dressing_Lower + Toileting
MDS = Dressing + Eating + Toilet use + Personal hygiene + Bathing
, FIM = Transfer (Bed, Chair, Wheelchair) + Transfer (Toilet) + Transfer (Tub, Shower) + Locomotion (Walk/Wheelchair) + Locomotion (Stairs)
MDS = Bed mobility + Transfer + Walk in room + Walk in corridor + Locomotion on unit + Locomotion off unit
, Distances between acute hospital and PAC setting using Zip Code centroids and ZIP Code Tabulation Area (ZCTA) Distance Database
Table 2.
Comorbidities across stroke type, inpatient rehabilitation facilities (IRFs) and skilled nursing facilities (SNFs)
| All Stroke | Ischemic Stroke | Hemorrhagic Stoke | ||||
|---|---|---|---|---|---|---|
| (N=122,084) | N=108,128 (88.6%) | N=13,956 (11.4%) | ||||
| Comorbidities | IRF (N=66246) | SNF (N=55838) | IRF (N=59027) | SNF (N=49101) | IRF (N=7219) | SNF (N=6737) |
| Specified Heart Arrhythmias | 7291 (11.01%) | 8149 (14.59%) | 6503 (11.02%) | 7206 (14.68%) | 788 (10.92%) | 943 (14.00%) |
| Congestive Heart Failure | 6082 (9.18%) | 7079 (12.68%) | 5548 (9.40%) | 6377 (12.99%) | 534 (7.40%) | 702 (10.42%) |
| Diabetes without Complication | 6464 (9.76%) | 6256 (12.20%) | 5874 (9.95%) | 5582 (11.37%) | 590 (8.17%) | 674 (10.00%) |
| Chronic Obstructive Pulmonary Disease | 3945 (5.96%) | 4256 (7.62%) | 3555 (6.02%) | 3766 (7.67%) | 390 (5.40%) | 490 (7.27%) |
| Acute Renal Failure | 3517 (5.31%) | 3909 (7.00%) | 3144 (5.33%) | 3463 (7.05%) | 375 (5.17%) | 446 (6.62%) |
| Vascular Disease | 3146 (4.75%) | 3154 (5.65%) | 2863 (4.85%) | 2808 (5.72%) | 283 (3.92%) | 346 (5.14%) |
| Hemiplegia/Hemiparesis | 2788 (4.21%) | 2681 (4.80%) | 2555 (4.33%) | 2392 (4.87%) | 233 (3.23%) | 289 (4.29%) |
| Diabetes with Chronic Complications | 2018 (3.05%) | 1817 (3.25%) | 1850 (3.13%) | 1626 (3.31%) | 168 (2.33%) | 191 (2.84%) |
| Cardio-Respiratory Failure and Shock | 1433 (2.16%) | 1629 (2.92%) | 1273 (2.16%) | 1411 (2.87%) | 160 (2.22%) | 218 (3.24%) |
| Coagulation Defects and Other Specified Hematological Disorders | 1459 (2.20%) | 1468 (2.63%) | 1274 (2.16%) | 1245 (2.54%) | 185 (2.56%) | 223 (3.31%) |
| Septicemia, Sepsis, Systemic Inflammatory Response Syndrome/Shock | 1123 (1.70%) | 1404 (2.51%) | 993 (1.68%) | 1201 (2.45%) | 130 (1.80%) | 203 (3.01%) |
| Protein-Calorie Malnutrition | 979 (1.48%) | 1227 (2.20%) | 884 (1.50%) | 1043 (2.12%) | 95 (1.32%) | 184 (2.73%) |
| Seizure Disorders and Convulsions | 953 (1.44%) | 1242 (2.22%) | 811 (1.37%) | 1024 (2.09%) | 142 (1.97%) | 218 (3.24%) |
| Ischemic or Unspecified Stroke | 999 (1.51%) | 1184 (2.12%) | 932 (1.58%) | 1086 (2.21%) | 67 (0.93%) | 98 (1.45%) |
| Rheumatoid Arthritis and Inflammatory Connective Tissue Disease | 993 (1.50%) | 1022 (1.83%) | 907 (1.54%) | 910 (1.85%) | 86 (1.19%) | 112 (1.66%) |
| Morbid Obesity | 976 (1.47%) | 902 (1.62%) | 883 (1.50%) | 808 (1.65%) | 93 (1.29%) | 94 (1.40%) |
| Unstable Angina and Other Acute Ischemic Heart Disease | 650 (0.98%) | 690 (1.24%) | 585 (0.99%) | 613 (1.25%) | 65 (0.90%) | 77 (1.14%) |
| Other Significant Endocrine and Metabolic Disorders | 606 (0.91%) | 627 (1.12%) | 509 (0.86%) | 508 (1.03%) | 97 (1.34%) | 119 (1.77%) |
| Parkinson's and Huntington's Diseases | 497 (0.75%) | 636 (1.14%) | 458 (0.78%) | 548 (1.12%) | 39 (0.54%) | 88 (1.31%) |
| Major Depressive, Bipolar, and Paranoid Disorders | 422 (0.64%) | 594 (1.06%) | 385 (0.65%) | 513 (1.04%) | 37 (0.51%) | 81(1.20%) |
| Intestinal Obstruction/Perforation | 452 (0.68%) | 494 (0.88%) | 386 (0.65%) | 445 (0.91%) | 66 (0.91%) | 49 (0.73%) |
| Breast, Prostate, and Other Cancers and Tumors | 409 (0.62%) | 474 (0.85%) | 362 (0.61%) | 412 (0.84%) | 47 (0.65%) | 62 (0.92%) |
| Acute Myocardial Infarction | 413 (0.62%) | 449 (0.80%) | 375 (0.64%) | 396 (0.81%) | 38 (0.53%) | 53 (0.79%) |
| Cerebral Hemorrhage | 375 (0.57%) | 483 (0.87%) | 251 (0.43%) | 298 (0.61%) | 124 (1.72%) | 185 (2.75%) |
| Aspiration and Specified Bacterial Pneumonias | 330 (0.50%) | 411 (0.74%) | 287 (0.49%) | 344 (0.70%) | 43 (0.60%) | 67 (0.99%) |
| Vascular Disease with Complications | 362 (0.55%) | 401 (0.72%) | 300 (0.51%) | 358 (0.73%) | 62 (0.86%) | 43 (0.64%) |
| Chronic Ulcer of Skin, Except Pressure | 323 (0.49%) | 408 (0.73%) | 298 (0.50%) | 351 (0.71%) | 25 (0.35%) | 57 (0.85%) |
| Metastatic Cancer and Acute Leukemia | 358 (0.54%) | 349 (0.63%) | 299 (0.51%) | 282 (0.57%) | 59 (0.82%) | 67 (0.99%) |
| Coma, Brain Compression/Anoxic Damage | 353 (0.53%) | 351 (0.63%) | 232 (0.39%) | 200 (0.41%) | 121 (1.68%) | 151 (2.24%) |
| Artificial Openings for Feeding or Elimination | 329 (0.50%) | 332 (0.59%) | 291 (0.49%) | 277 (0.56%) | 38 (0.53%) | 55 (0.82%) |
Note.
