A 48-year-old man with a medical history of metastatic small-bowel neuroendocrine tumor, who was using chemotherapy, presented with nausea, vomiting, and right upper-quadrant abdominal pain. His laboratory tests demonstrated abnormal liver enzymes (bilirubin 2.7 mg/dL, alkaline phosphatase 187 mg/dL, aspartate aminotransferase 174 mg/dL, and alanine aminotransferase 89 mg/dL). He had a low hemoglobin of 10.6 mg/dL. His liver enzymes and hemoglobin were normal 1 week before the presentation.
He underwent US of the abdomen and a CT scan of the abdomen without contrast material because of his worsening kidney function. US and CT without contrast material revealed newly diagnosed liver metastasis. MRCP demonstrated prominence of the intrahepatic duct. During the hospital stay, his liver function normalized and his abdominal pain resolved; he was discharged home. Two days later he was seen because of recurrence of abdominal pain and worsening of liver enzymes (bilirubin 4 mg/dL, alkaline phosphatase 366 mg/dL, aspartate aminotransferase 125 mg/dL, and alanine aminotransferase 145 mg/dL).
A hepato-iminodiacetic acid scan, obtained to rule out biliary obstruction as a cause of his elevated liver enzymes, revealed prompt liver uptake without excretion, suggestive of high-grade biliary obstruction.
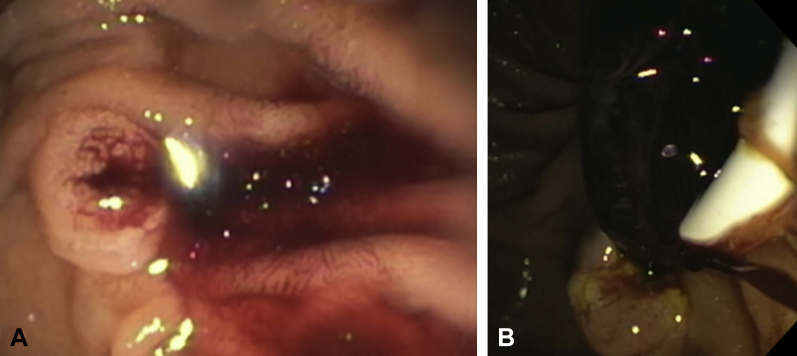
ERCP was performed, and blood was noted at the ampulla, raising suspicion for hemobilia (Fig. 1A). The common bile duct (CBD) was cannulated, and sphincterotomy was performed, followed by securing wire into the right and left hepatic ducts. The CBD was swept with a 12-mm balloon, and a large blood clot was extracted from the CBD (Fig. 1B). The right and left intrahepatic ducts were swept, and a small clot was removed. Two 10F × 15-cm plastic stents were placed into the right and left hepatic ducts to prevent recurrence of biliary obstruction. He maintained hemodynamic and hemoglobin stability after the procedure (Video 1, available online at www.VideoGIE.org).
Figure 1.
A, Endoscopic view of duodenoscope-demonstrated hemobilia. B, Balloon sweep with extraction of well-organized blood clot during ERCP.
The patient’s liver enzyme levels improved after the procedure. He was discharged home the following day. The patient was followed up by his oncologist, and capecitabine and temozolomide were started. Four weeks after the procedure, he maintained normal liver function. ERCP was performed to remove the biliary stents 4 weeks later. After removal of the biliary stents, a biliary sweep was performed, and no blood was seen during the procedure. Follow-up MRCP 8 weeks after the procedure did not show biliary obstruction or compression.
In conclusion, a newly diagnosed liver metastasis can present with hemobilia. Hemobilia and bile duct clots are a rare cause of recurrent biliary obstruction that can be missed by conventional imaging studies. ERCP with plastic stent placement can be used to maintain biliary drainage and prevent recurrent obstruction.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Endoscopic retrograde cholangiopancreatography for management of hemobilia.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic retrograde cholangiopancreatography for management of hemobilia.