, Chi-square test;
, significance at a α value of less than 0.05
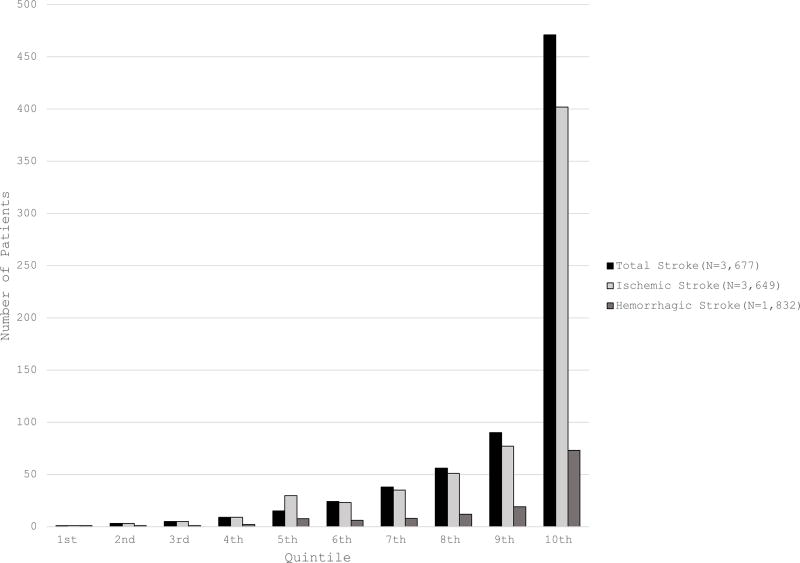
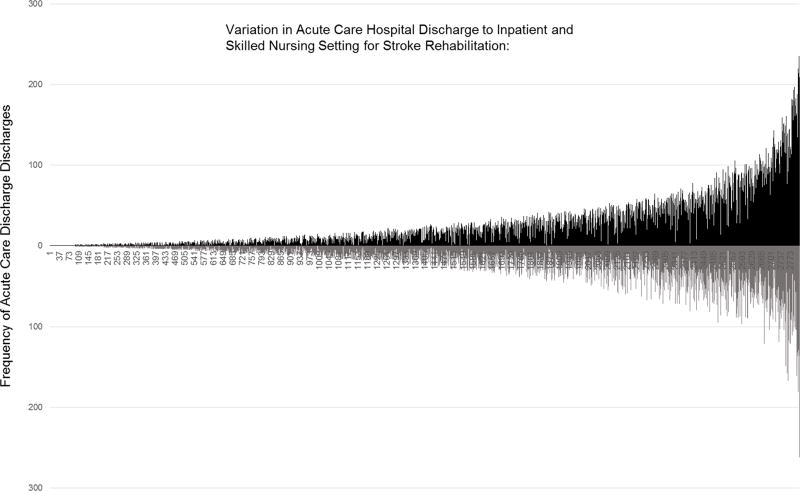
Across the 3,677 acute care hospitals there were differences in the amount of stroke patients discharged to IRF and SNF settings (range: 1 to 471) (Figure 2). There was also variation by stroke type with 3,649 acute care hospitals discharging patients with an ischemic event (range 1–402, median=15, interquartile range (IR) = 5–35). In contrast, only 1,832 acute care hospitals discharged patients with a hemorrhagic event (range 1 to 73 patients, median=4, IR = 1–8). Figure 3 shows the rank ordered distribution of IRF and SNF discharges by the frequency of acute care hospital discharges. Each line represents one acute care hospital with the black line denoting the frequency of IRF discharges and the grey line reflects the number of SNF. This graph indicates considerable differences in acute care discharges. Across the 3,677 hospitals the number of stroke patients discharged to IRF and SNF rehabilitation ranged from 1 to 471 (mean=15, SD=44.1) with a higher standard deviation for ischemic events (SD=26.4) compared to hemorrhagic stroke (SD=9.7). The graph shows that some acute hospitals utilize IRF and SNF equally while others have a tendency towards IRF or SNF rehabilitation settings.
Figure 2.
Comparison of discharges to inpatient (IRF) and skilled nursing (SNF) rehabilitation from acute care after stroke. Acute care hospitals quintiles by the number of patients (range: 1 – 471) for ischemic (range: 1 – 471) and hemorrhagic (range 1 – 402) stroke.
Figure 3.
The rank ordered distribution of IRF and SNF discharges by the frequency of acute care hospital discharges. Black lines represent the frequency of IRF discharges with grey denoting discharges to a SNF setting.
Table 3 presents HGLM models predicting the likelihood of being discharged from acute care hospitals to IRFs and SNFs across stroke type. Age and female were significantly associated with being discharged to IRFs, regardless of stroke type. Among patients with ischemic stroke, non-Hispanic Black (AOR=1.059, 95% confidence interval [CI]: 1.006–1.115, p=0.0289), Hispanic (AOR=1.283, 95% CI: 1.128–1.459, p=0.0001), and other race (AOR=1.312, 95% CI: 1.204–1.429, p< 0.0001) were significantly associated with being discharged to IRFs compared to non-Hispanic white. For hemorrhagic stroke, however, the odds of being discharged to IRFs were only significant for Hispanic patients (AOR=1.349, 95% CI: 1.003–1.813, p=0.0474). Regardless of stroke type, patients with chronic obstructive pulmonary disease, malnutrition, seizures, Parkinson's, depressions, and vascular disease with complications were significantly associated with being discharged to SNF settings. Conversely, those with an ICU stay during acute care (Ischemic: AOR=1.618, 95% CI: 1.547–1.682, and Hemorrhagic: AOR=2.024, 95% CI: 1.820–2.250, all p<0.0001) and those from higher volume acute hospitals (Ischemic: AOR=1.009, 95% CI: 1.008–1.010, and Hemorrhagic: AOR=1.005, 95% CI: 1.004–1.006, all p<0.0001) were significantly associated with being discharged to IRFs regardless of stroke type. Higher motor scores were significantly associated with discharge to IRF (Ischemic: AOR=1.053, 95% CI: 1.050–1.055 and AOR=1.064, 95% CI: 1.056–1.071, all p<0.001) while those with high self-care scores (Ischemic: AOR=0.981, 95% CI: 0.979–0.983 and Hemorrhagic: AOR=0.980, 95% CI: 0.975–0.985, all p<0.001) and Medicaid beneficiaries (Ischemic: AOR=0.599, 95% CI: 0.576–0.623 and Hemorrhagic: AOR=0.547, 95% CI: 0.490–0.611, all p<0.001) were significantly associated with discharge to SNF. While the distance from acute hospitals to SNF was shorter than the distance to IRF the distance was not significant for IRF discharge (Ischemic: AOR=1.000, 95CI=1.000–1.000, p=0.5224 and Hemorrhagic: AOR=1.000, 95CI=0.999–1.001, p=0.4106). We additionally examined the interactions between ischemic stroke, shorter length of stay and ICU stay which were all significantly related to IRF discharge (Ischemic: AOR=1.067, 95CI=1.028–1.107, p=0.0006; shorter length of stay [0–3 days vs. over 26 days]: AOR=9.186, 95%CI=7.314–11.538, p<0.001; ICU stay: AOR=1.557, 95%CI=1.520–1.595, p<0.001).
Table 3.
Hierarchical generalized linear mixed model predicting the likelihood of being discharged from acute care to inpatient rehabilitation (IRF) compared to skilled nursing (SNF)
| All Stroke | Ischemic Stroke | Hemorrhagic Stroke | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Variables | OR | 95%CI | p | OR | 95%CI | p | OR | 95%CI | p | |||
| Age, years | ||||||||||||
| 65–69 | Ref. | Ref. | Ref. | |||||||||
| 70–74 | 0.825 | 0.776 | 0.877 | <.0001* | 0.827 | 0.775 | 0.883 | <.0001* | 0.827 | 0.692 | 0.987 | 0.0349* |
| 75–79 | 0.617 | 0.582 | 0.655 | <.0001* | 0.630 | 0.592 | 0.671 | <.0001* | 0.569 | 0.481 | 0.674 | <.0001* |
| 80–84 | 0.438 | 0.413 | 0.464 | <.0001* | 0.452 | 0.425 | 0.481 | <.0001* | 0.387 | 0.328 | 0.457 | <.0001* |
| 85+ | 0.238 | 0.225 | 0.251 | <.0001* | 0.243 | 0.229 | 0.258 | <.0001* | 0.217 | 0.184 | 0.256 | <.0001* |
| Female | 0.777 | 0.755 | 0.799 | <.0001* | 0.780 | 0.757 | 0.805 | <.0001* | 0.721 | 0.664 | 0.782 | <.0001* |
| Race | ||||||||||||
| Non-Hispanic White | Ref. | Ref. | Ref. | |||||||||
| Non-Hispanic Black | 1.061 | 1.010 | 1.114 | 0.0179* | 1.059 | 1.006 | 1.115 | 0.0289* | 0.977 | 0.845 | 1.130 | 0.7587 |
| Hispanic/Latino | 1.257 | 1.117 | 1.415 | 0.0002* | 1.283 | 1.128 | 1.459 | 0.0001* | 1.349 | 1.003 | 1.813 | 0.0474* |
| Other race | 1.287 | 1.190 | 1.393 | <.0001* | 1.312 | 1.204 | 1.429 | <.0001* | 1.175 | 0.970 | 1.422 | 0.0984 |
| Length of Stay in Acute Care, days | ||||||||||||
| 0–3 | Ref. | Ref. | Ref. | |||||||||
| 4–7 | 0.603 | 0.584 | 0.623 | <.0001* | 0.602 | 0.582 | 0.622 | <.0001* | 0.680 | 0.610 | 0.758 | <.0001* |
| 8–11 | 0.353 | 0.335 | 0.371 | <.0001* | 0.349 | 0.330 | 0.368 | <.0001* | 0.434 | 0.378 | 0.498 | <.0001* |
| 12–25 | 0.177 | 0.165 | 0.190 | <.0001* | 0.174 | 0.161 | 0.188 | <.0001* | 0.226 | 0.191 | 0.268 | <.0001* |
| 26+ | 0.066 | 0.051 | 0.086 | <.0001* | 0.055 | 0.040 | 0.075 | <.0001* | 0.140 | 0.086 | 0.228 | <.0001* |
| Stay in ICU/CCU (Yes vs No) | 1.549 | 1.496 | 1.604 | <.0001* | 1.618 | 1.557 | 1.682 | <.0001* | 2.024 | 1.820 | 2.250 | <.0001* |
| Comorbidities | ||||||||||||
| Specified Heart Arrhythmias | 0.988 | 0.941 | 1.037 | 0.6262 | 0.975 | 0.926 | 1.026 | 0.3321 | 1.017 | 0.881 | 1.174 | 0.8209 |
| Congestive Heart Failure | 0.923 | 0.874 | 0.974 | 0.0037* | 0.924 | 0.873 | 0.979 | 0.0072* | 0.895 | 0.754 | 1.061 | 0.2016 |
| Diabetes without Complication | 0.889 | 0.847 | 0.934 | <.0001* | 0.883 | 0.838 | 0.930 | <.0001* | 0.904 | 0.778 | 1.052 | 0.1922 |
| Chronic Obstructive Pulmonary Disease | 0.845 | 0.795 | 0.897 | <.0001* | 0.853 | 0.800 | 0.909 | <.0001* | 0.794 | 0.663 | 0.951 | 0.0121* |
| Acute Renal Failure | 0.908 | 0.852 | 0.968 | 0.0029* | 0.898 | 0.839 | 0.961 | 0.0018* | 1.004 | 0.830 | 1.214 | 0.9685 |
| Vascular Disease | 0.960 | 0.899 | 1.025 | 0.2178 | 0.952 | 0.889 | 1.021 | 0.1683 | 1.022 | 0.834 | 1.252 | 0.8353 |
| Hemiplegia/Hemiparesis | 0.951 | 0.886 | 1.022 | 0.1700 | 0.949 | 0.881 | 1.023 | 0.1726 | 0.970 | 0.770 | 1.221 | 0.7937 |
| Diabetes with Chronic Complications | 0.952 | 0.875 | 1.036 | 0.2515 | 0.944 | 0.864 | 1.032 | 0.2026 | 0.947 | 0.725 | 1.236 | 0.6881 |
| Cardio-Respiratory Failure and Shock | 0.982 | 0.893 | 1.080 | 0.7083 | 0.982 | 0.887 | 1.086 | 0.7216 | 0.941 | 0.714 | 1.238 | 0.6629 |
| Coagulation Defects and Other Specified Hematological Disorders | 1.077 | 0.983 | 1.181 | 0.1125 | 1.105 | 1.001 | 1.221 | 0.0485* | 0.975 | 0.763 | 1.245 | 0.8368 |
| Septicemia, Sepsis, Systemic Inflammatory Response Syndrome/Shock | 0.888 | 0.803 | 0.982 | 0.0208* | 0.905 | 0.812 | 1.008 | 0.0697 | 0.805 | 0.608 | 1.067 | 0.1310 |
| Protein-Calorie Malnutrition | 0.845 | 0.760 | 0.939 | 0.0017* | 0.873 | 0.780 | 0.977 | 0.0184* | 0.675 | 0.494 | 0.923 | 0.0137* |
| Seizure Disorders and Convulsions | 0.680 | 0.612 | 0.755 | <.0001* | 0.699 | 0.623 | 0.784 | <.0001* | 0.647 | 0.496 | 0.844 | 0.0013* |
| Ischemic or Unspecified Stroke | 0.833 | 0.749 | 0.928 | 0.0009* | 0.830 | 0.742 | 0.928 | 0.0011* | 0.759 | 0.514 | 1.119 | 0.1638 |
| Rheumatoid Arthritis and Inflammatory Connective Tissue Disease | 0.924 | 0.830 | 1.029 | 0.1513 | 0.937 | 0.837 | 1.050 | 0.2633 | 0.789 | 0.560 | 1.112 | 0.1759 |
| Morbid Obesity | 0.894 | 0.798 | 1.001 | 0.0511 | 0.879 | 0.780 | 0.990 | 0.0340* | 1.131 | 0.787 | 1.625 | 0.5051 |
| Unstable Angina and Other Acute Ischemic Heart Disease | 0.887 | 0.777 | 1.012 | 0.0744 | 0.879 | 0.764 | 1.011 | 0.0700 | 0.908 | 0.601 | 1.372 | 0.6468 |
| Other Significant Endocrine and Metabolic Disorders | 0.968 | 0.843 | 1.110 | 0.6398 | 1.000 | 0.860 | 1.163 | 0.9956 | 0.942 | 0.671 | 1.322 | 0.7293 |
| Parkinson's and Huntington's Diseases | 0.708 | 0.615 | 0.816 | <.0001* | 0.742 | 0.639 | 0.862 | <.0001* | 0.507 | 0.321 | 0.800 | 0.0035* |
| Major Depressive, Bipolar, and Paranoid Disorders | 0.579 | 0.498 | 0.674 | <.0001* | 0.600 | 0.511 | 0.704 | <.0001* | 0.473 | 0.300 | 0.747 | 0.0013* |
| Intestinal Obstruction/Perforation | 0.961 | 0.820 | 1.126 | 0.6242 | 0.891 | 0.751 | 1.056 | 0.1832 | 1.589 | 1.008 | 2.504 | 0.0461* |
| Breast, Prostate, and Other Cancers and Tumors | 0.890 | 0.756 | 1.046 | 0.1579 | 0.886 | 0.745 | 1.054 | 0.1714 | 1.014 | 0.637 | 1.615 | 0.9534 |
| Acute Myocardial Infarction | 1.005 | 0.851 | 1.186 | 0.9542 | 1.019 | 0.855 | 1.214 | 0.8358 | 0.805 | 0.486 | 1.335 | 0.4007 |
| Cerebral Hemorrhage | 0.678 | 0.574 | 0.801 | <.0001* | 0.761 | 0.619 | 0.934 | 0.0090* | 0.619 | 0.461 | 0.831 | 0.0014* |
| Aspiration and Specified Bacterial Pneumonias | 0.987 | 0.823 | 1.183 | 0.8865 | 0.990 | 0.814 | 1.203 | 0.9189 | 1.086 | 0.662 | 1.779 | 0.7444 |
| Vascular Disease with Complications | 0.889 | 0.748 | 1.056 | 0.1804 | 0.790 | 0.656 | 0.952 | 0.0131* | 1.822 | 1.125 | 2.950 | 0.0147* |
| Chronic Ulcer of Skin, Except Pressure | 0.828 | 0.693 | 0.990 | 0.0387* | 0.911 | 0.754 | 1.100 | 0.3329 | 0.406 | 0.229 | 0.720 | 0.0020* |
| Metastatic Cancer and Acute Leukemia | 0.781 | 0.653 | 0.934 | 0.0069* | 0.764 | 0.626 | 0.931 | 0.0077* | 0.904 | 0.590 | 1.384 | 0.6410 |
| Coma, Brain Compression/Anoxic Damage | 1.031 | 0.854 | 1.244 | 0.7509 | 1.214 | 0.956 | 1.541 | 0.1108 | 0.947 | 0.689 | 1.301 | 0.7359 |
| Artificial Openings for Feeding or Elimination | 0.978 | 0.811 | 1.181 | 0.8205 | 1.014 | 0.827 | 1.242 | 0.8938 | 0.774 | 0.464 | 1.291 | 0.3262 |
| Number of Stroke Discharges from acute | 1.009 | 1.008 | 1.010 | <.0001* | 1.009 | 1.008 | 1.010 | <.0001* | 1.005 | 1.004 | 1.006 | <.0001* |
| Distance from Acute Hospital to PAC setting (Miles), Mean (SD) | 1.000 | 1.000 | 1.000 | 0.7550 | 1.000 | 1.000 | 1.000 | 0.5224 | 1.000 | 0.999 | 1.001 | 0.4106 |
| Medicaid Eligibility (Yes vs No) | 0.592 | 0.571 | 0.615 | <.0001* | 0.599 | 0.576 | 0.623 | <.0001* | 0.547 | 0.490 | 0.611 | <.0001* |
| Admission Mobility Score | 1.054 | 1.051 | 1.057 | <.0001* | 1.053 | 1.050 | 1.055 | <.0001* | 1.064 | 1.056 | 1.071 | <.0001* |
| Admission Self-Care Score | 0.981 | 0.979 | 0.983 | <.0001* | 0.981 | 0.979 | 0.983 | <.0001* | 0.980 | 0.975 | 0.985 | <.0001* |
|
| ||||||||||||
| −2 Res Log Pseudo-Likelihood | 553847.6 | 491081.4 | 61269.16 | |||||||||
| Gener. Chi-Square / DF | 0.95 | 0.94 | 0.91 | |||||||||
Note.
ICU, intensive care unit; CCU, coronary care unit
, Significance at an alpha level of 0.05.
Table 4 presents the amount of variation (ICC) in discharges to IRF vs. SNF attributed to the acute care hospitals by stroke type. There was more variation in acute hospital discharge to stroke rehabilitation for those with ischemic stroke compared to those with hemorrhagic stroke regardless of patient and facility characteristics. The ICC values of the null models for ischemic and hemorrhagic stroke were 0.316 and 0.168, respectively. When we adjusted patient characteristics (age, sex, race, top 30 HCCs, length of stay in acute care, function scores, and Medicaid eligibility), the ICC values for ischemic and hemorrhagic stroke increased to 8.22% (ICC=0.342) and 11.3% (ICC=0.187) respectively. However, when we additionally adjusted for facility characteristics (number of stroke discharges from acute hospitals and distance from acute hospital to PAC setting) with patient characteristics (age, sex, race, top 30 HCCs, length of stay in acute care, function scores, and Medicaid eligibility), the ICC values decreased to 7.01% (ICC=0.318) and 5.88% (ICC=0.176).
Table 4.
Intraclass Correlation (ICC) values: Amount of variation in discharges to inpatient rehabilitation (IRF) across the 3677 acute hospitals by stroke type
| Intraclass Correlation (ICC) | |||
|---|---|---|---|
|
|
|||
| All Stroke |
Ischemic Stroke |
Hemorrhagic Stroke |
|
| Null Model | 0.315 | 0.316 | 0.168 |
| Adjusted for Patient Characteristics† | 0.343 | 0.342 | 0.187 |
| Adjusted for Patient & Facility Characteristics‡ | 0.319 | 0.318 | 0.176 |
Note.
, Age, sex, race, top 30 HCCs, length of stay in acute care, Medicaid eligibility, function scores
, Age, sex, race, top 30 HCCs, length of stay in acute care, Medicaid eligibility, function scores, number of stroke discharges from acute hospitals, distance from acute hospital to PAC setting (miles)
Discussion
We explored discharge patterns and differences in characteristics among patients with ischemic and hemorrhagic stroke who transitioned from acute care hospitals to IRF and SNF settings. The study findings suggest considerable variation in stroke patients who received IRF and SNF rehabilitation attributed to acute hospitals. Even after adjusting for patient and facility-level characteristics, variation in the use of IRF and SNF remained. When considering discharges from acute care by stroke type (ischemic vs hemorrhagic), our findings indicate that there was greater variation in ischemic stroke discharge to IRF than hemorrhagic stroke (ICCs= 0.318 and 0.176, respectively). These findings are consistent with prior studies examining hospital variation for ischemic stroke.5,6 Our finding of lesser but considerable variation for hemorrhagic stroke that is only partially attributable to patient and facility level factors is noteworthy. Researchers examining variation have shown that there is less variation in procedures and healthcare use when there is more agreement or established guidelines driving practice decisions.30 With respect to stroke rehabilitation, those with hemorrhagic events are typically more severe and as such have a more clear need for rehabilitative services. Conversely ischemic events are more likely to resolve or result in less disabling conditions as shown by the higher functional status found in our study. As a result there may be more debate about the rehabilitation needs and the intensity of care. As part of this debate, some have suggested that the patient’s potential to benefit from rehabilitation influences discharge planning decisions,31–33 which likely also contributes to the variation differences between hemorrhagic and ischemic stroke.
Descriptively, our study shows that discharge for IRF and SNF stroke rehabilitation is multifactorial and not clearly associated with stroke complexity. We explored several indicators of stroke severity including length of stay in acute, the use of intensive care, medical comorbidities and functional limitations. Our findings suggest that there is not a clear distinction between complexity variables and discharge placement. Regardless of stroke type patients with longer lengths of stay in acute care were more likely to be discharged to SNF settings, while those with an intensive care unit stays during acute care were more likely to receiver IRF rehabilitation. Similar to other health services studies of PAC4,34 our study found that those with comorbidities were more likely to discharge to SNF rehabilitation while those with higher self-care and mobility capacity were more likely to go to IRF settings regardless of whether they had an ischemic or hemorrhagic stroke. For example, those with depression were less likely to receive IRF rehabilitation. These findings provide valuable information for physiatrists, other rehabilitation clinicians, and hospital administrators involved in PAC discharge planning decisions as well as those who provide care in IRF and SNF settings. Clinicians in SNF settings should be aware of the higher percentage of depression and may need to focus on monitoring and treating depressive symptoms among patients regardless of stroke type. Overall, our findings highlight the need for open discussions during care transitions from acute care to IRF and SNF rehabilitation, as well as studies that explore factors and acute care processes that influence discharge to PAC following stroke beyond demographic and clinical factors.
Our study findings indicate that demographics as well as stroke comorbidities were significantly different across IRFs and SNFs. These results support findings of unexplained variation in hospital use of IRF and SNF.14 Regardless of stroke type, patients admitted to SNFs had higher percentages of comorbidities than those who admitted to IRF, suggesting that those discharged to SNF had more residual impairments or disabilities prior to their index stroke. Knowledge of differences in acute discharges for hemorrhagic and ischemic stroke will allow researchers to develop conditional probability models that investigate stroke rehabilitation outcomes and potentially the cost effectiveness of IRF and SNF services.
An interesting finding from our study was that the variation attributed to acute hospitals rose when we introduce patient and facility-level factors within multilevel models. This finding is similar to Reistetter et al. (2015) study of functional status following stroke rehabilitation and reflects the masking effects of patient level characteristics.35 While the ICC usually decreases when adding covariates compared to a null model,36 our findings revealed that the ICC increased when adjusting for patient and facility characteristics (ischemic stroke=8.22% and hemorrhagic stroke=11.3%). Adding facility level variables reduced the ICC closer to the ICC in the null model for ischemic stroke. The ICC for hemorrhagic stroke remains meaningful compared to the ICC in the null model. These results suggest that admission practices or patterns across acute facilities are potentially influencing rehabilitation use. This finding indicates that patient characteristics and facility case mix is masking variation in discharges to PAC settings and suggests that systematic selection of patients at acute care is suppressing differences in acute care use of IRF and SNF rehabilitation.35 This suggests that differing discharge practice patterns, policies or procedures across acute care facilities may be influencing the discharge destination decisions. This finding supports the second purpose of our study and highlights the need for careful consideration of patient and clinical characteristics for those receiving IRF and SNF stroke rehabilitation.
An important issue influencing the PAC discharge decision process is the rapidly changing PAC practice environment. Current healthcare reform efforts targeting quality measures, transitions in care and delivery systems will have considerable impact on the use of IRF and SNF rehabilitation.37 With respect to IRF and SNF settings quality measure reporting on functional status, pressure injury, and care transitions began in 2016 consistent with the Improving Medicare Post-Acute Care Transition (IMPACT) Act.38 Our study supports the need to focus on these quality indicators in stroke rehabilitation.
Other policy effort influencing PAC stroke rehabilitation and transitions from acute care to IRF and SNF settings include site neutral payment,39 Accountable Care Organizations, and the Bundled Care Initiative.40 These efforts address healthcare delivery to manage service use and payment.40 Our findings of variation in acute care use of IRF and SNF rehabilitation as well as the patient and facility factors associated with IRF and SNF are of use to Accountable Care Organizations and the Center for Medicare and Medicaid services,7 as they seek to improve service delivery and quality outcomes in the most cost effective mechanism possible. Figure 3 also demonstrated that there were differences in acute care discharges across IRF and SNF. This finding highlights the need to adjust for hospital-level characteristics when comparing stroke rehabilitation outcomes.
Our study has several limitations. First, we only included IRF and SNF settings in our analysis. We did this because our focus was to examine those with comparable stroke events. As a result, our findings are not applicable to other rehabilitation venues like home health care, long-term acute care, or outpatient care. Also, our ICC estimation was conditional on discharges to IRF and SNF and not applicable to all PAC settings. Furthermore, we used function scores (self-care and mobility) at admission to compare the baseline functional status across IRFs and SNFs. We performed sensitivity analysis of variation models with and without functional scores and found the results to be similar. Consistent with other studies, we believe function plays a critical role in stroke rehabilitation and therefore reported functional scores within the model (Tables 3 and 4). These functional score comparisons were conducted based on the Rasch common-person equating methodologies (crosswalks between the FIM and MDS) from previous research.26 We attempted to construct a cognitive measure from the IRF-PAI and MDS items but were unable due to low precision of the MDS items. Likewise, researchers have shown that the cognitive items of the FIM consistently demonstrated low precision compared to the motor items.41 Given that cognition relates to overall functional status, future studies should include comparable cognitive scores across IRFs and SNF. In addition, inconsistent raters for the function (IRF-PAI by rehabilitation therapists and MDS by mostly nurses) might influence functional scores across PAC settings. Lastly, functional scores were from the PAC admission, not the acute hospital, which may not reflect patient functioning in the acute hospital. Therefore, functional crosswalk scores may not accurately reflect the use of function in the decision process to discharge to IRF and SNF. In addition, unmeasured variables (i.e., living situation prior, marital status, and/or able caregiver) might influence the differences in functional scores at the discharge from acute hospitals. The decision making process may also be based upon severity and complication that occurred in the acute setting other than the ICU stay not included in our study. Future studies exploring discharge processes are needed. Other geographic factors and availability also influence discharge patterns from acute hospitals to IRF and SNF.42 Future studies should control geographical factors. Even given these limitations, our findings provide valuable information for understanding patient characteristics and differences among those discharged to inpatient and skilled nursing stroke rehabilitation.
Conclusion
We found variation in acute hospital discharge patterns to IRF and SNF rehabilitation following ischemic and hemorrhagic stroke. Characteristics for patients with stroke who discharged from acute hospitals to IRF and SNF settings differed by demographic and clinical factors. Regardless of stroke type, those discharged to SNF were older, female, with greater medical comorbidities and lower self-care and mobility skills than those who went to IRF. Our findings provide clinicians and health policy makers with practical information about who receives IRF and SNF stroke rehabilitation. Additionally, our study highlights the presence of variation in discharge practices attributed to acute care settings by stroke type. These findings suggest the need for careful consideration of case mix and facility factors in comparative effectiveness studies for stroke rehabilitation. Based on the study findings, future research is needed controlling differences in stroke covariates with propensity score models to determine which setting yields the highest functional outcome following stroke.
Supplementary Material
Acknowledgments
This study was supported with funding from the Agency for Healthcare Quality and Research (R01-HS024711, R24-HS022134), National Institutes of Health (R01-AG033134; R24-HD065702; R01-HD069443; and K01-HD086290), National Institute on Aging OAIC (5P30-AG024832), Institute for Translational Sciences (UL1TR000071).
Footnotes
Conflict of Interest: None declared.
Financial benefits to the authors: Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
Suppliers
SAS statistical software version 9.4.
References
- 1.Centers for Disease Control Prevention. [Accessed December 1, 2017];Stroke facts. 2017 https://www.cdc.gov/stroke/facts.htm.
- 2.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare Medicaid Services. Medicare program; prospective payment system and consolidated billing for skilled nursing facilities for FY 2017, SNF value-based purchasing program, SNF quality reporting program, and SNF payment models research. final rule. Federal register. 2016;81(151):51969. [PubMed] [Google Scholar]
- 4.Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after postacute care for stroke and hip fracture. Med Care. 2010;48(9):776–784. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bettger JP, Thomas L, Liang L, et al. Hospital variation in functional recovery after stroke. Circ Cardiovasc Qual Outcomes. 2017;10:e002391. doi: 10.1161/CIRCOUTCOMES.115.002391. [DOI] [PubMed] [Google Scholar]
- 6.Kind AJ, Smith MA, Liou JI, Pandhi N, Frytak JR, Finch MD. Discharge destination's effect on bounce-back risk in black, white, and Hispanic acute ischemic stroke patients. Arch Phys Med Rehabil. 2010;91(2):189–195. doi: 10.1016/j.apmr.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Medicare & Medicaid Services. [Accessed April 24, 2016];Bundled payments for care improvement (BPCI) initiative: general information. 2016 https://innovationcmsgov/initiatives/bundled-payments/
- 8.Dummit LA, Kahvecioglu D, Marrufo G, et al. Association between hospital participation in a medicare bundled payment initiative and payments and quality outcomes for lower extremity joint replacement episodes. JAMA. 2016;316(12):1267–1278. doi: 10.1001/jama.2016.12717. [DOI] [PubMed] [Google Scholar]
- 9.Patient Protection and Affordable Care Act. 2010. Pub. L. 111–148, 42 U.S.C. §§18001–18121.
- 10.McWilliams JM, Gilstrap LG, Stevenson DG, Chernew ME, Huskamp HA, Grabowski DC. Changes in postacute care in the medicare shared savings program. JAMA Intern Med. 2017;177(4):518–526. doi: 10.1001/jamainternmed.2016.9115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Graham JE, Prvu Bettger J, Middleton A, Spratt H, Sharma G, Ottenbacher KJ. Effects of acute-postacute continuity on community discharge and 30-day rehospitalization following inpatient rehabilitation. Health Serv Res. 2017;52(5):1631–1646. doi: 10.1111/1475-6773.12678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magdon-Ismail Z, Sicklick A, Hedeman R, Bettger JP, Stein J. Selection of postacute stroke rehabilitation facilities: a survey of discharge planners from the northeast cerebrovascular consortium (NECC) region. Medicine. 2016;95(16):e3206. doi: 10.1097/MD.0000000000003206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy GM, Brock KA, Lunt AW, Black SJ. Factors influencing selection for rehabilitation after stroke: a questionnaire using case scenarios to investigate physician perspectives and level of agreement. Arch Phys Med Rehabil. 2012;93(8):1457–1459. doi: 10.1016/j.apmr.2011.11.036. [DOI] [PubMed] [Google Scholar]
- 14.Xian Y, Thomas L, Liang L, et al. Unexplained variation for hospitals' use of inpatient rehabilitation and skilled nursing facilities after an acute ischemic stroke. Stroke. 2017;48(10):2836–2842. doi: 10.1161/STROKEAHA.117.016904. [DOI] [PubMed] [Google Scholar]
- 15.Buntin MB. Access to postacute rehabilitation. Arch Phys Med Rehabil. 2007;88(11):1488–1493. doi: 10.1016/j.apmr.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 16.Conroy BE, DeJong G, Horn SD. Hospital-based stroke rehabilitation in the United States. Top Stroke Rehabil. 2009;16(1):34–43. doi: 10.1310/tsr1601-34. [DOI] [PubMed] [Google Scholar]
- 17.Dobkin BH. Rehabilitation after stroke. N Engl J of Med. 2005;352(16):1677–1684. doi: 10.1056/NEJMcp043511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan L, Sandel ME, Jette AM, et al. Does postacute care site matter? a longitudinal study assessing functional recovery after a stroke. Arch Phys Med Rehabil. 2013;94(4):622–629. doi: 10.1016/j.apmr.2012.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ottenbacher KJ, Smith PM, Illig SB, et al. Disparity in health services and outcomes for persons with hip fracture and lower extremity joint replacement. Med Care. 2003;41(2):232–241. doi: 10.1097/01.MLR.0000044902.01597.54. [DOI] [PubMed] [Google Scholar]
- 20.Harada ND, Chun A, Chiu V, Pakalniskis A. Patterns of rehabilitation utilization after hip fracture in acute hospitals and skilled nursing facilities. Med Care. 2000;38(11):1119–1130. doi: 10.1097/00005650-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 21.DeJong G. Are we asking the right question about postacute settings of care? Arch Phys Med Rehabil. 2014;95(2):218–221. doi: 10.1016/j.apmr.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Brinjikji W, Rabinstein AA, Cloft HJ. Hospitalization costs for acute ischemic stroke patients treated with intravenous thrombolysis in the United States are substantially higher than medicare payments. Stroke. 2012;43(4):1131–1133. doi: 10.1161/STROKEAHA.111.636142. [DOI] [PubMed] [Google Scholar]
- 23.National Quality Forum. [Accessed April 24, 2016];Risk adjustment for socioeconomic status or other sociodemographic factors. 2014 http://www.qualityforum.org/Home.aspx.
- 24.Sung SF, Chen SC, Hsieh CY, Li CY, Lai EC, Hu YH. A comparison of stroke severity proxy measures for claims data research: a population-based cohort study. Pharmacoepidemiol Drug Saf. 2016;25(4):438–443. doi: 10.1002/pds.3944. [DOI] [PubMed] [Google Scholar]
- 25.Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004;25(4):119–141. [PMC free article] [PubMed] [Google Scholar]
- 26.Mallinson TR, Deutsch A, Heinemann AW, Bateman J. Comparing function across post-acute rehabilitation settings after co-calibration of self-care and mobility items; ACRM-ASNR Annual Conference; 2012; Vancouver, Canada. [Google Scholar]
- 27.Masters GN. Common-person equating with the Rasch model. Applied Psychological Measurement. 1985;9(1):73–82. [Google Scholar]
- 28.Hox JJ, Moerbeek M, van de Schoot R. Multilevel analysis: techniques and applications. Routledge: 2010. [Google Scholar]
- 29.Goldstein H, Browne W, Rasbash J. Partitioning variation in multilevel models. Understanding Statistics: Statistical Issues in Psychology, Education, and the Social Sciences. 2002;1(4):223–231. [Google Scholar]
- 30.Birkmeyer JD, Sharp SM, Finlayson SRG, Fisher ES, Wennberg JE. Variation profiles of common surgical procedures. Surgery. 1998;124(5):917–923. [PubMed] [Google Scholar]
- 31.Ilett PA, Brock KA, Graven CJ, Cotton SM. Selecting patients for rehabilitation after acute stroke: are there variations in practice? Arch Phys Med Rehabil. 2010;91(5):788–793. doi: 10.1016/j.apmr.2009.11.028. [DOI] [PubMed] [Google Scholar]
- 32.Dennis M. Predictions models in acute stroke: potential uses and limitations. Stroke. 2008;39(6):1665–1666. doi: 10.1161/STROKEAHA.107.510271. [DOI] [PubMed] [Google Scholar]
- 33.Wade DT. Selection criteria for rehabilitation services. Clin Rehabil. 2003;17(2):115–118. doi: 10.1191/0269215503cr591ed. [DOI] [PubMed] [Google Scholar]
- 34.Deutsch A, Granger CV, Heinemann AW, et al. Poststroke rehabilitation: outcomes and reimbursement of inpatient rehabilitation facilities and subacute rehabilitation programs. Stroke. 2006;37(6):1477–1482. doi: 10.1161/01.STR.0000221172.99375.5a. [DOI] [PubMed] [Google Scholar]
- 35.Reistetter TA, Kuo YF, Karmarkar AM, et al. Geographic and facility variation in inpatient stroke rehabilitation: multilevel analysis of functional status. Arch Phys Med Rehabil. 2015;96(7):1248–1254. doi: 10.1016/j.apmr.2015.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1998;23(4):323–355. [Google Scholar]
- 37.DeJong G. Coming to Terms With the IMPACT Act of 2014. Am J Occup Ther. 2016;70(3) doi: 10.5014/ajot.2016.703003. 7003090010p7003090011-7003090010p7003090016. [DOI] [PubMed] [Google Scholar]
- 38.Improving Medicare Post-Acute Transformation Act of 2014, Pub. L. 113–185, 128 Stat. 1952 (1801 U.S.C. 6001 et seq.).
- 39.Medicare Payment Advisory Committee. [Accessed May 3, 2016];Report to the congress: medicare and the health care delivery system. 2016 http://www.medpac.gov/docs/default-source/reports/june-2016-report-to-the-congress-medicare-and-the-health-care-delivery-system.pdf?sfvrsn=0.
- 40.Matchar DB, Nguyen HV, Tian Y. Bundled payment and care of acute stroke. Stroke. 2015;46(5):1414–1421. doi: 10.1161/STROKEAHA.115.009089. [DOI] [PubMed] [Google Scholar]
- 41.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 42.Buntin MB, Garten A, Totten M, Paddock S, Saliba D, Escarce J. How much is post-acute care use affected by its availability+ accessibility. Health Serv Res. 2005;40(2):413–434. doi: 10.1111/j.1475-6773.2005.00365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.